Abstract
Background
Medical accessibility is important in liver transplantation (LT) because of the risk of infections associated with the use of immunosuppressants and complications that require continuous treatment, such as biliary stenosis. However, the effect of medical accessibility on LT success rates has yet to be scrutinized. The aim of this retrospective observational study is to determine whether medical accessibility affects LT outcomes.
Material/Methods
We enrolled patients who had undergone LT at Samsung Medical Center between January 2017 and December 2021. The level of medical access was divided into 2 categories (difficult and easy) based on a cutoff of a 120-min commute on public transportation to access LT. Baseline characteristics were calibrated with propensity score matching. The outcomes (overall survival and graft survival) and severity of emergency center visits according to medical accessibility were also investigated.
Results
A total of 486 patients was included in this study. The median time to reach the hospital by public transportation was 135 min. Sex, Child-Pugh classification, Model for End-stage Liver Disease score, presence of hepatocellular carcinoma, and donor type were calibrated with propensity score matching, and each group consisted of 186 patients. The overall survival (88.3% vs 86.2%, P=0.67, 5-year) and graft survival (98.6% vs 95.4%, P=0.086, 5-year) showed no significant differences between the difficult-to-access and easy-to-access groups. While severity of emergency center visits differed between the difficult group (27.6%) and the easy group (15.5%), the difference was not statistically significant.
Conclusions
Medical access to LT did tend to increase emergency center presentation severity but did not affect long-term outcomes.
Keywords: Liver Transplantation, Survival Analysis, Access to Primary Care
Introduction
Medical care is an essential service for all populations, but it is often not provided equally due to differences in economic status and physical accessibility [1–4]. To address the problems generated by lack of medical equity, some jurisdictions are trying to expand their national insurance systems through social consensus, and telemedicine technologies are being introduced to mitigate disparities in physical access [5–10]. The application of technologies that address limitations in physical access is rapidly expanding, particularly due to the experience of the COVID-19 pandemic [11]. However, little attention has been paid to whether improvements in medical accessibility are necessary for all diseases and how physical accessibility affects patient outcomes.
Liver transplantation (LT), which has been considered a high risk-procedure since it was first described in 1963, is a widely accepted treatment for end-stage liver disease due to the development of immunosuppressants and advanced surgical techniques [12–14]. For LT patients, medical accessibility and close surveillance are important to maintaining graft function because immunosuppressants increase the risks of various infections, with low levels of immunosuppression leading to graft rejection [15,16]. However, no studies are available on the effects of medical accessibility and LT.
Moreover, although centralized care has been shown to lead to more favorable outcomes in LT [17], there are inherent limitations in terms of patient access to hospitals when transplant centers are centralized. In this context, patient access to hospitals may be an important determinant of centralization of LT centers. However, there is controversy regarding the effect of hospital distance on LT outcomes [18,19].
The aim of this study was to investigate whether medical accessibility affects LT outcomes of graft and patient survival and severity of emergency room presentation.
Material and Methods
A retrospective observational study was performed at Samsung Medical Center, Seoul, Korea. Patients who underwent first LT between January 2017 and December 2021 were included. Exclusion criteria were age ≤18 years; death or graft failure within 1 month after LT; no discharge from the hospital more than 1 month after LT; or simultaneous liver and kidney transplantation.
Primary outcomes were Overall Survival (OS) and graft survival according to medical accessibility. Graft failure was defined as death due to liver failure or re-LT. Death due to cancer progression was excluded from graft failure. Secondary outcomes were severity and number of emergency center visits according to medical accessibility. The severity of admission through emergency center visits was categorized into 2 grades (mild-to-moderate and severe). A mild-to-moderate visit was defined as one in which the patient required treatment with medication and endoscopic or radiologic intervention. A severe visit was defined one in which the patient required surgical treatment or admission to an intensive care unit, or death. Hospital stays after admission through an emergency center were also investigated for secondary outcomes.
Data Collection
Data on sex, body mass index (BMI), underlying disease (hypertension, diabetes mellitus), liver function, donor type, etiology of LT, presence of HCC, ABO incompatibility, and history of emergency center visits were investigated through electronic medical records. Liver function was evaluated using the Child-Pugh classification and Model for End-stage Liver Disease (MELD) scores [20,21].
Regarding postoperative course, all variables (presence and severity of complications and presence and number of rejections) were investigated through medical records. The presence and number of rejections were defined as biopsy-proven rejection, including acute cellular rejection, chronic rejection, and antibody-mediated rejection. The severity of complications was assessed with the Clavien-Dindo classification [22].
Measure of Medical Accessibility
Based on the home addresses of all patients, distance to the hospital, commute time using personal transportation, and commute time using public transportation were measured. The commute time using public transportation was measured with Google Maps (maps.google.com). The distance to the hospital and the commute time using personal transportation were measured with TMAP (TMAP Mobility Corporation, TMAP, version 9.9.4.291622). All measurements assumed a departure time of 9 a.m. on weekdays to account for traffic congestion.
Medical accessibility was divided into 2 groups based on a cutoff of 120 min on public transportation. Those who took less than 120 min to reach the hospital were assigned to the easy medical accessibility group, and those who took more than 120 min were assigned to the difficult medical accessibility group. The cutoff of 120 minutes was chosen based on the maximum value from a previous study that examined the average travel time to healthcare services by public transportation [23].
Propensity Score Matching
The 2 groups of patients (difficult vs easy medical accessibility) were not randomly selected, and because various variables could differ due to selection bias, PSM was performed. One-to-one PSM was performed using differences in baseline characteristics between the 2 groups. The variables in the PSM were sex, Child-Pugh classification, MELD score, presence of HCC, and donor type. Matching analyses were performed using R software, MatchIt package (The R Core Team, Vienna, Austria).
