Abstract
Background
This study aimed to explore the relationship between ultra-processed foods (UPFs) consumption and gut microbiota in patients with type 2 diabetes (T2D).
Methods
This cross-sectional study included 362 participants with T2D. UPFs consumption was assessed using a brief-type self-administered diet history questionnaire, quantified as the density of UPFs intake (g/1000 kcal). Gut microbial composition was evaluated via 16S rRNA gene sequencing. We investigated the association between gut microbiota, previously identified as relevant to T2D, and the density of UPFs intake using Spearman rank correlation coefficients. Multiple regression analysis, adjusting for age, sex, BMI, smoking status, exercise, and medication use, was conducted to further investigate these associations.
Results
The mean age of participants was 68 (63–74) years. The density of UPFs intake showed significant associations with Bifidobacterium (r = 0.11, p = 0.031), Lactobacillus (r = 0.11, p = 0.046), Ruminococcus (r = −0.12, p = 0.019), Roseburia (r = 0.11, p = 0.045). After adjusting for covariates in multiple regression analysis, Ruminococcus and Roseburia showed modest negative (β = −0.11, p = 0.038) and positive (β = 0.12, p = 0.033) correlations, with the density of UPFs intake among participants with T2D, respectively.
Conclusions
The density of UPFs intake was modestly inversely associated with Ruminococcus among patients with T2D and modestly positively associated with Roseburia.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12986-024-00884-y.
Keywords: Ultra-processed food consumption, Gut microbiota, Type 2 diabetes
Background
The growing prevalence of Type 2 diabetes (T2D) is a significant public health concern [1]. It is a chronic disease requiring long-term management, and the global healthcare expenditures related to diabetes have been projected to increase from 2015 to 2030 [2]. Over the past few decades, pharmacological therapy has improved care for patients with T2D [3]; however, nutrition therapy has lagged behind other areas of diabetes research [4].
The global consumption of ultra-processed foods (UPFs) has been rising over recent years [5, 6]. UPFs are industrially manufactured formulations that contain minimal or no whole foods and are composed primarily of industrially-produced ingredients and additives [7]. Consumption of UPFs is associated with increased risk of T2D diabetes, hypertension, cardiovascular disease and all-cause mortality [8–10]. While Visioli et al. [11] showed that not all UPFs are associated with adverse health outcomes, excessive intake of UPFs as a proportion of total energy intake can contribute to health issues. Therefore, the increasing share of UPFs in our diets can raise serious concern for public health, and further research of UPFs is needed.
Diet influences the stability, functionality, and diversity of the gut microbiome [12], which has impacts on metabolism and immune function [13]. Therefore, elucidating the relationship between the gut microbiome and metabolism is essential to prevent diet-related health disorders. Atzeni et al. [14] previously reported a positive correlation between consumption of UPFs and Alloprevotella, Negativibacillus, Prevotella, Sutterella, which have been associated with inflammatory gastro-intestinal diseases among the patients with overweight or obesity. Additionally, Martinez et al. [15] proposed gut microbiota dysbiosis as a potential clinical marker for neuroinflammation and cognitive decline related to UPFs consumption. These findings highlight the importance of gut microbiota alterations in understanding the mechanisms of various health complications and underscore the need for further investigation in light of rising global UPFs consumption trends.
Previously, we highlighted the dysbiosis among patients with T2D and identified dominant gut microbial genera in Japanese patients with T2D [16]. While several studies have suggested that consumption of UPFs increases the risk of diabetes [17, 18], it remains unclear whether UPFs consumption is associated with gut dysbiosis in the patients with T2D.
In the present study, we investigated the association between gut microbiota and UPFs consumption for Japanese patients with T2D.
Methods
Study participants and data collection
This study received approval from the ethics committee of the Kyoto Prefectural University of Medicine (no. ERB-C-534 and no. RBMR-E-466-5), and adhered to the principles of the Declaration of Helsinki. Written informed consent was obtained from all participants prior to enrollment. From November 2016 to December 2017, a total of 523 individuals with available data on gut microbiota from fecal samples were included. This cohort excluded those who had used medications for antibiotics in the past 3 months, those with type 1 diabetes or other forms of diabetes, those without diabetes, and those lacking data of daily energy intake.
Data on medications for dyslipidemia, hypertension, diabetes, and usage of proton pump inhibitors were collected. T2D was diagnosed according to previously reported criteria [19]. Data on body weight (kg), height (cm), body mass index (BMI) (kg/m2), family history of diabetes and duration of diabetes (years) were recorded for all participants.
Smoking status was determined through a question asking, "Do you currently smoke?" with response choices "yes" or "no." Those who answered "yes" were classified as "smokers," and those who answered "no" as "non-smokers." Consequently, individuals with a history of smoking but who had quit were also categorized as "non-smokers" in this study. Regular exercisers were defined as those who played some type of sport more than once a week [20]. In addition, the participants who drank alcohol daily were defined as drinkers.
