Abstract
Background
SMARCA4-deficient undifferentiated tumor (SMARCA4-UT) is a rare and highly malignant primary tumor characterized by the loss of SMARCA4 expression. Despite advancements in oncology, diagnosing and treating SMARCA4-UT remain significant clinical challenges.
Case demonstration
A 67-year-old male with a history of smoking presented to the hospital with complaints of abdominal distention and pain lasting for more than four days. Abdominal computed tomography (CT) revealed a high-density mass measuring approximately 41 × 37 mm in the right lower quadrant. Additionally, chest CT identified a high-density mass measuring 63 × 48 mm in the upper lobe of the right lung. The patient underwent partial small bowel resection, and postoperative pathological examination confirmed a diagnosis of SMARCA4-UT originating in the small mesentery. Unfortunately, the patient succumbed to respiratory failure 21 days after the diagnosis.
Conclusion
SMARCA4-UT is an exceedingly rare and aggressive undifferentiated tumor. This case highlights a presentation of SMARCA4-UT with abdominal pain and distention as initial symptoms. Clinicians should consider SMARCA4-UT in middle-aged or elderly male patients with a history of smoking who present with large masses. Comprehensive chest imaging is essential to exclude the thoracic primary disease in such cases.
Keywords: SMARCA4, SMARCA4-deficient undifferentiated tumors, Intestine, Gastrointestinal symptoms, Diagnosis
Background
The SMARCA4 gene, located on the short arm of chromosome 19, encodes the BRG1 protein. Deficiency of SMARCA4 has been identified in various carcinomas and sarcomas, including undifferentiated or dedifferentiated carcinomas of the esophagus, gastrointestinal tract, uterus, ovary, and kidney [1]. In 2015, Le Loarer et al. [2] reported a series of 19 cases, predominantly involving young male smokers. They proposed the term “SMARCA4-deficient thoracic sarcoma (SMARCA4-DTS)” to describe this newly characterized tumor with distinctive clinicopathological features. Subsequently, the fifth edition of the World Health Organization (WHO) classification of thoracic tumors recognized SMARCA4-deficient undifferentiated tumors (SMARCA4-UT) as a unique entity, notable for its undifferentiated morphology and high invasiveness [3].
This paper presents a case of SMARCA4-UT originating in the right mesentery and leading to mechanical intestinal obstruction. The clinical presentation, histological morphology, immunohistochemical findings, differential diagnosis, and prognosis are discussed to enhance the understanding of this disease.
Case Presentation
A 67-year-old male with a history of smoking was admitted to the hospital with complaints of abdominal distention and pain lasting for more than four days. The symptoms began abruptly and without an identifiable cause, presenting as intermittent pain localized to the right abdomen, occasionally alleviated but unrelated to body position. The pain was accompanied by nausea and a single episode of vomiting, with gastric contents as the emesis. On physical examination, the abdomen appeared flat, with no visible gastrointestinal or peristaltic waves. Mild tenderness was noted in the right abdomen at the umbilical level. A pliable and movable mass measuring approximately 3.0 × 2.8 cm mass was palpated in this area, but it was non-tender and exhibited no rebound tenderness or muscle tension. Shifting dullness was negative, bowel sounds were active, and no splashing sounds were detected.
Abdominal computed tomography (CT) revealed a high-density mass measuring approximately 41 × 37 mm in the right lower abdomen, characterized by uneven density and a CT value of 51 HU. The enhancement pattern showed surface enhancement, with the mass closely associated with the adjacent small intestine. The upper small intestine appeared inflated and dilated, with multiple fluid levels, while the distal small intestine and large intestine were collapsed. Based on these findings, the radiologist suspected bleeding within the small bowel wall or adjacent mesentery, leading to mechanical small bowel obstruction.
Chest CT revealed a high-density mass measuring 63 × 48 mm in the upper lobe of the right lung. The mass had irregular edges, thickened adjacent pleura, and an increased anterior-posterior thoracic diameter. The lung density was unevenly reduced, with multiple spot-like, patchy, reticular, and cord-like shadows, some of which appeared indistinct. The pulmonary texture was markedly increased, with multiple track-like textures visible. Additionally, there was evidence of bronchial stenosis and occlusion in the posterior segment of the right upper lobe, along with enlarged right hilar lymph nodes.