Statistical Analysis
Continuous variables with normal distribution are summarized with mean±standard deviation, and non-normal continuous variables are expressed as median (range). Fisher’s exact test or Pearson’s chi-square test was applied as appropriate to compare proportions between groups. Fisher’s exact test was specifically chosen when the expected frequency was less than 5. For comparison of continuous variables, normality testing was performed with Kolmogorov-Smirnov and Shapiro-Wilk tests (Supplementary Table 1). The t test was used when the normal distribution was followed, and the Mann-Whitney U test was used when the distribution did not follow normal distribution. In Mann-Whitney U testing, ties were managed by assigning the average rank to tied values. The Cox proportional hazards model was used to evaluate prognostic variables, and an estimated HR with a 95% confidence interval was presented. A Kaplan-Meier curve was applied to analyze OS and graft survival, and P<0.05 was considered statistically significant. All analyses were performed using R software (The R Core Team, Vienna, Austria).
Ethics Approval
The study protocol confirmed to the ethics guidelines of the Declaration of Helsinki and was approved by the Institutional Review Board of Samsung Medical Center (IRB No. SMC 2022-09-014).
Informed Consent
The need for informed consent was waived by the IRB of Samsung Medical Center due to the retrospective nature of the study.
Results
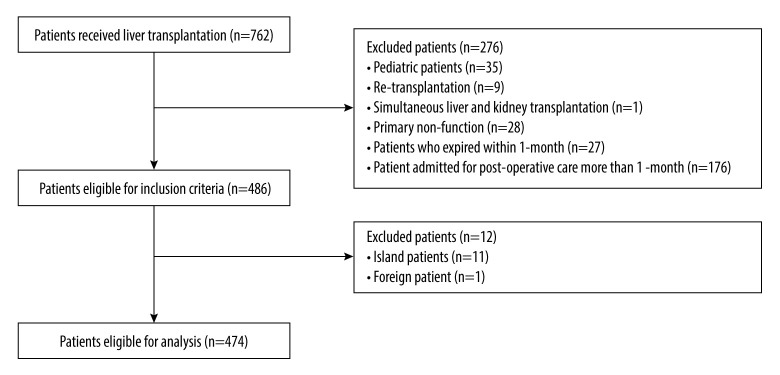
Among 762 patients considered for the study, 486 met the inclusion criteria. Twelve of these patients, for whom medical accessibility could not be investigated, were excluded, leaving 474 eligible for analysis. A flow diagram of the selection of patients included in the study is provided in Figure 1.
Figure 1.
A flow diagram of the selection criteria.
Distribution of Patients
The distance from a patient’s home to the hospital ranged from 29.2 km to 280.8 km, with a median value of 100 km. The median commute time of personal transportation was 92 min, ranging from 43 to 207 min, and the median commute time of public transportation was 135 min, ranging from 87 to 214 min. The distribution of all patients is illustrated in Figure 2.
Figure 2.
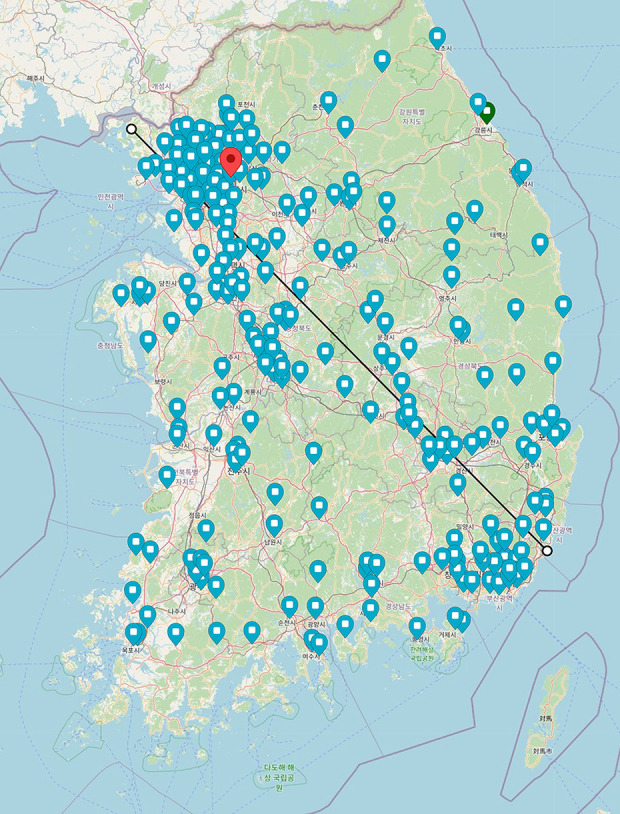
Distribution of all patients. The red dot indicates the location of Samsung Medical Center, and the green dots indicate the distribution of all patients. The black line represents the approximate size of Korea (369 km). The background map was sourced from openstreetmap.org, which provides maps as open source. This figure was created using Adobe Illustrator CC 2023, version 27.0.
Baseline Characteristics Before Propensity Score Matching
Based on the commute time using public transportation (120 min), 257 patients were classified into the difficult group and 217 into the easy group. A comparison of the characteristics of patients in the difficult and easy groups is summarized in Table 1.
Table 1.
