Abstract
Objective
To analytically depict the associated malformations of polysplenia syndrome (PS) in adults via computed tomography (CT).
Materials and methods
The incidence of malformations associated with PS in twelve adult patients was retrospectively analyzed via CT imaging.
Results
The number of splenic nodules ranged from three to twelve; the splenic nodules were located in the left upper quadrant in nine patients and in the right upper quadrant in three patients. A short pancreas was present in all twelve patients. Midgut malrotation was present in eight patients. Situs inversus totalis was present in two patients. Nine patients presented the absence of hepatic segmental inferior vena cava (IVC), with the hepatic vein directly converging into the right atrium and the continuation of the azygos vein. The preduodenal portal vein was present in six patients. Left lung heterotaxy was found in nine patients. The inferior vena cava was bilateral in one patient. Aberrant right subclavian arteries, bilateral common carotid arteries sharing trunks, abnormal renal vein branching and routing, and abdominal portal vein branching were also found in individual patients.
Conclusions
PS is a complex malformation syndrome involving multiple systems. The most common malformation is short pancreas, and other malformations, such as left lung heterogeneity, hepatic segmental IVC agenesis with continuation of the azygos vein, midgut malrotation, preduodenal portal vein, and left atrial heterotaxy, have relatively high prevalence rates.
Introduction
Polysplenia syndrome (PS), a rare syndrome of congenital anomalous spleen development with other multisystem malformations [1], is also known as left atrial isomerism syndrome (LAIS) because of the frequent occurrence of left atrial isomerism [2]. PS presenting in adults is very rare and has been reported mostly in case studies [3–5]. Compared with other examinations, thoracic and abdominal multilayer computed tomography (CT) is the best means to clarify the details of PS combined with various anatomical variants [6]; therefore, in this study, we retrospectively analyzed the CT imaging data of twelve adults with PS to summarize the concomitant deformities in adults with PS with the aim of improving the understanding of concomitant deformities of PS, avoiding misdiagnosis of anatomical variants as lesions and preventing unnecessary surgical injuries.
Materials and methods
Patients
This retrospective study was approved by the institutional review board (No. 2023177, The Affiliated Suzhou Hospital of Nanjing Medical University) with a waiver of written informed consent.
CT images of 12 PS patients from January 2015 to March 2024 were retrospectively collected. The data for this study were accessed from 10/10/2023 to10/10/2024. There were 5 men and 7 women, with an age range of 30–74 years. All 12 patients underwent plain CT examination of the chest and abdomen, and CT enhancement was performed for 6 patients.
Analysis methods
Two radiologists with 7 and 20 years of experience in diagnostic imaging observed and analyzed the CT images of each patient with PS, respectively, and the concomitant deformities of the PS were recorded.
Results
Medical history
A history of cholangiocarcinoma with cirrhosis, cholangiocarcinoma in the porta hepatis with cholecystitis, chronic inflammation of the bile ducts and duodenum, biliary stones, arrhythmia and right kidney stones, left kidney stones, polyps of the colon, and ventricular septal defect (VSD) were recorded in one patient each, and the other patients did not have any special medical history (Table 1).
Table 1. Clinical data of 12 patients with polysplenic syndrome.
| Case No. | Age (Year) | Sex | Medical history |
|---|---|---|---|
| 1 | 70 | F | Polyp of the colon |
| 2 | 38 | M | VSD |
| 3 | 53 | F | None |
| 4 | 38 | F | None |
| 5 | 74 | M | Cholangiocarcinoma, cirrhosis |
| 6 | 69 | F | Inflammation of the bile ducts and duodenum |
| 7 | 64 | F | Gallstones |
| 8 | 66 | M | Cholangiocarcinoma, Cholecystitis |
| 9 | 31 | M | Arrhythmia, right kidney stone |
| 10 | 30 | M | None |
| 11 | 57 | F | Left kidney stone |
| 12 | 65 | F | None |
VSD- ventricular septal defect
CT imaging findings
The concomitant deformities of the PS of 12 patients shown on CT are summarized in Table 2.
