Abstract
The Denver shunt is used for persistent chylothorax as a pleuroperitoneal shunt. Insertion of a Denver shunt was attempted in the current case involving a 3-year-old male with a refractory right cervical mediastinal lymphangioma. He was medicated with Eppikajutsuto® (0.65 g/kg) and underwent a Denver shunt for volume reduction of the cervical cyst to prevent airway obstruction. However, revision surgery for hemorrhage in the lymphangioma revealed that the tip of the shunt catheter had penetrated the cyst wall. The rounded tip of the catheter was placed back into the cyst. Oral administration of sirolimus (1 mg) was added. The Denver shunt was removed due to a catheter infection and administration of sirolimus was temporarily stopped because of an elevated blood concentration. Six months postoperatively from the third operation, neck swelling was negligible and radiologic findings showed complete regression of the lymphangioma.
Keywords: cervical mediastinal, lymphangioma, Eppikajutsuto, sirolimus, Denver shunt
Introduction
Peritoneovenous shunt placement is performed as a long-term treatment for chronic refractory ascites. The Denver shunt, which is comprised of two silastic tubes connected by a compressible pump, is most commonly used. The Denver shunt is also used for persistent chylothorax as a pleuroperitoneal shunt. Pleuroperitoneal shunting for chylothorax was first reported by Azizkhan et al. [1] for newborns with persistent chylothorax. The pleuroperitoneal catheter was cleared by pressure on the shunt bulb, which was continued at home several times daily. In the current case a Denver shunt was inserted from the right cervical region to the abdominal cavity for volume reduction of a cervical cyst to prevent airway obstruction for a refractory right cervical mediastinal lymphangioma.
Case report
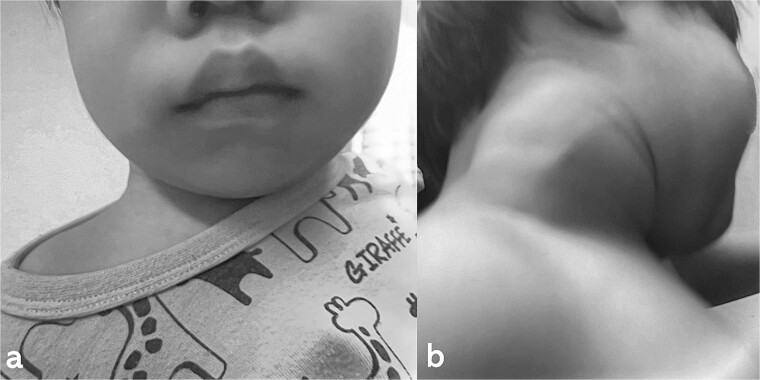
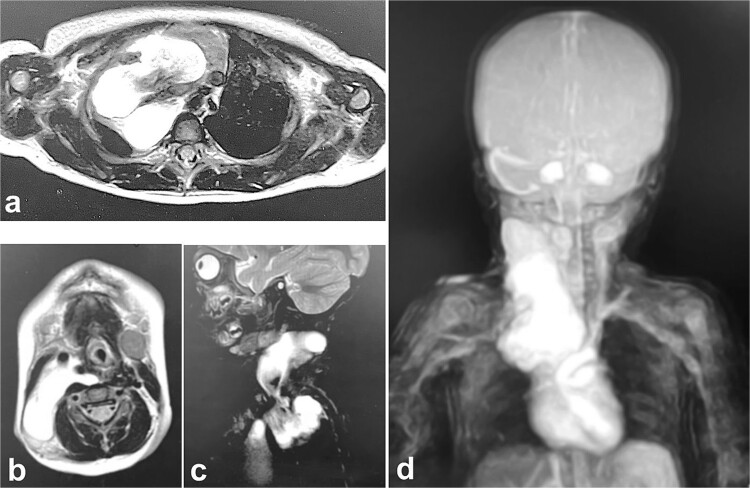
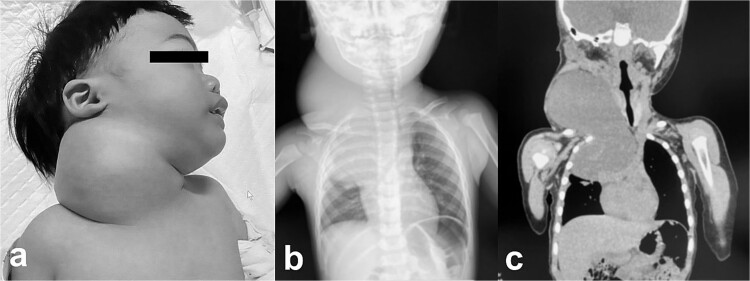
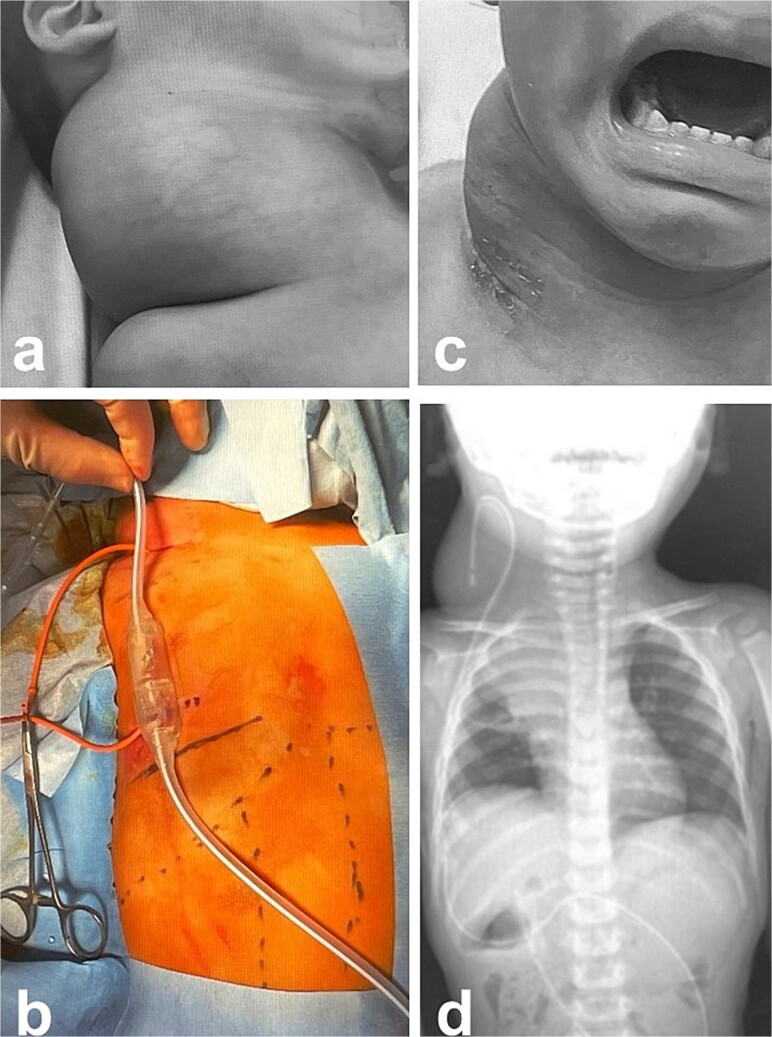
A male infant weighing 2726 g was born at 38 weeks of gestation. Antepartum ultrasonography and magnetic resonance imaging (MRI) revealed a right cervical cyst, suggestive of a lymphangioma. A right cervical cyst was noted at birth and gradually decreased in size thereafter. However, right cervical swelling became evident when he cried (Fig. 1a and b). An MRI obtained at 21 months of age showed a huge cyst in the right cervical mediastinal region. Following diagnosis of a lymphangioma with hemorrhage, he was treated with Eppikajutsuto®, a Japanese traditional Kampo medication, 2 g/d (0.2 g/kg). An MRI revealed tumor enlargement after oral administration of Eppikajutsuto® for 2 months. A complex vascular malformation was noted (Fig. 2) and