Characteristics of patients.
| Medical accessibility | P value | Test | ||
|---|---|---|---|---|
| Difficult (n=257) | Easy (n=217) | |||
| Age (years) | 55.6±8.4 | 54.2±10.4 | 0.112 | |
| Sex, n (%) | ||||
| Male | 192 (74.7) | 142 (65.4) | 0.035* | Chi-square |
| Female | 65 (25.3) | 75 (34.6) | ||
| Body mass index | 24.2 [16.4, 35.5] | 24.4 [15.7, 36.7] | 0.970 | |
| Hypertension, n (%) | ||||
| No | 198 (77.0) | 183 (84.3) | 0.061 | Chi-square |
| Yes | 59 (23.0) | 34 (15.7) | ||
| Diabetes mellitus, n (%) | ||||
| No | 192 (74.7) | 164 (75.6) | 0.912 | Chi-square |
| Yes | 65 (25.3) | 53 (24.4) | ||
| Child-Pugh score, n (%) | ||||
| A | 115 (44.7) | 76 (35.0) | 0.002* | Chi-square |
| B | 73 (28.4) | 49 (22.6) | ||
| C | 69 (26.8) | 92 (42.4) | ||
| MELD, median (IQR) | 13.0 (8.0, 21.0) | 14.0 (9.0, 31.0) | 0.001* | |
| Time after LT, month, mean | 32.9±17.9 | 32.6±17.4 | 0.877 | |
| Transplantation-related factors | ||||
| Type of donor, n (%) | ||||
| Cadaver | 38 (14.8) | 51 (23.5) | 0.021* | Chi-square |
| Living | 219 (85.2) | 166 (76.5) | ||
| ABO-incompatible, n (%) | ||||
| No | 200 (77.8) | 172 (79.3) | 0.788 | Chi-square |
| Yes | 57 (22.2) | 45 (20.7) | ||
| Etiology | ||||
| HBV | 146 (56.8) | 114 (52.5) | 0.202 | Exact |
| HCV | 7 (2.7) | 5 (2.3) | ||
| Alcoholism | 64 (24.9) | 55 (25.3) | ||
| HBV with HCV | 1 (0.4) | 0 (0.0) | ||
| HBV with alcoholism | 8 (3.1) | 2 (0.9) | ||
| HBV with others | 1 (0.4) | 0 (0.0) | ||
| Others | 30 (11.7) | 41 (18.9) | ||
| Presence of hepatocellular carcinoma | ||||
| No | 91 (35.4) | 100 (46.1) | 0.023* | Chi-square |
| Yes | 166 (64.6) | 117 (53.9) | ||
| Postoperative course | ||||
| Complications, n (%) | ||||
| No | 131 (51.0) | 98 (45.2) | 0.242 | Chi-square |
| Yes | 126 (49.0) | 119 (54.8) | ||
| Complications, Clavien-Dindo classification, n (%) | ||||
| I | 5 (4.0) | 4 (3.0) | 0.973 | Exact |
| II | 56 (44.4) | 51 (42.9) | ||
| IIIa | 34 (27.0) | 31 (26.1) | ||
| IIIb | 31 (24.6) | 32 (26.9) | ||
| IV | 0 (0.0) | 1 (0.8) | ||
| Rejections, n (%) | ||||
| No | 221 (86.0) | 191 (88.0) | 0.606 | Chi-square |
| Yes | 36 (14.0) | 26 (12.0) | ||
| Number of rejections, n (%) | ||||
| None | 73 (67.0) | 61 (70.1) | 0.944 | Exact |
| 1 | 30 (27.5) | 23 (26.4) | ||
| 2 | 5 (4.6) | 3 (3.4) | ||
| 3 | 1 (0.9) | 0 (0.0) | ||
| Medical accessibility | ||||
| Distance from hospital in km, mean | 242.1±109.2 | 38.8±42.4 | <0.001* | |
| Time in minutes, mean | ||||
| Personal transportation | 183.8±68.2 | 48.4±32.0 | <0.001* | |
| Public transportation | 213.0±63.5 | 81.2±28.3 | <0.001* | |
| Visit the emergency center at least once | ||||
| No | 123 (47.9) | 76 (35.0) | 0.006* | Chi-square |
| Yes | 134 (52.1) | 141 (65.0) | ||
± – standard deviations; Exact – Fisher’s exact test; Chi-square – Pearson’s Chi-square test.
Significant values.
In the medical accessibility factors, distance from hospital was approximately 6 times longer in the difficult group (mean=242.1 vs 38.8), whereas the time in minutes was 3.7 times longer for personal transportation (mean=183.8 vs 48.4) and 2.6 times longer for public transportation (mean 213.0 vs 81.2) in the difficult group. Interestingly, in the difficult group, there was no association in travel time between personal transportation and public transportation. However, in the easy group, public transportation took about twice as long as personal transportation.
There were no associations in age (mean=55.6 vs 54.2, P=0.112), BMI (median=24.2 vs 24.4, P=0.970), hypertension (23.0% vs 15.7%, P=0.061), and diabetes mellitus (25.3% vs 24.4%, P=0.912) between the difficult and easy groups. However, significant associations were found for sex (male 74.7% vs 65.4, P=0.035), Child-Pugh score (A 44.7% vs 35.0%, P=0.002), and MELD score (median 13.0 vs 14.0, P=0.001).
In the transplantation-related factors and postoperative course, the difficult group included a larger proportion of living donors (P=0.021) and those with hepatocellular carcinoma (HCC) (P=0.023). No significant associations were evident in the proportions of ABO-incompatible patients, etiology of transplantation, and postoperative course.
Baseline Characteristics After Propensity Score Matching
Patients in the difficult group were successfully matched one-to-one with those in the easy group. Each group included 186 patients. The variables that showed significant differences before matching (sex, Child-Pugh classification, MELD score, presence of HCC, and donor type) were not ignificant after propensity score matching (PSM). A comparison of the characteristics of patients in the difficult and easy groups after PSM is summarized in Table 2.
Table 2.
