Abstract
Background:
Hernia repairs are one of the most common general surgery procedures and an essential part of training for general surgery residents. The widespread incorporation of robotic hernia repairs warrants the development of a procedure-specific robotic curriculum to assist novice surgeons in improving technical skills.
Objective:
To evaluate a robotic hernia simulation-based curriculum for general surgery residents using video review.
Methods:
Retrospective cohort study of PGY-3 general surgery residents from the University of Chicago from 2019 to 2021. The residents completed inguinal hernia repair (IHR) and ventral hernia repair (VHR) drills as part of a robotic simulation curriculum. The drills were recorded and graded according to the modified objective structured assessment of technical skills (OSATS) and time to completion. The drills were completed by 3 attending surgeons to establish gold-standard benchmarks.
Results:
In total, 20 residents started the curriculum, 19 completed all IHR drills and 17 completed all VHR drills. Attending surgeon total OSATS scores and time to completion were significantly better than the trainees on the first attempt (P < 0.05). When comparing 1st to 4th attempt, resident OSATS scores improved significantly for IHR (15.5 vs 23.3; P < 0.001) and VHR (16.8 vs 23.3; P < 0.001). Time also improved over 4 attempts (IHR: 28.5 vs 20.5 minutes; P < 0.001 and VHR: 29.6 vs 21.2 minutes; P < 0.001). Residents achieved attending-level OSATS scores by their fourth attempt for VHR, but not for IHR. Residents did not achieve attending-level times for either hernia drills.
Conclusions:
The robotic hernia curriculum improved resident performance on hernia repair drills and was well-received by the residents.
Keywords: surgical education, robotic hernia repair, robotic surgery curriculum, inguinal hernia repair, ventral hernia repair
INTRODUCTION
In 2019, inguinal hernia repair was among the top 5 most common major ambulatory surgeries performed on males over the age of 18.1 While the majority of hernia operations are still performed with an open approach, minimally invasive techniques have become increasingly popular.2 According to the analysis of the American College of Surgeons National Surgical Quality Improvement Program database, between 2006 and 2017, the rate of minimally invasive inguinal and ventral hernia repairs (VHR) increased from 20.3% to 37.2%.3 Since the first robotic inguinal hernia repair (IHR) was performed by a general surgeon in 2015, the robot has been increasingly used to perform both IHR and VHR.4–6
Improved outcomes seen with a minimally invasive approach to hernia repair have driven surgeons to further explore the use of the robot.7,8 Robotic hernia repairs have been shown to have less postoperative pain and fewer complications compared with an open approach.9 Additionally, the robotic approach has been associated with improved short-term quality of life compared to both open and laparoscopic repairs for incisional hernias.10 Despite these improved outcomes and the advancements in technical innovation the robotic platform provides, concerns regarding cost and patient safety remain.5,11
As more surgeons transition to the robotic platform for hernia repairs and work through the learning curve, patient safety is a top concern.12 Several studies have demonstrated the successful and safe transition from laparoscopic to robotic hernia repair.13–16 Furthermore, the learning curve for a robotic IHR ranges from 11 to 35 cases, an easily attainable benchmark for most general surgeons.17–19 In the largest case series of over 300 robotic IHRs performed across 7 hospitals by 18 surgeons, the learning curve was as low as 11 to 12 cases.17 For robotic VHR, the learning curve is slightly longer, 38 to 55 cases.20–22 Despite attainable learning curves, proficiency-based training curricula afford surgeons the opportunity to obtain the necessary skills in a simulated environment.23,24
Among attending surgeons incorporating robotic IHR into their practice, completion of a proficiency-based robotic curriculum, including procedure-specific hernia drills, has been shown to decrease operative time and hospital costs compared with surgeons who did not complete a training program.25 Therefore, it stands to reason that offering a similar simulation-based curriculum to surgical trainees would provide a strong foundation and allow them to be more proficient in the operating room. Because hernia repairs are one of the most logged procedures among general surgery residents and given the widespread adoption of the robotic technique for hernia surgery, we incorporated IHR and VHR modules into our robotic skills curriculum.26,27 This study aims to evaluate the impact of implementing a procedure-specific robotic hernia curriculum on surgical residents’ technical skills at a tertiary referral center.
METHODS
Study Population
This study was approved by the institutional review board at NorthShore University HealthSystem, and was reported in accordance with the ethical standards of institutional research, the Declaration of Helsinki, and the Consolidated Standards of Reporting Trials statement.28 This is a retrospective review of a prospectively maintained institutional database on the robotic training of University of Chicago general surgery residents. The training curriculum was conducted in a hospital-based simulation laboratory, the Grainger Center for Simulation and Innovation, which includes both the SimNow and the da Vinci Surgical System (Intuitive Surgical Inc., Sunnyvale, CA).
