Abstract
Background
Despite the significant prevalence of chronic obstructive pulmonary disease (COPD) in Southwest China, cognitive function among middle-aged and elderly individuals in this area surpasses the national average. This study aims to reveal the overall pulmonary ventilation function status of this population, and investigate whether pulmonary ventilation dysfunction is a risk factor for mild cognitive impairment (MCI) in this region, as suggested by previous researches.
Methods
Data were obtained from the 2019–2021 baseline survey of a natural population cohort study conducted in Southwest China. Pulmonary function was tested by experienced and well-trained medical personnel using a spirometer. The Mini-Mental State Examination was used to evaluate cognitive function. Subsequently, multiple logistic regression analysis was employed to examine the associations between pulmonary function and cognitive levels.
Results
A total of 2,337 middle-aged and elderly adults were included in this study, with 10.18% (238 individuals) classified as having mild cognitive impairment. According to the Chinese experts’ consensus on the standardization of adult lung function diagnosis, approximately 41.16% (962/2,337) of middle-aged and elderly individuals in Southwest China suffer from pulmonary ventilation dysfunction, predominantly mild (37.53%, 877/2,337), with the primary type being obstructive ventilation dysfunction (38.60%, 902/2,337; COPD: 14.21%, 332 participants). And 81.56% participants (1,906/2,337) were found to have small airway dysfunction. Multiple logistic regression analyses showed that individuals with poor pulmonary ventilation function (PPF) were associated with an increased risk of MCI (OR [95% CI]: 1.38 [1.04, 1.83], P = 0.026). Moreover, the more severe the pulmonary ventilation dysfunction, the higher the risk of cognitive impairment (P for trend = 0.009). Similar association were found between PPF and MCI when we use ATS/ERS technical standards. No significant association was observed between small airway dysfunction and cognitive impairment (OR [95% CI]: 1.05 [0.72, 1.56], P = 0.819).
Conclusions
The pulmonary function status of middle-aged and elderly individuals in Southwest China requires attention, particularly regarding obstructive pulmonary ventilation dysfunction. We recommend integrating pulmonary health assessments into routine care for these populations to raise awareness of lung health, improve lung function, and ultimately enhance cognitive function.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12890-024-03403-0.
Keywords: Pulmonary ventilation function, Lung function, Cognitive function, Mild cognitive impairment
Background
With the intensifying trend of population aging [1], elderly health issues have garnered widespread attention. Among these, cognitive function problems, such as mild cognitive impairment (MCI) and dementia, have been regarded as a global health priority for the elderly by the WHO [2]. According to the WHO’s 2019 report on the leading causes of global deaths, dementia ranked seventh [3]. And it is projected that the number of dementia patients worldwide will increase from 54.7 million in 2019 to 152.8 million by 2050 [4]. The progression of dementia can be divided into three stages: the preclinical phase, mild cognitive impairment, and the dementia stage [5, 6]. Due to the lack of effective treatments [3], once patients enter the dementia stage, the disease course becomes irreversible. Therefore, the reversible MCI stage is a critical juncture for intervention and prevention of dementia. Identifying modifiable risk factors during the MCI stage may be one of the most effective strategies to delay the onset of dementia.
Previous epidemiological studies have shown that poor lung function is associated with cognitive decline and an increased risk of dementia [7–12]. Impaired lung function may affect cognitive function through mechanisms such as mediating chronic hypoxemia, systemic inflammation, oxidative stress, cerebral arteriosclerosis, and vascular injury [13]. However, some inconsistent findings remain [14, 15]. To date, evidence from mainland China is relatively limited [16, 17]. Furthermore, most studies have focused on dementia as the outcome measure, with limited attention to the reversible stage of mild cognitive impairment (MCI) [8, 10, 15]. Additionally, the evaluation of lung function in these studies has often centered on chronic obstructive pulmonary disease (COPD) [10, 18] or some lung function indicators [7, 11], with few comprehensive assessments of pulmonary ventilation function [8]. Therefore, it is essential to explore the association between the overall pulmonary ventilation function and MCI in mainland China.