Characteristics of patients after PS matching.
| Medical accessibility | P value | Test | ||
|---|---|---|---|---|
| Difficult (n=186) | Easy (n=186) | |||
| Age (years) | 55.5±9.0 | 54.1±10.0 | 0.167 | |
| Sex, n (%) | ||||
| Male | 132 (71.0) | 132 (71.0) | 1.000 | Chi-square |
| Female | 54 (29.0) | 54 (29.0) | ||
| Body mass index | 24.6 [22.2, 27.1] | 24.6 [22.3, 27.1] | 1.000 | |
| Hypertension, n (%) | ||||
| No | 144 (77.4) | 155 (83.3) | 0.192 | Chi-square |
| Yes | 42 (22.6) | 31 (16.7) | ||
| Diabetes mellitus, n (%) | ||||
| No | 136 (73.1) | 140 (75.3) | 0.722 | Chi-square |
| Yes | 50 (26.9) | 46 (24.7) | ||
| Child-Pugh score, n (%) | ||||
| A | 72 (38.7) | 76 (40.9) | 0.872 | Chi-square |
| B | 50 (26.9) | 46 (24.7) | ||
| C | 64 (34.4) | 64 (34.4) | ||
| MELD, median (IQR) | 14.0 (9.0, 26.0) | 13.0 (9.0, 26.5) | 0.726 | |
| Time after LT, month, mean | 32.4±17.8 | 32.6±17.4 | 0.888 | |
| Transplantation-related factors | ||||
| Type of donor, n (%) | ||||
| Cadaver | 34 (18.3) | 36 (19.4) | 0.894 | Chi-square |
| Living | 152 (81.7) | 150 (80.6) | ||
| ABO-incompatible, n (%) | ||||
| No | 148 (79.6) | 145 (78.0) | 0.800 | Chi-square |
| Yes | 38 (20.4) | 41 (22.0) | ||
| Etiology | ||||
| HBV | 89 (47.8) | 103 (55.4) | 0.367 | Exact |
| HCV | 6 (3.2) | 5 (2.7) | ||
| Alcoholism | 55 (29.6) | 45 (24.2) | ||
| HBV with HCV | 0 (0.0) | 0 (0.0) | ||
| HBV with alcoholism | 7 (3.7) | 2 (1.1) | ||
| HBV with others | 1 (0.5) | 0 (0.0) | ||
| Others | 28 (15.1) | 31 (16.7) | ||
| Presence of hepatocellular carcinoma | ||||
| No | 75 (40.3) | 78 (41.9) | 0.833 | Chi-square |
| Yes | 111 (59.7) | 108 (58.1) | ||
| Postoperative course | ||||
| Complications, n (%) | ||||
| No | 92 (49.5) | 87 (46.8) | 0.678 | Chi-square |
| Yes | 94 (50.5) | 99 (53.2) | ||
| Complications, Clavien-Dindo classification, n (%) | ||||
| I | 2 (2.1) | 4 (4.0) | 0.835 | Exact |
| II | 40 (42.6) | 45 (45.5) | ||
| III a | 28 (29.8) | 27 (27.3) | ||
| III b | 24 (25.5) | 22 (22.2) | ||
| IV | 0 (0.0) | 1 (1.0) | ||
| Rejections, n (%) | ||||
| No | 157 (84.4) | 162 (87.1) | 0.553 | Chi-square |
| Yes | 29 (15.6) | 24 (12.9) | ||
| Number of rejections, n (%) | ||||
| None | 54 (65.1) | 52 (68.4) | 0.901 | Exact |
| 1 | 23 (27.7) | 21 (27.6) | ||
| 2 | 5 (6.0) | 3 (3.9) | ||
| 3 | 1 (1.2) | 0 (0.0) | ||
| Medical accessibility | ||||
| Distance from hospital in km, mean | 226.9±107.9 | 40.0±44.8 | 0.001* | |
| Time in minutes, mean | ||||
| Personal transportation | 174.3±68.5 | 49.2±33.7 | 0.001* | |
| Public transportation | 202.5±58.3 | 80.3±28.6 | <0.001* | |
| Visit the emergency center at least once | ||||
| No | 91 (48.9) | 63 (33.9) | 0.004* | Chi-square |
| Yes | 95 (51.1) | 123 (66.1) | ||
± – standard deviations; Exact – Fisher’s exact test; Chi-square – Pearson’s Chi-square test.
Significant values.
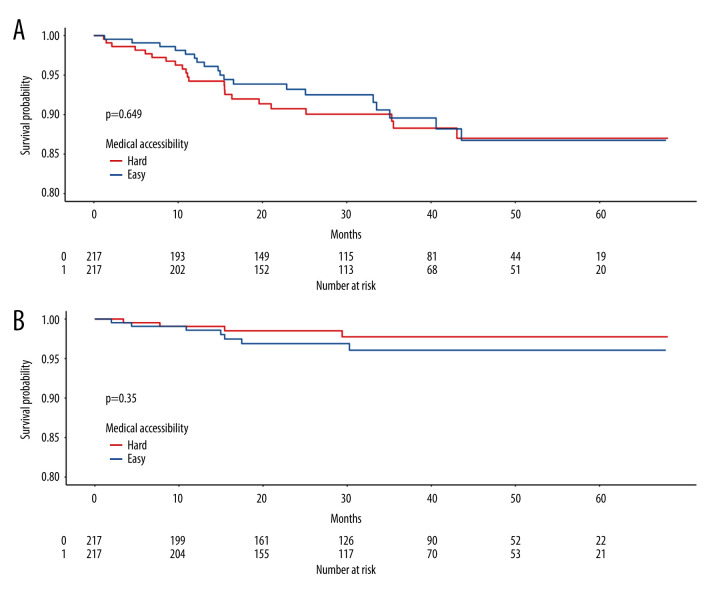
Medical Accessibility and Outcomes
Medical accessibility outcomes were analyzed with post-PSM data. In an analysis of primary outcomes, there were no significant differences in 5-year OS (88.3% vs 86.2%, P=0.67, 5-year) and 5-year graft survival (98.6% vs 95.4%, P=0.086, 5-year) between the difficult and easy groups (Figure 3).
