Abstract
Background
Maternal smoking during pregnancy carries significant health risks for both mothers and infants, especially in vulnerable regions like rural and Appalachian areas with high smoking rates. Understanding the causes of high smoking rates in vulnerable areas is crucial for designing effective interventions to promote smoking cessation and reduce preventable health disparities.
Methods
Data from the Virginia Pregnancy Risk Assessment Monitoring System (PRAMS; years 2009–2020) comprised of 7,861 women aged over 18 were used in this cross-sectional observational study. Pregnant individuals were categorized as smoking if they reported smoking during the last trimester. A multi-level logistic regression was employed to examine the association of individual sociodemographic factors, rurality, Appalachian status, and county socioeconomic status (SES) proxied by Yost Index quintiles with smoking behaviors during pregnancy. The county of residence was considered as a random factor in the analysis. Trend analysis were also conducted.
Results
Out of the overall sample, 92.8% (n = 7,292) were non-smokers, while 7.2% (n = 569) were smokers. The multi-level logistic regression analysis showed pregnant individuals aged 18–24 had 1.06 times higher odds of smoking compared to those over 35 (95% CI [1.02–1.10]). Those with a college education or higher had significantly reduced odds (OR: 0.10, 95% CI [0.10, 0.10]), as did racially minoritized individuals (OR: 0.59, 95% CI [0.51–0.68]) and Hispanic individuals (OR: 0.14, 95% CI [0.09–0.21]). Living in rural areas was associated with a 26% higher likelihood of smoking during pregnancy compared to urban areas (OR: 1.26, 95% CI [1.21–1.31]), while residing in Appalachian regions led to a 25% higher probability of smoking. Additionally, lower SES quintiles were linked to higher odds of smoking, with the lowest quintile at OR: 2.10 (95% CI [1.67–2.65]) and the second quintile at OR: 1.64 (95% CI [1.53–1.76]) as compared with the most affluent quintile. Trend analsysis shows smoking has declined across all quintiles, but a substantial gap persists between lowest and highest SES regions.
Conclusions
Smoking rates during pregnancy have dropped overall but remain alarmingly high in specific rural and Appalachian areas. As smoking during pregnancy poses significant health risks, targeted interventions and resources for tobacco cessation programs are needed in these highly vulnerable regions.
Trial registration
Not Applicable.
Keywords: Pregnancy smoking, Rural areas, Vulnerable populations, Tobacco cessation, Composite socioeconomic index
Introduction
Maternal smoking during pregnancy poses substantial risks to the health of both mothers and infants, leading to adverse outcomes such as miscarriage, stillbirth, placental abruption, and low birth weight [1]. Despite extensive documentation of these risks, prenatal smoking remains prevalent among pregnant women [2], particularly in certain regions of the U.S.
In 2016, 7.2% of pregnant women smoked during pregnancy in the U.S [3]. Some Geographic regions in the U.S., notably the Appalachian area, have reported significantly higher rates of prenatal smoking. The Appalachian region of the U.S. makes up 423 counties across 13 states beginning in southern New York and stretching through northern Mississippi [4]. Furthermore, prenatal smoking rates have consistently been higher in rural areas compared to urban regions in this region [5, 6]. These geographical disparities in smoking rates highlights variations in prenatal health behaviors, underscoring the necessity for region-specific research on these issues.
Previous research has identified a wide range of factors contributing to the disproportionate prevalence of maternal smoking in rural areas during pregnancy, encompassing lower educational attainment, socioeconomic status (SES), and health literacy, as well as elevated unemployment rates [7]. Moreover, rural regions commonly face a scarcity of healthcare providers and resources, amplifying the challenges for pregnant women seeking support to quit smoking [8].
Additionally, smoking may be more socially acceptable in certain rural communities, complicating efforts for smoking cessation. A study by Campbell et al. 2018 suggested that social acceptance of smoking acts as a substantial obstacle to quitting [9]. Additionally, tobacco cultivation in rural Appalachian communities serves as a crucial source of income, further reinforcing both its relevance and prevalence [10].
Previous studies [7] on socioeconomic factors have predominantly concentrated on individual variables such as poverty, income, and employment [11]. However, SES is a multifaceted concept, and the interplay among various factors—such as income, education, employment type, and housing conditions—can collectively influence and contribute to risky health behaviors. Despite numerous studies focusing on individual factors, there remains limited understanding of the interrelations among these factors that could elucidate smoking behaviors.