Table 2. The malformations of 12 patients with polysplenic syndrome on CT.
| Malformations | Percentage of Occurrence | Case1 | Case2 | Case3 | Case4 | Case5 | Case6 | Case7 | Case8 | Case9 | Case10 | Case11 | Case 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Left lung heterogeneity | 75% | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | No | Yes | Yes |
| Left atrial heterotaxy | 42% | Yes | Yes | No | No | Yes | No | Yes | Yes | No | No | No | No |
| Location of spleen | Left | Left | Right | Left | Left | Left | Left | Left | Left | Left | Right | Right | |
| Number of spleens | 5 | 12 | 4 | 7 | 4 | 3 | 11 | 5 | 12 | 5 | 8 | 5 | |
| Liver: small left lobe | 8% | Yes | No | No | No | No | No | No | No | No | No | No | No |
| Left liver | 17% | No | No | Yes | No | No | No | No | No | No | No | No | Yes |
| Horizontal liver | No | No | No | No | No | No | Yes | Yes | No | No | Yes | No | |
| Location of gallbladder | Right | Right | Left | Right | Right | Right | Right | Median | Right | Right | Right | Left | |
| Short pancreas | 100% | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Midgut malrotation | 67% | Yes | Yes | Yes | No | Yes | No | Yes | Yes | Yes | No | Yes | No |
| Hepatic segmental IVC agenesis with continuation of AZ | 75% | Yes | No | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes |
| Bilateral IVC | 8% | No | No | Yes | No | No | No | No | No | No | No | No | No |
| PDPV | 42% | No | Yes | No | Yes | Yes | No | No | No | Yes | Yes | Yes | No |
| Double LRV | 8% | Yes | No | No | No | No | No | No | No | No | No | No | No |
| Double RRV | 8% | No | No | Yes | No | No | No | No | No | No | No | No | No |
| Bilateral RV inflow AZ | 8% | No | No | No | No | No | No | No | Yes | No | No | No | No |
| LRV travels behind AA, and bilateral RV flow into AZ | 8% | No | No | No | No | No | No | No | No | Yes | No | No | No |
| RRV flows into AZ, LRV flows into HAZ | 17% | No | No | No | No | No | No | No | No | No | No | Yes | Yes |
| Bilateral CCA shared trunks | 17% | Yes | No | No | No | No | No | No | Yes | No | No | No | No |
| ARSA | 17% | Yes | No | No | No | No | No | No | Yes | No | No | No | No |
| RAA | 17% | No | No | Yes | No | No | No | No | Yes | No | No | No | No |
| DPT | 17% | No | No | Yes | No | No | No | No | Yes | No | No | No | No |
| Dextrocardia | 17% | No | No | Yes | No | No | No | No | Yes | No | No | No | No |
| SIT | 17% | No | No | Yes | No | No | No | No | No | No | No | No | Yes |
| The anterior branch of the portal vein enters the liver from the anterior edge of the liver | 8% | Yes | No | No | No | No | No | No | No | No | No | No | No |
IVC-inferior vena cava; AZ-azygos vein; PDPV-preduodenal portal vein; RV-renal vein; LRV-left renal vein; RRV- right renal vein; AA-abdominal aorta; SVC-superior vena cava; HAZ-hemiazygos vein; ARSA- aberrant right subclavian artery; CCA-common carotid artery; SIT-Situs inversus totalis; RAA-right aortic arch; DPT-dextral pulmonary trunk
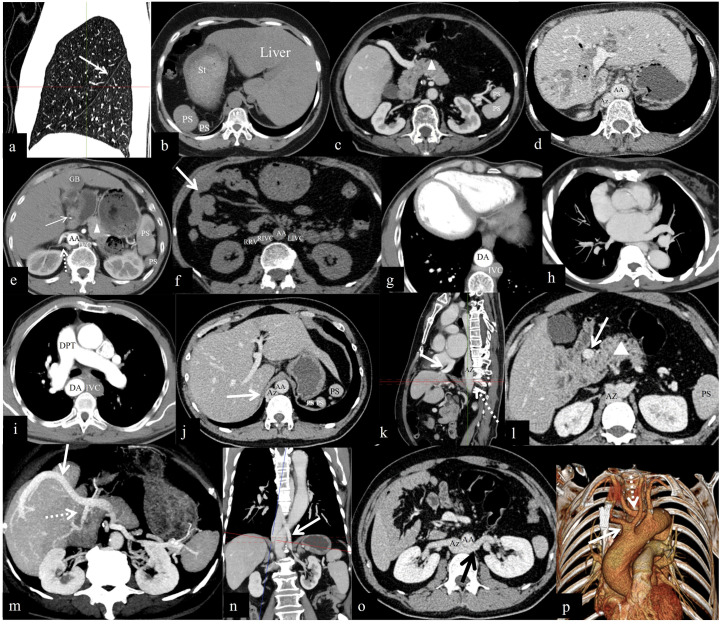
Respiratory system: Nine patients (75%, 9/12) presented with left lung heterogeneity (i.e., both the lungs and bilateral bronchi presented with left-sided morphology) (Fig 1a).
