Abstract
Background
The purpose of this study was to analysis the nostril symmetry and nasal stability following secondary rhinoplasty performed with either nasal septal cartilage implantation (G1) or simple alar cartilage suspension and internal fixation (G2) in patients with unilateral secondary cleft nasal deformity.
Methods
Nostril and alar symmetry were analyzed retrospectively in 13 consecutive patients in G1 and 17 in G2. Assessment of three indexes was first performed using photogrammetric measurements of photographs at pre-operation(T1), 7 days after repair (T2), and at least 6 months after repair (T3). The ratio of the cleft side to the noncleft side for nostril width, nostril height and alar height were used to assess symmetry. Changes in the mean ratios of the cleft side to the noncleft side at three different time points for three parameters were used to assess stability.
Results
In both groups, the alar height was improved after operation and remained stable in the follow-up period. The nostril width significantly decreased in G1 and G2, remaining consistent in the follow-up for G1 but increasing in G2. The nostril height significantly increased in G1 and stabilized during the follow-up, while it decreased after operation and remained so throughout the follow-up for G2.
Conclusion
Both techniques can maintain stability more than six months after surgery, except for the nostril width with simple alar cartilage suspension and internal fixation technique. The nasal septal cartilage implantation technique may have advantages in improving the nasal symmetry of the nostril width and height.
Keywords: Secondary rhinoplasty, Septal cartilage, Alar cartilage, Nostril symmetry
Introduction
Secondary nasal deformity after cleft lip primary repair remains one of the most challenging problems for plastic surgeons in rhinoplasty. Numerous techniques for correcting this issue have been described including the combination of open rhinoplasty with the Dibbell and Tajima techniques, which was first introduced by Court B. Cutting [1]. Open approach combining reverse U incision, septal extension graft could result in the nose of the patients with cleft lip nasal deformity being closer to that of the normative profile [2].
During surgical correction, traction forces generated by sutures could well restore the position of the cartilage and thus the normal contour of the nose [3]. Huang hanyao et al. also used the biomechanical analyses to verify the fixation with suture at the medial crus might be an efficient method in restoring the nasal symmetry [4]. However, Chong Kun et al. surveyed the satisfaction rate of several suture fixation techniques without any graft or implantation with septo-turbinoplasty, the worst was based on the nostril symmetry [5]. In addition, Araco et al. assessed whether patients were satisfaction with 4 kinds of autogenous cartilage implantation (auricular cartilage graft, septal cartilage graft, costal cartilage graft, composite graft), and found that most patients with auricular or septal cartilage grafts were highly satisfied [6].Therefore, combining cartilage transplantation has been designed to improve surgical outcomes in secondary rhinoplasty of cleft patients, but the risks of absorption also exist [7].
Despite the pros and cons, the objective of this study was to analyze the efficacy and stability of nostril and alar symmetry following secondary rhinoplasty done with either nasal septal cartilage implantation or simple alar cartilage suspension and internal fixation in patients with unilateral cleft nasal deformity.
Materials and methods
Patients
A retrospective study was conducted on patients with unilateral cleft nasal deformity between 2017 and 2020 at West China Hospital of Stomatology. Patients eligible for inclusion in the study were non-syndromic complete cleft lip and palate (CLP) patients who underwent a combined Dibbell/Tajima open rhinoplasty with or without cartilage transplantation and had a follow-up of greater than 6 months. A total of 30 patients were identified for the study by these selection criteria. None of the patients underwent secondary repair of nasolabial region or presurgical nasoalveolar molding. Also it was ethically approved from the institutional ethics committee at the West China School of Stomatology, Sichuan University (No: WCHSIRB-ST-2016-164), and has been conducted in accordance to the guidelines of the declaration of Helsinki. Written informed consent was taken from each participant or parents/legal guardians for pediatric patients for publication of the data and accompanying images.
Surgical techniques
After fully explaining the condition and the two surgical methods, patients ultimately chose either nasal septal cartilage implantation or simple alar cartilage suspension and internal fixation through preoperative informed consent. All surgeries were performed by experienced surgeons under general anesthesia.