Figure 3.
A Kaplan-Meier survival graph for each group of difficult and easy patients’ accessibility according to medical accessibility. (A) Overall survival. (B) Graft survival.
In an analysis of secondary outcomes, the proportions of severe patients (27.6% vs 15.5, P=0.057) and admission rates (91.6% vs 89.4%, P=0.763) were higher in the difficult group than in the easy group, but the difference was not statistically significant. However, the number of visits to emergency centers was higher in the easy group (P=0.001). Characteristics of patient visits to the emergency centers between the difficult and easy groups are summarized in Table 3. Among patients who visited an emergency room, the mean number of visits was higher in the easy group (1.5±2.4) than in the difficult group. (2.3±3.0), and the difference was statistically significant (P=0.001). Although lacking statistical significance, the difficult group (n=24, 27.6%) had a larger proportion of severe emergency center visits compared with the easy group (n=17, 15.5%, P=0.057).
Table 3.
Characteristics of patient visits to the emergency center.
| Medical accessibility | P value | Test | ||
|---|---|---|---|---|
| Difficult (n=95) | Easy (n=123) | |||
| Mean number of visits, n | 1.5±2.4 | 2.3±3.0 | 0.001* | |
| Need for admission | ||||
| No | 8 (8.4) | 13 (10.6) | 0.763 | Chi-square |
| Yes | 87 (91.6) | 110 (89.4) | ||
| Hospital days if admitted, median (IQR) | 11.0 (7.0, 24.5) | 16.0 (9.0, 23.0) | 0.406 | |
| Severity of admission | ||||
| Mild-to-moderate | 63 (72.4) | 93 (84.5) | 0.057 | Chi-square |
| Severe | 24 (27.6) | 17 (15.5) | ||
± – standard deviations; Chi-square – Pearson’s Chi-square test.
Significant values.
Analyses of Factors Affecting Overall Survival
In univariate analysis of factors affecting OS, visiting an emergency center at least once (hazard ratio [HR]=5.22, P=0.002) was the only factor associated with OS. To address the potential underestimation of omitted covariates [24], we performed a multivariate analysis that incorporated variables with P values <0.1 from the univariate analysis. The variables included HCV etiology (HR 3.16, P=0.068) and ABO incompatibility (HR 1.53, P=0.254). Visiting an emergency center at least once was the only statistically significant factor associated with OS in the multivariate analysis (HR=5.01, P=0.003). Details of analyses are summarized in Table 4.
Table 4.
Univariate and multivariate analyses of prognostic factors associated with overall survival.
| Variables | Univariate | Multivariate | ||
|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | |
| Gender, Male vs Female | 1.04 (0.5, 2.17) | 0.922 | ||
| Age | 1.00 (0.96, 1.03) | 0.789 | ||
| Body mass index | 0.95 (0.86, 1.04) | 0.278 | ||
| Child-Pugh score: ref.=A | ||||
| B | 0.44 (0.14, 1.33) | 0.144 | ||
| C | 1.34 (0.65, 2.75) | 0.423 | ||
| Etiology: ref.=HBV | ||||
| HCV | 3.17 (0.93, 10.76) | 0.065 | 3.16 (0.92, 10.88) | 0.068 |
| Alcoholism | 0.64 (0.26, 1.62) | 0.351 | ||
| Others | 1.3 (0.54, 3.12) | 0.553 | ||
| MELD | 1.02 (0.99, 1.05) | 0.154 | ||
| Hypertension Yes vs No | 0.56 (0.2, 1.59) | 0.275 | ||
| Diabetes mellitus Yes vs No | 0.77 (0.34, 1.77) | 0.537 | ||
| Type of donor, living vs cadaver | 0.68 (0.32, 1.45) | 0.316 | ||
| ABO-incompatible vs compatible | 1.82 (0.89, 3.73) | 0.103 | 1.53 (0.74, 3.19) | 0.254 |
| Hepatocellular carcinoma Yes vs No | 1.28 (0.64, 2.59) | 0.486 | ||
| Rejection Yes vs No | 1.45 (0.63, 3.33) | 0.381 | ||
| Complications Yes vs No | 1.29 (0.65, 2.53) | 0.467 | ||
| Distance, km | 1.00 (1.00, 1.00) | 0.679 | ||
| Time, min | ||||
| Personal transportation | 1.00 (0.99, 1.00) | 0.598 | ||
| Public transportation | 1.00 (1.00, 1.00) | 0.955 | ||
| Visit the emergency center at least once, Yes vs No | 5.22 (1.84, 14.83) | 0.002 | 5.01 (1.76, 14.26) | 0.003 |
Discussion
Rapid innovations in medicine over the past half-century allow humans to live longer and healthier lives [25–27]. Medical advances after the first solid organ transplantation in 1954 have led to new milestones in life extension. Now, research on xenotransplantation is being conducted, and the pace of its development is accelerating [28,29]. However, with the COVID-19 pandemic, the medical field faced an unprecedented situation of restrictions on activities and movement to prevent the spread of infection, greatly complicating traditional medical care.
Several studies on the relationship between transfer time and disease course have been published. However, most were limited to cardiovascular disease, for which early intervention is important [30–32]. In contrast, the present study focuses on medical accessibility and long-term outcomes of a specific medical procedure (LT).
Our results show that medical accessibility was not correlated with long-term prognosis in LT patients. LT patients require daily administration of immunosuppressants to prevent rejection. However, because immunosuppressants increase the risk of infection, appropriate drug concentrations must be chosen. For this reason, LT patients require constant hospital visits and close surveillance. This factor likely influenced the association between medical accessibility and prognoses. In addition, our center operates a patient hotline to help them quickly triage themselves to determine whether they need to visit the hospital. Because of this early triage, the impact of medical accessibility may have been underestimated.