Serum creatine (mg/dl), hemoglobin A1c (mmol/mol), fasting plasma glucose (mg/dl), and C-peptide levels (ng/ml) were evaluated using blood samples. The glomerular filtration rate (mL/min/1.73 m2) was estimated according to the estimation recommended by Japanese Society of Nephrology [21]. C-peptide immunoreactivity index and secretory units of islets in transplantation index were used to evaluate insulin secretion capacity. [22]
Dietary habits were evaluated via a brief-type self-administered diet history questionnaire (BDHQ) [23]. The detail of the BDHQ were fully described elsewhere [24]. In this study, the daily consumption of UPFs (g/day) was evaluated based on dietary intake derived from the BDHQ [25]. The estimation of UPFs was conducted by applying the weight ratios (for example, the weight ratio for “egg” was 4.4%, while for “udon”, it was 7.1%) of each UPFs reported for 147 food codes in prior research by Shinozaki et al. [25] to the weights of individual food items calculated using the BDHQ. Shinozaki et al. [25] pointed out that some food groups in the BDHQ are composed of different food codes. To avoid misestimation in the calculation of UPFs, Shinozaki et al. [25] did not estimate UPFs intake by categorizing each food item in the BDHQ as UPFs or non-UPFs. Instead, they assigned each food code a probability of UPFs, defined as a weight ratio. Based on nutrient density, daily UPFs intake was adjusted for total daily energy intake [26]. Specifically, the total daily amount of UPFs intake per 1000 kcal was calculated, defined as the density of UPFs intake (g/1000 kcal).
Sampling, DNA extraction, sequencing and data analysis
The detailed methods for fecal sample collection and analysis of gut bacterial composition were published elsewhere [27–29]. Briefly, according to the manufacturer's instructions, genomic deoxyribonucleic acid (DNA) was extracted using the Nucleospin Microbial DNA kit (Macherey-Nagal, Düren, Germany) and purified through the Agencourt AMPure XP (Beckman Couler, Brea, CA, USA) from collected stool samples (fecal collection kit; Techno Suruga lab, Shizuoka, Japan).
We used 16S ribosomal ribonucleic acid (rRNA) metagenomic sequencing to analyze DNA. Sequence libraries from purified DNA samples were generated using a two-step polymerase chain reaction (PCR), with detailed methods available in a previous publication [16], and these libraries were sequenced for 250 paired-end bases using the MiSeq Reagent v3 kit. This process was performed using the MiSeq platform (Illumina, San Diego, CA, USA) at the Biomedical Center at Takara Bio (Shiga, Japan).
The DADA2 plugin within Quantitative Insights Into Microbial Ecology 2 (QIIME2) version 2019.4 was used to generate amplicon sequence variant (ASV) tables, with quality and chimeric variant filtering applied [30]. Taxonomy assignment for each ASV was performed using the Sklearn classifier algorithm with Greengenes database version 13_8 (99% OTU dataset). A total of 6,902 ASVs were identified, excluding five ASVs with a Nearest Sequenced Taxon Index greater than 2.
Statistical analysis
In the previous study, we identified the predominant gut microbial genera among Japanese patients with T2D, with methodology detailed in another publication. [16]
Categorical variables were expressed as numbers and summarized as percentages. Continuous variables were shown as the mean (standard deviations; SD) if normally distributed, as the median (25th, 75th quartile) if not normally distributed. Spearman rank correlation coefficient was used to analyze the association between the density of UPFs intake and the gut microbial composition. Subsequently, multiple regression analysis was performed to calculate the partial regression coefficients (β) and p-values of Bifidobacterium, Lactobacillus, Ruminococcus, Roseburia, as these were significantly correlated with the density of UPFs intake. The analysis was adjusted for age, sex, BMI, smoking status, exercise, use of biguanide, alpha-glucosidase inhibitors, potassium-competitive acid blocker, or other proton pump inhibitors. The statistical analyses were performed using JMP Pro 17.2.0 (SAS, Cary, NC, USA). Statistical significance was defined as p < 0.05.
Results
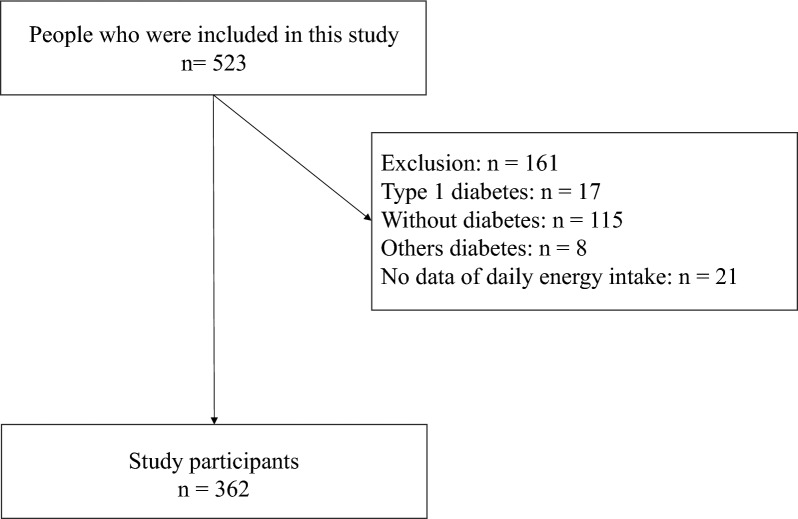
Ultimately, all of 362 participants with T2D were included, and 161 participants were excluded, as shown in Fig. 1 (those with type 1 diabetes; n = 17, those without diabetes; n = 115, those with other diabetes; n = 8, those with missing daily energy intake data; n = 21). The baseline characteristics of the participants are presented in Table 1. In this study, 199 men and 163 women were included. The mean age was 68 (63–74) years, and the mean BMI was 23.7 (21.5–26.2) kg/m2.