Given the patient’s symptoms of intestinal obstruction, an exploratory laparotomy was performed, followed by small bowel decompression, partial small bowel resection, and anastomosis. Intraoperative exploration revealed an irregular mass measuring approximately 5 × 3 cm, located 180 cm away distal to Trez’s ligament and adjacent to the intestinal mesentery. The surface of the mass was smooth, with a wide and firm base. The mass exerted significant compression on the intestine, causing incomplete intestinal obstruction and proximal intestine dilation. Postoperatively, the excised tissue was sent for pathological examination.
Histopathological examination revealed a 10 cm segment of intestine with a diameter of 3.0 cm. The mucosa appeared smooth, with no obvious mass or ulceration. However, an oval mass measuring 4.5 × 4 × 3.5 cm was identified in the mesentery on the serosal surface of the intestinal midsection. The mass had a gray-red cut surface, was solid yet soft in texture, and exhibited areas of hemorrhage and necrosis. Its boundaries were poorly defined, blending into the surrounding tissue (Fig. 1).
Fig. 1.

An oval mass located in the mesentery on the serosal surface of the middle segment of the intestine
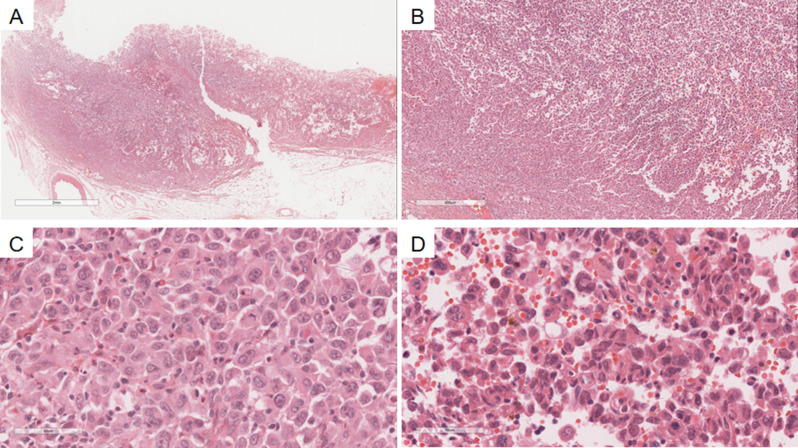
Microscopically, at low magnification (Fig. 2A), the tumor cells were diffusely distributed in patchy areas, with areas of hemorrhage, necrosis, and indistinct margins blending with adjacent tissues. At medium magnification (Fig. 2B), the cells exhibited fusiform and ovoid shapes, arranged in sheets or bundles. High magnification analysis revealed that the tumor comprised round to epithelioid cells (Fig. 2C), which were monomorphic and loosely cohesive, with vesicular nuclei, prominent nucleoli, and abundant eosinophilic cytoplasm. In some areas, rhabdoid tumor cells (Fig. 2D) were observed, characterized by cytoplasmic inclusions, eccentric nuclei, active mitotic figures, and the presence of giant tumor cells. Geographic necrosis was also present, with numerous apoptotic bodies interspersed among the tumor cells and granular blue-stained nuclear debris.
Fig. 2.
A Low-magnification view of the tumor showing a diffuse, patchy distribution. H&E x7. B Medium-magnification view revealing the tumor arranged in diffuse sheets, with areas displaying epithelioid, fusiform, and rhabdoid morphology. H&E x16. C High-magnification view showing epithelioid areas of the tumor. H&E x400. D High-magnification view showing tumor cells with giant cell and rhabdoid morphology. H&E x400
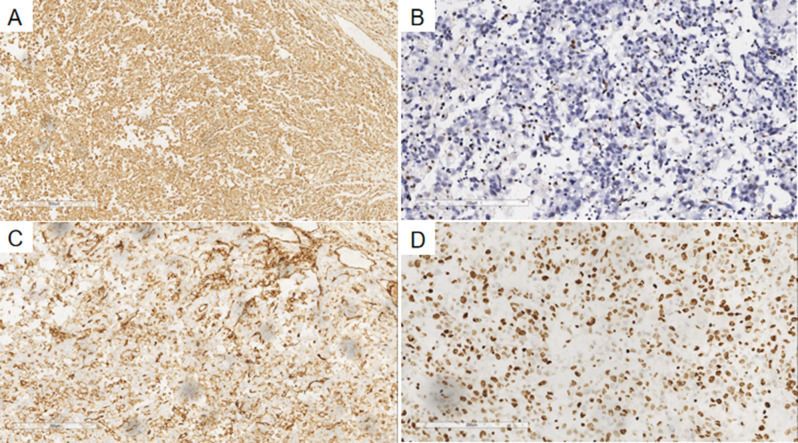
Immunohistochemical analysis showed the tumor cells were positive for Vimentin (Fig. 3A) and negative for BRG1, with inflammatory and vascular endothelial cells serving as internal nuclear-positive controls (Fig. 3B). Additional markers included CD34(+) (Fig. 3C), CK(partial+), CD10(partial+), and a high Ki-67 proliferation index (80%) (Fig. 3D). The tumor cells were negative for CK7, TTF1, P40, Bcl-2, CD15, CD20, CD3, CD21, CD30, c-Myc, cyclin D1, HMB45, Melan-A, MUM1, EMA, CD117, CDX2, Dog-1, SDH (no missing), INI-1 (no missing), SMA, calretinin, WT1, CD31, F8, ERG, Fli-1, galectin 3, and hepatocyte markers.