Our results also indicate a trend towards higher severity of emergency department visits among patients with difficult medical accessibility. This suggests that even though our hospital’s hotline advises patients to visit the hospital when necessary, those with difficult medical accessibility may delay their visit until their condition worsens significantly. This indicates that despite receiving guidance from the hotline, practical barriers to accessing the hospital can lead to disease exacerbation. Therefore, while medical accessibility may not significantly impact long-term outcomes, it can have a substantial effect on emergency situations.
Several studies have been conducted on telemedicine in LT. For example, Koc et al reported that telemedicine-based remote monitoring after LT is eligible in patients with stable conditions [33]. Santonicola et al reported that telemedicine is promising in LT as it can reassure the patients and improve the quality of healthcare [34]. Research on such telemedicine is being conducted not only in LT but also in hepatology, and the demand for it is increasing [35]. In keeping with these changing times, it is expected that the results of the present study will be used as evidence to answer the question of ‘what can be obtained through telemedicine?’ for doctors who want to introduce telemedicine in LT.
Our prognostic factor analyses found that visiting an emergency center at least once was the only influential factor. There have been several analyses of prognostic factor in LT. Kim et al found that older recipient age and use of a cadaver donor were significantly associated with increased risk of death [36]. Patkowski et al reported that improved MELD score, ischemic time, and routine biliary drainage were associated with better long-term survival [37]. Because we excluded patients who died within 1 month after LT, selection bias may have affected the results. To better analyze how visiting an emergency center at least once affects OS, future research and additional data on reasons for visiting emergency centers and causes of death are needed.
There were some limitations in this study. First, as a single-center retrospective study with a small number of patients, its generalizability is limited. Second, the standard of medical accessibility was subjective (120 min) without clear references. Furthermore, medical accessibility is a concept that includes not only distance, but socio-economic factors, which were not evaluated here in any detail. Comprehensive and large-volume studies that include socio-economic factors, urbanization rates, and population densities are needed.
Additionally, the study did not address hematologic parameters, which are critical in monitoring patients with acute inflammation [38] Parameters related to inflammation, such as C-reactive protein (CRP) and prothrombin time (PT), provide essential insights into patient severity. Including these parameters in future research could enhance our understanding of the impact of medical accessibility.
However, our study did reveal that transportation time as calculated by commercial applications can be used in a medical study. This type of research can be applied to other fields and medical services. Although we did not find any differences in long-term outcomes of LT, the finding itself is valuable in the setting of Korea’s LT recipients. We found that, in Korea, medical accessibility, regardless of the distance traveled, is not critically different for patients with LT. Although the numbers of emergency center visits differed, the study’s failure to include the number of visits to other emergency centers near the patients’ homes should be considered.
Conclusions
In conclusion, several limitations exist in our study, such as not including factors like socio-economic status, availability of specialized care, patient mobility, and geographic features. However, our study indicates that, within the specific context of LT, medical accessibility may not be a predominant factor affecting long-term outcomes. On the other hand, the severity of emergency visits could be influenced by medical accessibility. Additionally, our study suggests that certain medical conditions, such as LT, may diverge from the pattern seen in conditions like cardiovascular diseases, where accessibility plays a more important role. Our research points to the potential for exploring alternative strategies beyond simply advocating for increased medical accessibility. These may include extending the follow-up period for patients, concentrating complex surgeries like LT in larger centers located farther from patients’ residences, and other innovative models tailored to the unique characteristics of each medical condition. This nuanced perspective calls for tailored healthcare strategies that recognize the distinctive needs of conditions like LT and the potential for distinct healthcare approaches compared to other medical conditions.
Data Availability
These data cannot be shared publicly because of legal reasons. Data are available from the Samsung Medical Center Institutional Data Access/Ethics Committee (contact via yhsky.jung@samsung.com) for researchers who meet the criteria for access to confidential data.
Supplementary Data
Supplementary Table 1.
Normality test.
| Medical accessibility | Kolmogorov-Smirnov | Shapiro-Wilk | |
|---|---|---|---|
| p value | p value | ||
| Pre-matching data | |||
| Age | Difficult | 0.037 | <0.001 |
| Easy | <0.001 | <0.001 | |
| BMI | Difficult | 0.046 | 0.025 |
| Easy | 0.200* | 0.101 | |
| Distance from hospital, km. | Difficult | <0.001 | <0.001 |
| Easy | <0.001 | <0.001 | |
| Time in minute, personal transportation, min. | Difficult | <0.001 | <0.001 |
| Easy | <0.001 | <0.001 | |
| Time in minute, public transportation, min. | Difficult | 0.004 | <0.001 |
| Easy | <0.001 | <0.001 | |
| Post-matching data | |||
| Age | Difficult | 0.011 | 0.002 |
| Easy | <0.001 | <0.001 | |
| BMI | Difficult | 0.200* | 0.413 |
| Easy | 0.200* | 0.284 | |
| Distance from hospital.km. | Difficult | 0.001 | <0.001 |
| Easy | <0.001 | <0.001 | |
| Time in minute, personal transportation, min. | Difficult | 0.002 | <0.001 |
| Easy | <0.001 | <0.001 | |
| Time in minute, public transportation, min. | Difficult | 0.001 | <0.001 |
| Easy | 0.004 | <0.001 | |
Acknowledgements
We acknowledge that part of this research was previously presented at the ATW 2022 conference (https://doi.org/10.4285/ATW2022.F-3060) and have obtained permission for its inclusion here from Clinical Transplantation and Research (Korean Journal of Transplantation) [39].