Fig. 1.
Flow diagram for the registration of participants
Table 1.
Characteristic of study participants
| N | ALL n = 362 |
|---|---|
| Age, years | 68 (63–74) |
| Men, % (n) | 55.0 (199) |
| Duration of diabetes, years | 13 (6–20) |
| Family history of diabetes, % (n) | 45.0 (163) |
| Height, cm | 160.9 (9.1) |
| Body weight, kg | 61.2 (55–69) |
| Body mass index, kg/m2 | 23.7 (21.5–26.2) |
| Systolic blood pressure, mmHg | 132 (122–144) |
| Diastolic blood pressure, mmHg | 78 (71–85) |
| Use of antihypertensive drugs, % (n) | 53.6 (194) |
| Hypertension, % (n) | 53.0 (192) |
| Use of Insulin, % (n) | 24.3 (88) |
| Use of SGLT-2 inhibitors, % (n) | 16.3 (59) |
| Use of GLP-1 agonist, % (n) | 16.0 (58) |
| Use of Biguanide, % (n) | 41.2 (149) |
| Use of Alpha-Glucosidase inhibitors, % (n) | 12.7 (46) |
| Use of Sulfonylurea, % (n) | 23.2 (84) |
| Use of DPP-4 inhibitors, % (n) | 52.2 (189) |
| Use of Thiazolidine, % (n) | 3.9 (14) |
| Use of P-CAB or PPI, % (n) | 7.2 (26) |
| Smoker, % (n) | 14.4 (52) |
| Exerciser, % (n) | 48.9 (177) |
| Drinker, % (n) | 67.4 (244) |
| HbA1c, mmol/mol | 53.5 (48.6–60.6) |
| Plasma glucose, mg/dL | 137 (116–166) |
| C-peptide, ng/mL | 1.6 (1.1–2.5) |
| C-peptide index | 1.1 (0.8–1.5) |
| Serum creatine, mg/dl | 0.7 (0.6–0.9) |
| eGFR, mL/min/1.73 m2 | 69.5 (19.4) |
Data were presented as mean (standard deviation, or percentage) if normally distributed and median (25% quartile-75% quartile) if not normally distributed, or absolute number
SGLT-2, Sodium-glucose cotransporter 2; GLP-1, glucagon-like peptide 1; DPP-4, dipeptidyl peptidase 4; P-CAB, potassium-competitive acid blocker; and PPI, proton pump inhibitors
In addition, the habitual dietary intake data of study participants are shown in Table 2. The mean energy intake was 29.1 (23.8–35.6) kcal/kg IBW/day. The total intake of UPFs was 217.6 (154.3–311.1) g/day, and the density of UPFs intake was 131.8 (101.2–184.7) g/1000 kcal.
Table 2.
Habitual diet intake of study participants
| All n = 362 | |
|---|---|
| Total energy intake, kcal/day | 1663.2 (1320.9–2058.7) |
| Energy intake, kcal/kg IBW/day | 29.1 (23.8–35.6) |
| Total protein intake, g/day | 66.8 (54.9–85.4) |
| Protein intake per energy intake, % | 16.3 (14.3–18.9) |
| Animal protein intake, g/day | 40.7 (29.9–54.1) |
| Vegetable protein intake, g/day | 26.9 (21.3–33.0) |
| Total Fat intake, g/day | 51.6 (39.7–65.6) |
| Fat intake per energy intake, % | 28.6 (6.3) |
| Total Carbohydrate intake, g/day | 213.1 (161.7–259.0) |
| Carbohydrate intake per energy intake, % | 50.8 (8.8) |
| Ultra-processed food intake, g/day | 217.6 (154.3–311.1) |
| Density of UPFs intake, g/1000kal | 131.8 (101.2–184.7) |
Data were presented as mean (standard deviation, or percentage) if normally distributed and median (25% quartile-75% quartile) if not normally distributed, or absolute number. Density of UPFs intake, daily Ultra-processed foods intake per daily total energy intake
IBW, ideal body weight,
In Table 3, we present the correlation between the density of UPFs intake and the gut microbiota composition in participants with T2D. Our findings showed that the density of UPFs intake was positively associated with Bifidobacterium (r = 0.11, p = 0.031), Lactobacillus (r = 0.11, p = 0.046), Roseburia (r = 0.11, p = 0.045), while a negative correlation was observed with Ruminococcus (r = −0.12, p = 0.019). We performed multiple regression analysis for the four types of gut microbiota mentioned above (Table 4). Then, Ruminococcus and Roseburia respectively showed an association with the density of UPFs intake, after adjusting covariates (age, sex, BMI, smoking status, exercise, use of biguanide, use of alpha-glucosidase and/or inhibitors, use of potassium-competitive acid blocker or proton pump inhibitors). Additionally, we revealed the link between Ruminococcus and UPFs intake alone (g/day) for patients with T2D, as shown in Table S1 (β = −0.12, p = 0.026).