Robotic Curriculum
During the third clinical year, University of Chicago general surgery residents undergo an extensive 2-week robotic simulation training curriculum.29 As part of the 2-week curriculum, residents complete virtual reality and inanimate exercises on a da Vinci lab-based system. Two inanimate exercises included in the curriculum are an IHR and a VHR. These drills are performed 4 times each on the 5th day of the curriculum. All participants completed an internet survey following each drill. Participant demographics, prior robotic experience, and curriculum feedback were collected. All subject data were deidentified and stored on a secure, password-protected computer.
Hernia Models
Materials to create the inguinal and ventral hernia models were donated to the Grainger Center from Medtronic, Inc. (Minneapolis, Minnesota) and Intuitive Surgical, Inc. (Sunnyvale, California), respectively. Before performing each drill, residents were provided instruction slides, videos of attendings performing the drills, and intraoperative recordings of robotic IHR and VHRs. The drills were assembled by research staff on the da Vinci robot.
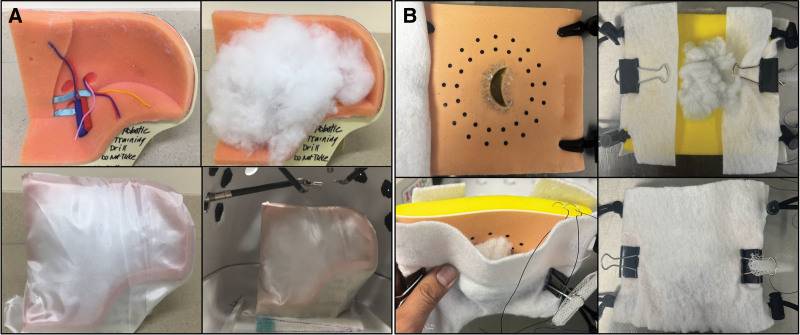
The IHR drill is created using the Medtronic anatomical model of the inguinal region. White fabric mimics the peritoneum, while loose cotton mimics the herniated peritoneal fat (Fig. 1A). Curved scissors are used to make an incision along the peritoneum, the “peritoneal flap” is developed, and the hernia is reduced by removing the cotton filling. Mesh is placed in the developed “pocket” and unfolded. A running 2-0 silk suture is used to close the peritoneum (see Video, Supplemental Digital Content 1, which demonstrates the inguinal hernia drill).
FIGURE 1.
(A) Inguinal hernia model and drill set-up. (B) Ventral hernia model and drill set-up.
The VHR drill is created using an Intuitive Surgical model of a hernia defect and models a robotic intraperitoneal underlay mesh repair. The white felt fabric mimics the peritoneum, and the loose cotton mimics the herniated peritoneal fat (Fig. 1B). The hernia is reduced by removing the cotton from the fascial defect, which is then closed in a running fashion using a Quill suture. The mesh is unrolled, placed over the fascial defect, and sutured in place on both sides of the defect using a 2-0 silk suture. An additional 2-0 silk suture is used to close the peritoneum (see Video, Supplemental Digital Content 2, which demonstrates the ventral hernia drill).
Grading of Robotic Hernia Drills
Each attempt of the hernia drill was video-recorded and graded by blinded expert surgeons using the modified Objective Structured Assessment of Technical Skills (OSATS) in the following domains: gentleness, time and motion, instrument handling, flow of operation, tissue exposure, and summary score.30,31 The duration of each attempt was recorded.
Establishing Grading Benchmarks
Benchmarks for trainee performance were established by 3 attending surgeons who had exceeded their learning curve in robotic hernia repair. These surgeons were either minimally invasive fellowship trained or had been in practice for over 20 years. All surgeons had well surpassed the learning curve for either robotic IHRs or VHRs. Each attending surgeon completed the IHR and VHR drills. The attempts were recorded and graded using the modified OSATS scoring system. The median OSATS scores and times from the 3 attending surgeons were used to establish benchmarks of proficiency for the residents. After completing the drills, the attendings graded the drills on their similarity to a real robotic hernia repair on a 5-point Likert scale, with 1 being “not close at all” and 5 being “extremely close”. Three critical steps of each hernia drill were graded: hernia reduction, mesh placement, and peritoneal closure, for a total score of 15.
Internet Survey
At the study’s conclusion, both residents and attendings were asked to undergo an exit survey regarding their attitudes towards the curriculum, including difficulty and utility.
Statistical Analysis
All statistical analysis was performed using SAS 9.4 (SAS Institute, Cary, NC). Continuous data are presented as mean and standard deviation (SD) or median with interquartile range based on the distribution of the data. Categorical variables are reported as frequencies and percentages. Intra-class correlation coefficients were calculated for the 2 graders, using a 2-way random effects model for agreement with average measures. Resident first and last attempts on the drill were compared to the attending median using the Wilcoxon rank-sum test. Resident attempts were also compared to subsequent prior attempts to evaluate for improvement using the paired t test. All tests were two-tailed with statistical significance considered as a P value < 0.05.
RESULTS
Trainee Cohort
Twenty residents started the hernia curriculum. Nineteen residents completed all 4 attempts of the IHR drill, while 17 residents completed all 4 attempts of the VHR drill. All residents completed the proficiency-based virtual reality curriculum before the hernia drills.
