Summary:
True parenchymal breast changes following COVID-19 vaccination are exceedingly rare. Equally rare are incidences of pseudoangiomatous stromal hyperplasia (PASH)–associated gigantomastia. The patient in this case report presented with both occurrences and experienced massive breast enlargement 1 week postadministration of the Pfizer/BioNTech COVID-19 vaccine, which worsened after her second dose. Definitive treatment was achieved through reduction mammoplasty, with the final pathology report confirming uniformly dense terminal duct lobular units with interspersed PASH units. The association between the COVID-19 vaccine, PASH, and breast hypertrophy warrants further investigation to comprehend the spectrum of reactions to the vaccine.
Gigantomastia is a rare condition characterized by rapid, diffuse, and excessive breast growth.1 The etiology of gigantomastia is incompletely understood, but triggers have been classified into (1) idiopathic spontaneous growth, (2) endogenous hormone overproduction, and (3) pharmacological agents.1
Recent reports suggest that some on social media have claimed to experience breast growth following Pfizer COVID-19 vaccine administration—dubbed the “Pfizer boob job.”2 Although axillary lymphadenopathy is a known side effect of COVID-19 mRNA vaccines, such changes are transient and contribute only to the perception of breast growth.3 To date, there has been only 1 published case outlining lasting parenchymal breast changes, presenting as a palpable mass, following administration of the Pfizer COVID-19 mRNA booster.4 No formal studies have established a link between breast parenchymal growth and the Pfizer COVID-19 vaccine. Although these social media claims have been disputed by the New Zealand Ministry of Health, more research is needed to further investigate these findings.2
A known cause of gigantomastia is pseudoangiomatous stromal hyperplasia (PASH). PASH is characterized by idiopathic fibrous mammary stroma hyperplasia, typically associated with estrogen and progesterone overexpression.5 Most commonly, PASH manifests as incidental histological findings in the evaluation of breast lesions or as a palpable mass.6 There are fewer than 20 reports of PASH presenting as bilateral gigantomastia.7–9 (See table, Supplemental Digital Content 1, which displays case reports of PASH-associated gigantomastia, http://links.lww.com/PRSGO/D710.) This case is the first to demonstrate a temporal association between PASH-associated gigantomastia and a vaccine. The management of PASH-related gigantomastia typically involves surgical treatment with bilateral mammoplasty or total mastectomy, conservative treatment (eg, tamoxifen), and/or careful observation in patients with low concern for breast cancer.5
Here, we present a case of bilateral gigantomastia following Pfizer COVID-19 vaccine administration. Ultimately, pathology indicated PASH interspersed in dense glandular breasts.
CASE REPORT
A healthy, nulliparous 19-year-old woman experienced significant breast hypertrophy starting 1 week after receiving the Pfizer COVID-19 vaccine in September 2022. Her medical history was unremarkable, with no hormonal disturbances detected on bloodwork.
The patient initially reported tingling paresthesia in her breasts, followed by sudden bilateral growth which worsened after receiving the second vaccine dose. Over 6 months, her breast size increased from a B cup to a triple G (Fig. 1). Physical examination revealed dense, warm, edematous, ptotic breasts with no palpable masses or axillary lymphadenopathy.
Fig. 1.
Preoperative image of patient with triple G cup breasts following development of macromastia after administration of Pfizer COVID-19 vaccine.
Breast ultrasound and chest computed tomography showed diffuse bilateral breast enlargement with mild axillary lymphadenopathy and hyperattenuating areas likely representing hypertrophic tissue. Core biopsies suggested fibroepithelial lesions, such as fibroadenoma, hamartoma, and PASH. Despite a trial of steroids and antibiotics, symptoms persisted and no clear etiology was identified, leading to the decision of surgical management.
Eleven months post vaccine, the plastic surgery team opted for bilateral reduction mammoplasty, as breast growth had stabilized for 5 months and comprehensive work-up was normal.
Intraoperatively, a Wise pattern reduction with a superomedial pedicle approach was performed. Despite standard blood loss control methods, there was significant blood loss (1.2–1.5 L), likely due to increased tissue vascularity and inadequate penetration of tumescence in dense tissue. Hemodynamic stability was regained with intravenous fluid support; however, further reduction was limited to minimize greater blood loss. Left and right specimens weighed 1906 and 1664 g, respectively, reducing her breast size from a triple G to a double D (Figs. 2, 3).
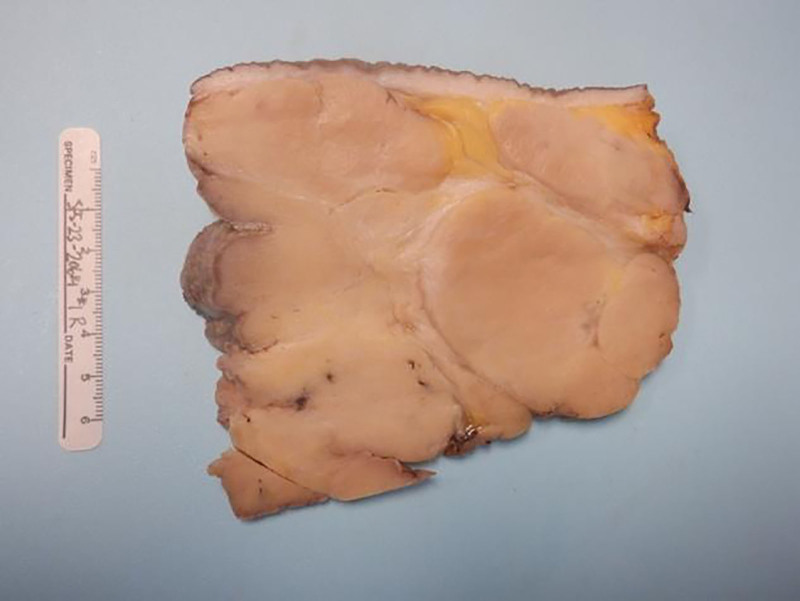
Fig. 2.