Both techniques used the modified Tajima method, commencing with a reverse-U incision. The nasal skin and mucosa were thoroughly undermined around the affected nasal cartilages. The connecting ligament between the lower lateral cartilage and the upper lateral cartilage was delicately dissected and released.
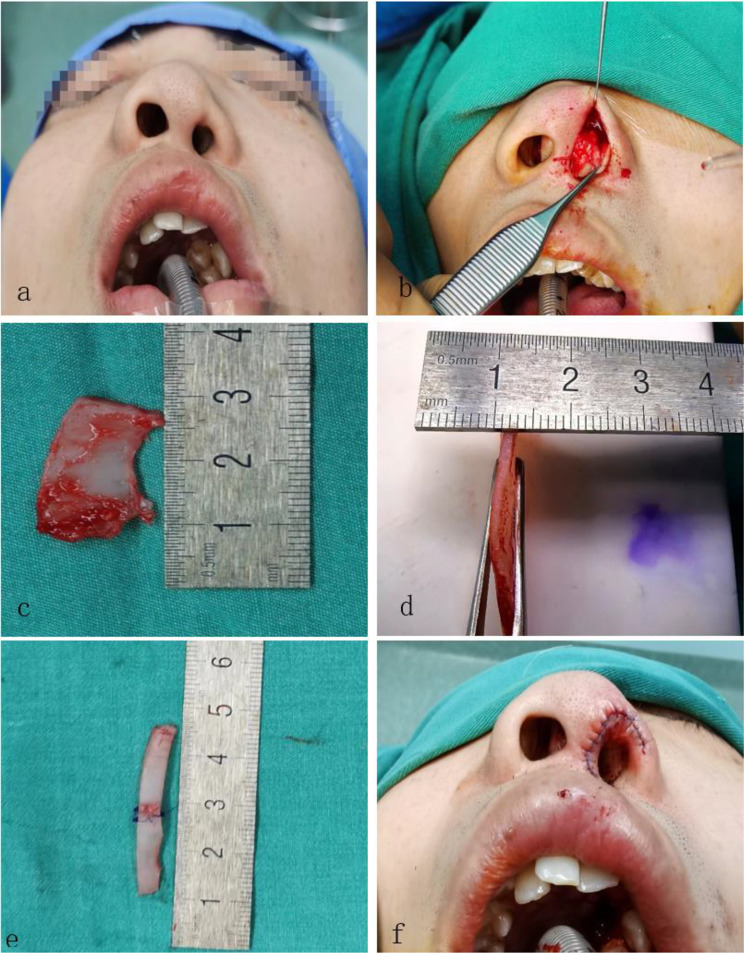
In nasal septal cartilage implantation, the septum was exposed and dissected, leaving a L-strut of at least 1-cm caudal and 1.5-cm dorsal cartilage to provide structural support for the nose [8]. The obtained septal cartilage was then converted into long strips as needed, with the length and width tailored to each patient’s degree of deformity (Fig. 1). One end of the nasal septal cartilage was inserted between the two medial crura of the bilateral alar cartilage to support the tip and extend the nasal columella. The other end was inserted along the arc of the alar cartilage on the cleft side, extending as far as possible along the lateral crura of the alar cartilage to elevate the ala and correct the alar collapse deformity. The medial and lateral crura of nasal alar cartilage and septal cartilage were fixed with sutures (Fig. 2).
Fig. 1.