This study aims to fill this gap by employing the Yost index [12], a composite measure derived from seven critical county-level socioeconomic deprivation indicators (including median household income, median home value, median rent, the percentage of individuals below 150% of the federal poverty line, unemployment rate, the proportion engaged in working-class occupations, and an educational achievement index). Numerous studies have validated the effectiveness of the Yost Index in assessing social determinants of health outcomes, but none have yet utilized it to understand smoking prevalence, nor has it been evaluated specifically among pregnant women. The current study utilizes this index to gain a comprehensive insight into SES and its influence on smoking behavior during pregnancy, to further understanding of the disproportionately high rates of smoking in rural and Appalachian areas.
Methods
Study sample
Data for this cross-sectional observational study were from the Virginia Pregnancy Risk Assessment Monitoring System (PRAMS) collected between 2009 and 2020 [13]. In Virginia (consistent with the general PRAMS methodology used in each participating state/area), birth certificate records are used to select a representative sample of all women who delivered a live-born infant. These women are then contacted to complete the survey by either mail or telephone. The weighted response rate ranged from 57.6 to 65% over the years of data used in these analyses. In this study, the sample comprised 7,861 women aged over 18 from Virginia, excluding individuals lacking data on location and key demographic information such as age, race, education, and marital status (n = 592, 7%). Study procedures were approved by the Virginia Department of Health and the University of Virginia Institutional Review Board.
Measures
Sociodemographic characteristics
Participants self-reported their race, ethnicity, education, and age.
Smoking behaviors
Participants also reported on their cigarette smoking behaviors during the final three months of pregnancy (third trimester). Pregnant individuals were categorized as smoking if they reported smoking during the last trimester; otherwise, they were classified as non-smoking. Smoking status is the primary outcome variable of the study.
Rurality and region
We classified the counties where each participant resided using the Rural-Urban Continuum Codes (2013), with code values 1–3 classified as urban and code values 4–9 classified as rural [14]. Counties were considered Appalachian or non-Appalachian based on the Appalachian Regional Commission database [15].
County-level socioeconomic status
The Yost Index, employed by the National Cancer Institute, serves as a comprehensive measure to evaluate SES at the county level. Derived from geocoded patient data, this validated composite score includes seven SES parameters: median household income, median home value, median rent, the percentage of individuals below 150% of the federal poverty line, unemployment rate, the proportion engaged in working-class occupations, and an educational achievement index. We aligned the PRAMS data from 2009 to 2016 with the respective Yost index. However, for the years 2017 to 2020, we utilized the 2016 Yost index as it is the most recent available data. Typically, the Yost Index is segmented into quintiles, with the lowest SES designated in the first quintile (representing the most vulnerable counties, or the lowest SES) and the highest in the 5th quintile represents the more affluent areas (highest SES) [12]. The primary exposure of interest in the study is the categorical Yost index.
Statistical analysis
Chi-squared tests were applied to evaluate significant differences in the characteristics of pregnant individuals and the attributes related to their county of residence, comparing non-smoking and smoking subgroups. A multi-level logistic regression was utilized to explore the connection between individual sociodemographic characteristics (e.g., age, race, ethnicity, marital status), rurality, Appalachian status, and county SES with smoking behaviors, with the county of residence serving as the random intercept. The analyses were conducted using clustered robust standard errors and were executed using STATA 18 [16]. The level of significance was set at α = 0.05.
Results
Table 1 provides sample statistics based on smoking status. The non-smoking subgroup constituted 92.8% (n = 7,292) of the participants, while the smoking subgroup accounted for 7.2% (n = 569). Pregnant individuals who reported smoking tended to be in the youngest age category (31.1%, aged 18–24 years) compared to only 17.1% of the non-smoking subgroup (p < 0.001). The smoking subgroup had lower education compared to the non-smoking subgroups (91.2% vs. 53.1% had some college or less (p < 0.001). Differences in race were not significant; however, the non-smoking subgroup had a higher prevalence of Hispanic individuals (14.4% vs. 3.2%, p < 0.001). Rural areas showed higher smoking rates 17.6% ( ) compared to urban areas (6.2%=
) compared to urban areas (6.2%= , p < 0.001). While 18.6% (
, p < 0.001). While 18.6% ( ) of respondents from Appalachian counties reported smoking, compared to 6.7% (=
) of respondents from Appalachian counties reported smoking, compared to 6.7% (= ) of respondents from non-Appalachian counties (p = 0.001). The lowest SES areas had rates of smoking respondents at 19.5% (
) of respondents from non-Appalachian counties (p = 0.001). The lowest SES areas had rates of smoking respondents at 19.5% ( ) compared to highest SES areas at 4.0% (
) compared to highest SES areas at 4.0% ( , p < 0.001).