Pulmonary function tests are considered the gold standard for diagnosing pulmonary ventilation dysfunction. However, reports indicated that the rate of pulmonary function testing among Chinese residents aged 40 and above was only 6.7% in 2019–2020 [19]. Consequently, the awareness rate of pulmonary function impairment among middle-aged and elderly individuals in China is generally low, with only 0.9% for COPD [20]. Due to differences in environment and lifestyle [21, 22], pulmonary function levels seems to vary among populations in different regions of China. For instance, in the case of chronic obstructive pulmonary disease (COPD), data from the Chinese Center for Disease Control and Prevention in 2018 indicated that the prevalence of COPD among individuals aged 40 and above is highest in the Southwest region at 20.2%, and lowest in the Central region at 10.2% [20]. To the best of our knowledge, no studies have reported in detail the real-world status of pulmonary ventilation function, such as the proportion, types, and severity of pulmonary ventilation dysfunctions, among middle-aged and elderly individuals over 45 years old in Southwest China.
Sichuan Province, located in Southwest China, has been reported to have a relatively superior cognitive function status among its population compared to the national average, with the prevalence of dementia in adults aged 60 years or older being approximately 4.74% (average: 6.0%) [23]. However, the prevalence of COPD, one of the most common type of pulmonary ventilation dysfunction, in this region, seems to be higher than the national average (Sichuan 16.11% vs. average 8.60%) [24, 25]. We are curious whether pulmonary ventilation dysfunction in this region remains a potential risk factor for cognitive impairment, as suggested by previous studies. Therefore, based on the natural population cohort established by West China Hospital of Sichuan University, this study aimed to comprehensively reveal the characteristics of pulmonary ventilation function status in people over 45 years old in this region and its association with cognitive function from the aspects of the type and severity of pulmonary ventilation dysfunction. The findings may help identify modifiable risk factors for cognitive decline and provide a theoretical basis for the prevention and control of cognitive impairment.
Methods
Study design and data sources
We conducted a cross-sectional study, and the data were obtained from the baseline survey of the Natural Population Cohort Study of West China Hospital, Sichuan University (No.ChiCTR1900024623) [26]. Residents over the age of 20 from communities in Sichuan Province were invited to voluntarily participate in this cohort study. Baseline data were gathered through structured questionnaires, biological sample collections, and physical/clinical examinations. So far, the cohort has completed its baseline survey in the cities of Chengdu, Mianzhu, and Ganzi between 2019 and 2021.
This study included baseline participants who have completed the assessment of cognitive function and lung function. Individuals who lacked information on some key covariates (such as smoking status, and history of neurological or respiratory diseases) were excluded. The study was approved by the ethical community of West China Hospital, Sichuan University, and all participants signed informed consent forms.
Measurement of pulmonary function
Pulmonary function was tested using a spirometer (Jaeger-MasterScreen Pneumo, Germany). Participants who screened positive for major contraindications to spirometry, such as myocardial infarction, stroke or shock in the past three months, were excluded. The examination was conducted in a relatively quiet, well-ventilated environment with stable temperature and humidity. The procedure was carried out by medical personnel with relevant operational experience who had passed the necessary assessments. Each participant’s test was repeated at least three times, and the results meeting quality control standards were used as the final pulmonary function parameter values. Through this examination, we obtained the following parameters: FVC (Forced Vital Capacity), FEV1 (Forced Expiratory Volume in one second), FEV1/FVC, MMEF25 − 75% (Maximal Mid-Expiratory Flow between 75% and 25% of the FVC), MEF50% (Maximal Expiratory Flow at 50% of the FVC), and MEF25% (Maximal Expiratory Flow at 25% of the FVC).
According to the Chinese experts’ consensus on the standardization of adult lung function diagnosis [27], we defined participants’ pulmonary ventilation function as follows: (1) Obstructive ventilatory dysfunction: FEV1/FVC% pred < 92%. (2) Restrictive ventilatory dysfunction: FVC% pred < 80%. (3) Mixed ventilatory dysfunction: Both of the above criteria are met simultaneously. (4) Normal pulmonary ventilation function: None of the above criteria are met. Furthermore, we classified individuals with any ventilatory dysfunction as having poor pulmonary function (PPF), while the others were classified as having normal pulmonary function (NPF). Additionally, according to commonly used standards by clinicians in China, we graded the severity of lung function impairment in the PPF group based on FEV1% pred: mild impairment for FEV1% pred > = 70% and moderate-to-severe impairment for FEV1% pred < 70% [28]. To assess small airway dysfunction, we utilized MMEF25 − 75%, MEF50%, and MEF25%. A diagnosis of small airway dysfunction was made when at least two of these three indicators were less than 65% of predicted values [29]. In addition, we assessed COPD based on the Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria [30]: (1) Non-COPD: FEV1/FVC ≥ 0.7; (2) COPD: FEV1/FVC < 0.7.
