Abstract
Purpose: To describe a case of frosted branch angiitis–like retinal vasculitis that developed after scleral buckle surgery. Methods: A single case was evaluated. Results: Five days after nondrainage scleral buckle surgery with a segmental buckle and encircling band, an otherwise healthy 39-year-old man presented with frosted branch angiitis. Treatment initially involved oral corticosteroids. After 5 days of treatment, there was a decrease in the subretinal exudation; however, the break appeared to be lifting with persistent subretinal fluid. Pars plana vitrectomy (PPV) with silicone oil (SO) injection was performed. A vitreous biopsy was taken during the PPV that was negative for bacterial, fungal, and viral markers. The patient’s blood and urine culture showed no microbial growth, ruling out an infectious cause. Ultimately, the SO was removed, with a good visual outcome. Conclusions: Although the cause is unknown, retinal vasculitis may occur after scleral buckle surgery, albeit rarely.
Keywords: frosted branch angiitis, retinal vasculitis, scleral buckle, retinal detachment, postoperative
Introduction
Frosted branch angiitis is an immune-mediated disorder of the retinal vasculature. 1 It is an uncommon form of retinal vasculitis that is characterized by prominent perivascular sheathing of the retinal vessels resembling frost on tree branches during icy winters. 2 Frosted branch angiitis can be idiopathic or secondary to infectious, inflammatory, or neoplastic systemic diseases; it can also occur after ocular trauma.3,4
Postoperative retinal vasculitis has been reported to occur after pars plana vitrectomy (PPV) in rare cases; however, to our knowledge retinal vasculitis after scleral buckle surgery has not been reported in the literature.5,6 We present a case of frosted branch angiitis–like vasculitis that developed early in the postoperative period after uneventful scleral buckle surgery for a rhegmatogenous retinal detachment (RRD).
Case Report
A 39-year-old man presented to the retina clinic with a report of seeing a large floater in the nasal field of vision of the left eye for 5 days. He had no history of systemic disease, recent fever, or illness; was not taking any medications; and had no history of ocular trauma.
Fifteen years previously, the patient had laser in situ keratomileusis in both eyes. Before the refractive surgery, he had barrage laser application in both eyes for lattice degeneration. The patient also had scleral buckle surgery for an RRD in the right eye 7 years previously. His best-corrected visual acuity (BCVA) was 20/25 OU, and the intraocular pressures were within normal limits. An anterior segment examination was unremarkable. A fundus examination of the right eye showed an attached retina with a good buckle indent and multiple areas of laser and cryopexy scars (Figure 1A). The fundus examination of the left eye showed an inferotemporal RRD with subretinal fluid (SRF) encroaching on the macula. A horseshoe tear was seen temporally in the detached retina and another horseshoe tear inferonasally in the attached retina with barrage laser scars around the previously lasered lattice degeneration (Figure 1B).
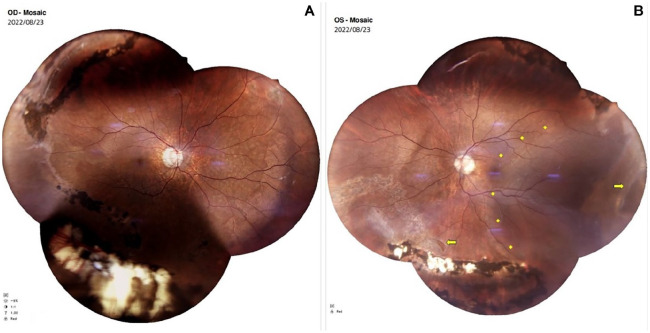
Figure 1.
Preoperative color fundus photographs show (A) an attached retina in the right eye after scleral buckle surgery and (B) an inferotemporal retinal detachment (marked by yellow rhomboids) with a horseshoe tear in the temporal detached retina and an inferonasal attached retina (marked by yellow arrows) in the left eye.
The patient had nondrainage scleral buckle surgery. Cryopexy was applied at the site of the break, and a temporal segmental buckle (number 276) was secured with 5-0 polytetrafluoroethylene (Dacron) sutures along with an encircling band (number 240) secured with scleral tunnels. Augmentation of anesthesia was not needed during surgery, and the ocular surface was washed with 5% povidone–iodine at the end of the case.
One day postoperatively, the patient’s BCVA was 20/400 OS and the fundus examination showed a good buckle indent with less SRF than preoperatively. The patient was started on routine topical postoperative medications (ie, antibiotics, corticosteroids, and cycloplegic eye drops) and was scheduled for a follow-up appointment 5 days later.