Fig 1.
(a) Left lung heterogeneity: Sagittal image of the right lung showing only the major oblique fissure (arrow). (b) Visceral inversion: the liver is located on the left side, the stomach (St) is on the right side, and multiple splenic nodules (PSs) are present in the right upper quadrant. (c) A short pancreas (Δ). (d) Horizontal liver. (e) Hepatic hilar cholangiocarcinoma (arrow) and median gallbladder (GB). (f) Malrotation of the midgut (arrow). (g) Dextrocardia. (h) Left atrial heterotaxy. (i) Dextral pulmonary trunk (DPT); the IVC is on the left, and the descending aorta (DA) is on the right. (j) The thickening AZ (arrow) and absence of the IVC of the hepatic segment. (k) The hepatic segment of the IVC is absent, and the left, middle, and right hepatic veins converge and are injected directly into the right atrium (arrow); a thickened AZ (dotted arrow). (l) Preduodenal portal vein (PDPV) (arrow). (m) The portal vein travels anteriorly to the head of the pancreas and then bifurcates into two branches, with the thicker branch traveling along the anterior edge of the liver to the diaphragmatic surface of the liver to enter the liver (solid arrow) and the thinner branch entering the liver in the first hepatic hilar (dotted arrow). (n) Left renal veins converging directly into the azygos vein (arrow). (o) The left renal vein crosses the abdominal aorta (AA) posteriorly to join the Az (arrow), and the right renal vein joins directly to the Az; malrotation of the midgut. (p) Bilateral common carotid artery shared trunks (arrow). Aberrant right subclavian artery (dotted arrow).
Spleen: The number of splenic nodules ranged from three to twelve, with sizes ranging from 3×4×6 mm to 18×30×88 mm (Fig 1b). Polysplenia nodules were located in the left upper quadrant in nine patients (75%, 9/12) and in the right upper quadrant (25%, 3/12) in three patients (Fig 1b). Splenic nodules were distributed along the external and posterior parts of the greater curvature of the stomach (Fig 1b).
Pancreas: A short pancreas was observed in all twelve patients (100%, 12/12) (the head and uncinate process of the pancreas were enlarged, and the body and tail of the pancreas were short or absent) (Fig 1c).
Hepatobiliary system: Six patients exhibited normal anatomy (50%, 6/12). The liver and gallbladder were found in the left upper quadrant in two patients (17%, 2/12). A small left lobe of the liver was detected in one patient (8%, 1/12), a horizontal liver with a right gallbladder was detected in two patients (17%, 2/12) (Fig 1d), and a horizontal liver and median gallbladder were detected in one patient (8%, 1/12) (Fig 1e).
Gastrointestinal tract: The stomach was located on the right side (Fig 1c) in three patients (25%, 3/12), and midgut malrotation was found in eight patients (67%, 8/12) (Fig 1f).
Heart: Dextrocardia was found in two patients (17%, 2/12) (Fig 1g).
Atrium: CT suggested possible left atrial heterotaxy in five patients (42%, 5/12) (Fig 1h).