Table 3.
Correlation coefficient between the gut microbiota and the density of UPFs intake
| Genera | r | p-value |
|---|---|---|
| p_Bacteroidetes f_Bacteroidaceae g_Bacteroides | − 0.03 | 0.622 |
| p_Actinobacteria f_Bifidobacteriaceae g_Bifidobacterium | 0.11 | 0.031* |
| p_Firmicutes f_Ruminococcaceae g_Faecalibacteriumu | − 0.08 | 0.125 |
| p_Bactereroidetes f_Prevptellaceae g_Prevotella | 0.01 | 0.802 |
| p_Actinobacteria f_Coriobacteriaceae g_Collinsella | 0.10 | 0.059 |
| p_Firmicutes f_Lactobacillaceae g_Lactobacillus | 0.11 | 0.046* |
| p_Firmicutes f_Streptococcaceae g_Streptococcus | 0.02 | 0.649 |
| p_Firmicutes f_Lachnospiraceae g_Blautia | − 0.001 | 0.981 |
| p_Firmicutes f_Ruminococcaceae g_Ruminococcus | − 0.12 | 0.019* |
| p_Firmicutes f_Veillonellaceae g_Megamonas | 0.07 | 0.161 |
| p_Firmicutes f_Lachnospiraceae g_[Ruminococcus] | 0.02 | 0.773 |
| p_Bacteroidetes f_Porphyromonadaceae g_Parabacteroides | 0.02 | 0.657 |
| p_Firmicutes f_Lachnospiraceae g_Roseburia | 0.11 | 0.045* |
| p_Firmicutes f_Lachnospiraceae g_Other | − 0.05 | 0.370 |
| p_Firmicutes f_Lachnospiraceae g_Dorea | − 0.05 | 0.367 |
| p_Firmicutes Unclassfied f_Lachnospiraceae | 0.02 | 0.764 |
| p_Firmicutes f_Lachnospiraceae g_Lachnospira | − 0.05 | 0.301 |
| p_Firmicutes f_Erysipelotrichaceae g_[Eubacterium] | 0.02 | 0.729 |
*significant at p < 0.05
Table 4.
Univariate and multiple regression analysis on the density of UPFs intake (g/1000 kcal)
| g_Bifidobacterium | g_Lactobacillus | g_Ruminococcus | g_Roseburia | |||||
|---|---|---|---|---|---|---|---|---|
| β | p-value | β | p-value | β | p-value | β | p-value | |
| Age | − 0.12 | 0.020* | 0.03 | 0.633 | 0.13 | 0.027* | 0.04 | 0.480 |
| Sex | − 0.05 | 0.307 | 0.04 | 0.406 | − 0.03 | 0.579 | − 0.04 | 0.518 |
| BMI | 0.07 | 0.177 | − 0.04 | 0.401 | − 0.08 | 0.164 | 0.12 | 0.030* |
| Smoking status | 0.02 | 0.618 | 0.02 | 0.654 | − 0.0002 | 0.997 | − 0.05 | 0.371 |
| Exercise | 0.004 | 0.931 | 0.03 | 0.458 | 0.01 | 0.848 | 0.08 | 0.132 |
| Use of BG | 0.05 | 0.328 | 0.09 | 0.077 | 0.04 | 0.433 | − 0.05 | 0.379 |
| Use of α-GI | − 0.48 | < 0.0001** | − 0.47 | < 0.0001** | 0.16 | 0.0029** | 0.15 | 0.003** |
| Use of P-CAB or PPI | 0.007 | 0.886 | − 0.16 | 0.0005** | − 0.04 | 0.494 | 0.03 | 0.584 |
| Density of UPFs intake | 0.06 | 0.249 | − 0.01 | 0.791 | − 0.11 | 0.038* | 0.12 | 0.033* |
| Density of UPFs intake (Crude) | 0.09 | 0.071 | 0.02 | 0.717 | − 0.16 | 0.003** | 0.10 | 0.071 |
Density of UPFs intake, daily Ultra-processed foods intake per daily total energy intake; Multivariate regression analysis was adjusted age, sex, BMI, smoking status, exercise, use of BG, use of α-GI, Use of P-CAB or PPI and Density of UPFs intake (g/1000 kcal)
BMI, Body mass index; BG, biguanide; α-GI, alfa-glucosidase inhibitors; P-CAB, potassium-competitive acid blocker; PPI, proton pump inhibitors; UPFs, ultra-processed foods
**significant at p < 0.01; * significant at p < 0.05
Discussion
Our major finding was that Ruminococcus and Roseburia were associated with the density of UPFs intake for patients with T2D. The density of UPFs intake was negatively associated with Ruminococcus, and positively associated with Roseburia for these patients.