Fig. 3.
A Immunohistochemical staining showing positive Vimentin expression in tumor cells. EnVision, x200. B Immunohistochemical staining indicating BRG1 negativity in tumor cells, with inflammatory and vascular endothelial cells showing nuclear positivity as internal controls. EnVision, x200. C Immunohistochemical staining showing positive CD34 expression in tumor cells. EnVision, x200. D Immunohistochemical staining demonstrating that approximately 80% of the tumor cells were Ki-67 positive. EnVision, x200
Based on the histopathological features and immunohistochemical findings, the patient was diagnosed with SMARCA4-UT originating in the small mesentery. However, no pathological biopsy was performed on the lung mass. Given the imaging findings and the size of the lung mass, it was presumed to be the primary tumor, with widespread metastasis, including to the small mesentery.
Following partial small bowel resection, the patient received symptomatic treatments, including anti-infection measures, hemostasis, fluid replacement, and nutritional support. These interventions alleviated the symptoms of intestinal obstruction, allowing for discharge from the hospital.
Twenty days after discharge, the patient experienced a recurrence of abdominal pain and distention and was referred to the emergency department. Physical examination revealed a flat abdomen without visible gastrointestinal or peristaltic waves but mild tenderness in the right abdomen. A 10 cm old surgical scar from the previous procedure was noted along the midline, and bowel sounds were active. An abdominal CT scan revealed thickening of part of the small bowel wall in the lower abdominal-pelvic area, accompanied by cord-like high-density shadows. Nodular high-density shadows were observed on the right side of the sacrum, and bilateral inguinal lymph nodes were enlarged. Despite symptomatic treatment, including fluid infusion, the patient’s condition rapidly deteriorated. On the second day after admission, he suffered a sudden loss of consciousness, cardiac arrest, and respiratory failure leading to his death.
Discussion
The BRGl protein, a critical component of the SWI/SNF chromosome remodeling complex, is encoded by the SMARCA4 gene on chromosome 19. Loss of BRGl protein expression typically results from the SMARCA4 gene mutations [4, 5]. SMARCA4-UT is a high-grade malignancy that predominantly affects the thorax in adults. It exhibits an undifferentiated or rhabdoid phenotype and is characterized by the loss of SMARCA4, a key component of the BAF chromatin remodeling complex. The fifth edition of the WHO classification of lung tumors categorizes SMARCA4-UT under “other epithelial tumors of the lung,” alongside NUT carcinoma.
Clinically, SMARCA4-UT is a rare primary lung tumor with high invasiveness, poor prognosis, and a short median overall survival. Common presenting symptoms include dyspnea and chest pain [4]. At initial diagnosis, some patients exhibit lymph node metastasis or symptoms from metastatic sites, including the gastrointestinal tract, abdominal cavity, and pelvis. Metastases to the liver, ribs, adrenal glands, and even the temporal lobe have also been reported.