Intra-Class Correlation Coefficient
There was sufficient intra-class correlation between the 2 graders for OSATS technical scores for the IHR and VHR drills. For all hernia drills, the intra-class correlation was calculated as 0.61 (95% confidence interval: 0.40–0.61; P = 0.045], indicating moderate agreement between the graders.32
Expert Surgeon Drill Performance
Three experienced robotic hernia surgeons performed the IHR and VHR drills, with their times and OSATS scores recorded and used as a benchmark value for the trainees. For the IHR drill, attending median time was 14 (range 10–15) minutes and attending median total OSATS score was 26.5 (range 25–28) (Table 1). For the VHR drill, attending median time was 13 (range 12–15) minutes and attending median total OSATS score was 24 (range 23.5–28.5) (Table 2). Following completion of the hernia drills, the attending surgeons graded the drills based on their likeness to a real robotic hernia repair. The median score per drill was calculated from the 5-point Likert scale score per step, across the 3 steps. The median score for the likeness of the IHR drill was 12/15. The median score for the likeness of the VHR drill was 12/15.
TABLE 1.
Inguinal Hernia Drill, Resident OSATS Scores by Attempt vs. Attending Scores
| Average Resident OSATS Score Attempt 1 | Average Resident OSATS Score Attempt 2 | Average Resident OSATS Score Attempt 3 | Average Resident OSATS Score Attempt 4 | Change from Attempt 1 to 4 | P value | Median Attending OSATS Score (n = 3) | Median Resident OSATS Score Attempt 1 (n = 20) | P value | Median Resident OSATS Score Attempt 4 (n=19) | P value | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | 1st vs. 4th Attempt | Median (Min-Max) | Median (Min-Max) | Resident 1st Attempt vs. Attending | Median (Min-Max) | Resident 4th Attempt vs. Attending | |
| Respect for tissue | 2.9 ± 0.4 | 3.2 ± 0.4 | 3.5 ± 0.4 | 3.8 ± 0.5 | 1.0 ± 0.5 | <0.0001 | 5 (5–5) | 3 (2–3.5) | 0.0044 | 4 (2.5–4.5) | 0.0047 |
| Time and motion | 2.3 ± 0.7 | 2.9 ± 0.6 | 3.1 ± 0.7 | 3.8 ± 0.7 | 1.4 ± 0.7 | <0.0001 | 3.5 (3.5–4) | 2.5 (1–4) | 0.0106 | 3.5 (2–4.5) | 0.6877 |
| Instrument handling | 2.5 ± 0.6 | 3.0 ± 0.5 | 3.4 ± 0.5 | 3.9 ± 0.4 | 1.3 ± 0.6 | <0.0001 | 4 (4–4.5) | 2.5 (1.5–3.5) | 0.0051 | 4 (3–4.5) | 0.2131 |
| Flow and forward progress | 2.4 ± 0.7 | 3.0 ± 0.5 | 3.2 ± 0.7 | 3.8 ± 0.4 | 1.3 ± 0.7 | <0.0001 | 4.5 (4–4.5) | 2.5 (1.5–3.5) | 0.0054 | 4 (3–4.5) | 0.0622 |
| Tissue exposure | 3.0 ± 0.5 | 3.4 ± 0.7 | 3.7 ± 0.5 | 4.0 ± 0.4 | 1.0 ± 0.4 | <0.0001 | 5 (4.5–5) | 3 (2–4) | 0.0047 | 4 (3.5–4.5) | 0.0123 |
| Summary score | 2.4 ± 0.7 | 3.0 ± 0.7 | 3.3 ± 0.6 | 3.9 ± 0.5 | 1.5 ± 0.7 | <0.0001 | 4.5 (4–5) | 2.5 (1–4) | 0.0062 | 4 (3–4.5) | 0.0992 |
| Total OSATS | 15.5 ± 3.3 | 18.5 ± 3.2 | 20.1 ± 2.8 | 23.3 ± 2.4 | 7.5 ± 3.1 | <0.0001 | 26.5 (25–28) | 15.5 (9.5–22) | 0.0061 | 23.5 (18.5–27) | 0.0440 |
| Time (minutes) | 28.5 ± 9.3 | 25.2 ± 8.7 | 23.1 ± 5.3 | 20.5 ± 5.6 | −7.3 ± 8.7* | <0.0001 | 14 (10–15) | 28 (18–56) | 0.0061 | 19 (11–31) | 0.0241 |
OSATS: the modified objective structured assessment of technical skills.
Median = −6 minutes, Min = −37 minutes, Max = 0 minutes
Table 2.