When the patient presented to the retina clinic on postoperative day 5, an examination showed inferotemporal retinal vasculitis in the left eye with a frosted branch angiitis–like appearance, subretinal yellow–white exudation, and intraretinal hemorrhages (Figure 2). Despite the appearance of the fundus, the patient was otherwise comfortable, and his VA was maintained. He did not report eye pain, and the eye congestion was less than on the first postoperative day. Oral ciprofloxacin was initiated.
Figure 2.
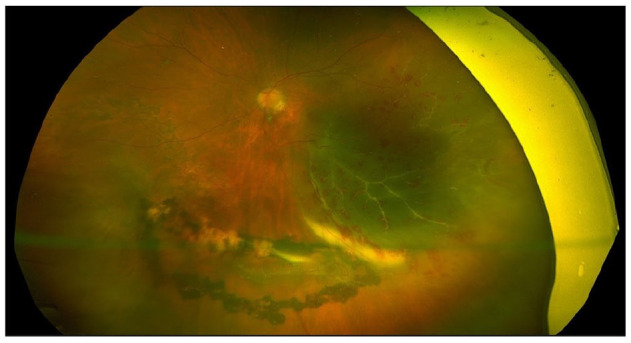
Color fundus photograph of the left eye shows frosted branch angiitis 5 days after scleral buckle surgery.
The patient was asked to return the next day, by which time the retinal exudation and vitritis had increased; therefore, oral corticosteroids (prednisolone) were started with the dose based on his body weight. Blood and urine cultures were negative. After 1 week of oral corticosteroid therapy, although the vasculitis had almost resolved, the break appeared to be lifting with persistent SRF (Figure 3). PPV with endolaser treatment and silicone oil (SO) injection was planned.
Figure 3.
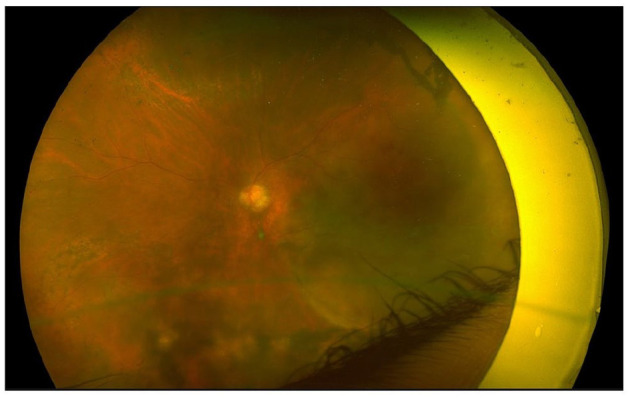
Color fundus photograph of the left eye shows vasculitis with persistent subretinal fluid that has almost resolved after 1 week of oral corticosteroid therapy.
A vitreous biopsy taken at the time of PPV was negative. Polymerase chain reaction (PCR) testing for bacterial, fungal, and viral markers, including toxoplasma, varicella zoster virus, cytomegalovirus, and herpes simplex virus DNA, was also negative. A systemic assessment, including a general physical examination with a complete blood count, a peripheral blood smear, a liver function test, a renal function test, routine and microscopic urine examinations, a chest x-ray, and testing for human immunodeficiency virus and hepatitis B surface antigen, was done before the scleral buckle surgery. All results were unremarkable.
After PPV with SO injection, the retina was attached and the vasculitis had completely resolved. Oral corticosteroids were continued with the dose tapered over 3 days. Six weeks after PPV, the SO was removed. Two months after SO removal, the retina was attached (Figure 4), and the BCVA was 20/30 OS.
Figure 4.
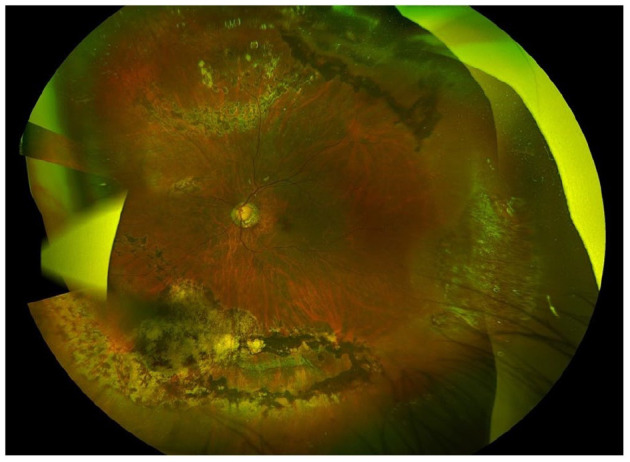
Color fundus photograph of the left eye 2 months after silicone oil removal shows an attached retina with resolved vasculitis.