While most patients with SMARCA4-UT present with respiratory symptoms, our case was atypical. The patient exhibited abdominal pain and bloating caused by mechanical intestinal obstruction, with no significant respiratory complaints. This highlights the importance of considering SMARCA4-UT when evaluating large masses, particularly in middle-aged or elderly male patients with a history of smoking. A similar case reported by Fatma et al. [6] described intestinal SMARCA4-UT presenting with small intestinal perforation and a concurrent large mediastinal mass, suggesting an abdominal primary origin. Additionally, there are reports where the clinical manifestations of thoracic SMARCA4-UT primarily involved abdominal metastasis [7]. These findings underscore the diagnostic value of chest imaging in identifying the primary tumor. In our case, the radiological features and the size of the lung mass strongly suggested that the lung was the primary tumor, with the small mesenteric lesion representing metastasis. However, as the patient did not undergo lung biopsy, the primary tumor could not be confirmed histopathologically.
Imaging characteristics of SMARCA4-UT typically reveal a large, ill-defined soft tissue mass accompanied by compression of adjacent structures [8]. In the present case, imaging findings exhibited malignant features in both the lung and small intestine, consistent with the aggressive nature of SMARCA4-UT. Histologically, SMARCA4-UT tumors vary in size, ranging from 1.5 to 11 cm in maximum diameter, with a mean of 5.1 cm. These tumors are poorly circumscribed, with gray-yellow or grayish-yellow cut surfaces and a firm texture.
Microscopically, the tumor cells are diffusely arranged in sheets and are characterized by their large size, round-to-epithelioid shape, and poor adherence. The nuclei typically exhibit vacuolated chromatin and prominent nucleoli, with a relatively uniform appearance, although occasional mild to moderate pleomorphism is observed. Focal rhabdomyoblast-like cells are present, while mitotic figures and necrosis are frequently noted. Rare histological features include spindle cell morphology, mucoid changes, sclerosis, alveolar patterns, and clear cell changes [2]. Evidence of epithelial differentiation, such as glandular, papillary, or keratinization, is generally absent in most cases, though approximately 5% of tumors may exhibit a mixed histologic morphology characteristic of non-small cell lung cancer (NSCLC) [3]. In this case, the microscopic findings closely paralleled these typical features.
Immunohistochemically [9], SMARCA4 (BRG1) expression is entirely absent or significantly reduced, with approximately 25% of cases exhibiting diffuse but weakened expression. Loss of SMARCA2 (BRM) expression is common, while SMARCB1 (INI1) remains intact. Most cases demonstrate positivity for CD34, SOX2, or SALL4, with p53 overexpression observed in the majority. Cytokeratin expression is often focal, weak, or completely absent, rarely showing diffuse and strong expression. Synaptophysin expression is notable, requiring differentiation from neuroendocrine carcinoma. Claudin-4 is typically negative or localized. In rare instances, markers such as TTF1, p63, p40, or WT1 may show localized expression. Additionally, mismatch repair protein expression is preserved, indicating no deficiencies in this pathway.
In molecular genetics, SMARCA4 gene mutations are frequently detected in SMARCA4-UT, often coexisting with TP53 mutations. Additional mutations commonly associated include those in KRAS, STK11, or KEAP1, indicating a high tumor mutation burden. In some cases, TSC2, ROS1, and ATM mutations are also observed [3].
Given the morphologic diversity of SMARCA4-UT, its pathological diagnosis requires differentiation from the following tumors:
(1) SMARCA4-deficient NSCLC (SMARCA4-NSCLC): SMARCA4-NSCLC is typically better differentiated, presenting as well-defined adenocarcinoma or, rarely, squamous cell carcinoma. Adenocarcinomas are predominantly of the solid type and exhibit multiple differentiation patterns, such as acinar, mucinous, papillary, or signet-ring cell morphology. Tumor cells frequently appear as clear cells with focal rhabdoid cells or sarcomatoid areas. SMARCA4-NSCLC rarely shows loss of BRM, is almost universally positive for claudin-4 (> 95%) [9], and diffusely expresses CK7. In contrast, it is typically negative for CD34, with SOX2 and SALL4 focal expression observed in only 10 to 15% of cases.
(2) NUT carcinoma: This tumor usually occurs in the midline structures of the body and is characterized by its unique morphology, notably “sudden keratinization” within a background of small, undifferentiated cells. NUT carcinoma expresses the NUT protein and is often associated with the BRD4-NUTM1 gene fusion [10].
(3) Malignant melanoma: Malignant melanoma often presents with tumor cells that lose adhesion, exhibit prominent nucleoli, and possess nuclei with a characteristic irregular, bean-sprout-like appearance. These tumors are distinguished by the melanin marker expression, including HMB45, S100, Melan-A, and MiTF.