, p < 0.001).
Table 1.
Summary statistics of PRAMS respondent characteristics by smoking status
| Smoking status in last trimester | |||
|---|---|---|---|
| Non-smoking | Smoking | P-value* | |
| N (%) | 7,292.0 (92.8%) | 569.0 (7.2%) | |
| Age group (years) | |||
| 18–24 | 1,246.0 (17.1%) | 177.0 (31.1%) | < 0.001 |
| 25–29 | 2,031.0 (27.9%) | 184.0 (32.3%) | |
| 30–34 | 2,339.0 (32.1%) | 126.0 (22.1%) | |
| 35+ | 1,676.0 (23.0%) | 82.0 (14.4%) | |
| Education level | |||
| Some college or less | 3,875.0 (53.1%) | 519.0 (91.2%) | < 0.001 |
| College degree or more education | 3,417.0 (46.9%) | 50.0 (8.8%) | |
| Race | |||
| Minoritized racial group | 2,637.0 (36.2%) | 187.0 (32.9%) | 0.1 |
| White | 4,655.0 (63.8%) | 382.0 (67.1%) | |
| Ethnicity | |||
| Hispanic | 1,048.0 (14.4%) | 18.0 (3.2%) | < 0.001 |
| Not Hispanic | 6,244.0 (85.6%) | 551.0 (96.8%) | |
| Marital status | |||
| Single | 2,170.0 (29.9%) | 363.0 (64.7%) | < 0.001 |
| Married | 5,090.0 (70.1%) | 198.0 (35.3%) | |
| Rurality a | |||
| Rural | 536.0 (7.4%) | 115.0 (20.2%) | < 0.001 |
| Urban | 6,756.0 (92.6%) | 454.0 (79.8%) | |
| Appalachian | |||
| Non-Appalachian | 7,016.0 (96.2%) | 506.0 (88.9%) | < 0.001 |
| Appalachian | 276.0 (3.8%) | 63.0 (11.1%) | |
| Yost Quintiles b | |||
| Lowest SES | 325.0 (4.5%) | 79.0 (13.9%) | < 0.001 |
| SES-2nd quintile | 2,016.0 (27.6%) | 193.0 (33.9%) | |
| SES-3rd quintile | 802.0 (11.0%) | 83.0 (14.6%) | |
| SES-4th quintile | 1,359.0 (18.6%) | 97.0 (17.0%) | |
| Highest SES | 2,790.0 (38.3%) | 117.0 (20.6%) | |
Note: *The results of the test are derived from a chi-squared test
a Rural-Urban continuum codes were used for rural-urban classifications
b Yost index score includes seven SES parameters: median household income, median home value, median rent, the percentage of individuals below 150% of the federal poverty line, unemployment rate, the proportion engaged in working-class occupations, and an educational achievement index
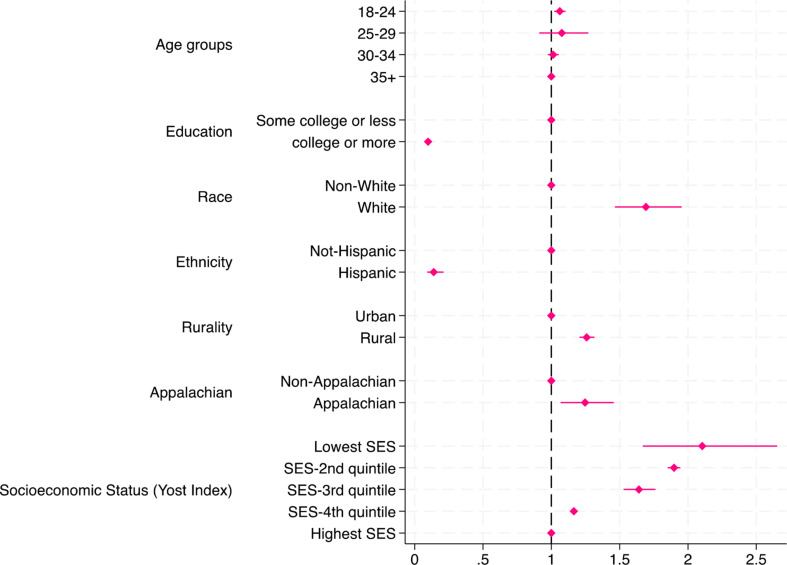
Figure 1 presents the multi-level logistic regression outcomes examining the impact of smoking on the demographic characteristics of pregnant individuals and their county of residence features, such as rurality, Appalachian status, and SES based on the YOST index. Notably, individuals between 18 and 24 years old had 1.06 times higher odds of smoking during pregnancy compared to those over 35 years old (95% confidence interval (CI) [1.02–1.10]). Conversely, those with a college degree or higher demonstrated markedly reduced odds of smoking during pregnancy (odds ratio (OR): 0.10, 95% CI [0.10, 0.10]) compared to individuals with less educational attainment. Racially minoritized individuals had significantly lower odds of smoking during pregnancy compared to White individuals (OR: 0.59, 95% CI [0.51–0.68]). Similarly, Hispanic individuals exhibited notably lower odds of smoking during pregnancy compared to Non-Hispanics (OR: 0.14, 95% CI [0.09–0.21]).