the dose was increased to 5 g/day (0.5 g/kg). A repeat MRI 2 months after the dose increase showed no reduction in the size of the tumor. After another 4 months, the dose of Eppikajutsuto® was further increased to 7.5 g/d (0.65 g/kg). The tumor in the cervical region had enlarged further with an accompanying risk of airway system compression (Fig. 3a–c). A puncture and suction of the lymphangioma was performed for volume reduction and the content was prepared for bacterial culture. The content was dark red in color, which was consistent with hemorrhage. The white blood cell count (WBC) was 19 190/μl and the C-reactive protein (CRP) concentration was 5.77 mg/dl. He was admitted to the hospital to undergo treatment with intravenous and oral antibiotics. The bacterial culture results were negative. On the 22nd day of hospitalization, the WBC count was 8780/μl and the CRP concentration was 0.39 mg/dl. On the 24th day of hospitalization, a Denver shunt was inserted from the right cervical region to the abdominal cavity to reduce the volume of the cervical cyst to prevent airway obstruction (Fig. 4a–c). A pump chamber with a backflow prevention valve was implanted in the right anterior chest subcutaneous tissue (Fig. 4b). By applying pressure to the chamber, the cyst fluid in the neck was returned to the abdominal cavity. The patient was discharged on the 6th post-operative day. The swelling in the right neck was reduced and the pressure on the trachea was relieved based on the X-ray findings (Fig. 4c and d). On the 5th day after hospital discharge, the patient was febrile and the right neck swelling recurred. A hemogram revealed severe anemia and bleeding within the neck cyst was suspected. He was readmitted to the hospital and on the 2nd day after admission the cervical cyst was punctured, which yielded bloody contents. A transfusion was performed for anemia secondary to hemorrhage in the neck cyst. Sirolimus (1 mg), a mammalian target of rapamycin inhibitor, was added 7 months after starting Eppikajutsuto® due to a concern that administration of a Kampo medication and insertion of the Denver shunt might not be effective. An X-ray showed that the tip of the catheter may have moved within the cyst, which caused the catheter tip to penetrate the cyst and resulted in bleeding within the neck cyst (Fig. 5a). Serial MRI findings showed that the old bleeding site was within the mediastinal region of the lymphangioma. Revision surgery was performed 3 weeks after inserting the Denver shunt. Intraoperative findings showed that the tip of the catheter had penetrated the cyst wall (Fig. 5c). There were cyst walls with a septum on the mediastinal side of the cyst and when incised old bleeding was noted and the walls were