Aortic arch: A right aortic arch (RAA) and dextral pulmonary trunk were observed in two patients (17%, 2/12) (Fig 1i).
Superior vena cava (SVC): A persistent left superior vena cava (PLSVC) was found in one patient (8%, 1/12).
Inferior vena cava (IVC): The absence of the hepatic segment of the IVC (Fig 1j and 1k), which continued upward as a thickened azygos vein was found in nine patients (75%, 9/12) (Fig 1k), and a bilateral IVC was found in one patient (8%, 1/12) (Fig 1f).
Portal vein: The preduodenal portal vein (PDPV) was present in six patients (50%, 6/12) (Fig 1l). In one patient (8%, 1/12), the portal vein traveled in front of the head of the pancreas and then bifurcated into two branches; the thicker branch traveled along the anterior border of the liver to the diaphragmatic surface of the liver into the liver, and the thinner branch entered the liver in the first hepatic portal (Fig 1m).
Hepatic vein: In nine patients (75%, 9/12), the hepatic vein exited the second porta hepatis and converged directly into the right atrium (Fig 1k).
Renal veins: Two patients (17%, 2/12) had unilateral renal veins with double-branched variants: one patient had both renal veins converging directly into the azygos vein (Fig 1n), one patient had the left renal vein traveling posterior to the abdominal aorta (Fig 1o), and one patient had the right renal vein flowing back into the azygos vein and injecting upward into the SVC. In two patients (17%, 2/12), the left renal vein first converged into the hemiazygos vein and then into the azygos vein in the posterior mediastinum.
Common carotid artery (CCA): Bilateral CCAs shared trunks in two patients (17%, 2/12) (Fig 1p).
Others: An aberrant right subclavian artery (ARSA) was found in two patients (17%, 2/12) (Fig 1p).
Discussion
Pathogenesis and survival rates
PS was first reported by Baillie in 1788 [7], but the exact cause of PS is still unclear, and studies have shown that its occurrence is closely related to embryonic development, inheritance, teratogenic factors, genetic mutations and other factors [6]. The 5th–7th week of embryo development is a critical stage for the development and rotation of the spleen, atrial septum, trunk of the conus artery and atrioventricular valve, as well as the process of the gastrointestinal tract returning to the abdominal cavity from the umbilical cord for rotation. Cardiovascular and visceral anomalies occur when this process is impaired. Situs solitus describes the normal anatomic position of organs or structures. Situs inversus refers to a left–right inversion, resulting in the mirror image of situs solitus. Situs ambiguous, a synonym for left or right isomerism, characterizes the positions of organs or structures lateralizing across the left–right axis and cannot be categorized as situs solitus or inversus. Any type of situs other than situs solitus can be described as heterotaxy [8].
PS is very rare, with an infantile morbidity rate of only 1/250000, and the degree of congenital heart disease malformation affects the survival of patients with PS. The mortality rate in the first year is 50–60%; 25% of patients with PS survive to the age of 5 years, and only 10% have normal hearts or only minor heart defects and therefore survive to adulthood [9–11]. Some studies have reported [4, 9] that the prevalence of PS is greater in females than in males, and our findings are consistent with the literature.
CT findings
Multiple spleens
The number of spleens reported in the literature is between two and sixteen [10], with different sizes, no main spleen, no increase in the total weight of the spleen, and no hypersplenism, and the spleen can be located in the left upper quadrant, right upper quadrant, or both sides of the abdomen, with the left upper quadrant being the most common. The spleen is usually located on the side of the greater curvature of the stomach and shows "Zebra pattern" enhancement in the arterial phase and uniform enhancement in the venous and delayed phases. The degree of enhancement is consistent with that of a normal spleen [6, 11].
The number of spleens in this group ranged from three to twelve, twelve of which were located next to the greater curvature of the stomach and, three of which were located in the right upper quadrant. Six patients who completed the CT enhancement examination had an arterial "Zebra pattern" and uniform venous enhancement, twelve patients had no main spleen, and the size of the splenic nodules varied, which was consistent with previous reports.