To facilitate sensitivity analyses, we reclassified pulmonary ventilation function according to ATS/ERS technical standards [31]: (1) Obstructive ventilatory dysfunction: FEV1/FVC < LLN (the lower limit of normal). (2) Restrictive ventilatory dysfunction: FVC < LLN. (3) Mixed ventilatory dysfunction: Both criteria are met simultaneously. (4) Normal pulmonary ventilation function: absence of restrictive or obstructive impairment. The LLN values were calculated using the formula applicable to the Chinese population, incorporating age, sex, and height [32]. The severity of ventilatory dysfunction was graded using Z-scores [31].
Assessment of cognitive function
We used the Mini-Mental State Examination (MMSE) to evaluate the cognitive function of participants [33]. This scale has good reliability and validity [34] and is completed under the guidance of two professionals in a quiet environment, using unified terminology. The total score of MMSE ranges from 0 to 30, and a higher score indicates better cognitive function. In this study, an MMSE score of less than 24 was defined as MCI [35].
Measurement of covariates
Structured questionnaire [26] was used to collect information of covariates including age, gender, occupation, marital status, education level, drinking status, smoking status, leisure-time physical activity (LTPA), live alone, eat alone, status of depression, anxiety, and history of diabetes, hypertension, cancer, dyslipidemia, nervous system disease, and respiratory disease. Besides, fasting blood was collected for biochemical detection to evaluate the health status, such as dyslipidemia and diabetes. Objective measurements were used to assess the status of body mass index (BMI) and hypertension. To identify hypertension, diabetes, or dyslipidemia, either a positive self-report by the participant or a positive clinical test result was sufficient. Overweight was defined as a BMI ≥ 24.
Statistical analysis
Data were expressed as frequency (percentage) and median (interquartile range, IQR) for baseline characteristics. Nonparametric tests for continuous variables and chi-square tests for categorical variables were performed to compare the differences in baseline characteristics across different pulmonary function groups. Multiple logistic regression models were used to test the relationship between pulmonary function and cognitive function, and the variables with a p-value < 0.1 in univariate analysis were selected as potential confounding variables in the model. Further subgroup analyses were conducted according to age, gender, smoking status, drinking status, LTPA level, and history of pulmonary diseases. Additionally, we reassessed the level of pulmonary ventilation function according to ATS/ERS standards and conducted sensitivity analyses to explore the robustness of the association between pulmonary ventilation function and cognitive function. All analyses were performed using R 4.1.2 software, and 2-sided p-values < 0.05 were considered statistically significant.
Results
Participant characteristics
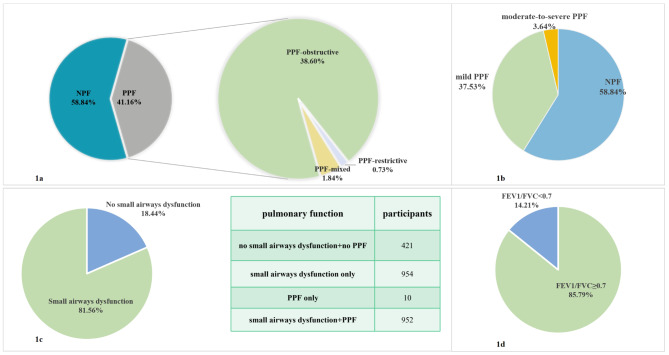
A total of 2,337 subjects were included in the analyses. Among them, 238 individuals (10.18%) were classified as having mild cognitive impairment. Based on the classification standards for pulmonary ventilation function outlined in the Chinese expert consensus, 41.16% (962 participants) were classified as having poor pulmonary function (PPF). The breakdown of PPF was as follows: 38.60% (902 participants) were identified with obstructive ventilatory dysfunction (COPD: 14.21%, 332 participants), 0.73% (17 participants) had restrictive ventilatory dysfunction, and 1.84% (43 participants) had mixed ventilatory dysfunction (Fig. 1). Regarding the severity of lung function impairment, 37.53% (877 participants) had mild PPF, and 3.64% (85 participants) had moderate-to-severe PPF. Additionally, a high proportion of participants, 81.56% (1,906 participants), were found to have small airway dysfunction. Based on the ATS/ERS technical standards for pulmonary function classification, the ventilatory function status of the enrolled population is shown in Supplementary Fig. 1.