opened as much as possible (Fig. 5d). The tip of the catheter was rounded and fixed with threads. The catheter was returned to the cyst and the wound was closed (Fig. 5b). The patient was discharged 9 days after the 2nd surgery. The concentration of sirolimus on the 14th day of administration was 9.9 ng/mL (normal range: 5–15 ng/ml). On the 16th day after the second hospital discharge, the neck had enlarged, the surgical wound was erythematous, and discharge was noted at the site of the pump chamber. Bacterial cultures of the punctured the neck cyst content and the wound discharge grew Staphylococcus aureus. On the 24th day after the 2nd hospital discharge, the blood concentration of sirolimus 1 month after starting oral administration was 19.7 ng/ml. Therefore, the oral administration of sirolimus was temporarily discontinued. At the same time the patient developed a high fever and the 3rd operation was performed to remove the Denver shunt due to a catheter infection. The blood concentration of sirolimus 6 days after discontinuation was 1.4 ng/ml. An MRI on the 6th post-operative day from the 3rd operation revealed two different intensities in the neck and mediastinal regions where the Denver shunt was inserted (Fig. 6a). On the 10th day after the 3rd operation, the patient was discharged from the hospital but laboratory testing showed an elevated WBC count (13 250/μl) and CRP concentration (6.03 mg/dl). Three months after the 3rd hospital discharge, the right neck swelling abruptly decreased in size and the WBC count and the CRP concentration decreased to the normal range. An MRI 2 months after the 3rd operation showed that the mediastinal lesion was smaller with near-complete regression (Fig. 6b). The neck swelling was minimal 6 months after the 3rd operation. An X-ray showed no tumor shadow and no compression of the trachea by the lymphangioma (Fig. 6c) and magnetic resonance angiography (MRA) showed that the lymphangioma had regressed (Fig. 6d). Currently, no right cervical swelling is evident when the patient cries (Fig. 6e and f) and he is doing well with oral administration of Eppikajutsuto® (7.5 g/d [0.65 g/kg]).
Figure 1.
Physiologic findings when crying. (a) smiling and (b) crying.
Figure 2.
MRI at evaluation after 2 months of Kampo medicine administration. A huge right cervical mediastinal lymphangioma is recognized. (a) Horizontal section in mediastinal region, (b) horizontal section in cervical region, (c) sagittal section in cervical mediastinal region, (d) MRA.
Figure 3.
Pathologic findings on the first administration. The tumor size in the cervical region was quite large and there may be a risk of airway system compression. (a) physical finding, (b) chest X-ray, (c) plain computed tomography.