Visceral abnormalities
In our group, all twelve patients had short pancreas, including two patients with pancreatic inversion, which was the most prevalent extrasplenic abnormality. Some studies [12–15] have reported that pancreatic abnormalities are associated with PS. The pancreas is formed by the fusion of ventral and dorsal pancreatic buds; the ventral pancreatic buds give rise to the uncinate process and head, and the dorsal pancreatic buds give rise to the body and tail [14]. When the pancreas is dorsally underdeveloped, dysplasia of the body and tail of the pancreas, occurs which mostly manifests as a short pancreas [14].
In this group, one patient had a small left lobe of the liver accompanied by a right gallbladder, two patients had total visceral inversion manifesting as a left liver and gallbladder, two patients had a horizontal liver with a right gallbladder, and one patient had a horizontal liver with a median gallbladder. Some previous studies have also reported these hepatobiliary anomalies [4, 12].
In our group, there were eight cases of midgut malrotation (8/12, 67%), including two cases of gastrointestinal anteversion (total visceral anteversion), which is consistent with the published literature showing small bowel malrotation in 60.4% of PS patients [4, 16].
In our group, we found kidney stones in two of our twelve patients, and no other genitourinary anomalies, such as a double ureter or renal hypoplasia [17, 18], were observed.
Vascular malformations
In our group, hepatic segmental IVC agenesis with continuation of azygos was found in nine patients. When the hepatic segment of the IVC fails to anastomose with the suprarenal segment during embryonic development, the renal segment and lower segment flow back into the SVC via the azygos or hemiazygos vein [6], which is considered the most common vascular malformation in PS [9, 19, 20].
In our group, PDPV was present in six patients. PDPV [21, 22] is a rare congenital anomaly, especially in adults, in which the portal vein passes through the anterior part of the duodenum rather than the posterior part and leaves an abnormal vein in the anterior part of the duodenum due to an anomaly of rotation during intestinal rotation or an anomaly of closure of the vitelline vein (umbilical vein), which results in the formation of a portal vein. In patients who require surgery, failure to detect the presence of PDPV before surgery may lead to serious complications such as intraoperative bleeding. In addition, it has been reported [23] that PDPV may compress the duodenum and biliary tract, causing intestinal obstruction and biliary obstruction.
Renal vein anomalies mainly manifest as the retro-aortic renal vein and the right renal vein flowing back into the azygos vein to inject upward into the SVC, and the left renal vein converges into the hemiazygos vein, which converges into the azygos vein in the posterior mediastinum [4]. Among them, the retro-aortic renal vein usually occurs unilaterally on the left side, which can lead to hematuria, left-sided pain, and a variety of other symptoms, often suggesting posterior nutcracker syndrome [24], which is relatively rare and is consistent with the presentation in one patient in our group.
Other vascular malformations, including ARSA and bilateral CCA shared trunks [4], were found in our group, with the exception of vertebral artery origin anomalies. In our study, two special manifestations were observed that were not reported in the previous PS-related literatures: bilateral IVC and portal vein abnormalities bifurcated into two branches with the thicker branch traveling along the anterior border of the liver to the diaphragmatic surface of the liver to enter the liver and the thinner branch entering the liver at the first hepatic hilar.
Lung anomalies
Nine patients in our group exhibited left lung heterogeneity, with a higher incidence than that reported in previous studies, which reported an incidence of 55% [10]. A previous study [6] also revealed that the incidence of bilateral lung heterogeneity on the left side was much lower in adults with PS, which suggested that since adults with PS usually do not have cardiac anomalies such as abnormal pulmonary venous return or atrial septal defect (ASD), they do not experience bilateral left-sided changes. In our group, there were only two patients with cardiac abnormalities, which is not consistent with previous reports in the literature [6, 10]. The reason for this may be that left lung heterogeneity is related not only to cardiac abnormalities but also to other factors that need further confirmation.