Fig. 1.
Characteristics of pulmonary ventilation function of the study participants (classified according to Chinese expert consensus). a. Distribution of pulmonary function status in study participants. b. Severity distribution of pulmonary function impairment. c. Distribution of small airway dysfunction prevalence. d. Distribution of COPD (FEV1/FVC < 0.7) status. NPF, normal pulmonary function; PPF, poor pulmonary function; PPF-obstructive, obstructive ventilatory dysfunction; PPF-restrictive, restrictive ventilatory dysfunction; PPF-mixed, mixed ventilatory dysfunction
The median ages were both 59 years for participants with normal and poor pulmonary function (Table 1). Participants with PPF status seemed to have higher proportion of MCI (12.37% VS 8.65%). In addition, there were significant differences in gender, education level, BMI, and history of respiratory disease between the participants with NPF and PPF status (P < 0.05).
Table 1.
Characteristics of study participants
| Variables | NPF(n = 1375) | PPF(n = 962) | Z/χ2 | P |
|---|---|---|---|---|
| Age (years), median [q1, q3] | 59 [54, 65] | 59 [54, 66] | -0.83 | 0.404 |
| Gender, n (%) | 4.80 | 0.028 | ||
| Male | 447 (32.51) | 271 (28.17) | ||
| Female | 928 (67.49) | 691 (71.83) | ||
| Education, n (%) | 13.55 | 0.004 | ||
| Primary school and below | 447 (32.51) | 363 (37.73) | ||
| Middle school | 578 (42.04) | 379 (39.40) | ||
| High school or vocational high school | 253 (18.40) | 180 (18.71) | ||
| College and above | 97 (7.05) | 40 (4.16) | ||
| Marital status, n (%) | 0.06 | 0.812 | ||
| Unmarried/divorced | 131 (9.53) | 88 (9.15) | ||
| Married/cohabitation | 1244 (90.47) | 874 (90.85) | ||
| Occupation, n (%) | 2.05 | 0.152 | ||
| None | 1052 (76.51) | 761 (79.11) | ||
| In work | 323 (23.49) | 201 (20.89) | ||
| Smoking, n (%) | 1.87 | 0.393 | ||
| Never | 1152 (83.78) | 786 (81.70) | ||
| Ever | 103 (7.49) | 78 (8.11) | ||
| Current | 120 (8.73) | 98 (10.19) | ||
| Passive smoking, n (%)* | 0.83 | 0.363 | ||
| No | 959 (74.11) | 681 (75.92) | ||
| Yes | 335 (25.89) | 216 (24.08) | ||
| Drinking, n (%) | 2.27 | 0.321 | ||
| Never | 964 (70.11) | 702 (72.97) | ||
| Ever | 202 (14.69) | 127 (13.20) | ||
| Current | 209 (15.20) | 133 (13.83) | ||
| Live alone, n (%) | 0.44 | 0.509 | ||
| No | 1274 (92.65) | 899 (93.45) | ||
| Yes | 101 (7.35) | 63 (6.55) | ||
| Eat alone, n (%) | 0.05 | 0.821 | ||
| No | 1250 (90.91) | 878 (91.27) | ||
| Yes | 125 (9.09) | 84 (8.73) | ||
| Physical activity, n (%) | 2.32 | 0.128 | ||
| < 11.25 MET-hours/week | 453 (32.95) | 347 (36.07) | ||
| >=11.25 MET-hours/week | 922 (67.05) | 615 (63.93) | ||
| Body mass index, n (%) | 12.88 | <0.001 | ||
| < 24 kg/m2 | 583 (42.40) | 481 (50.00) | ||
| >=24 kg/m2 | 792 (57.60) | 481 (50.00) | ||
| Depression, n (%) | 0.40 | 0.528 | ||
| No | 1299 (94.47) | 902 (93.76) | ||
| Yes | 76 (5.53) | 60 (6.24) | ||
| Anxiety, n (%) | 0.15 | 0.697 | ||
| No | 1293 (94.04) | 900 (93.56) | ||
| Yes | 82 (5.96) | 62 (6.44) | ||
| Diabetes, n (%) | 2.13 | 0.144 | ||
| No | 1210 (88.00) | 866 (90.02) | ||
| Yes | 165 (12.00) | 96 (9.98) | ||
| Hypertension, n (%) | 1.05 | 0.306 | ||
| No | 803 (58.40) | 583 (60.60) | ||
| Yes | 572 (41.60) | 379 (39.40) | ||
| Dyslipidemia, n (%) | 3.79 | 0.052 | ||
| No | 418 (30.40) | 330 (34.30) | ||
| Yes | 957 (69.60) | 632 (65.70) | ||
| Cancer, n (%) | 1.01 | 0.314 | ||
| No | 1351 (98.25) | 951 (98.86) | ||
| Yes | 24 (1.75) | 11 (1.14) | ||
| Nervous system disease, n (%) | 0.03 | 0.869 | ||
| No | 1251 (90.98) | 878 (91.27) | ||
| Yes | 124 (9.02) | 84 (8.73) | ||
| Respiratory disease, n (%) | 16.09 | < 0.001 | ||
| No | 1252 (91.05) | 824 (85.65) | ||
| Yes | 123 (8.95) | 138 (14.35) | ||
| MCI, n (%) | 8.14 | 0.004 | ||