Gross specimen postbilateral reduction mammoplasty for gigantomastia.
Fig. 3.
Image of patient 5 months postreduction mammoplasty, now with double D breasts.
Final pathology confirmed hypertrophied glandular breast tissue with multiple well-defined regions of PASH bilaterally (Fig. 3). The patient additionally had increased density of terminal duct lobular units interspersed with PASH.
Due to significant intraoperative blood loss, the patient’s hemoglobin dropped from 11 g/dL preoperatively to 6.7 g/dL postoperatively, necessitating transfusion of 3 units of packed red blood cells over 2 days. By postoperative day 2, her hemoglobin stabilized at 8.1 g/dL, and she was discharged. On postoperative day 3, she returned to the emergency department with fever (103.1°F) and chest pain but remained hemodynamically stable. There was no evidence of infection, transfusion reaction, bleeding, or pulmonary embolism. Her hemoglobin dropped to 7.2 g/dL, and she received 300 mg intravenous Venofer, with plans for further outpatient doses.
At 5 months postoperation, breast asymmetry and areolar hypopigmentation were noted. There has been no recurrence of breast growth, and further breast reduction is being considered to correct asymmetry and return to her normal breast size.
DISCUSSION
This case presents a healthy young woman with rapid bilateral breast enlargement 1 week following Pfizer COVID-19 vaccine administration. After ruling out other potential causes, she underwent bilateral reduction mammoplasty, with histology revealing dense terminal duct lobular units interspersed with PASH.
The patient believed that the vaccine caused her breast growth; however, her concerns were not adequately addressed by her primary care physicians, leading to mistrust in the healthcare system. After multiple specialist consultations and unsuccessful medication trials, she underwent definitive surgical treatment. Although a temporal relationship does not establish causality, dismissing patient concerns can erode trust. Physicians should consider and value patient concerns when developing therapeutic relationships.10
PASH-associated gigantomastia is rare, with fewer than 20 documented cases (Supplemental Digital Content 1, http://links.lww.com/PRSGO/D710).7–9 Current gigantomastia classification systems do not account for PASH as an etiological factor and lack detail on the timeline of breast growth or the type of tissue involved.1 Including these elements could improve clinical decision-making and streamline management. Further research is needed to develop a comprehensive classification system for gigantomastia that assists in treatment planning and deepens understanding of PASH.
CONCLUSIONS
The cause of gigantomastia remains unclear. Here, we present the case of a healthy female patient who experienced rapid breast enlargement, progressing from a B cup to a triple G cup over 6 months, beginning 1 week following Pfizer COVID-19 vaccination. She underwent bilateral reduction mammoplasty, complicated by intraoperative bleeding, necessitating postoperative transfusions. Surgical specimens confirmed PASH. Further research is needed to understand PASH etiology, refine gigantomastia classification, and explore the potential link between the Pfizer vaccine, gigantomastia, and PASH.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Supplementary Material
Footnotes
Published online 20 December 2024.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Dancey A, Khan M, Dawson J, et al. Gigantomastia - a classification and review of the literature. J Plast Reconstr Aesthet Surg. 2008;61:493–502. [DOI] [PubMed] [Google Scholar]
- 2.NZ Herald. Covid 19 coronavirus: women’s claims breasts get bigger after Pfizer vaccine rubbished by Ministry of Health. The New Zealand Herald; 2021. Available at: https://www.nzherald.co.nz/nz/covid-19-coronavirus-womens-claims-breasts-get-bigger-after-pfizer-vaccine-rubbished-by-ministry-of-health/FASABDQAI7IAWPYQZSVQC5FGBE/. Accessed July 3, 2024. [Google Scholar]
- 3.Özütemiz C, Krystosek LA, Church AL, et al. Lymphadenopathy in COVID-19 vaccine recipients: diagnostic dilemma in oncologic patients. Radiology. 2021;300:E296–E300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Soeder E, Toro-Pape FW, Lampen-Sachar K. Isolated breast parenchymal changes following COVID-19 vaccine booster. Radiol Case Rep. 2022;17:4556–4560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gresik CM, Godellas C, Aranha GV, et al. Pseudoangiomatous stromal hyperplasia of the breast: a contemporary approach to its clinical and radiologic features and ideal management. Surgery. 2010;148:752–757; discussion 757. [DOI] [PubMed] [Google Scholar]
- 6.Jaunoo SS, Thrush S, Dunn P. Pseudoangiomatous stromal hyperplasia (PASH): a brief review. Int J Surg. 2011;9:20–22. [DOI] [PubMed] [Google Scholar]
- 7.Parisi P, Vinci F, Di Meglio F, et al. Recurrent extreme bilateral gigantomastia caused by pseudoangiomatous stromal hyperplasia (PASH) syndrome: a case report. Plast Reconstr Surg Glob Open. 2023;11:e4571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krawczyk N, Fehm T, Ruckhäberle E, et al. Bilateral diffuse pseudoangiomatous stromal hyperplasia (PASH) causing gigantomastia in a 33-year-old pregnant woman: case report. Breast Care. 2016;11:356–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vashistha A, Rundla M, Khan F, et al. Idiopathic gigantomastia with pseudoangiomatous stromal hyperplasia: a case report. Int J Surg Case Rep. 2020;77:915–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fuehrer S, Weil A, Osterberg LG, et al. Building authentic connection in the patient-physician relationship. J Prim Care Community Health. 2024;15:21501319231225996. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.