Previously, Qin et al. [31] described gut microbial dysbiosis in Asian populations with T2D, and Karlsson et al. [32] reported similar findings for European populations. Specifically, T2D is characterized by a reduction in butyrate-producing microbes (e.g., Ruminococcus, Roseburia, and Faecalibacterium prausnitzii), which results in the promotion of inflammation in the gut [33]. However, among the participants with T2D in our study, we showed negative correlation between the density of UPFs and Ruminococcus, while Roseburia showed a positive correlation with the density of UPFs. Previous research has shown that UPFs consumption is associated with an increased risk of developing T2D [17], and our findings diverge slightly from the typical gut microbiota profile in these patients. This discrepancy could be attributed to the age of our study participants, with a mean age of 68 years. Park et al. [34] reported an increase in Roseburia with aging among Japanese participants, suggesting that the higher proportion of older participants in our study could have influenced our results.
Dietary therapy can significantly contribute to the management of diabetes, as well as exercise and pharmacotherapy. Xu et al. [35] demonstrated that dietary therapy positively impacted metabolic profiles in patients with T2D and this may be mediated through effects on the gut microbiota. Additionally, Zinöcker et al. [36] suggested the potential effects of UPFs on gut microbiota. Previous research indicated a positive association between Ruminococcus and carbohydrate intake [37], while carbohydrate intake and dietary fiber intake were negatively associated with UPFs intake [38]. This suggests that carbohydrate, including dietary fiber, may exert a significant influence on the negative correlation between Ruminococcus and UPFs consumption observed in the present study. Additionally, Roseburia has been reported to be more abundant in patients with T2D following low-carbohydrate dietary interventions that include dietary fiber, compared to those following low-fat diets [39]. Therefore, carbohydrates, including dietary fiber, may contribute to the positive association between Roseburia and UPFs, considering the inverse relationship between carbohydrate intake and UPFs. [38]
One of the characteristic ingredients of UPFs is emulsifiers [40]. UPFs containing emulsifiers have been reported to affect the gut microbiota [41], and Salame et al. [42] showed an association between exposure to dietary emulsifiers and T2D. Previous research by Holder et al. [43] demonstrated that dietary emulsifiers induced chronic intestinal inflammation and a reduction in Ruminococcus, using female mice. Furthermore, Chassaing et al. [44] showed a reduction in Ruminococcus among healthy participants who consumed dietary emulsifiers. This finding suggests that the consumption of dietary emulsifiers may be involved in the negative correlation between UPFs consumption and Ruminococcus, as observed in this study.
It is also important to recognize that foods possess various physiological effects beyond the quantification of UPFs, influenced by specific components such as dietary fiber, polyphenols, and probiotic/prebiotic intake. Since polyphenol and probiotic/prebiotic intake cannot be evaluated by BDHQ, we investigated the association between dietary fiber intake and Ruminococcus or Roseburia and found no relationship between dietary fiber intake and Ruminococcus (r = −0.0008, p = 0.988) or Roseburia (r = −0.05, p = 0.338). Therefore, although the evaluation of UPFs is critical in clinical practice, we should consider the food components when designing the dietary intervention, even though no significant correlation was found with dietary fiber.
The high intake of UPFs has been associated with increased risk for various adverse health outcomes [10], including T2D [42] and mortality risk [45], as UPFs consumption has been increasing globally [46]. Martini et al. [47] showed that up to 80% of total calorie intake was derived from UPFs consumption, primarily from sweets and sugar-containing beverages in the United States and Canada. However, a reduction in UPFs consumption has been reported to potentially reduce cardiovascular diseases [48], and Walker et al. [49] reported that lifestyle interventions reduced UPFs consumption, impacting treatment and prevention of metabolic syndrome. Therefore, the reduction in UPFs consumption is necessary worldwide in the future [50]. Moreover, further investigation is required to explore the effects of reducing UPFs consumption on the gut microbiota.
The limitations of this study are outlined below. First, the current study did not demonstrate a causal relationship between UPFs consumption and the gut microbiota. Secondly, our study included only Japanese patients, and the influence of ethnicity and race remains consideration. The gut microbiota composition has been reported to vary among different races and ethnicities [51], and the caution is warranted when generalizing our findings. Thirdly, the multiple regression analysis conducted in the current study did not include comorbidities, dietary fiber intake, probiotic consumption, or supplement use as covariates, and these factors may represent potential limitations. Even after adjusting for all these factors in the regression analysis, residual confounding may still exist. Fourth, in the multiple regression analysis of the current study, the association between UPFs and Ruminococcus or Roseburia demonstrated relatively small β-values, with p-values nearing the 0.05 threshold. These findings could be influenced by either confounding factors or the sample size. Notably, the relatively small sample size in our study could have contributed to instability of the β estimates. Therefore, future studies with larger sample sizes are warranted to provide more robust conclusions. Fifth, the total amount of physical activity was not assessed for participants categorized as exercising. Sixth, in our study, we estimated UPFs intake from the BDHQ based on the methodology reported by Shinozaki et al. [25]. Although the validity of their UPFs calculation method has been previously validated [25], there are limitations associated with using the BDHQ. It is challenging to include all food items using the BDHQ, and the BDHQ may not be applicable for studies involving populations with different regional and cultural dietary habits. However, our study also had strength. To the best of our knowledge, the current study represents the first investigation into the relationship between UPFs and gut microbiota among patients with T2D.