Fig. 1.
Logistic Regression Odds Ratios (with 95% CI) for Smoking: Adjusted for Individual and Residencial Characteristics. Note: Rural-Urban continuum codes were used for rural-urban classifications. Yost index score includes seven SES parameters: median household income, median home value, median rent, the percentage of individuals below 150% of the federal poverty line, unemployment rate, the proportion engaged in working-class occupations, and an educational achievement index
The results also suggest a significant association between rural residence and increased odds of smoking during pregnancy compared to urban areas (OR: 1.26, 95% CI [1.21–1.31]). This signifies a 26% higher likelihood of smoking during pregnancy among pregnant individuals living in rural areas compared to urban areas. Moreover, residing in Appalachian regions was linked to a 25% higher probability of smoking during pregnancy compared to non-Appalachian areas. Analyzing the YOST index revealed that individuals with the lowest quintile of SES were significantly more likely to smoke during pregnancy (OR: 2.10; 95% CI [1.67–2.65]) compared to those in the most affluent 5th quintile. Additionally, individuals in the second quintile had a 64% higher probability of smoking during pregnancy compared to those in the 5th quintile (OR: 1.64, 95% CI [1.53–1.76]). However, even after adjusting for individual characteristics and various county features like rurality, Appalachian status, and the SES, 7% of the variability in smoking among pregnant individuals is due to additional, unmeasured differences between counties.
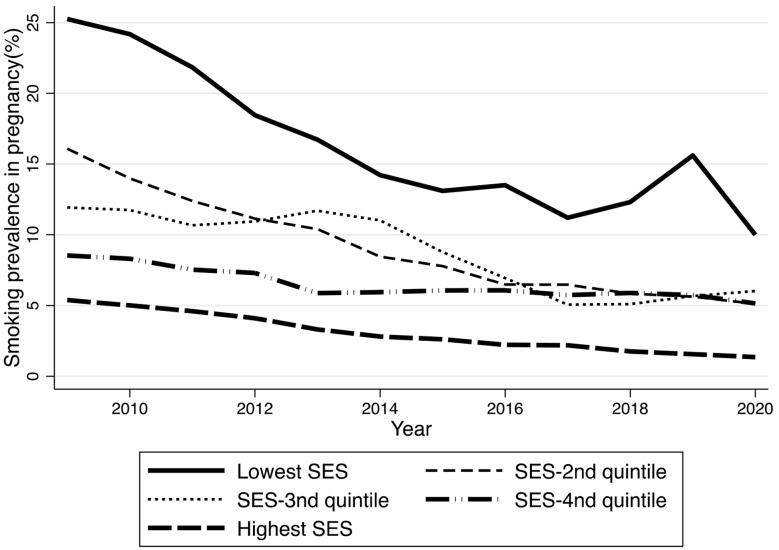
Furthermore, the analysis showed a consistent declining trend in the odds of smoking during pregnancy over time from 2009 to 2020 (OR: 0.38, 95% CI [0.33, 0.46]). Each subsequent year exhibited reduced odds of smoking, suggesting a temporal shift in smoking behavior among pregnant individuals. To provide a more in-depth analysis of the trends, Fig. 2 illustrates a ten-year trajectory of smoking prevalence based on Yost Index Quintiles. While there has been an overall decline in smoking rates across all five SES quintiles, a notable disparity persists between regions characterized by lowest SES and those with highest SES. In contrast, the middle SES groups have shown a convergence in smoking prevalence. Despite this convergence, areas with low SES continue to exhibit markedly high smoking rates (10%).