Conclusions
To our knowledge, this is the first reported case of frosted branch angiitis and vasculitis after scleral buckle surgery. In rare cases, vasculitis has been reported to occur after PPV with SO injection as a manifestation of toxic posterior segment syndrome, 5 while frosted branch angiitis has been reported to occur after repair of an open-globe injury7,8 and in a case after blunt trauma. 9
Frosted branch angiitis was first reported and named by Ito et al, 2 who reported the condition in a healthy 6-year-old child with bilateral involvement. Kleiner 3 subsequently classified frosted branch angiitis into 3 groups based on etiology: type 1 in leukemia or lymphoma, type 2 in association with viral or autoimmune diseases, and type 3, which is idiopathic. In type 1 disease, vasculitis is believed to result from the direct infiltration of blood vessel walls by cancer cells. In type 2 disease, vasculitis is believed to be immune-mediated and to be caused by immune complex deposition.
The exact mechanism and cause of vasculitis in our case is uncertain. Our patient was an otherwise healthy man with no systemic illness or previous prodrome or illness. He had none of the systemic associations reported with frosted branch angiitis. Systemic illness and leukemia or lymphoma were ruled out during the preoperative assessment. Frosted branch angiitis has been reported to be associated with cytomegalovirus infection,10–12 ocular toxoplasmosis,13,14 ocular tuberculosis,1,4 varicella zoster virus infection, 15 and herpes simplex virus infection. 16 The vitreous biopsy taken at the time of PPV was negative for all these infections, and our patient had a complete recovery without being treated for any of them.
Although vasculitis can be a presenting feature of endophthalmitis,17,18 the patient’s blood and urine cultures as well as the vitreous biopsy smear and culture were all negative. In addition, the vitreous biopsy PCR was negative for bacterial, fungal, and viral DNA markers. Moreover, the vasculitis resolved rapidly after oral corticosteroid therapy was initiated, thereby supporting an immune-mediated rather than an infectious origin.
A possible mechanism of vasculitis in our case could have been an indentation caused by the cryopexy probe, mimicking blunt trauma to the eye. This, coupled with a breakdown of the blood–retinal barrier from the cryopexy, could have stimulated an immune response to self-antigens. However, the patient’s fellow eye had uneventful scleral buckle surgery in the past. In addition, scleral buckle surgery for RRD has been practiced worldwide for more than 60 years, and to our knowledge no previous reports of vasculitis after scleral buckle surgery exist, making it a less likely cause.
In conclusion, although the cause in this case is unknown, vasculitis can occur after scleral buckle surgery. Timely initiation of treatment can provide a good outcome without long-term vision-threatening sequelae.
Footnotes
Ethical Approval: This case report was conducted in accordance with the Declaration of Helsinki. The collection and evaluation of all protected patient health information were performed in a US Health Insurance Portability and Accountably Act–compliant manner.
Statement of Informed Consent: The patient consented to publication of the clinical history, findings, and images.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of the article.
Funding: Funded by Hyderabad Eye Research Foundation.