Conclusions
In conclusion, we showed the association between the gut microbial composition, particularly represented by Ruminococcus and Roseburia, and the density of UPFs intake in patients with T2D. In the future, further research is needed to focus on elucidating the detailed mechanisms and causal relationships between UPFs consumption and the gut microbiata.
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- UPFs
Ultra-processed foods
- T2D
Type 2 diabetes
- BMI
Body mass index
- BDHQ
Brief-type self-administered diet history questionnaire
- DNA
Deoxyribonucleic acid
- rRNA
Ribosomal ribonucleic acid
- PCR
Polymerase chain reaction
- SD
Standard deviations
- β
The partial regression coefficient
Author contributions
T.I. conceptualized the present study and conducted the data analysis and wrote the original manuscript. Y.H. conceptualized the present study, collected the data and contributed the discussion. Y.I. and S.K. conducted the data analysis and contributed the discussion. A.K., R.S. and T.O. collected the data and contributed the discussion. R.I. conducted the data analysis and contributed the discussion. S.K., K.M., K.U. and T.T. conceptualized the present study, collected the data and contributed the discussion. Y.N. conceptualized the present study, performed funding acquisition, collected the data and contributed the discussion. M.H. and M.F. collected the data, contributed the discussion and supervised this study. All authors reviewed and approved the revised manuscript.
Funding
Not applicable.
Availability of data and materials
The sequence data used in this study have been submitted to Sequence Read Archive (SRA) with the accession number PRJNA766337 (Available from 1 November 2021).
Declarations
Ethics approval and consent to participate
The present study received approval by the ethics committee of the Kyoto Prefectural University of Medicine (no. ERB-C-534 and no. RBMR-E-466-5), and adhered to the principles of the Declaration of Helsinki. Written informed consent was obtained from all participants prior enrollment.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sun H, Saeedi P, Karuranga S, et al. IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. 10.1016/j.diabres.2021.109119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bommer C, Sagalova V, Heesemann E, et al. Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care. 2018;41(5):963–70. 10.2337/dc17-1962. [DOI] [PubMed] [Google Scholar]
- 3.American Diabetes Association Professional Practice Committee. pharmacologic approaches to glycemic treatment: standards of care in diabetes—2024. Diabetes Care. 2024;47:S158–78. 10.2337/dc24-S009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evert AB, Dennison M, Gardner CD, et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care. 2019;42(5):731–54. 10.2337/dci19-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang L, Martínez Steele E, Du M, et al. Trends in consumption of ultraprocessed foods among US youths aged 2–19 years, 1999–2018. JAMA. 2021;326(6):519. 10.1001/jama.2021.10238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vandevijvere S, Jaacks LM, Monteiro CA, et al. Global trends in ultraprocessed food and drink product sales and their association with adult body mass index trajectories. Obes Rev. 2019;20(S2):10–9. 10.1111/obr.12860. [DOI] [PubMed] [Google Scholar]
- 7.Monteiro CA, Cannon G, Moubarac JC, Levy RB, Louzada MLC, Jaime PC. The UN decade of nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018;21(1):5–17. 10.1017/S1368980017000234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Llavero-Valero M, Escalada-San Martín J, Martínez-González MA, Basterra-Gortari FJ, de la Fuente-Arrillaga C, Bes-Rastrollo M. Ultra-processed foods and type-2 diabetes risk in the SUN project: a prospective cohort study. Clin Nutr. 2021;40(5):2817–24. 10.1016/j.clnu.2021.03.039. [DOI] [PubMed] [Google Scholar]
- 9.Pant A, Gribbin S, Machado P, et al. Ultra-processed foods and incident cardiovascular disease and hypertension in middle-aged women. Eur J Nutr. 2024;63(3):713–25. 10.1007/s00394-023-03297-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lane MM, Gamage E, Du S, et al. Ultra-processed food exposure and adverse health outcomes: umbrella review of epidemiological meta-analyses. BMJ. 2024. 10.1136/bmj-2023-077310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Visioli F, Del Rio D, Fogliano V, Marangoni F, Ricci C, Poli A. Ultra-processed foods and health: are we correctly interpreting the available evidence? Eur J Clin Nutr. 2024. 10.1038/s41430-024-01515-8. [DOI] [PubMed] [Google Scholar]
- 12.Ross FC, Patangia D, Grimaud G, et al. The interplay between diet and the gut microbiome: implications for health and disease. Nat Rev Microbiol. 2024;22(11):671–86. 10.1038/s41579-024-01068-4. [DOI] [PubMed] [Google Scholar]