Cardiac abnormalities
In this group, five CT scans suggested the possibility of left atrial heterotaxy, one had a history of VSD, and cardiac ultrasound suggested a tumor in the membranous portion of the interventricular septum. PS in adults is usually not associated with cardiac developmental abnormalities or only with mild cardiac abnormalities [3]. These abnormalities mainly include positional abnormalities of the heart, such as dextrocardia [9]; structural abnormalities, such as ASD, VSD, right ventricular double outlet, atrial septal hypertrophy, and lipoma [11]; and arrhythmias, such as atrioventricular block and bradycardia [25], some of which are difficult to diagnose via CT and usually rely on cardiac ultrasound and electrocardiogram.
Comorbid tumors
In our group, there were two patients with cholangiocellular carcinoma, which was also reported previously [26], and the cause is hypothesized to be related to biliary obstruction due to developmental malformations of the biliopancreatic duct and recurrent infections of the biliary system in patients with PS. Previous case reports [15, 26–28] have shown that PS can co-occur with malignant tumors, such as hepatocellular carcinoma, intrahepatic cholangiocarcinoma, gastric carcinoma, rectal carcinoma, and breast cancer. However, there is no evidence that PS is a precancerous syndrome or that there is a greater incidence of tumors than in the normal population.
Differential diagnosis
PS needs to be differentiated from asplenia syndrome (AS), accessory spleen, simple visceral inversion, enlarged lymph nodes in the abdominal cavity, and other nodular masses in the abdominal cavity [7, 9, 29]. (1) AS can present as congenital splenic hypoplasia or absence of the spleen, with trilobarism of both lungs (right-sided heterotaxy of both lungs), a median liver, and more frequent and more severe cardiovascular malformation than PS, and the IVC is located on the same side of the spine as the aorta. (2) Accessory spleen: There is a large primary spleen, with a large difference in volume between the primary and secondary spleens, whereas there is no primary spleen in PS. (3) Simple inversion of the viscera: partial or total inversion of the viscera, resembling the mirror image of a normal person, is not associated with cardiovascular or visceral developmental malformations. (4) Enlarged lymph nodes in the abdominal cavity and other nodular masses in the abdominal cavity: There is a history of inflammation or malignant tumors, often multiple, located in the abdominal cavity and retroperitoneum, without a splenic hilar incision or splenic hilar vessels, and homogeneous enhancement in all three phases is observed.
Conclusions
PS is a complex malformation syndrome involving multiple systems. The most common malformation is a short pancreas, and other malformations, such as left lung heterogeneity, hepatic segmental IVC agenesis with continuation of the azygos vein, midgut malrotation, preduodenal portal vein, and left atrial heterotaxy, have relatively high prevalence.
Being familiar with the occurrence of malformations associated with PS is conducive to avoiding misdiagnosis and mistreatment. Because the malformations involve multiple systems, multidisciplinary consultation is more conducive to the evaluation of this disease.
Data Availability
All relevant data are within the manuscript.
Funding Statement