(a) Preoperative nasal morphology. (b) Dissecting the alar and septal cartilage. (c & d) Acquired nasal septum cartilage. (e) Cartilage grafts were trimmed and connected for elevating ala. (f) The basal view after septal cartilage implantation
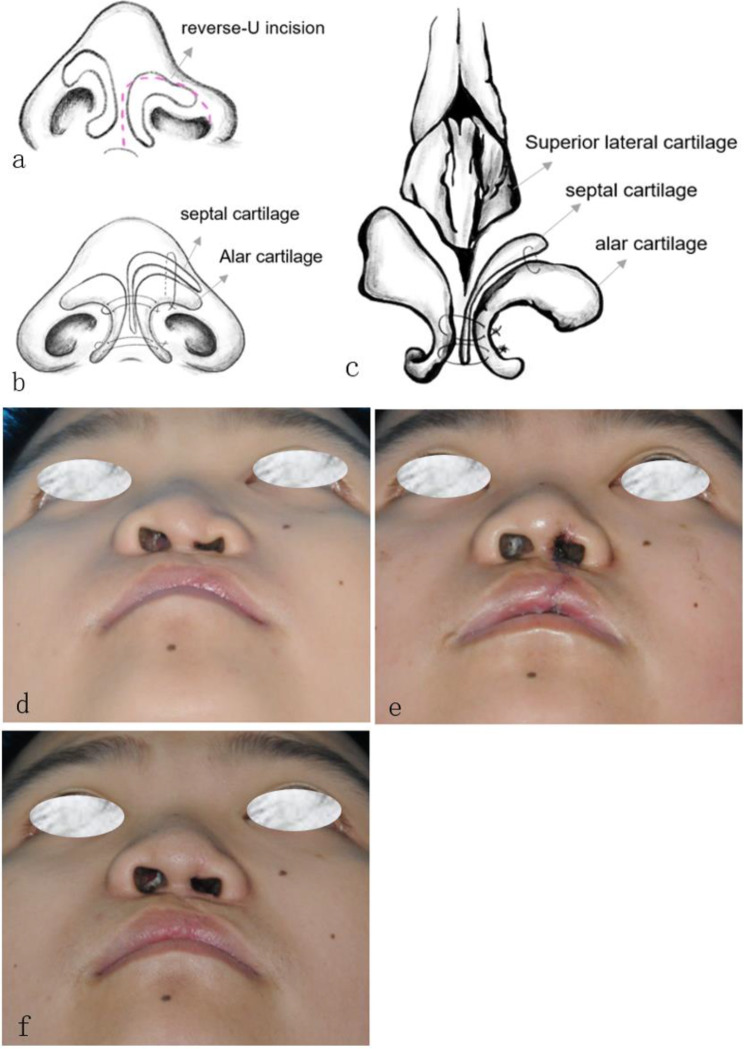
Fig. 2.
(a) Illustration of the reverse-U incision. (b & c) Illustration depicts the placement of sutures on medial and lateral crura of nasal alar cartilage and septal cartilage from a basal (b) and frontal view(c). (d, e & f) Patient underwent nasal septal cartilage implantation (G1) preoperative (T1), 7 days post-operative (T2) and follow up (T3), respectively
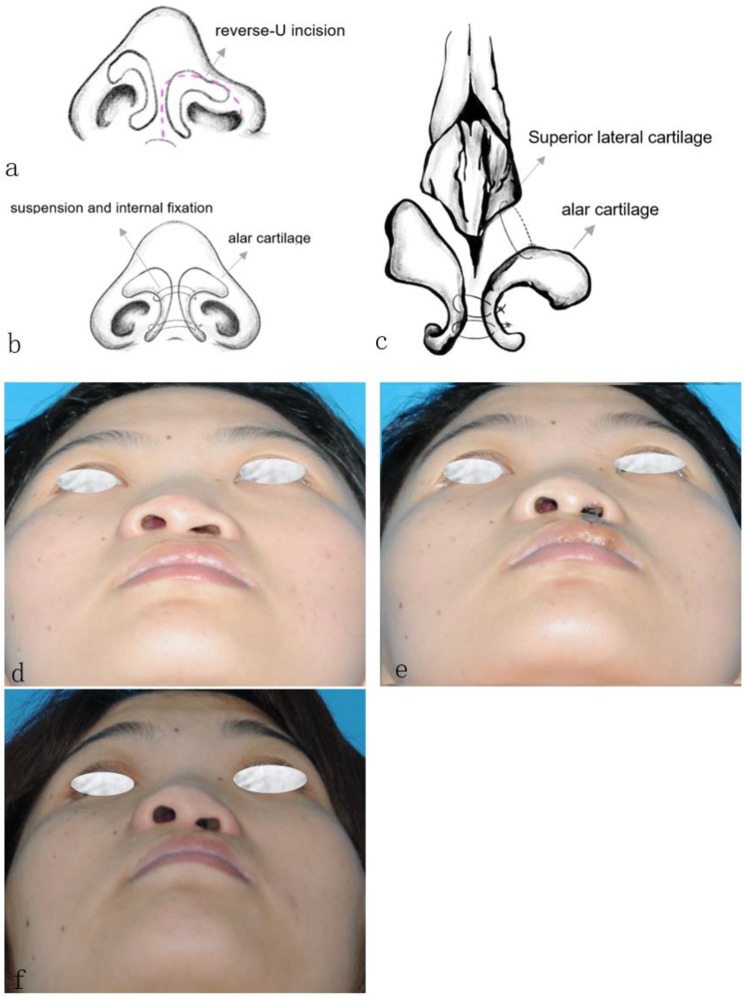
In simple alar cartilage suspension and internal fixation, the lateral crura of the nasal alar cartilage was anchored to the upper lateral cartilage, while the medial crura was sutured to the contralateral side with 5 − 0 nylon to achieve symmetrical elevation (Fig. 3).