Ventral Hernia Drill, Resident OSATS Scores by Attempt vs. Attending Scores
| Average Resident OSATS Score Attempt 1 | Average Resident OSATS Score Attempt 2 | Average Resident OSATS Score Attempt 3 | Average Resident OSATS Score Attempt 4 | Change from Attempt 1 to 4 | p-value | Median Attending OSATS Score (n=3) | Median Resident OSATS Score Attempt 1 (n=17) | p-value | Median Resident OSATS Score Attempt 4 (n=17) | p-value | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | 1st vs. 4th | Median (Min-Max) | Median (Min-Max) | Resident 1st Attempt vs. Attending | Median (Min-Max) | Resident 4th Attempt vs. Attending | |
| Respect for tissue | 3.1 ± 0.8 | 3.6 ± 0.6 | 3.9 ± 0.6 | 4.2 ± 0.6 | 1.1 ± 0.9 | 0.0007 | 4 (4–4.5) | 3 (1.5–4.5) | 0.0321 | 4.5 (3–5) | 0.7017 |
| Time and motion | 2.4 ± 0.8 | 3.1 ± 0.7 | 3.5 ± 0.6 | 3.5 ± 0.5 | 1.1 ± 0.9 | 0.0002 | 4 (3.5–5) | 2.5 (1–4) | 0.0117 | 3.5 (2.5–4) | 0.1216 |
| Instrument handling | 2.6 ± 0.7 | 3.1 ± 0.6 | 3.4 ± 0.6 | 3.5 ± 0.6 | 0.9 ± 0.8 | 0.0009 | 3.5 (3–4) | 2.5 (1.5–4.5) | 0.0312 | 3.5 (2–4.5) | 0.9120 |
| Flow and forward progress | 2.6 ± 0.8 | 3.1 ± 0.7 | 3.7 ± 0.6 | 3.8 ± 0.6 | 1.2 ± 0.9 | 0.0001 | 4.5 (4–5) | 2.5 (1–4) | 0.0068 | 4 (2.5–4.5) | 0.0712 |
| Tissue exposure | 3.5 ± 0.6 | 3.9 ± 0.4 | 4.4 ± 0.4 | 4.5 ± 0.5 | 1.0 ± 0.6 | <0.0001 | 5 (4.5–5) | 3.5 (2.5–4.5) | 0.0076 | 4.5 (3.5–5) | 0.1909 |
| Summary score | 2.6 ± 0.8 | 3.2 ± 0.7 | 3.8 ± 0.4 | 3.9 ± 0.5 | 1.3 ± 0.8 | <0.0001 | 4 (3.5–5) | 2.5 (1.5–4.5) | 0.0167 | 4 (3–4.5) | 0.5413 |
| Total OSATS | 16.8 ± 4.0 | 20.2 ± 3.2 | 22.6 ± 2.6 | 23.3 ± 2.9 | 6.5 ± 4.1 | <0.0001 | 24 (23.5–28.5) | 17 (10.5–26) | 0.0195 | 24.5 (17.5–26.5) | 0.4563 |
| Time (minutes) | 29.6 ± 6.5 | 23.8 ± 4.4 | 22.6 ± 4.4 | 21.2 ± 4.2 | −8.5 ± 4.9 | <0.0001 | 13 (12–15) | 30 (18–40) | 0.0068 | 22 (11–29) | 0.0192 |
OSATS: the modified objective structured assessment of technical skills.
IHR Trainee Performance
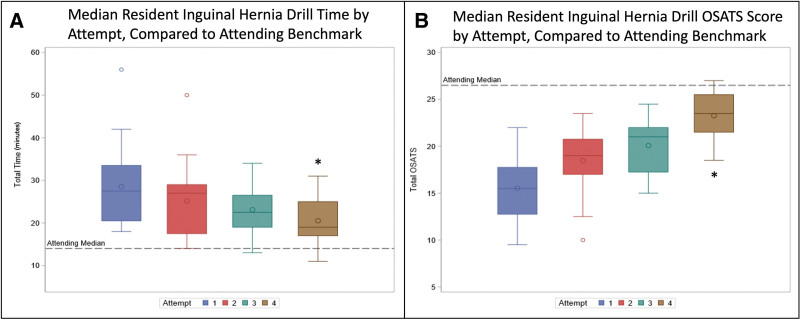
For the IHR drill, improvement in time was observed between the 1st and 4th attempt (28.5 ± 9.3 minutes vs 20.5 ± 5.6 minutes, P < 0.001). The average improvement was 7.3 ± 8.7 minutes. Additionally, improvement was observed in the average total OSATS score between the 1st and 4th attempt (15.5 ± 3.3 vs 23.3 ± 2.4; P < 0.001). The average improvement in score was 7.5 ± 3.1 points. By the 4th attempt, the residents achieved attending-level proficiency in 3 OSATS domains (time and motion, instrument handling, and flow of operation) and in the summary score (4 vs 4.5; P = 0.1), but not in total OSATS score (23.5 vs 26; P = 0.04) or time (19 vs 14 mins; P = 0.02) (Table 1). Figure 2A,B show median resident OSATS scores and time by attempt compared to attending benchmarks.
FIGURE 2.