Figure 4.
Intra- and post-operative findings from the first operation. (a) Intraoperative findings showed a huge bulge in the right neck. (b) A Denver shunt (peritoneovenous shunt) was inserted from the right cervical region to the abdominal cavity for volume reduction of the cervical cyst to prevent airway obstruction. Pump chamber with backflow prevention valve was implanted in the right anterior chest subcutaneous tissue. (c) Post-operative findings showed a reduction in the right neck swelling, even when crying. (d) The pressure on the trachea was shown to be relieved on the X-ray.
Figure 5.
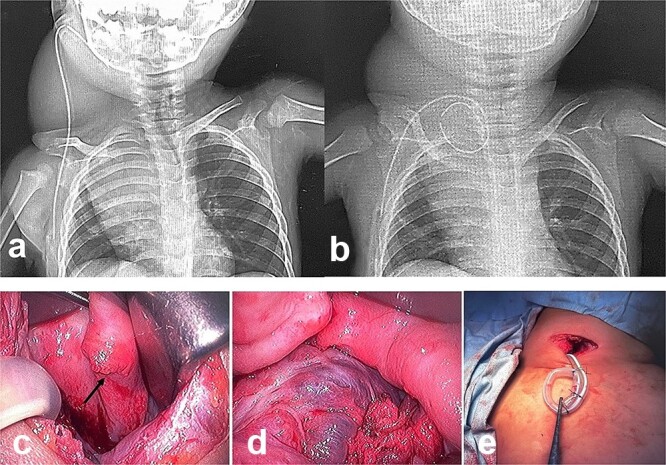
Intra- and post-operative findings from the second operation. (a) The X-ray showed that the tip of the catheter may have moved within the cyst, causing the catheter tip to penetrate the cyst. (b) The X-ray showed the rounded tip of the catheter fixed with threads. (c) Intraoperative findings showed that the tip of the catheter penetrated the cyst wall (black arrow). (d) There were cyst walls with a septum on the mediastinal side of the cyst and when incised old bleeding was noted. The walls were opened as much as possible. (e) The tip of the catheter was rounded and fixed with threads. The catheter was then placed back into the cyst and the wound was closed.
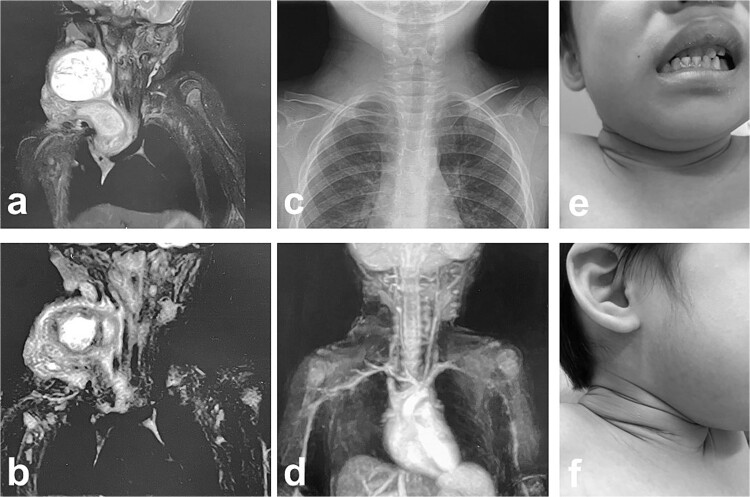
Figure 6.
MRI findings after removal of the Denver shunt catheter. (a) MRI findings showed two different areas of intensity in the neck region and the mediastinal region where the Denver shunt was inserted. (b) MRI findings 2 months postoperatively showed that the mediastinal lesion was smaller with near-complete regression. (c) X-ray showed no tumor shadow and no compression of the trachea by the lymphangioma. (d) MRA showed disappearance of the lymphangioma. (e) and (f) Right cervical swelling did not become evident, even when crying (e: crying, f: smiling).