Fig. 3.
(a) Illustration of the reverse-U incision. (b) Illustration depicts the placement of sutures on medial and lateral crura of nasal alar cartilage from a basal view. (c). Illustration depicts the placement of sutures on lower and upper lateral cartilage from frontal view. (d, e & f) Patient underwent simple alar cartilage suspension and internal fixation (G2) preoperative (T1), 7 days post-operative (T2) and follow up (T3), respectively
Data acquisition
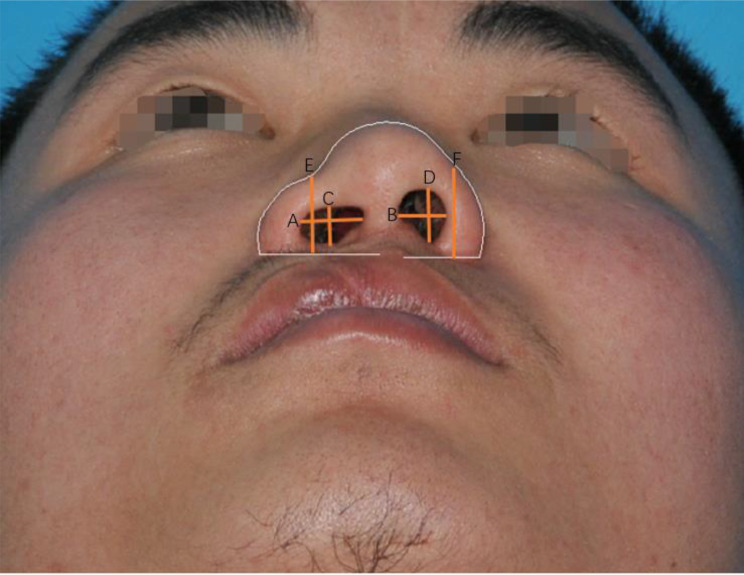
Basal photographic views and indirect anthropometric measurement tools were used for analysis. Standard photographs were taken pre-operation (T1), 7 days after repair (T2) and at least 6 months after repair (T3) with a Nikon Coolpix 950 digital camera (Nikon Corp., Tokyo, Japan) and cropped to contain only the eyes, nose, and lips to avoid possible bias caused by background and irrelevant facial features according to the Farkas principle [9–11]. Indirect anthropometric measurements were taken by the same technician once a week, for a total of three times, on the digital photographs processed by AutoCAD 2021 Software, including nostril width, nostril height and alar height of the cleft side and the noncleft side (Fig. 4; Table 1). To control for measurement error, 27 out of 90 photos were randomly selected for measurement and intra-group correlation coefficient (ICC) analysis prior to the official measurements. The survey technician was blinded to the surgical groups. The average values of each parameter were used for analysis. To avoid bias caused by irrelevant facial features and different sizes of photographs, all the data are presented as the ratio of the cleft side to the noncleft side.
Fig. 4.
the nostril width (Lines A&B), the nostril height (lines C&D) and the alar height (lines E & F) of the cleft side and the noncleft side
Table 1.