The funding for the research has been provided by " Suzhou key diseases project (LCZX202212), Suzhou Science and Technology Bureau Project (SKY2023064, SKYD2023255)" and the funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Abdullah RA, Alharbi MA, Alnutaifi FM, Faqih AI, Alduraibi KM, Alharbi AS. Polysplenia Syndrome Complicated by Splenic Infarction: A Report of a Rare Case. Cureus. 2023;15(5):e38589. Epub 2023/06/07. doi: 10.7759/cureus.38589 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frescura C, Ho SY, Giordano M, Thiene G. Isomerism of the atrial appendages: morphology and terminology. Cardiovasc Pathol. 2020;47:107205. Epub 20200116. doi: 10.1016/j.carpath.2020.107205 . [DOI] [PubMed] [Google Scholar]
- 3.Malki MC, Outznit M, Mechhor S, Bouibaouen B, Nkurunziza L, Bacha HE, et al. Polysplenia syndrome in adulthood: a case report. Pan Afr Med J. 2022;41:67. Epub 2022/04/05. doi: 10.11604/pamj.2022.41.67.29014 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rameshbabu CS, Gupta KK, Qasim M, Gupta OP. Heterotaxy Polysplenia Syndrome In An Adult With Unique Vascular Anomalies: Case Report With Review Of Literature. J Radiol Case Rep. 2015;9(7):22–37. Epub 2015/12/03. doi: 10.3941/jrcr.v9i7.2210 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mountassir ME, Borahma M, Benelbarhdadi I, Lagdali N, Hosni A, Ajana FZ. Polysplenia syndrome revealed in adulthood by pancreatic and vascular malformations: a case report. Pan Afr Med J. 2022;43:77. Epub 2023/01/03. doi: 10.11604/pamj.2022.43.77.31496 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tawfik AM, Batouty NM, Zaky MM, Eladalany MA, Elmokadem AH. Polysplenia syndrome: a review of the relationship with viscero-atrial situs and the spectrum of extra-cardiac anomalies. Surg Radiol Anat. 2013;35(8):647–53. Epub 2013/03/20. doi: 10.1007/s00276-013-1100-x . [DOI] [PubMed] [Google Scholar]
- 7.Vaughan TJ, Hawkins IF Jr., Elliott LP. Diagnosis of polysplenia syndrome. Radiology. 1971;101(3):511–8. Epub 1971/12/01. doi: 10.1148/101.3.511 . [DOI] [PubMed] [Google Scholar]
- 8.Wolla CD, Hlavacek AM, Schoepf UJ, Bucher AM, Chowdhury S. Cardiovascular manifestations of heterotaxy and related situs abnormalities assessed with CT angiography. J Cardiovasc Comput Tomogr. 2013;7(6):408–16. Epub 2013/12/18. doi: 10.1016/j.jcct.2013.11.008 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gayer G, Apter S, Jonas T, Amitai M, Zissin R, Sella T, et al. Polysplenia syndrome detected in adulthood: report of eight cases and review of the literature. Abdom Imaging. 1999;24(2):178–84. doi: 10.1007/s002619900471 . [DOI] [PubMed] [Google Scholar]
- 10.Peoples WM, Moller JH, Edwards JE. Polysplenia: a review of 146 cases. Pediatr Cardiol. 1983;4(2):129–37. doi: 10.1007/BF02076338 . [DOI] [PubMed] [Google Scholar]
- 11.Low JP, Williams D, Chaganti JR. Polysplenia syndrome with agenesis of the dorsal pancreas and preduodenal portal vein presenting with obstructive jaundice—a case report and literature review. Br J Radiol. 2011;84(1007):e217–20. doi: 10.1259/bjr/27680217 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kayhan A, Lakadamyali H, Oommen J, Oto A. Polysplenia syndrome accompanied with situs inversus totalis and annular pancreas in an elderly patient. Clin Imaging. 2010;34(6):472–5. Epub 2010/11/26. doi: 10.1016/j.clinimag.2009.11.011 . [DOI] [PubMed] [Google Scholar]
- 13.Kobayashi H, Kawamoto S, Tamaki T, Konishi J, Togashi K. Polysplenia associated with semiannular pancreas. Eur Radiol. 2001;11(9):1639–41. Epub 2001/08/21. doi: 10.1007/s003300000757 . [DOI] [PubMed] [Google Scholar]
- 14.Maier M, Wiesner W, Mengiardi B. Annular pancreas and agenesis of the dorsal pancreas in a patient with polysplenia syndrome. AJR Am J Roentgenol. 2007;188(2):W150–3. Epub 2007/01/24. doi: 10.2214/AJR.05.1859 . [DOI] [PubMed] [Google Scholar]
- 15.Ito H, Ohgi S, Kanno T, Ishibashi T. Heterotaxy syndrome with pancreatic malrotation: CT features. Abdom Imaging. 2003;28(6):856–8. doi: 10.1007/s00261-003-0034-x . [DOI] [PubMed] [Google Scholar]