(A) Median resident time duration for the inguinal hernia repair drill (1st attempt vs 4th attempt: 28.5 ± 9.3 minutes vs 20.5 ± 5.6 minutes, * = P < 0.001), and (B) median resident OSATS score (1st attempt vs 4th attempt: 15.5 ± 3.3 vs 23.3 ± 2.4, * = P < 0.001), compared to attending set benchmarks (dashed line).
VHR Trainee Performance
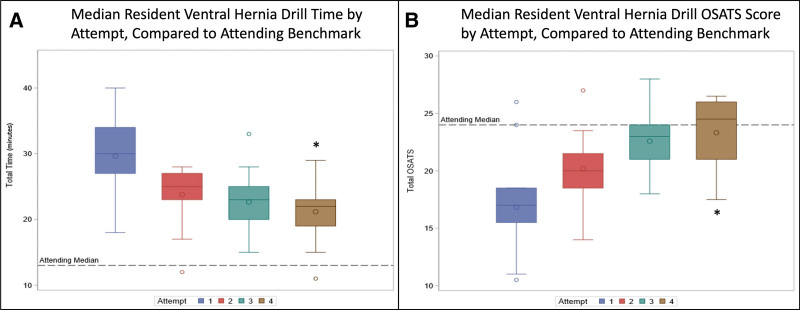
For the VHR drill, improvement in time was observed between the 1st and 4th attempt (29.6 ± 6.5 minutes vs 21.2 ± 4.2 minutes; P < 0.001). The average improvement was 8.5 ± 4.9 minutes. Additionally, improvement was observed in the average total OSATS score between the 1st and 4th attempt (16.8 ± 4.0 vs 23.3 ± 2.9; P < 0.001). The average improvement was 6.5 ± 4.1 points. By the 4th attempt, the residents achieved attending-level proficiency in total OSATS score (24.5 vs 24; P = 0.46), but not time (22 minutes vs 13 minutes; P = 0.02) (Table 2). Figure 3A,B show median resident OSATS scores and time by attempt compared to attending benchmarks.
FIGURE 3.
(A) Median resident time duration for the ventral hernia repair drill (1st attempt vs 4th attempt: 29.6 ± 6.5 minutes vs 21.2 ± 4.2 minutes, * = P < 0.001) and (B) median resident OSATS score (1st attempt vs 4th attempt: 16.8 ± 4.0 vs 23.3 ± 2.9, * = P < 0.001), compared to attending set benchmarks (dashed line).
Curriculum Perceptions
After completion of the hernia drills, all resident and attending opinions were surveyed regarding the difficulty and utility of the hernia drills. All assessments were conducted using a 5-point Likert scale. For difficulty, 1 was considered not difficult, while 5 was extremely difficult. For utility, 1 was considered not useful and 5 was extremely useful. Among the attendings, both the inguinal and ventral hernia drills were rated an average of 2 out of 5 in difficulty (range 1–2), and 4 out of 5 in utility (range 3–5). Among the residents, the hernia drills were rated an average of 2 out of 5 in difficulty (range 2–4), and a 4 out of 5 in utility (range 2–5).
DISCUSSION
This study is the first to investigate the impact of procedure-specific inanimate simulation of IHR and VHRs on general surgery resident robotic skills as part of a robotic training curriculum. Resident OSATS scores improved with each attempt, achieving attending-level proficiency in the VHR drill by the fourth attempt, and approaching attending-level proficiency in the IHR drill. The residents were not able to achieve attending-level proficiency in time to complete each drill. This is consistent with previous reports, which found that surgeons who did not complete robotic training before introducing robotic hernia surgery into their practice would need to complete approximately 28 additional cases to match the expected operative time of surgeons who did complete training.25 Furthermore, in the learning curve literature, operative time has been shown to be the most challenging metric to decrease and does not necessarily correlate with operative outcomes.32,33
The curriculum was well-received by the residents, who favored the implementation of procedure-specific simulation curricula. Attendings shared this opinion and universally agreed that residents should complete procedure-specific drills before sitting on the robot console. The hernia drills were not found to be particularly challenging, which is why these were the first drills performed after virtual simulation during the curriculum. However, both residents and attendings felt the drills were useful for training in robotic hernia repair, and residents still stood to improve further.29 In the future, such drills could be used as a way to determine resident preparedness to perform such procedures in the operating room.
The hernia drills were developed based on the previous robotic IHR experience from a high-volume center. On video review of 24 unilateral robotic IHRs, breakdown of the mean operative time by steps found the most time-consuming steps were the mesh placement and peritoneal closure.17 These steps also demonstrated the greatest improvement over time. Thus, the hernia drills were developed with a deliberate focus on these critical steps to maximize technical improvement. Tam et al25 found attending surgeons who completed a training program, including these hernia drills, before incorporating robotic IHRs in their practice decreased the learning curve and decreased cost per surgery by $1207.