Description of the measurements
| Aspects | Description |
|---|---|
| Alar height |
the vertical line from the midpoint of the curve from root to tip of one side to the base of the nose |
| Nostril width | perpendicular line forming the narrowest part of the columella to the lateral wall of the ala |
| Nostril height | perpendicular line forming the highest part of the nostril sill to the base of the nostril |
Statistical analysis
All the statistical analyses were performed using SPSS22.0 statistical software. The values on the cleft side were divided by the those on the noncleft side. A ratio of 1 indicated perfect symmetry, and any deviation from 1 represented asymmetry. The changes of symmetry and differences between the two groups were evaluated by paired t tests, and the nasal stability was tested by repeated-measures ANOVA based on the change in the mean ratio of the cleft side to the noncleft side at three different time points. Only P values < 0.05 indicated significant differences, suggesting changes within and between groups. In addition, P values < 0.05 at T1-T2 indicated that the operation was effective, and P values > 0.05 at T2-T3 indicated that the operative outcome was stable. The reliability of all the results was guaranteed by the ICC testing of random sampling.
Results
Demographic data and intra-class correlation coefficient (ICC)
The study included 30 consecutive patients, with ages ranging from 13 to 31 years and an average age of 21 years at the time of surgery. Thirteen males and 17 females were enrolled in two groups, with 13 undergoing nasal septal cartilage implantation (G1) and the others undergoing simple alar cartilage suspension and internal fixation (G2).Twenty-one patients had a left-sided cleft, whereas 9 patients had a right-sided cleft. The demographic data for each group are presented in Table 2.
Table 2.
Demographic data
| Data from study patient | G1 (n = 13) | G2 (n = 17) | Total |
|---|---|---|---|
| Male (%) | 4 (30.77%) | 9(69.23%) | 13(43.33%) |
| Famale (%) | 9 (52.94%) | 8(47.06%) | 17(56.67%) |
| Right side (%) | 3 (33.33%) | 6(66.67%) | 9(30.00%) |
| Left side (%) | 10(47.62%) | 11(52.38%) | 21(60.00) |
| Mean Age(years) | 19.46 ± 5.08 | 21.35 ± 5.04 | 20.53 ± 5.06 |
All three measurements were subjected to ICC testing, and the results showed all ICC values were greater than 0.8 (Table 3), indicating the reliability of the measurements.
Table 3.
ICC of the measurements
| Index | ICC P |
|---|---|
| Alar height | 0.994 (P = 0.000) |
| Nostril width | 0.999 (P = 0.000) |
| Nostril height | 0.998 (P = 0.000) |
Abbreviation: ICC: Intra-class Correlation Coefficient
P values < 0.05 are marked in Bold
Operative effect
It was showed in Table 4 that there was no significant difference in any of the three parameters of preoperative deformity (T1) between G1 and G2 (P = 0.09, P = 0.64, P = 0.11, respectively). The alar height of cleft side showed significant improvement in both groups after surgery (P < 0.001 for G1, P = 0.003 for G2), with no discernible difference observed between the two groups at T2 (P = 0.70). Additionally, both groups exhibited substantial enhancement in nostril width symmetry at T2 (P = 0.01 for G1, P < 0.001 for G2), with no significant disparity noted between the two groups (P = 0.08). Notably, the nostril height of G1 was elevated (P = 0.001) but decreased in G2 (P = 0.04), resulting a significant difference between the two groups at T2 (P = 0.001).
Table 4.