- 16.Burton EC, Olson M, Rooper L. Defects in laterality with emphasis on heterotaxy syndromes with asplenia and polysplenia: an autopsy case series at a single institution. Pediatr Dev Pathol. 2014;17(4):250–64. Epub 20140415. doi: 10.2350/13-11-1406-OA.1 . [DOI] [PubMed] [Google Scholar]
- 17.Hadar H, Gadoth N, Herskovitz P, Heifetz M. Short pancreas in polysplenia syndrome. Acta Radiol. 1991;32(4):299–301. Epub 1991/07/01. . [PubMed] [Google Scholar]
- 18.Herman TE, Siegel MJ. Polysplenia syndrome with congenital short pancreas. AJR Am J Roentgenol. 1991;156(4):799–800. Epub 1991/04/01. doi: 10.2214/ajr.156.4.2003448 . [DOI] [PubMed] [Google Scholar]
- 19.Fulcher AS, Turner MA. Abdominal manifestations of situs anomalies in adults. Radiographics. 2002;22(6):1439–56. doi: 10.1148/rg.226025016 . [DOI] [PubMed] [Google Scholar]
- 20.Li ZG, Lin ZC, Mu HY. Polysplenia Syndrome With Splenic and Skeletal Muscle Metastases From Thyroid Carcinoma Evaluated by FDG PET/CT: Case Report and Literature Review: A Care-Compliant Article. Medicine (Baltimore). 2016;95(4):e2532. doi: 10.1097/MD.0000000000002532 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.G AL, Kagali NA, M S, Prasad BS. Preduodenal portal vein in adult with polysplenia syndrome revisited with a case report. Indian J Surg. 2014;76(2):137–42. Epub 2014/06/04. doi: 10.1007/s12262-013-0812-9 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seo HI, Jeon TY, Sim MS, Kim S. Polysplenia syndrome with preduodenal portal vein detected in adults. World J Gastroenterol. 2008;14(41):6418–20. doi: 10.3748/wjg.14.6418 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Salma EH, Najwa A, Mehdi T, Nazik A, Latifa C, Siham EH. Polysplenia Syndrome With Persistent Left Superior Vena Cava: Case Report and Review of the Literature. Glob Pediatr Health. 2022;9:2333794X221127640. Epub 20220927. doi: 10.1177/2333794X221127640 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lai B, Zhong J, Zhong J. Polysplenia syndrome complicated with posterior nutcracker syndrome. Asian J Surg. 2023;46(12):5460–1. Epub 2023/08/05. doi: 10.1016/j.asjsur.2023.07.115 . [DOI] [PubMed] [Google Scholar]
- 25.Montero-Macias R, Krief D, Villefranque V, Kilani M, Castillo-Tunon JM. Anatomy, embryology, and imaging of situs ambiguous with polysplenia and left IVC. Radiol Case Rep. 2023;18(5):1727–32. Epub 20230227. doi: 10.1016/j.radcr.2023.02.005 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yorita K, Sasaki S, Kawada A, Okazaki M, Yamai H, Uchita K, et al. Hepatoid Adenocarcinoma of the Extrahepatic Bile Duct in a Patient with Polysplenia Syndrome. Intern Med. 2017;56(4):401–7. Epub 2017/02/17. doi: 10.2169/internalmedicine.56.7526 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mimatsu K, Oida T, Kano H, Kawasaki A, Fukino N, Kida K, et al. Preduodenal portal vein, intestinal malrotation, polysplenia, and interruption of the inferior vena cava: a review of anatomical anomalies associated with gastric cancer. Surg Radiol Anat. 2012;34(2):179–86. Epub 20111112. doi: 10.1007/s00276-011-0894-7 . [DOI] [PubMed] [Google Scholar]
- 28.Iwamura T, Shibata N, Haraguchi Y, Hisashi Y, Nishikawa T, Yamada H, et al. Synchronous double cancer of the stomach and rectum with situs inversus totalis and polysplenia syndrome. J Clin Gastroenterol. 2001;33(2):148–53. Epub 2001/07/27. doi: 10.1097/00004836-200108000-00012 . [DOI] [PubMed] [Google Scholar]
- 29.Yoneyama H, Kondo C, Yamasaki A, Nakanishi T, Sakai S. Comparison of situs ambiguous patterns between heterotaxy syndromes with polysplenia and asplenia. Eur J Radiol. 2015;84(11):2301–6. Epub 2015/08/26. doi: 10.1016/j.ejrad.2015.08.004 . [DOI] [PubMed] [Google Scholar]