- 13.Menafra D, Proganò M, Tecce N, Pivonello R, Colao A. Diet and gut microbiome: Impact of each factor and mutual interactions on prevention and treatment of type 1, type 2, and gestational diabetes mellitus. Human Nutr Metab. 2024. 10.1016/j.hnm.2024.200286. [Google Scholar]
- 14.Atzeni A, Martínez MÁ, Babio N, et al. Association between ultra-processed food consumption and gut microbiota in senior subjects with overweight/obesity and metabolic syndrome. Front Nutr. 2022. 10.3389/fnut.2022.976547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martínez Leo EE, Segura Campos MR. Effect of ultra-processed diet on gut microbiota and thus its role in neurodegenerative diseases. Nutrition. 2020. 10.1016/j.nut.2019.110609. [DOI] [PubMed] [Google Scholar]
- 16.Hashimoto Y, Hamaguchi M, Kaji A, et al. Intake of sucrose affects gut dysbiosis in patients with type 2 diabetes. J Diabetes Investig. 2020;11(6):1623–34. 10.1111/jdi.13293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen Z, Khandpur N, Desjardins C, et al. Ultra-processed food consumption and risk of type 2 diabetes: three large prospective U.S. cohort studies. Diabetes Care. 2023;46(7):1335–44. 10.2337/dc22-1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Delpino FM, Figueiredo LM, Bielemann RM, et al. Ultra-processed food and risk of type 2 diabetes: a systematic review and meta-analysis of longitudinal studies. Int J Epidemiol. 2022;51(4):1120–41. 10.1093/ije/dyab247. [DOI] [PubMed] [Google Scholar]
- 19.American Diabetes Association. Classification and diagnosis of diabetes: standards of medical care in diabetesd 2018. Diabetes Care. 2018;41:S13–27. 10.2337/dc18-S002. [DOI] [PubMed] [Google Scholar]
- 20.Hamaguchi M, Kojima T, Takeda N, et al. The metabolic syndrome as a predictor of nonalcoholic fatty liver disease. Ann Intern Med. 2005;143(10):722. 10.7326/0003-4819-143-10-200511150-00009. [DOI] [PubMed] [Google Scholar]
- 21.Matsuo S, Imai E, Horio M, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53(6):982–92. 10.1053/j.ajkd.2008.12.034. [DOI] [PubMed] [Google Scholar]
- 22.Iwata M, Matsushita Y, Fukuda K, et al. Secretory units of islets in transplantation index is a useful predictor of insulin requirement in Japanese type 2 diabetic patients. J Diabetes Investig. 2014;5(5):570–80. 10.1111/jdi.12181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hashimoto Y, Kaji A, Sakai R, et al. Skipping breakfast is associated with glycemic variability in patients with type 2 diabetes. Nutrition. 2020. 10.1016/j.nut.2019.110639. [DOI] [PubMed] [Google Scholar]
- 24.Kobayashi S, Murakami K, Sasaki S, et al. Comparison of relative validity of food group intakes estimated by comprehensive and brief-type self-administered diet history questionnaires against 16 d dietary records in Japanese adults. Public Health Nutr. 2011;14(7):1200–11. 10.1017/S1368980011000504. [DOI] [PubMed] [Google Scholar]
- 25.Shinozaki N, Murakami K, Yuan X, et al. The association of highly processed food consumption with food choice values and food literacy in Japanese adults: a nationwide cross-sectional study. Int J Behav Nutr Phys Act. 2023. 10.1186/s12966-023-01538-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Willett W, Howe G, Kushi L. Adjustment for total energy intake in epidemiologic studies. Am J Clin Nutr. 1997;65(4):1220S-1228S. 10.1093/ajcn/65.4.1220S. [DOI] [PubMed] [Google Scholar]
- 27.Inoue R, Ohueekitano R, Tsukahara T, et al. Prediction of functional profiles of gut microbiota from 16S rRNA metagenomic data provides a more robust evaluation of gut dysbiosis occurring in Japanese type 2 diabetic patients. J Clin Biochem Nutr. 2017;61(3):217–21. 10.3164/jcbn.17744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Takagi T, Naito Y, Inoue R, et al. The influence of longgterm use of proton pump inhibitors on the gut microbiota: an ageesexxmatched caseecontrol study. J Clin Biochem Nutr. 2018;62(1):100–5. 10.3164/jcbn.17778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nishino K, Nishida A, Inoue R, et al. Analysis of endoscopic brush samples identified mucosa-associated dysbiosis in inflammatory bowel disease. J Gastroenterol. 2018;53(1):95–106. 10.1007/s00535-017-1384-4. [DOI] [PubMed] [Google Scholar]
- 30.Bolyen E, Rideout JR, Dillon MR, et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2. Nat Biotechnol. 2019;37(8):850–2. 10.1038/s41587-019-0190-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang J, Qin J, Li Y, et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature. 2012;490(7418):55–60. 10.1038/nature11450. [DOI] [PubMed] [Google Scholar]
- 32.Karlsson FH, Tremaroli V, Nookaew I, et al. Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature. 2013;498(7452):99–103. 10.1038/nature12198. [DOI] [PubMed] [Google Scholar]