Preoperative、immediately postoperative and follow-up photographic analysis
| Mean ratio [95%CI] |
Group | T1 | T2 | (T2-T1) t(P) |
T3 | (T3-T2) t(P) |
F(P) |
|---|---|---|---|---|---|---|---|
| Alar height | G1 | 0.85[0.82, 0.89] | 0.94[0.90, 0.97] | 5.32(<0.001) | 0.91[0.88, 0.94] | 2.05(0.06) | 1.595(0.22) |
| G2 | 0.90[0.87, 0.93] | 0.95[0.91, 0.98] | 3.51(0.003) | 0.93[0.90, 0.96] | 1.07(0.30) | ||
| t(P) | 1.83(0.09) | 0.39(0.70) | 1.01(0.33) | ||||
| Nostril width | G1 | 1.25[1.06, 1.43] | 1.06[0.87, 1.25] | 3.33(0.01) | 0.97[0.80, 1.15] | 1.89(0.08) | 6.91(0.002) |
| G2 | 1.20[1.09, 1.31] | 0.90[0.82, 0.98] | 6.73(< 0.001) | 1.06[0.97, 1.14] | 3.68(0.002) | ||
| t(P) | 0.48(0.64) | 1.84(0.08) | 0.53(0.60) | ||||
| Nostril height | G1 | 0.75[0.63, 0.87] | 1.03[0.94, 1.13] | 4.29(0.001) | 0.94[0.81, 1.07] | 1.56(0.15) | 14.53(< 0.001) |
| G2 | 0.85[0.79, 0.92] | 0.80[0.69, 0.90] | 2.18(0.04) | 0.85[0.78, 0.93] | 1.72(0.11) | ||
| t(P) | 1.68(0.11) | 3.54(0.001) | 0.82(0.42) |
Abbreviation: Mean ratio: cleft/non-cleft; 95%CI: 95% confidence interval
T1, pre-operation; T2, 7 days after repair; T3, at least 6 months after repair
G1: Nasal septal cartilage implantation; G2: Simple alar cartilage suspension and internal fixation
t: t-value >2 are marked in Bold
P values < 0.05 are marked in Bold
F: The value of intergroup effect
Operative effect and stability
As shown in Table 4, there was no significant discrepancy in growth rates between cleft and noncleft sides in both groups except for the nostril width in G2.
The alar height on the cleft side in G2 exhibited a mean difference of 5% lower post-surgery (T2), which subsequently worsened to 7% lower at T3 (P = 0.30). This is slightly better than G1, which exhibited 6% lower at T2 and deteriorated to 9% at T3 (P = 0.06). However, there was no significant difference between the two groups (P = 0.22).
The nostril width on the cleft side in G1 exhibited a 6% increase than the noncleft side at T2, but decreased to a 3% at T3 (P = 0.08). In contrast, G2 showed a change from being 10% narrower at T2 to 6% wider at T3, with significant alteration during follow-up (P = 0.002) although no difference was found between G1 and G2 at T3 (P = 0.60).
The nostril height displayed no discernible change in either group from T2 to T3. At T2, the nostril height on the cleft side in G1 was 3% higher compared to the other side and 20% lower in G2. Nevertheless, it decreased to 6% shorter at T3 for G1 while increased to 15% lower for G2 (P = 0.15, P = 0.11, respectively); ultimately presenting no significant difference between groups at T3 (P = 0.42).
Discussion
Although primary rhinoplasty can correct nose deformity to a certain extent, it is mainly focused on improving the morphology of the lower third of the nose. However, secondary nasal deformity presents a completely different challenge for secondary rhinoplasty, for example, an inferiorly and medially rotated lower lateral cartilage and lateralized alar base. As suggested by previous studies, the secondary deformity is a result of the baseline congenital deformity subjected to secondary scarring from prior iatrogenic interventions and deformational changes imparted through craniofacial growth [11–13].
The issue of whether secondary cleft lip nasal deformity existing in the cartilage stunting is still controversial and warrants further investigation. Park et al. and Kim et al. concluded that the lateral crus and the medial crus of the alar cartilage on the cleft side are not hypoplastic [2, 14]. In 35 patients with unilateral cleft nasal deformity investigated in Park’s study, the width of the lateral crus of the alar cartilage was significantly greater on the cleft side than on the noncleft side, but the difference in the thickness and length of the lateral crus was not significantly different between the cleft and noncleft sides. Therefore, cartilage grafting might be an unnecessary and simple alar cartilage suspension and internal fixation between the LLC and ULC should be a valid method.