| No | 1256 (91.35) | 843 (87.63) | ||
| Yes | 119 (8.65) | 119 (12.37) |
Notes: MCI, mild cognitive impairment; NPF, normal pulmonary function; PPF, poor pulmonary function
*only 2191 participants reported passive smoking status
Association between pulmonary ventilation function and mild cognitive impairment among middle-aged and older adults in Southwest China
Multiple logistic regression analyses showed that individuals with poor pulmonary ventilation function were associated with an increased risk of MCI (OR [95% CI]: 1.38 [1.04, 1.83], P = 0.026, Table 2). Furthermore, higher severity of lung dysfunction seemed to be associated with a higher risk of MCI (OR [95% CI] for mild impairment: 1.33 [0.99, 1.79], P = 0.061; OR [95% CI] for moderate to severe impairment: 2.10 [1.07, 3.96], P = 0.026; P for trend = 0.009). Regarding the types of ventilatory dysfunction, we found that individuals with obstructive pulmonary ventilation dysfunction had a higher risk of MCI compared to those without ventilatory dysfunction (OR [95% CI]: 1.35 [1.01, 1.79], P = 0.040). Similar results were found in individuals with COPD (OR [95% CI]: 1.60 [1.09, 2.32], P = 0.014). However, no significant association was observed in individuals with restrictive ventilatory dysfunction (OR [95% CI]: 1.76 [0.80, 3.54], P = 0.135). Additionally, no significant association was found between small airway dysfunction and MCI (OR [95% CI]: 1.05 [0.72, 1.56], P = 0.819).
Table 2.
The association between pulmonary ventilation function and mild cognitive impairment
| Pulmonary Function | No. of controls/cases (n = 2099/238) |
OR (95%CI) | P |
|---|---|---|---|
| Pulmonary ventilation function1 | |||
| NPF | 1256/119 | 1.00 | |
| PPF | 843/119 | 1.38 (1.04, 1.83) | 0.026 |
| Pulmonary ventilation function2 | |||
| Normal | 1256/119 | 1.00 | |
| Mild impairment | 774/103 | 1.33 (0.99, 1.79) | 0.061 |
| Moderate to severe impairment | 69/16 | 2.10 (1.07, 3.96) | 0.026 |
| Obstructive pulmonary ventilation dysfunction3 | |||
| No | 1270/122 | 1.00 | |
| Yes | 829/116 | 1.35 (1.01, 1.79) | 0.040 |
| COPD4 | |||
| No | 1823/182 | 1.00 | |
| Yes | 276/56 | 1.60 (1.09, 2.32) | 0.014 |
| Restrictive pulmonary ventilation dysfunction5 | |||
| No | 2049/228 | 1.00 | |
| Yes | 50/10 | 1.76 (0.80, 3.54) | 0.135 |
| Small airways dysfunction6 | |||
| No | 394/37 | 1.00 | |
| Yes | 1705/201 | 1.05 (0.72, 1.56) | 0.819 |
Model 1: adjusted for gender, education level, BMI, and history of respiratory disease and dyslipidemia. Model 2: adjusted for gender, age, education level, BMI, smoking, anxiety, and history of respiratory disease and dyslipidemia. Model 3: adjusted for gender, education level, BMI and history of respiratory disease and dyslipidemia. Model 4: adjusted for gender, age, education level, smoking, drinking, and history of hypertension, diabetes, respiratory disease and dyslipidemia. Model 5: adjusted for gender, age, smoking, and history of respiratory disease and hypertension. Model 6: adjusted for gender, education level, and history of respiratory disease and dyslipidemia. NPF, normal pulmonary function; PPF, poor pulmonary function
Results from sensitivity analysis indicated that when applying the ATS/ERS technical standards for pulmonary function assessment, ventilatory dysfunction remained positively associated with MCI (OR [95% CI]: 1.47 [1.04, 2.07], P = 0.029, Supplementary Table 2). This association was primarily evident in individuals with obstructive ventilatory dysfunction (OR [95% CI]: 1.54 [1.04, 2.55], P = 0.027). Moreover, a greater severity of obstruction was linked to an increased risk of MCI (OR [95% CI] for mild impairment: 1.34 [0.81, 2.16], P = 0.235; OR [95% CI] for moderate to severe impairment: 1.87 [1.08, 3.18], P = 0.023; P for trend = 0.014).