Abbreviations
- HCC
hepatocellular carcinoma
- LT
liver transplantation
- PSM
propensity score matching
- OS
overall survival
- MELD
Model for End-stage Liver Disease
- HR
hazard ratio
- IRB
Institutional Review Board
- BMI
body mass index
- HBV
hepatitis B virus
- HCV
hepatitis C virus
Footnotes
Conflict of interest: None declared
Publisher’s note: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher
Declaration of Figures’ Authenticity: All figures submitted have been created by the authors, who confirm that the images are original with no duplication and have not been previously published in whole or in part.
Financial support: This research was supported by the Basic Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science and ICT (NRF-2023R1A2C2005946) and Future Medicine 2030 Project of the Samsung Medical Center (#SMX1240051)
References
- 1.Gulliford M, Figueroa-Munoz J, Morgan M, et al. What does ‘access to health care’ mean? J Health Serv Res Policy. 2002;7(3):186–88. doi: 10.1258/135581902760082517. [DOI] [PubMed] [Google Scholar]
- 2.Nguyen KH, Wilson IB, Wallack AR, Trivedi AN. Racial and ethnic disparities in patient experience of care among nonelderly medicaid managed care enrollees. Health Aff (Millwood) 2022;41(2):256–64. doi: 10.1377/hlthaff.2021.01331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Burrows J. Inequalities and healthcare reform in Chile: Equity of what? J Med Ethics. 2008;34(9):e13. doi: 10.1136/jme.2007.022715. [DOI] [PubMed] [Google Scholar]
- 4.Gilbar R, Bar-Mor H. Justice, equality and solidarity: The limits of the right to health care in Israel. Med Law Rev. 2008;16(2):225–60. doi: 10.1093/medlaw/fwn003. [DOI] [PubMed] [Google Scholar]
- 5.Wherry L, Finegold K. Changes in health insurance coverage and health status by race and ethnicity, 1997–2002. J Natl Med Assoc. 2004;96(12):1577–82. [PMC free article] [PubMed] [Google Scholar]
- 6.Lee HO. Effect of four major severe diseases benefit expansion policies on the health care utilization and catastrophic health expenditure. Korean J Soc Welf. 2018;70(1):89–116. [Google Scholar]
- 7.Obama B. United States health care reform: Progress to date and next steps. JAMA. 2016;316(5):525–32. doi: 10.1001/jama.2016.9797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Loehrer AP, Song Z, Haynes AB, et al. Impact of health insurance expansion on the treatment of colorectal cancer. J Clin Oncol. 2016;34(34):4110–15. doi: 10.1200/JCO.2016.68.5701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Su D, Zhou J, Kelley MS, et al. Does telemedicine improve treatment outcomes for diabetes? A meta-analysis of results from 55 randomized controlled trials. Diabetes Res Clin Pract. 2016;116:136–48. doi: 10.1016/j.diabres.2016.04.019. [DOI] [PubMed] [Google Scholar]
- 10.Alajmi D, Almansour S, Househ MS. Recommendations for implementing telemedicine in the developing world. Stud Health Technol Inform. 2013;190:118–20. [PubMed] [Google Scholar]
- 11.Seshamani M. Medicare and telehealth: delivering on innovation’s promise for equity, quality, access, and sustainability. Health Affairs. 2022;41(5):651–53. doi: 10.1377/hlthaff.2022.00323. [DOI] [PubMed] [Google Scholar]
- 12.Verdonk RC, van den Berg AP, Slooff MJ, et al. Liver transplantation: An update. Neth J Med. 2007;65(10):372–80. [PubMed] [Google Scholar]
- 13.Yang LS, Shan LL, Saxena A, Morris DL. Liver transplantation: A systematic review of long-term quality of life. Liver Int. 2014;34(9):1298–313. doi: 10.1111/liv.12553. [DOI] [PubMed] [Google Scholar]
- 14.Yang J, Rhu J, Kwon J, et al. Hepatic venous territory mapping in living donor liver transplantation using right liver graft: An objective parameter for venous reconstruction. Ann Surg Treat Res. 2023;104(6):348–57. doi: 10.4174/astr.2023.104.6.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Halliday N, Westbrook RH. Liver transplantation: post-transplant management. Br J Hosp Med (Lond) 2017;78(5):278–85. doi: 10.12968/hmed.2017.78.5.278. [DOI] [PubMed] [Google Scholar]
- 16.Kochhar G, Parungao JM, Hanouneh IA, Parsi MA. Biliary complications following liver transplantation. World J Gastroenterol. 2013;19(19):2841–46. doi: 10.3748/wjg.v19.i19.2841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Edwards EB, Roberts JP, McBride MA, et al. The effect of the volume of procedures at transplantation centers on mortality after liver transplantation. N Engl J Med. 1999;341(27):2049–53. doi: 10.1056/NEJM199912303412703. [DOI] [PubMed] [Google Scholar]
- 18.Goldberg DS, French B, Forde KA, et al. Association of distance from a transplant center with access to waitlist placement, receipt of liver transplantation, and survival among US veterans. JAMA. 2014;311(12):1234–43. doi: 10.1001/jama.2014.2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Webb GJ, Hodson J, Chauhan A, et al. Proximity to transplant center and outcome among liver transplant patients. Am J Transplant. 2019;19(1):208–20. doi: 10.1111/ajt.15004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pugh RN, Murray-Lyon IM, Dawson JL, et al. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60(8):646–49. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 21.Kamath PS, Kim WR Advanced Liver Disease Study Group. The model for end-stage liver disease (MELD) Hepatology. 2007;45(3):797–805. doi: 10.1002/hep.21563. [DOI] [PubMed] [Google Scholar]
- 22.Bolliger M, Kroehnert JA, Molineus F, et al. Experiences with the standardized classification of surgical complications (Clavien-Dindo) in general surgery patients. Eur Surg. 2018;50(6):256–61. doi: 10.1007/s10353-018-0551-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee S. Spatial and socioeconomic inequalities in accessibility to healthcare services in South Korea. Healthcare (Basel) 2022;10(10):2049. doi: 10.3390/healthcare10102049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bretagnolle J, Huber-Carol C. Effects of omitting covariates in Cox’s model for survival data. Scand J Stat. 1988;15(2):125–38. [Google Scholar]
- 25.Weon BM, Je JH. Trends in scale and shape of survival curves. Sci Rep. 2012;2(1):504. doi: 10.1038/srep00504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Acemoglu D, Johnson S. Disease and development: The effect of life expectancy on economic growth. J Polit Econ. 2007;115(6):925–85. [Google Scholar]
- 27.Roser M, Ortiz-Ospina E, Ritchie H. Life Expectancy. OurWorldInData.org. 2013. Updated 2019. [cited 2022 July 7]. Available from: https://ourworldindata.org/life-expectancy.