According to the results nasal septal cartilage transplantation might be more effective in achieving symmetry of the nostril, and the outcomes remained stable during follow-up period. Both techniques effectively reduced the nostril width (P = 0.01 for G1, P < 0.001 for G2) on the cleft side after surgery, but G2 (P = 0.002) experienced a reoccurrence while G1 remained stable (P = 0.08). There was no statistical difference between two groups in postoperative appearance. Discrepancies in nostril height between the two groups were evidenced at T2 (P = 0.001), but no significant difference was found at T3 (P = 0.42). In general, the immediate postoperative outcome of cartilage transplantation is superior to that of simple alar cartilage suspension and internal fixation, but over time, the statistical difference in effectiveness between the two groups becomes insignificant.
In the present study, septal cartilage as the grafting was used for correcting nasal deformity and a promising immediate postoperative outcome of quantitative measurements of nostril width, nostril height and alar height were achieved. Removing the deflected nasal septum into the nasal columella may provide better support and retention to the nasal tip and ala than other techniques. This study revealed that nasal septal cartilage implantation improved the symmetry of nostril height and width, and enhanced the stability as well, but the symmetry of the alar height was not significantly satisfied. A possible explanation for this might be that the aim of the surgical methods performed was more concerned with the support of the nostril rather than the ala. The limited size of the obtained septal cartilage may also be the factor.
New wounds at the donor site of the auricular or costal cartilage were unacceptable for some patients. Patients with unilateral cleft lip and palate mostly present a deviated nasal septum to the cleft side resulting in various degrees of nasal obstruction and deviation of nasal dorsum [15], which was verified during the operation. Obtained septal cartilage from the same surgical incision also could adjust the deviation and improve airway patency as H. L. Nguyen confirmed [16]. Moreover, the absorption and infection of nasal septum cartilage grafts have rarely been reported in the clinical setting (17–18). Almost no complications were recorded after surgery. There were no cases of infection, or cartilage loss.
This paper specifically focuses on the change of nostril, without addressing the overall change of nasal appearance. It is acknowledged that the depression of the nasal base can impact the overall height of the nasal wing. However, based on the data, it is evident that both methods are effective in improving alar height and nasal height. A subsequent study will further explore the impact of nasal base depression, including the structural integrity of the nasal base bone and the constructive techniques for addressing nasal base issues.
There are some limitations to this study. First, this was a retrospective study that included only 30 consecutive patients. Increasing the sample size and the measured parameters is needed for further research. Second, clinically, there is a slight difference in bilateral nostril height before surgery, surgeons tend to choose suspension technique, which is easier to grasp and cost-saving. Lastly, Different from the primary rhinoplasty, the second rhinoplasty will pay more attention to aesthetics, so patient satisfaction is an important evaluation index of plastic surgery. In the study, some patients were less than 5 years after surgery and we will conduct a more in-depth study on this indicator in the future.
Conclusion
In summary, these two surgical methods can improve the symmetry of some aspects. Despite the data show that the implantation of nasal septum cartilage had an advantage over simple internal fixation of the alar cartilage for improving nasal symmetry in patients with secondary unilateral cleft lip nasal deformities, a longer-term longitudinal research is still required to evaluate the influence of two methods on nasal profile. The authors considered that regardless of whether the alar cartilage has developmental deficiencies, reconstruction with nasal septum grafts can provide better support and reduce recurrence compared to simple internal fixation.
Acknowledgements
Not applicable.
Author contributions
Shuxia Dong and Yulang Xu conceived and drafted the manuscript. Ni Zeng revised and edited the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (grant no. 81800951) and the Sichuan Province Science and Technology Support Program (grant no. 2022NSFSC1519) to NZ.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethical approval and consent to participate
Ethical approval was obtained from the institutional ethics committee at the West China School of Stomatology, Sichuan University (No: WCHSIRB-ST-2016-164). Written informed consent was taken from each participant or parents/legal guardians for pediatric patients for publication of the data and accompanying images.
Consent for publication
All presentations of case reports have consent for publication.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shuxia Dong and Yulang Xu contributed equally to this work and thus share the first authorship.