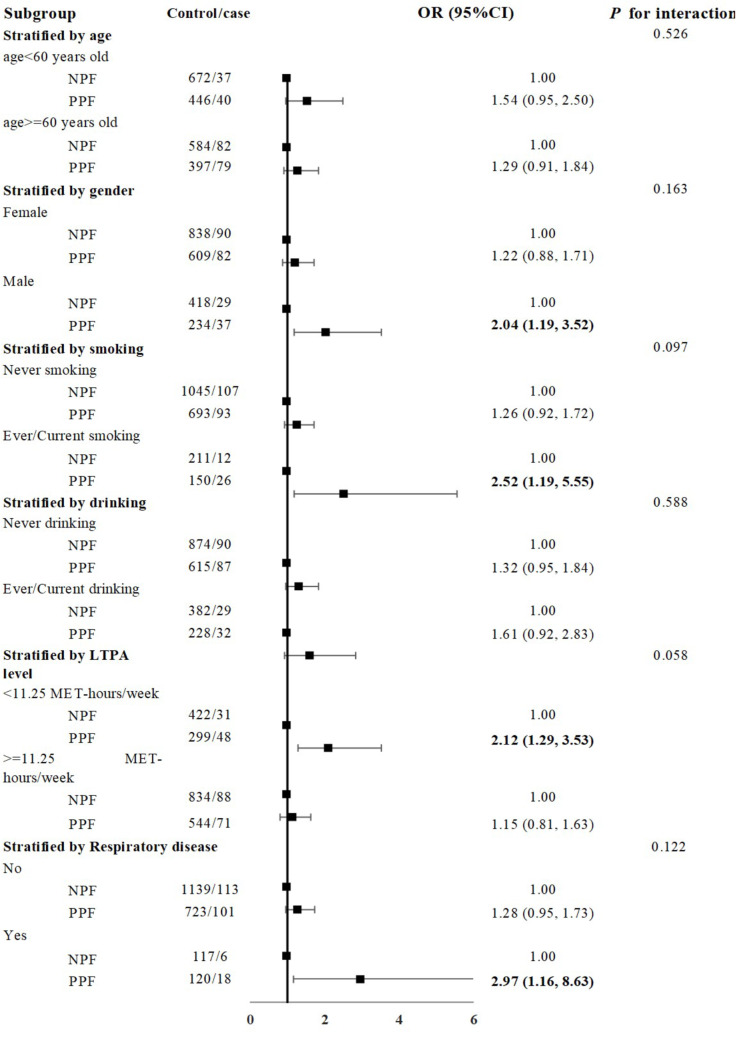
Subgroup analysis
Although there was no statistically significant difference in the correlation between pulmonary function levels and the risk of MCI when stratified by age, gender, smoking status, drinking status, LTPA level or history of respiratory disease (all P for interaction > 0.05), the association seemed to be more obvious in males, ever/current smoker, those with an LTPA level < 11.25 MET-hours/week, and those with a history of respiratory disease (Fig. 2).
Fig. 2.