(4) Epithelioid sarcoma: Composed of polygonal epithelioid cells mixed with variable numbers of spindle cells, epithelioid sarcoma is characterized immunohistochemically by the CK and EMA expression, while INI-1 expression is typically lost. Abnormalities in the SMARCB1 gene are observed in more than 95% of cases [11].
Currently, there is no established standard treatment for SMARCA4-UT. Patients diagnosed with early-stage or locally advanced disease may benefit from radical surgery and adjuvant chemotherapy (or both) combined with bevacizumab. In recent years, novel targeted therapies and epigenetic regulators have shown promise, including CDK4/6 [12], OXPHOS, BET, AURKA, PARP, and ATR inhibitors. However, their efficacy remains to be validated through large-scale clinical studies. Future research must delve deeper into the pathogenesis, biological behavior, and molecular characteristics of thoracic SMARCA4-deficient UT (TSDUT) to identify more effective therapeutic strategies and improve patient outcomes [13, 14]. In our case, the patient presented with advanced disease and metastasis at the time of diagnosis, succumbing to the illness within one month. This highlights the highly aggressive nature of SMARCA4-UT and underscores the significant challenges that remain in its treatment.
In this case, the patient presented with a large mass in the lung, local bronchial stenosis, and occlusion, accompanied by chronic bronchitis, bilateral emphysema, pulmonary bullae, pulmonary interstitial lesions, left ventricular enlargement, and aortic sclerosis. Upon admission due to abdominal pain, a pathological biopsy confirmed an undifferentiated tumor with the deficiency of SMARCA4 in the small bowel mesentery. Although the patient also had a large mass in the lung, a biopsy was not performed due to the patient’s poor cardiopulmonary function and refusal from both the patient and their family. This limitation restricted definitive pathological confirmation of the lung lesion. However, based on imaging findings and the size of the lung mass, the lung was strongly suspected to be the primary tumor, with widespread metastasis to the small bowel mesentery. At the time of diagnosis, the patient was already at an advanced stage, accompanied by pre-existing cardiopulmonary conditions. The patient eventually succumbed to sudden disturbance of consciousness, cardiac arrest, and respiratory failure. This case underscores the highly aggressive nature of SMARCA4-UT and its poor prognosis, emphasizing the critical need for early detection and more effective therapeutic strategies.
Conclusion
In conclusion, SMARCA4-UT is a rare and highly aggressive, undifferentiated tumor that presents significant challenges in treatment. Early detection and timely intervention are critical to improving patient prognosis. Routine BRG1 immunohistochemistry should be considered for all patients with pulmonary malignancies to identify the presence of SMARCA4-UT. This report highlights a unique case where the patient initially presented with gastrointestinal symptoms, including abdominal pain and bloating, without prominent respiratory symptoms. When encountering a large extrapulmonary mass, especially in middle-aged or elderly male patients with a history of smoking, chest imaging should be performed to evaluate for a potential thoracic primary tumor.
Acknowledgements
The authors would like to thank all the reviewers who participated in the review and thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Abbreviations
- SMARCA4-UT
SMARCA4-deficient undifferentiated tumor
- SMARCA4-DTS
SMARCA4-deficient thoracic sarcoma
- SMARCA4-NSCLC
SMARCA4-deficient non-small cell lung cancer
- CT
Computed tomography
- ESD
Endoscopic submucosal dissection
Author contributions
Writing–original draft: S L and XX T, Writing & editing: S L, JJ W. XX T and T X prepared all figures.All the authors have read & approved the final manuscript.
Funding
None.
Data availability
All the data regarding the findings are available within the manuscript.
Declarations
Ethics approval and consent to participate
This case report was approved by the Ethics Committee of the Affiliated Hospital of Zunyi Medical University. Written informed consent was obtained from the patient and the patient’s family for publication of this clinical case report.