References
- 1.Flores RL, Sailon AM, Cutting CB. A Novel Cleft Rhinoplasty Procedure combining an Open Rhinoplasty with the Dibbell and Tajima techniques: a 10-Year review. Plast Reconstr Surg. 2009;124(6):2041–7. [DOI] [PubMed] [Google Scholar]
- 2.Saito T, Lonic D, Lo CC, Tu JC, Hattori Y, Lo LJ. Septal extension graft in Cleft Rhinoplasty: patients with secondary unilateral cleft lip nasal deformity. Plast Reconstr Surg. 2024;154(5):e949–62. [DOI] [PubMed] [Google Scholar]
- 3.Huang H, Li Y, Luo X, Cheng X, Shi B, Li J. Mechanical analyses of critical surgical maneuvers in the correction of cleft lip nasal deformity. PLoS ONE. 2018;13(4):e0195583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang H, Cheng X, Luo X, Shi B, Li J. Biomechanical analyses of common suspension sutures in primary cleft lip rhinoplasty. Head Face Med. 2019;15(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee CK, Min BD. Open rhinoplasty in secondary cleft nose deformity with suture techniques. Arch Craniofac Surg. 2022;23(5):211–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Araco A, Gravante G, Araco F, et al. Autologous cartilage graft rhinoplasties. Aesthetic Plast Surg. 2006;30(2):169–74. [DOI] [PubMed] [Google Scholar]
- 7.Fisher M, Alba B, Ahmad J, et al. Current practices in dorsal augmentation rhinoplasty. Plast Reconstr Surg. 2022;149(5):1088–102. [DOI] [PubMed] [Google Scholar]
- 8.Lee JS, Lee DC, Ha DH, Kim SW, Cho DW. Redefining the septal L-Strut to prevent collapse. PLoS ONE. 2016;11(4):e0153056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farkas LG, Bryson W, Klotz J. Is photogrammetry of the face reliable? Plast Reconstr Surg. 1980;66(3):346–55. [PubMed] [Google Scholar]
- 10.Zhang R, Zhang LG, Li XH, Li R. [Evaluation of the symmetry in nasolabial area of unilateral complete cleft lip with the method of rotation descent step by step]. Shanghai Kou Qiang Yi Xue. 2020;29(1):51–4. [PubMed] [Google Scholar]
- 11.Knight ZL, Ganske I, Deutsch CK, Mulliken JB. The changing nasolabial dimensions following repair of Unilateral Cleft lip: an anthropometric study in late childhood. Plast Reconstr Surg. 2016;138(5):e879–86. [DOI] [PubMed] [Google Scholar]
- 12.Rohrich RJ, Benkler M, Avashia YJ, Savetsky IL. Secondary Rhinoplasty for Unilateral Cleft Nasal deformity. Plast Reconstr Surg. 2021;148(1):133–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang L, Wang Z, Shan Z, et al. Nasal asymmetry changes during growth and development in 6- to 12-year-old children with repaired unilateral cleft lip and palate: a 3D computed tomography analysis. J Anat. 2022;240(1):155–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee DW, Choi BK, Park BY. Seven fundamental procedures for definitive correction of unilateral secondary cleft lip nasal deformity in soft tissue aspects. J Oral Maxillofac Surg. 2011;69(11):e420–430. [DOI] [PubMed] [Google Scholar]
- 15.Howard BK, Rohrich RJ. Understanding the nasal airway: principles and practice. Plast Reconstr Surg. 2002;109(3):1128–46. [DOI] [PubMed] [Google Scholar]
- 16.Nguyen HL, Hoang MP, Nguyen VM, Tran TT, Le VS. Use of Septal Cartilage in Rhinoplasty to correct nasal deformity after unilateral cleft lip and palate surgery. Clin Cosmet Investig Dent. 2022;14:131–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Karaca H. Using the septal shift technique to correct crooked nose deformity. Plast Reconstr Surg. 2022;150(2):e300–6. [DOI] [PubMed] [Google Scholar]
- 18.Li KY, Li BH, Wang J, Chen LJ, Zhou X. [Application of septal extension graft with autogenous septal cartilage and auricular cartilage in rhinoplasty]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2021;56(3):242–8. Chinese. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.