Fig. 2.
Smoking prevalence trends by Socioeconomic status using Yost Index quintile. Note: Yost index score includes seven SES parameters: median household income, median home value, median rent, the percentage of individuals below 150% of the federal poverty line, unemployment rate, the proportion engaged in working-class occupations, and an educational achievement index
Discussion
Overall rates of smoking during pregnancy remain quite high (7.2%). The findings in this study highlight several influential factors related to smoking behavior during pregnancy. Younger age, lower educational attainment, and lower SES are associated with higher smoking prevalence among pregnant individuals, consistent with previous studies [17–19]. Notably, there was a 26% higher likelihood of smoking during pregnancy among pregnant individuals living in rural areas compared to urban areas. In addition, those who resided in Appalachian regions had a 25% higher probability of smoking during pregnancy compared to non-Appalachian areas. However, even after adjusting for these county-level features, 7% of the variance between counties was associated with unmeasured factors, suggesting that other county-specific factors such as healthcare access and cultural attitudes towards smoking are influencing smoking behaviors among pregnant individuals [20]. Thus, future research should aim to examine other potentially relevant county-level characteristics like tobacco agriculture and health care professional shortages.
Moreover, trends of smoking rates during pregnancy, stratified by SES, highlights a substantial disparity. Despite a sharp decline in pregnancy smoking rates overall, the rates remain quite high (10%) in regions with low SES as compared to highest SES region (1.3%), signaling the need for substantial efforts to address this ongoing issue. Smoking during pregnancy is associated with numerous adverse birth outcomes, including preterm birth, low birth weight, and developmental issues [1]. Therefore, smoking cessation is crucial in mitigating these risks.
Smoking cessation programs tailored to pregnant individuals, especially in low SES regions, could significantly reduce the incidence of these adverse outcomes. Interventions such as behavioral interventions and nicotine replacement therapy have been shown to be effective in helping pregnant individuals quit smoking [21, 22]. Additionally, social support and healthcare provider interventions play a vital role in encouraging and maintaining smoking cessation. By addressing the higher smoking rates in low SES regions through targeted cessation programs, we can improve maternal and infant health outcomes. Our findings underscore the complex interplay of individual characteristics and geographic factors in shaping smoking habits during pregnancy, emphasizing the need for targeted interventions addressing diverse socio-demographic contexts to reduce smoking rates among pregnant individuals.
This study is not without limitations. First, it relies on self-reported smoking habits, which may introduce underreporting due to the social stigma associated with smoking during pregnancy or overreporting due to recall bias, potentially affecting the reliability of the findings. Second, the cross-sectional nature of the study restricts the ability to establish causality or track changes in smoking behaviors over time within individuals. Third, the PRAMS questionnaire used in these analyses only assessed smoking status in the third trimester of pregnancy; thus, we were unable to provide a full picture on smoking behaviors throughout the pregnancy (e.g., quit attempts upon pregnancy confirmation, relapse during pregnancy). Moreover, it does not account for the intensity of smoking during pregnancy, making it unable to distinguish between heavy smoking and lighter smoking. Fourth, as mentioned previously, despite considering various individual and county-level factors, there may be unmeasured variables like psychological factors, stress, or access to support services that could significantly impact smoking behaviors during pregnancy but were not addressed in the analysis. Fifth, these analyses focus solely on cigarette smoking behaviors only, as assessment of e-cigarette use only occurred for a portion of the study period. Finally, the most recent Yost Index available is from 2016. However, as the analysis relies on the discrete quintiles of the Yost index rather than continuous values, and there was no significant change observed in the quintiles of the Yost index for each county from one year to the next, it is unlikely that this significantly impacted the findings.