Discussion
It is necessary to perform a tracheostomy in cases of infant cervical mediastinal lymphangioma given the risk of airway obstruction. Surgical treatment, sclerotherapy (e.g. OK-432), radiotherapy, and Eppikajutsuto® have been used in the treatment of lymphangiomas [2–7]. Ogawa-Ochiai et al. [4] reported the first case of a child with a lymphatic malformation treated with Eppikajutsuto® and Ogikenchuto. Recently, sirolimus has been reported to be effective in the treatment of lymphangiomas. Sirolimus is an immunosuppressive and antitumor agent that belongs to the mammalian target of rapamycin inhibitor group. Sirolimus inhibits abnormal vascular proliferation [8]. In the present case, the blood concentration of sirolimus 1 month after starting oral administration was highly elevated (19.7 ng/ml). At the same time, a Denver shunt catheter infection was recognized. The relationship between the infection and the high value of sirolimus has not been elucidated. The effectiveness of Eppikajutsuto® and sirolimus was not confirmed but the effectiveness of the Denver shunt was recognized, even temporarily. Family members, especially his mother, had to push the pump chamber frequently and it was difficult to push the pump chamber efficiently because the patient could not remain still.
The cause of the cervical mediastinal lymphangioma was an infection or bleeding in the cyst and there was a risk of suffocation by compressing the trachea. A tracheostomy may be temporarily performed, but in the case presented herein the Denver shunt was placed as a measure against a refractory cervical mediastinal lymphangioma and the pressure on the trachea was temporarily reduced. In the future, Denver shunt catheters should be utilized as an effective treatment while using medical treatment.
Contributor Information
Yukihiro Tatekawa, Department of Pediatric Surgery, Okinawa Prefectural Nanbu Medical Center & Children’s Medical Center, 118-1 Arakawa, Haebaru-cho, Shimajiri-gun, Okinawa 901-1193, Japan.
Yukihiro Tsuzuki, Department of Pediatric Surgery, Okinawa Prefectural Nanbu Medical Center & Children’s Medical Center, 118-1 Arakawa, Haebaru-cho, Shimajiri-gun, Okinawa 901-1193, Japan.
Yoshimitsu Fukuzato, Department of Pediatric Surgery, Okinawa Prefectural Nanbu Medical Center & Children’s Medical Center, 118-1 Arakawa, Haebaru-cho, Shimajiri-gun, Okinawa 901-1193, Japan.
Conflict of interest statement
None declared.
Funding
None declared.
References
- 1. Shimmyo T, Morita K, Mineshita M, et al. Pleuroperitoneal shunt for chylothorax and chylopericardium in lung cancer: a case report. Ann Thorac Cardiovasc Surg 2011;17:63–6. 10.5761/atcs.cr.09.01482. [DOI] [PubMed] [Google Scholar]
- 2. Nam SH, Kwon KA. Treatment of giant cervico-mediastinal lymphatic malformations: a case series. J Med Case Reports 2018;12:167. 10.1186/s13256-018-1705-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Prasad GR, Nori M, Naseeruddin MD, et al. Giant thoracocervical lymphangioma with multivisceral involvement: a different concept. International Journal of Phonosurgery and Laryngology 2014;4:63–6. 10.5005/jp-journals-10023-1085. [DOI] [Google Scholar]
- 4. Ogawa-Ochiai K, Sekiya N, Kasahara Y, et al. A case of mediastinal lymphangioma successfully treated with Kampo medicine. J Altern Complement Med 2011;17:563–5. 10.1089/acm.2010.0562. [DOI] [PubMed] [Google Scholar]
- 5. Hashizume N, Yagi M, Egami H, et al. Clinical efficacy of herbal medicine for pediatric lymphatic malformations: a pilot study. Pediatr Dermatol 2016;33:191–5. 10.1111/pde.12777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nakahata K, Ogawa-Ochiai K, Yamanaka H, et al. A large cervical lymphatic malformation in a neonate successfully treated with Kampo medicine A case report. Medicine Case Reports and Study Protocols 2021;2:e0030. 10.1097/MD9.0000000000000030. [DOI] [Google Scholar]
- 7. Tamura-Sugiyama T, Noguchi TH, Satake-Ozawa M, et al. A pediatric case of common lymphatic malformation in the floor of the mouth successfully treated with the Kampo medicine, Eppikajutsuto: a case report. Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology 2022;34:501–6. 10.1016/j.ajoms.2021.12.003. [DOI] [Google Scholar]
- 8. Amodeo I, Colnaghi M, Raffaeli G, et al. The use of sirolimus in the treatment of giant cystic lymphangioma. Medicine (Baltimore) 2017;96:e8871. 10.1097/MD.0000000000008871. [DOI] [PMC free article] [PubMed] [Google Scholar]