Consent for publication
Written informed consent was obtained from the patient and the patient’s family for publication of this case report and any accompanying images.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Schallenberg S, Bork J, Essakly A, Alakus H, Buettner R, Hillmer AM, Bruns C, Schroeder W, Zander T, Loeser H, et al. Loss of the SWI/SNF-ATPase subunit members SMARCF1 (ARID1A), SMARCA2 (BRM), SMARCA4 (BRG1) and SMARCB1 (INI1) in oesophageal adenocarcinoma. BMC Cancer. 2020;20(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Le Loarer F, Watson S, Pierron G, de Montpreville VT, Ballet S, Firmin N, Auguste A, Pissaloux D, Boyault S, Paindavoine S, et al. SMARCA4 inactivation defines a group of undifferentiated thoracic malignancies transcriptionally related to BAF-deficient sarcomas. Nat Genet. 2015;47(10):1200–5. [DOI] [PubMed] [Google Scholar]
- 3.Yoshida ABJM, Loarer FL, et al. WHO classification of tumours of the lung, pleura, thymus and heart[M]. 5th ed. Lyon:IARC; 2021. pp. 111–4.
- 4.Chatzopoulos K, Boland JM. Update on genetically defined lung neoplasms: NUT carcinoma and thoracic SMARCA4-deficient undifferentiated tumors. Virchows Archiv: Int J Pathol. 2021;478(1):21–30. [DOI] [PubMed] [Google Scholar]
- 5.Medina PP, Carretero J, Fraga MF, Esteller M, Sidransky D, Sanchez-Cespedes M. Genetic and epigenetic screening for gene alterations of the chromatin-remodeling factor, SMARCA4/BRG1, in lung tumors. Genes Chromosomes Cancer. 2004;41(2):170–7. [DOI] [PubMed] [Google Scholar]
- 6.Khanchel F, Hedhili R, Zenaidi H, Helal I, Yahmadi A, Ben Néji H, Ksontini F, Ben Brahim E, Jouini R, Chadli A. SMARCA4-deficient thoracic sarcoma revealed by metastasis to the small intestine: a diagnostic dilemma. Gen Thorac Cardiovasc Surg. 2021;69(7):1155–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yoshida A, Kobayashi E, Kubo T, Kodaira M, Motoi T, Motoi N, Yonemori K, Ohe Y, Watanabe SI, Kawai A, et al. Clinicopathological and molecular characterization of SMARCA4-deficient thoracic sarcomas with comparison to potentially related entities. Mod pathology: official J United States Can Acad Pathol Inc. 2017;30(6):797–809. [DOI] [PubMed] [Google Scholar]
- 8.Zhu PP, Li JH, Liu XL, Du HY, Su J, Wang J. [Clinicopathological features of SMARCA4-deficient tumors]. Zhonghua bing li xue za zhi = Chinese. J Pathol. 2022;51(8):792–8. [DOI] [PubMed] [Google Scholar]
- 9.Perret R, Chalabreysse L, Watson S, Serre I, Garcia S, Forest F, Yvorel V, Pissaloux D, Thomas de Montpreville V, Masliah-Planchon J, et al. SMARCA4-deficient Thoracic Sarcomas: Clinicopathologic Study of 30 Cases With an Emphasis on Their Nosology and Differential Diagnoses. Am J Surg Pathol. 2019;43(4):455–65. [DOI] [PubMed] [Google Scholar]
- 10.Bishop JA, Westra WH. NUT midline carcinomas of the sinonasal tract. Am J Surg Pathol. 2012;36(8):1216–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haefliger S, Chervova O, Davies C, Nottley S, Hargreaves S, Sumathi VP, Amary F, Tirabosco R, Pillay N, Beck S, et al. Subclassification of epithelioid sarcoma with potential therapeutic impact. J Pathol. 2023;260(4):368–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xue Y, Meehan B, Macdonald E, Venneti S, Wang XQD, Witkowski L, et al. CDK4/6 inhibitors target SMARCA4-determined cyclin D1 deficiency in hypercalcemic small cell carcinoma of the ovary. Nat Commun. 2019;10(1):558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Romero OA, Vilarrubi A, Alburquerque-Bejar JJ, Gomez A, Andrades A, Trastulli D, Pros E, Setien F, Verdura S, Farré L, et al. SMARCA4 deficient tumours are vulnerable to KDM6A/UTX and KDM6B/JMJD3 blockade. Nat Commun. 2021;12(1):4319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shinno Y, Yoshida A, Masuda K, Matsumoto Y, Okuma Y, Yoshida T, Goto Y, Horinouchi H, Yamamoto N, Yatabe Y, et al. Efficacy of Immune Checkpoint Inhibitors in SMARCA4-Deficient Thoracic Tumor. Clin Lung Cancer. 2022;23(5):386–92. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the data regarding the findings are available within the manuscript.