ORCID iDs: Arjun Desai  https://orcid.org/0009-0001-0790-629X
https://orcid.org/0009-0001-0790-629X
Mudit Tyagi  https://orcid.org/0000-0001-9211-917X
https://orcid.org/0000-0001-9211-917X
Ritesh Narula  https://orcid.org/0000-0003-0192-0178
https://orcid.org/0000-0003-0192-0178
References
- 1. Walker S, Iguchi A, Jones NP. Frosted branch angiitis: a review. Eye (Lond). 2004;18(5):527-533. doi: 10.1038/sj.eye.6700712 [DOI] [PubMed] [Google Scholar]
- 2. Ito Y, Nakano M, Kyu N, Takeuchi M. Frosted branch angiitis in a child. Rinsho Ganka (Jpn J Clin Ophthalmol). 1976;30:797-803. [Google Scholar]
- 3. Kleiner RC. Frosted branch angiitis: clinical syndrome or clinical sign? Retina. 1997;17(5):370-371. doi: 10.1097/00006982-199709000-00002 [DOI] [PubMed] [Google Scholar]
- 4. Lee K, Jung S, Chin HS. Frosted branch angiitis; case series and literature review. Ocul Immunol Inflamm. 2024;32(1):31-39. doi: 10.1080/09273948.2022.2148112 [DOI] [PubMed] [Google Scholar]
- 5. Sahoo NK, Behera S, Narayanan R, Chhablani J. Toxic posterior segment syndrome presenting as occlusive retinal vasculitis following vitreoretinal surgery. J Curr Ophthalmol. 2021;33(3):345-348. doi: 10.4103/joco.joco_42_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Markan A, Singla P, Singh R. Development of retinal vasculitis following an uneventful pars plana vitrectomy. BMJ Case Rep. 2022;15(8):e251917. doi: 10.1136/bcr-2022-251917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ramachandran NO, Kohli P, Babu N, Mishra C, Chakrabarti A. Frosted branch angiitis following corneal tear repair. Taiwan J Ophthalmol. 2022;12(4):491-494. doi: 10.4103/tjo.tjo_52_21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Madanagopalan VG, Nagesha CK, Velis G, Devulapally S, Balamurugan S. Frosted branch angiitis with penetrating ocular trauma and retained intraocular foreign body. Indian J Ophthalmol. 2018;66(7):1031-1033. doi: 10.4103/ijo.IJO_1276_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kahloun R, Abroug N, Ammari W, et al. Acute retinal periphlebitis mimicking frosted branch angiitis associated with exudative retinal detachment after blunt eye trauma. Int Ophthalmol. 2014;34(5):1149-1151. doi: 10.1007/s10792-014-9958-0 [DOI] [PubMed] [Google Scholar]
- 10. Geier SA, Nasemann J, Klauss V, Kronawitter U, Goebel FD. Frosted branch angiitis associated with cytomegalovirus retinitis. Am J Ophthalmol. 1992;114(4):514-516. doi: 10.1016/s0002-9394(14)71876-8 [DOI] [PubMed] [Google Scholar]
- 11. Secchi AG, Tognon MS, Turrini B, Carniel G. Acute frosted retinal periphlebitis associated with cytomegalovirus retinitis. Retina. 1992;12(3):245-247. doi: 10.1097/00006982-199212030-00008 [DOI] [PubMed] [Google Scholar]
- 12. Rodrigues TM, Marques JP, Fonseca C. Multimodal imaging of cytomegalovirus-associated frosted branch angiitis. Ophthalmol Retina. 2018;2(1):37. doi: 10.1016/j.oret.2017.09.009 [DOI] [PubMed] [Google Scholar]
- 13. Ysasaga JE, Davis J. Frosted branch angiitis with ocular toxoplasmosis. Arch Ophthalmol. 1999;117(9):1260-1261. doi: 10.1001/archopht.117.9.1260 [DOI] [PubMed] [Google Scholar]
- 14. Oh J, Huh K, Kim SW. Recurrent secondary frosted branch angiitis after toxoplasmosis vasculitis. Acta Ophthalmol Scand. 2005;83(1):115-117. doi: 10.1111/j.1600-0420.2005.00399.x [DOI] [PubMed] [Google Scholar]
- 15. Kleiner RC, Kaplan HJ, Shakin JL, Yannuzzi LA, Crosswell HHJ, McLean WCJ. Acute frosted retinal periphlebitis. Am J Ophthalmol. 1988;106(1):27-34. [PubMed] [Google Scholar]
- 16. Markomichelakis NN, Barampouti F, Zafirakis P, Chalkiadakis I, Kouris T, Ekonomopoulos N. Retinal vasculitis with a frosted branch angiitis-like response due to herpes simplex virus type 2. Retina. 1999;19(5):455-457. doi: 10.1097/00006982-199919050-00019 [DOI] [PubMed] [Google Scholar]
- 17. Relhan N, Jalali S, Nalamada S, Dave V, Mathai A. Traumatic endophthalmitis presenting as isolated retinal vasculitis and white-centered hemorrhages: case report and review of literature. Indian J Ophthalmol. 2012;60(4):317-319. doi: 10.4103/0301-4738.98715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Subbiah S, McAvoy CE, Best JL. Retinal vasculitis as an early sign of bacterial post-operative endophthalmitis. Eye (Lond). 2010;24(8):1410-1411. doi: 10.1038/eye.2010.18 [DOI] [PubMed] [Google Scholar]