After completing the hernia drills, the expert attendings were asked their opinion of the curriculum as a tool to introduce robotic IHR and VHR to surgical residents. The expert attendings agreed that the hernia drills were similar to the real procedures and served as a useful training tool. The difference in performance between the attendings and residents, and the stepwise improvement in resident performance with each attempt, demonstrates the construct validity of the hernia repair robotic curriculum with general surgery residents, as defined in a recent JAMA Surgery surgical education guide.34
With the increasing utilization of robotics in general surgery, it is essential to provide residents with adequate training on this platform, which is initially more technically laborious to learn than traditional open or laparoscopic instruments. Furthermore, the robotic platform also changes a traditional two-person operation at the bedside to a one-person operation at the console. Without the integration of general surgery residents in robotic cases, the rise of robotic surgery at academic centers could be detrimental to resident surgical training, perpetuating the prolonged proficiency cycle of adoption of new technology.27 While the majority of general surgery residents train at programs with access to a surgical robot system and have participated in robotic surgical cases, less than half of these residents have had any formal training on the robot and are often relegated to bedside assistants.35 In a multi-institutional needs assessment, VHR and IHR were identified as important procedures to include in a general surgery residency robotic curriculum.36 The need for the development of a robotic curriculum with the incorporation of hernia drills at the resident level is clear and unequivocal.
Proficiency-based simulation curriculums have already been shown to be effective in operative predictive validity among other surgical specialties, and can serve as models for general surgery.37 At 1 academic center, the implementation of a robotic training curriculum led to increased resident participation in robotic operative cases.38 Unsurprisingly, residents with experience performing robotic IHRs are noted to have better technical skills and receive greater operative autonomy.39 When residents were provided with adequate exposure to both laparoscopic and robotic techniques, residents not only performed better but actually preferred using the robot.40 The current study demonstrates that simulated robotic IHR and VHR drills can improve resident performance to a level similar to that of experienced attendings, reinforcing that robotic simulation and procedure-specific deliberate practice can improve resident operative technique and assist in proficiency of both the platform and procedure.
Pandora’s box has been opened with respect to the robotic platform in general surgery. Not only has implementation sky-rocketed, but robot availability and block time have become a major factor in recruitment across all surgical specialties. The crucial next steps will be improving training, optimizing case selection, and controlling cost. One way to do so is to implement proficiency-based credentialing, as opposed to minimum surgical volume privileging.41 After over 2 decades of the robot on the market, the target audience is shifting to an earlier career phase, making residency the ideal time to learn this technology.
There are several limitations to this study. First, the residents were assessed as a group rather than as individuals. Individual resident exposure to robotic surgery before starting the curriculum was not controlled for, and thus, residents have a variable level of baseline skill. Given the small cohort, outlier performance may have a larger influence on the results. Furthermore, there was no control group of residents who did not receive training. Given prior studies, which indicate worse performance without training, we deemed it unethical to withhold a training opportunity from residents.41 Second, there was an initial discrepancy in the intra-class correlation, which required re-training of video graders.
This study was performed at a well-resourced tertiary center. The resources available to the surgical residents, including the robotic curriculum, are not available to all surgeons across training environments. The cost associated with maintaining a robotic training program, including the simulation robot, the robotic instruments, and the staff to set up and evaluate resident performance, is expensive. This not only limits the ability to reproduce these results at other centers but is a barrier to broader dissemination of the curriculum.
While the IHR drill performed during the curriculum is modeled after the transabdominal preperitoneal mesh approach, the standard approach for all robotic IHRs, the VHR drill is modeled after the intraperitoneal underlay mesh repair. The intraperitoneal underlay mesh approach likely does not represent the majority of robotic VHRs performed, as many are performed using an enhanced totally extraperitoneal or robotic transabdominal preperitoneal approach. Thus, the VHR drill may not be as robust of a training model as the IHR drill. For VHRs performed using an enhanced totally extraperitoneal or robotic transabdominal preperitoneal approach, the dissection and hernia reduction are the most challenging aspects of the operation and require further refinement of the model to replicate.
Finally, this study only assesses resident performance on inanimate simulation and does not assess intraoperative performance. Future studies will aim to investigate how simulation-based robotic training influences surgical resident intraoperative performance. Investigation of skill retention is also ongoing.
In conclusion, a procedure-specific robotic hernia training curriculum improved residents’ technical skills in both the IHR and VHR drills. Future studies translating performance on simulated robotic hernia drills to the operating room remain necessary. Requiring residents to complete a robotic curriculum before operating robotically may be one way to shorten the learning curve and maintain patient safety while continuing to teach and progress trainee technical skills. We maintain that this training model is not only an effective way to teach residents various robotic hernia repairs but also serves as a framework for a broader resident robotic curriculum and future proficiency-based credentialing pathways for surgeons.
ACKNOWLEDGMENTS
Study conception and design: A.A.A., A.R., M.R.B., M.T., and M.E.H. Data acquisition: S.B.H., A.A.A, A.R., M.R.B., S.A.M., S.H., H.M.H., and J.L. Quality control of data and algorithms, data analysis and interpretation, and statistical analysis: S.B.H., A.A.A., K.K., A.R., S.A.M., M.T., and M.E.H. Manuscript preparation: S.B.H., A.A.A., and M.E.H. Manuscript editing and review: S.B.H., A.A.A., K.K., A.R., M.R.B., S.A.M., S.H., H.M.H., J.L., M.T., and M.E.H.