Despite the limitations, the study’s strengths lie in its utilization of a large and diverse sample, providing a comprehensive insight into smoking behaviors among pregnant individuals. It distinguishes itself by pioneering the use of the Yost index within the context of pregnancy, unlike previous literature that predominantly relied on single socioeconomic variables such as median income and education attainment. While these single item variables offer insights, they lack the capacity to capture the complex interplay among different factors. The use of the Yost index is thus a notable strength as it integrates seven distinct socioeconomic variables, enabling a more comprehensive and nuanced understanding of the multifaceted influences on smoking behaviors among pregnant individuals.
Conclusion
While the past decade has seen a decline in smoking among pregnant individuals, high smoking rates persist, particularly in specific rural and Appalachian areas. Addressing this requires targeted interventions and resource allocation. Allocating resources towards tobacco cessation programs, especially in these vulnerable rural, Appalachian, and low SES areas, is critical to reducing these structural and persistent inequalities. Smoking during pregnancy poses substantial health risks for both mothers and their babies, leading to complications such as preterm birth and low infant birth weight. This study underscores the pressing need for targeted interventions and resource allocation, particularly in these vulnerable areas, to address smoking and enhance health outcomes. Additionally, future work should focus on employing qualitative research methods, such as interviews or focus groups with pregnant individuals who smoke, to uncover underlying reasons and motivations for smoking, as well as barriers to cessation. A more detailed examination of the socioeconomic and cultural factors influencing smoking behaviors at community-level could identify specific community needs and tailor interventions accordingly. Investigating the impact of policy changes, such as taxation, on smoking rates during pregnancy could provide valuable information for public health strategies. Therefore, further research is needed to address these questions, which will offer practical implications for improving maternal and infant health outcomes.
Acknowledgements
The authors would like to thank the Virginia Department of Health’s Tobacco Control Program for their support in conducting this research.
Author contributions
A.P. conducted data analysis, study design, conceptualization, main manuscript writing and editing. A.C. conducted the literature review and manuscript editing. R.K. contributed in conceptualization, study design, manuscript writing and editing. M.L. as the lead contributor contributed to project conceptualization, secured funding, as well as manuscript writing and editing.
Funding
This work was supported by the Cancer Control and Population Health (CPH) program at the University of Virginia Cancer Center, provided through the NIH Cancer Center Support Grant: P30CA044579.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Study procedures were approved by the Virginia Department of Health and the University of Virginia Institutional Review Board in accordance with the principles of the Declaration of Helsinki. All participants provided informed consent. For minors younger than 18 informed consent was waived by CDC (Centers for Disease Control and Prevention).
Human ethics and consent to participate
Not applicable.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.McDonnell BP, Regan C. Smoking in pregnancy: pathophysiology of harm and current evidence for monitoring and cessation. Obstetric Gynaecologis. 2019;21(3):169–75. 10.1111/tog.12585. [Google Scholar]
- 2.Lange S, Probst C, Rehm J, Popova S. National, regional, and global prevalence of smoking during pregnancy in the general population: a systematic review and meta-analysis. Lancet Global Health. 2018;6(7):e769–76. 10.1016/S2214-109X(18)30223-7. [DOI] [PubMed] [Google Scholar]
- 3.Drake P, Driscoll A, Mathews TJ, National Center for Health Statistics (U.S.). Division of Vital Statistics. Cigarette smoking during pregnancy: United States, 2016. Published online February 2018. https://stacks.cdc.gov/view/cdc/52304 [PubMed]
- 4.About the Appalachian Region. Appalachian Regional Commission. Accessed December 19. 2023. https://www.arc.gov/about-the-appalachian-region/