- 28.Linden PK. History of solid organ transplantation and organ donation. Crit Care Clin. 2009;25(1):165–84,ix. doi: 10.1016/j.ccc.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 29.Lu T, Yang B, Wang R, Qin C. Xenotransplantation: Current status in preclinical research. Front Immunol. 2019;10:3060. doi: 10.3389/fimmu.2019.03060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Izumisawa Y, Endo H, Ichihara N, et al. Association between prehospital transfer distance and surgical mortality in emergency thoracic aortic surgery. J Thorac Cardiovasc Surg. 2022;163(1):28–35e1. doi: 10.1016/j.jtcvs.2020.03.043. [DOI] [PubMed] [Google Scholar]
- 31.Meuli L, Zimmermann A, Menges AL, et al. Helicopter emergency medical service for time critical interfacility transfers of patients with cardiovascular emergencies. Scand J Trauma Resusc Emerg Med. 2021;29(1):168. doi: 10.1186/s13049-021-00981-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oh S, Hyun DY, Cho KH, et al. Long-term outcomes in ST-elevation myocardial infarction patients treated according to hospital visit time. Korean J Intern Med. 2022;37(3):605–17. doi: 10.3904/kjim.2021.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Koc Ö M, Pierco M, Remans K, et al. Telemedicine based remote monitoring after liver transplantation: Feasible in a select group and a more stringent control of immunosuppression. Clin Transplant. 2022;36(1):e14494. doi: 10.1111/ctr.14494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Santonicola A, Zingone F, Camera S, et al. Telemedicine in the COVID-19 era for liver transplant recipients: An Italian lockdown area experience. Clin Res Hepatol Gastroenterol. 2021;45(3):101508. doi: 10.1016/j.clinre.2020.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Piao C, Terrault NA, Sarkar S. Telemedicine: An evolving field in hepatology. Hepatol Commun. 2019;3(5):716–21. doi: 10.1002/hep4.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim JM, Kim DG, Kim J, et al. Outcomes after liver transplantation in Korea: Incidence and risk factors from Korean transplantation registry. Clin Mol Hepatol. 2021;27(3):451–62. doi: 10.3350/cmh.2020.0292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patkowski W, Zieniewicz K, Skalski M, Krawczyk M. Correlation between selected prognostic factors and postoperative course in liver transplant recipients. Transplant Proc. 2009;41(8):3091–102. doi: 10.1016/j.transproceed.2009.09.038. [DOI] [PubMed] [Google Scholar]
- 38.Baranovskii DS, Klabukov ID, Krasilnikova OA, et al. Prolonged prothrombin time as an early prognostic indicator of severe acute respiratory distress syndrome in patients with COVID-19 related pneumonia. Curr Med Res Opin. 2021;37(1):21–25. doi: 10.1080/03007995.2020.1853510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jo SJ, Rhu J, Joh J, et al. Medical accessibility and outcomes in liver transplantation. Clin Transplant Res. 2022;36:180. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table 1.
Normality test.
| Medical accessibility | Kolmogorov-Smirnov | Shapiro-Wilk | |
|---|---|---|---|
| p value | p value | ||
| Pre-matching data | |||
| Age | Difficult | 0.037 | <0.001 |
| Easy | <0.001 | <0.001 | |
| BMI | Difficult | 0.046 | 0.025 |
| Easy | 0.200* | 0.101 | |
| Distance from hospital, km. | Difficult | <0.001 | <0.001 |
| Easy | <0.001 | <0.001 | |
| Time in minute, personal transportation, min. | Difficult | <0.001 | <0.001 |
| Easy | <0.001 | <0.001 | |
| Time in minute, public transportation, min. | Difficult | 0.004 | <0.001 |
| Easy | <0.001 | <0.001 | |
| Post-matching data | |||
| Age | Difficult | 0.011 | 0.002 |
| Easy | <0.001 | <0.001 | |
| BMI | Difficult | 0.200* | 0.413 |
| Easy | 0.200* | 0.284 | |
| Distance from hospital.km. | Difficult | 0.001 | <0.001 |
| Easy | <0.001 | <0.001 | |
| Time in minute, personal transportation, min. | Difficult | 0.002 | <0.001 |
| Easy | <0.001 | <0.001 | |
| Time in minute, public transportation, min. | Difficult | 0.001 | <0.001 |
| Easy | 0.004 | <0.001 | |
Data Availability Statement
These data cannot be shared publicly because of legal reasons. Data are available from the Samsung Medical Center Institutional Data Access/Ethics Committee (contact via yhsky.jung@samsung.com) for researchers who meet the criteria for access to confidential data.