Footnotes
Sarah B. Hays and Amr I. Al Abbas are considered as co-first authors.
M.E.H. has received funding from Intuitive Surgical, Inc. to NorthShore University HealthSystem for robotic training and resident education. S.H. has received consulting fees from Medtronic, Inc., a teaching honorarium from Intuitive Surgical, Inc., and serves on the Data Safety Monitoring Board for Becton Dickinson. J.L. serves as a consultant for WL Gore and Associates. Other authors declare that they have nothing to disclose.
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.annalsofsurgery.com).
REFERENCES
- 1.McDermott KW, Liang L. Overview of major ambulatory surgeries performed in hospital-owned facilities, 2019. Statistical Brief #287. 2021. Available at: https://hcup-us.ahrq.gov/reports/statbriefs/sb287-Ambulatory-Surgery-Overview-2019.jsp. Accessed January 9, 2024. [PubMed] [Google Scholar]
- 2.Howard R, Thumma J, Ehlers A, et al. Trends in surgical technique and outcomes of ventral hernia repair in the United States. Ann Surg. 2023;278:274–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Madion M, Goldblatt MI, Gould JC, et al. Ten-year trends in minimally invasive hernia repair: a NSQIP database review. Surg Endosc. 2021;35:7200–7208. [DOI] [PubMed] [Google Scholar]
- 4.Escobar Dominguez JE, Gonzalez A, Donkor C. Robotic inguinal hernia repair. J Surg Oncol. 2015;112:310–314. [DOI] [PubMed] [Google Scholar]
- 5.Sheetz KH, Claflin J, Dimick JB. Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw Open. 2020;3:e1918911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bonner SN, Thumma JR, Dimick JB, et al. Trends in use of robotic surgery for privately insured patients and medicare fee-for-service beneficiaries. JAMA Netw Open. 2023;6:e2315052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pahwa HS, Kumar A, Agarwal P, et al. Current trends in laparoscopic groin hernia repair: a review. World J Clin Cases. 2015;3:789–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Memon MA, Cooper NJ, Memon B, et al. Meta-analysis of randomized clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg. 2003;90:1479–1492. [DOI] [PubMed] [Google Scholar]
- 9.Iraniha A, Peloquin J. Long-term quality of life and outcomes following robotic assisted TAPP inguinal hernia repair. J Robot Surg. 2018;12:261–269. [DOI] [PubMed] [Google Scholar]
- 10.Forester B, Attaar M, Donovan K, et al. Short-term quality of life comparison of laparoscopic, open, and robotic incisional hernia repairs. Surg Endosc. 2021;35:2781–2788. [DOI] [PubMed] [Google Scholar]
- 11.Kalata S, Thumma JR, Norton EC, et al. Comparative safety of robotic-assisted vs laparoscopic cholecystectomy. JAMA Surg. 2023;158:1303–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pradarelli JC, Thornton JP, Dimick JB. Who is responsible for the safe introduction of new surgical technology?: an important legal precedent from the da Vinci Surgical System Trials. JAMA Surg. 2017;152:717–718. [DOI] [PubMed] [Google Scholar]
- 13.Arcerito M, Changchien E, Bernal O, et al. Robotic inguinal hernia repair: technique and early experience. Am Surg. 2016;82:1014–1017. [PubMed] [Google Scholar]
- 14.Escobar Dominguez JE, Ramos MG, Seetharamaiah R, et al. Feasibility of robotic inguinal hernia repair, a single-institution experience. Surg Endosc. 2016;30:4042–4048. [DOI] [PubMed] [Google Scholar]
- 15.Kudsi OY, McCarty JC, Paluvoi N, et al. Transition from laparoscopic totally extraperitoneal inguinal hernia repair to robotic transabdominal preperitoneal inguinal hernia repair: a retrospective review of a single surgeon’s experience. World J Surg. 2017;41:2251–2257. [DOI] [PubMed] [Google Scholar]
- 16.Oviedo RJ, Robertson JC, Alrajhi S. First 101 robotic general surgery cases in a community hospital. JSLS. 2016;20:e2016.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tam V, Rogers DE, Al-Abbas A, et al. Robotic inguinal hernia repair: a large health system’s experience with the first 300 cases and review of the literature. J Surg Res. 2019;235:98–104. [DOI] [PubMed] [Google Scholar]