Subgroup analysis. All models were adjusted for education level, BMI, history of dyslipidemia, and (where appropriate) gender, and history of respiratory diseases. NPF, normal pulmonary function; PPF, poor pulmonary function
Discussion
This study is the first to assess the overall pulmonary ventilation function status and its association with cognitive function among middle-aged and elderly populations in Southwest China under real-world conditions. We found that the lung function health of individuals aged 45 and above in this region should not be overlooked, and that pulmonary ventilation dysfunction is associated with a higher risk of mild cognitive impairment.
Overall status of pulmonary ventilation dysfunction in Southwest China
Based on Chinese experts’ consensus on the standardization of adult lung function diagnosis, our study revealed that approximately 41.16% (962/2337) of middle-aged and elderly individuals in Southwest China suffer from pulmonary ventilation dysfunction, predominantly mild (91.16%, 877/962), with the primary type being obstructive ventilation dysfunction (93.76%, 902/962). Previous research also indicates that the prevalence of obstructive ventilation dysfunction is higher than that of restrictive dysfunction [8, 36]. Obstructive pulmonary ventilation dysfunction refers to the obstruction of airflow in the bronchi and bronchioles, encompassing diseases such as chronic obstructive pulmonary disease (COPD), asthma, bronchiectasis, and cystic fibrosis [37]. Among these, COPD contributes the most significant disease burden [25, 38], yet the awareness rate among patients is less than 2% [24]. Research has highlighted that by the time asymptomatic and unaware COPD patients experience symptoms such as shortness of breath, their lung function may already be impaired by more than 50%, suggesting a missed opportunity for optimal intervention [39]. Therefore, it is imperative to implement measures to improve the level of pulmonary function testing among residents aged 40 and above, especially high-risk groups for chronic respiratory diseases, to increase their awareness of lung function status.
Relationship between pulmonary ventilation dysfunction and MCI
Despite middle-aged and elderly individuals in this region exhibiting relatively poor lung function but relatively good cognitive function compared to the national average, our study still found that impaired pulmonary ventilation may be a potential risk factor for MCI. Following sensitivity analysis using the ATS/ERS standards, ventilatory dysfunction remained positively associated with MCI, reinforcing the robustness of this relationship. The study suggests that hypoxia resulting from ventilatory impairment may impact the activity of oxygen-dependent enzymes crucial for synthesizing neurotransmitters such as acetylcholine, potentially leading to neuronal dysfunction [40]. Additionally, systemic inflammation associated with ventilatory dysfunction may damage the central nervous system via the cyclooxygenase pathway, with sustained inflammatory responses accelerating neurodegenerative changes and impairing cognitive function [41–43]. Previous research has reported that individuals with impaired lung function could exhibit greater overall and frontal-parietal grey matter loss, as well as higher volumes of white matter hyperintensities [8], thus contributing to cognitive decline [44–46]. Although previous studies have suggested that the association between lung function and cognitive function may be partly due to shared risk factors [47], such as older age, lower educational level, smoking, and lack of physical activity [22, 25, 48], our study found that even after controlling for these confounding factors, the association remained significant. This suggests a potentially independent relationship between poor lung function and cognitive decline. Furthermore, a study found that COPD patients have a significantly greater proportion of individuals with motoric cognitive risk (MCR) syndrome compared to healthy subjects and asthmatics, indicating possible interconnections between the brain and pulmonary system and skeletal muscle [49].
Unlike other regions, Sichuan province in Southwest China is known for its leisure culture and slow-paced lifestyle [50]. Sichuan residents, particularly the elderly who have more free time, enjoy gathering for tea and playing mahjong [50]. Simultaneously, they place a strong emphasis on physical activity, often going for evening walks or engaging in square dancing with friends or partners, resulting in higher physical activity levels than the national average [51]. This lifestyle, characterized by an emphasis on both physical exercise and social interaction, is beneficial for cognitive function [51, 52]. It may help us understand why, despite having poorer lung function, the cognitive levels of the middle-aged and elderly in this region are higher than the national average. Based on these findings, we recommend that middle-aged and elderly individuals prioritize lung health and actively engage in physical activities and social interactions to enhance their cognitive function. Additionally, considering the detrimental effects of air pollution and smoking on lung and cognitive function [16, 53], we urge policymakers to take proactive measures to control air pollution and improve air quality, as well as to implement community-based pulmonary rehabilitation programs and smoking cessation support to enhance residents’ lung health.
Our further analysis found that the positive association between PPF and MCI was only observed in the obstructive PPF group and not in the restrictive PPF group, while previous researches have shown that both restrictive and obstructive pulmonary ventilation dysfunctions are associated with an increased risk of cognitive impairment [8, 36]. The discrepancy in our study might be attributed to the sample size and the lower detection rate of restrictive PPF in our participants.