- 33.Cunningham AL, Stephens JW, Harris DA. Gut microbiota influence in type 2 diabetes mellitus (T2DM). Gut Pathog. 2021. 10.1186/s13099-021-00446-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Park J, Kato K, Murakami H, et al. Comprehensive analysis of gut microbiota of a healthy population and covariates affecting microbial variation in two large Japanese cohorts. BMC Microbiol. 2021. 10.1186/s12866-021-02215-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xu X, Zhang F, Ren J, et al. Dietary intervention improves metabolic levels in patients with type 2 diabetes through the gut microbiota: a systematic review and meta-analysis. Front Nutr. 2023. 10.3389/fnut.2023.1243095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zinöcker MK, Lindseth IA. The western diet–microbiome-host interaction and its role in metabolic disease. Nutrients. 2018. 10.3390/nu10030365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hoffmann C, Dollive S, Grunberg S, et al. Archaea and fungi of the human gut microbiome: correlations with diet and bacterial residents. PLoS ONE. 2013. 10.1371/journal.pone.0066019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bielemann RM, Santos Motta JV, Minten GC, Horta BL, Gigante DP. Consumption of ultra-processed foods and their impact on the diet of young adults. Rev Saude Publica. 2015. 10.1590/S0034-8910.2015049005572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ren M, Zhang H, Qi J, et al. An almond-based low carbohydrate diet improves depression and glycometabolism in patients with type 2 diabetes through modulating gut microbiota and glp-1: a randomized controlled trial. Nutrients. 2020;12(10):1–21. 10.3390/nu12103036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Monteiro CA, Cannon G, Levy RB, et al. Ultra-processed foods: what they are and how to identify them. Public Health Nutr. 2019;22(5):936–41. 10.1017/S1368980018003762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Whelan K, Bancil AS, Lindsay JO, Chassaing B. Ultra-processed foods and food additives in gut health and disease. Nat Rev Gastroenterol Hepatol. 2024;21(6):406–27. 10.1038/s41575-024-00893-5. [DOI] [PubMed] [Google Scholar]
- 42.Salame C, Javaux G, Sellem L, et al. Food additive emulsifiers and the risk of type 2 diabetes: analysis of data from the NutriNet-Santé prospective cohort study. Lancet Diabetes Endocrinol. 2024;12(5):339–49. 10.1016/S2213-8587(24)00086-X. [DOI] [PubMed] [Google Scholar]
- 43.Holder MK, Peters NV, Whylings J, et al. Dietary emulsifiers consumption alters anxiety-like and social-related behaviors in mice in a sex-dependent manner. Sci Rep. 2019;9(1):172. 10.1038/s41598-018-36890-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chassaing B, Compher C, Bonhomme B, et al. Randomized controlled-feeding study of dietary emulsifier carboxymethylcellulose reveals detrimental impacts on the gut microbiota and metabolome. Gastroenterology. 2022;162(3):743–56. 10.1053/j.gastro.2021.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fang Z, Rossato SL, Hang D, et al. Association of ultra-processed food consumption with all cause and cause specific mortality: population based cohort study. BMJ. 2024. 10.1136/bmj-2023-078476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baker P, Machado P, Santos T, et al. Ultra-processed foods and the nutrition transition: Global, regional and national trends, food systems transformations and political economy drivers. Obes Rev. 2020. 10.1111/obr.13126. [DOI] [PubMed] [Google Scholar]
- 47.Martini D, Godos J, Bonaccio M, Vitaglione P, Grosso G. Ultra-processed foods and nutritional dietary profile: a meta-analysis of nationally representative samples. Nutrients. 2021. 10.3390/nu13103390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Moreira PVL, Hyseni L, Moubarac JC, et al. Effects of reducing processed culinary ingredients and ultra-processed foods in the Brazilian diet: a cardiovascular modelling study. Public Health Nutr. 2018;21(1):181–8. 10.1017/S1368980017002063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Walker MS, Tarasiuk FS, Gustavo AS, Oliveira MS, Donadio MVF, Feoli AMP. Lifestyle improvement reduces the consumption of ultra-processed foods in adults with metabolic syndrome. Nutr Metab Cardiovasc Dis. 2022;32(8):1990–7. 10.1016/j.numecd.2022.04.016. [DOI] [PubMed] [Google Scholar]
- 50.Popkin BM, Barquera S, Corvalan C, et al. Towards unified and impactful policies to reduce ultra-processed food consumption and promote healthier eating. Lancet Diabetes Endocrinol. 2021;9(7):462–70. 10.1016/S2213-8587(21)00078-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Brooks AW, Priya S, Blekhman R, Bordenstein SR. Gut microbiota diversity across ethnicities in the United States. PLoS Biol. 2018. 10.1371/journal.pbio.2006842. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The sequence data used in this study have been submitted to Sequence Read Archive (SRA) with the accession number PRJNA766337 (Available from 1 November 2021).