- 18.Solaini L, Cavaliere D, Rocco G, et al. Differences in the learning curve of robotic transabdominal preperitoneal inguinal hernia repair according to surgeon’s robotic experience. Hernia. 2023;27:1123–1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choi YS, Kim KD, Choi MS, et al. Initial Experience of robot-assisted transabdominal preperitoneal (TAPP) inguinal hernia repair by a single surgeon in South Korea. Medicina (Kaunas). 2023;59:582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kudsi OY, Gokcal F, Bou-Ayash N, et al. Learning curve in robotic transabdominal preperitoneal (rTAPP) ventral hernia repair: a cumulative sum (CUSUM) analysis. Hernia. 2021;25:755–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kudsi OY, Gokcal F, Bou-Ayash N, et al. Learning curve in robotic primary ventral hernia repair using intraperitoneal onlay mesh: a cumulative sum analysis. Surg Laparosc Endosc Percutan Tech. 2020;31:346–355. [DOI] [PubMed] [Google Scholar]
- 22.Lima DL, Berk R, Cavazzola LT, et al. Learning curve of robotic enhanced-view extraperitoneal approach for ventral hernia repairs. J Laparoendosc Adv Surg Tech A. 2023;33:81–86. [DOI] [PubMed] [Google Scholar]
- 23.Rice MK, Hodges JC, Bellon J, et al. Association of mentorship and a formal robotic proficiency skills curriculum with subsequent generations’ learning curve and safety for robotic pancreaticoduodenectomy. JAMA Surg. 2020;155:607–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al Abbas AI, Wang C, Hamad AB, et al. Mentorship and formal robotic proficiency skills curriculum improve subsequent generations’ learning curve for the robotic distal pancreatectomy. HPB. 2021;23:1849–1855. [DOI] [PubMed] [Google Scholar]
- 25.Tam V, Borrebach J, Dunn SA, et al. Proficiency-based training and credentialing can improve patient outcomes and decrease cost to a hospital system. Am J Surg. 2019;217:591–596. [DOI] [PubMed] [Google Scholar]
- 26.Richards MK, McAteer JP, Drake FT, et al. A national review of the frequency of minimally invasive surgery among general surgery residents: assessment of ACGME case logs during 2 decades of general surgery resident training. JAMA Surg. 2015;150:169–172. [DOI] [PubMed] [Google Scholar]
- 27.Mehaffey JH, Michaels AD, Mullen MG, et al. Adoption of robotics in a general surgery residency program: at what cost? J Surg Res. 2017;213:269–273. [DOI] [PubMed] [Google Scholar]
- 28.Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ. 2010;340:c869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ramirez Barriga M, Rojas A, Roggin KK, et al. Development of a two-week dedicated robotic surgery curriculum for general surgery residents. J Surg Educ. 2022;79:861–866. [DOI] [PubMed] [Google Scholar]
- 30.Martin JA, Regehr G, Reznick R, et al. Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg. 1997;84:273–278. [DOI] [PubMed] [Google Scholar]
- 31.Birkmeyer JD, Finks JF, O’Reilly A, et al. ; Michigan Bariatric Surgery Collaborative. Surgical skill and complication rates after bariatric surgery. N Engl J Med. 2013;369:1434–1442. [DOI] [PubMed] [Google Scholar]
- 32.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boone BA, Zenati M, Hogg ME, et al. Assessment of quality outcomes for robotic pancreaticoduodenectomy: identification of the learning curve. JAMA Surg. 2015;150:416–422. [DOI] [PubMed] [Google Scholar]
- 34.Stefanidis D, Torbeck L, Kaji AH. Practical guide to common flaws with surgical education research. JAMA Surg. 2024;159:339–340. [DOI] [PubMed] [Google Scholar]
- 35.Farivar BS, Flannagan M, Leitman IM. General surgery residents’ perception of robot-assisted procedures during surgical training. J Surg Educ. 2015;72:235–242. [DOI] [PubMed] [Google Scholar]
- 36.Imai T, Amersi F, Tillou A, et al. A multi-institutional needs assessment in the development of a robotic surgery curriculum: perceptions from resident and faculty surgeons. J Surg Educ. 2023;80:93–101. [DOI] [PubMed] [Google Scholar]
- 37.Culligan P, Gurshumov E, Lewis C, et al. Predictive validity of a training protocol using a robotic surgery simulator. Female Pelvic Med Reconstr Surg. 2014;20:48–51. [DOI] [PubMed] [Google Scholar]
- 38.Grannan HR, Hetzel E, Goldblatt MI, et al. Robotic general surgery resident training curriculum: a pilot experience. Surg Laparosc Endosc Percutan Tech. 2021;31:588–593. [DOI] [PubMed] [Google Scholar]
- 39.Ebeling PA, Beale KG, Van Sickle KR, et al. Resident training experience with robotic assisted transabdominal preperitoneal inguinal hernia repair. Am J Surg. 2020;219:278–282. [DOI] [PubMed] [Google Scholar]
- 40.Choi SH, Kuchta K, Rojas A, et al. Residents perform better technically, have less stress and workload, and prefer robotic to laparoscopic technique during inanimate simulation. Surg Endosc. 2023;37:7230–7237. [DOI] [PubMed] [Google Scholar]
- 41.Tam V, Zeh HJ, Hogg ME. Incorporating metrics of surgical proficiency into credentialing and privileging pathways. JAMA Surg. 2017;152:494–495. [DOI] [PubMed] [Google Scholar]