- 5.Nighbor TD, Doogan NJ, Roberts ME et al. Smoking prevalence and trends among a U.S. national sample of women of reproductive age in rural versus urban settings. Cassidy RN, ed. PLoS ONE. 2018;13(11):e0207818. 10.1371/journal.pone.0207818 [DOI] [PMC free article] [PubMed]
- 6.Tong VT, Dietz PM, Morrow B et al. Trends in Smoking Before, During, and After Pregnancy — Pregnancy Risk Assessment Monitoring System, United States, 40 Sites, 2000–2010. Morbidity and Mortality Weekly Report. Published online November 8, 2013. Accessed December 19, 2023. https://www.cdc.gov/mmwr/preview/mmwrhtml/ss6206a1.htm [PubMed]
- 7.Jacobson LT, Dong F, Scheuermann TS, Redmond ML, Collins TC. Smoking behaviors among urban and rural pregnant women enrolled in the Kansas WIC Program. J Community Health. 2015;40(5):1037–46. 10.1007/s10900-015-0029-x. [DOI] [PubMed] [Google Scholar]
- 8.Pilehvari A, You W, Krukowski RA, Little MA. Examining smoking prevalence disparities in Virginia counties by Rurality, Appalachian Status, and Social Vulnerability, 2011–2019. Am J Public Health. 2023;113(7):811–4. 10.2105/AJPH.2023.307298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Campbell K, Fergie L, Coleman-Haynes T, et al. Improving behavioral support for Smoking Cessation in pregnancy: what are the barriers to stopping and which Behavior Change techniques can influence them? Application of theoretical domains Framework. IJERPH. 2018;15(2):359. 10.3390/ijerph15020359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Buettner-Schmidt K, Miller DR, Maack B. Disparities in rural Tobacco Use, smoke-free policies, and Tobacco taxes. West J Nurs Res. 2019;41(8):1184–202. 10.1177/0193945919828061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.CDCTobaccoFree. 2020 SGR: Smoking Cessation. Centers for Disease Control and Prevention. Published June 7, 2022. Accessed December 19, 2023. https://www.cdc.gov/tobacco/sgr/2020-smoking-cessation/index.html
- 12.Yost K, Perkins C, Cohen R, Morris C, Wright W. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control. 2001;12(8):703–11. 10.1023/A:1011240019516. [DOI] [PubMed] [Google Scholar]
- 13.Shulman HB, D’Angelo DV, Harrison L, Smith RA, Warner L. The pregnancy risk Assessment Monitoring System (PRAMS): overview of design and methodology. Am J Public Health. 2018;108(10):1305–13. 10.2105/AJPH.2018.304563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.USDA Economic Research Service. Rural-Urban Continuum Codes. Published December 20. 2020. Accessed December 19, 2023. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx
- 15.Appalachian Counties Served by ARC. Appalachian Regional Commission. Accessed December 19. 2023. https://www.arc.gov/appalachian-counties-served-by-arc/
- 16.StataCorp. Stata Statistical Software: Release 18. College Station. TX: StataCorp LLC; 2023. Published online 2023. [Google Scholar]
- 17.Hiscock R, Bauld L, Amos A, Fidler JA, Munafò M. Socioeconomic status and smoking: a review. Ann N Y Acad Sci. 2012;1248(1):107–23. 10.1111/j.1749-6632.2011.06202.x. [DOI] [PubMed] [Google Scholar]
- 18.Cnattingius S. The epidemiology of smoking during pregnancy: smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tob Res. 2004;6:125–40. 10.1080/14622200410001669187. [DOI] [PubMed] [Google Scholar]
- 19.Kondracki AJ. Prevalence and patterns of cigarette smoking before and during early and late pregnancy according to maternal characteristics: the first national data based on the 2003 birth certificate revision, United States, 2016. Reproductive Health. 2019;16:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pilehvari A, Krukowski RA, You W et al. Unveiling rural and Appalachian disparities in cigarette smoking through the social vulnerability index and other county-level characteristics. The Journal of Rural Health. n/a(n/a). 10.1111/jrh.12860 [DOI] [PMC free article] [PubMed]
- 21.Coleman T, Chamberlain C, Cooper S, Leonardi-Bee J. Efficacy and safety of nicotine replacement therapy for smoking cessation in pregnancy: systematic review and meta-analysis. In: Database of Abstracts of Reviews of Effects (DARE): Quality-Assessed Reviews [Internet]. Centre for Reviews and Dissemination (UK); 2011. Accessed June 29, 2024. https://www.ncbi.nlm.nih.gov/books/NBK80857/ [DOI] [PubMed]
- 22.Lumley J, Chamberlain C, Dowswell T, Oliver S, Oakley L, Watson L. Interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst Rev. 2009;3CD001055. 10.1002/14651858.CD001055.pub3. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.