Small airway dysfunction and its relationship with MCI
Our study also found that the prevalence of small airway dysfunction among middle-aged and elderly individuals in Southwest China is as high as 81.56%. A national cross-sectional study similarly reported that the prevalence of small airway dysfunction among Chinese individuals aged 45 and above ranges from approximately 50–80%, with an increasing prevalence with advancing age [54]. However, our study did not find an association between small airway dysfunction and cognitive impairment. This may be because small airway dysfunction is considered a precursor to COPD and asthma [54]. Initially, the obstruction in these airways leads to minimal measurable changes in airway resistance. It is only in the later stages of the disease that small airway obstruction may disproportionately harm lung function [55]. For our study participants with small airway dysfunction (1906 participants), 50.05% (954/1906) had isolated small airway dysfunction, while approximately 49.95% (952/1906) had concomitant pulmonary ventilation dysfunction, the vast majority of which was mild and in the early stages of the disease. Therefore, the impact of small airway dysfunction on lung ventilation function and blood oxygen levels may not have been evident, explaining the lack of a significant association with cognitive impairment. Nonetheless, as a precursor symptom, small airway dysfunction can provide an important early warning for potential lung function impairment.
Findings from subgroup analysis
Previous studies have shown that individuals who smoke or have a history of respiratory diseases are more likely to experience impaired lung function [25]. Additionally, males, due to higher smoking rates and higher likelihood of occupational exposures to dust, are at a greater risk for compromised lung function. Therefore, the association between lung function and cognitive function may be more detectable in these groups. It is known that moderate physical activity is a protective factor for cognitive function [22]. Our study showed a significant association between pulmonary ventilation dysfunction and cognitive impairment among those lacking physical activity, whereas this association was not statistically significant in individuals actively engaging in physical activity. These findings suggest that for middle-aged and elderly individuals with impaired lung function, encouraging regular physical exercise, smoking cessation, and minimizing occupational dust exposure could be effective measures to improve lung function and cognitive levels in this population.
Limitations and future research directions
There are several limitations to this study. First, as a cross-sectional study, it does not allow for the inference of causal relationships between lung function decline and cognitive impairment. Second, we primarily utilized pulmonary ventilation function criteria from the Chinese expert consensus, which, while widely employed by clinicians in China for lung function diagnosis, has not been broadly recognized internationally. However, even when applying the ATS/ERS standard for classifying pulmonary ventilation function, the main results remained unchanged, thereby reflecting the robustness of our findings from an alternative perspective. Third, similar to the China Kadoorie Biobank study, our participants did not inhale bronchodilators before undergoing pulmonary function tests, which may affect the accuracy of estimating the detection rate of pulmonary ventilation dysfunction [56]. Fourth, although only three cities in Sichuan Province were surveyed, we took into account regions with different income levels to maximize the representation of participants with limited resources. Despite these limitations, this study revealed the real-world status of pulmonary ventilation function among middle-aged and older people in Southwest China from multiple dimensions and demonstrated the positive association between lung function and cognitive function. Our results will help expand the list of modifiable risk factors for MCI and provide a reference for the development of early warning and prevention strategies for MCI in the future. Additionally, future research could consider enhancing pulmonary measurements, such as employing bronchodilators during lung function tests; measuring carbon monoxide and other pollutants in the blood and investigating their roles in inflammatory damage to airways, blood vessels, immune cells, and neurons.
Conclusions
The lung health status of middle-aged and elderly individuals in Southwest China warrants attention, especially the prevalence of obstructive pulmonary ventilation dysfunction. Poor pulmonary ventilation function is associated with a higher risk of cognitive impairment, and early intervention in lung health maye serve as a viable strategy for mitigating cognitive decline. We recommend incorporating pulmonary health assessments into routine care for these populations to enhance awareness of lung health, improve lung function, and subsequently boost cognitive function.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank all participants of this study.
Author contributions
X.L. contributed to the conception, design, analysis, and manuscript preparation. L.L. contributed to the design and data analysis. S.M.J. and A.J.P. contributed to the data collection and manuscript revision. L.C. contributed to the conception and revised the final draft of the manuscript.
Funding
This work was supported by Sichuan Science and Technology Program (2023ZYD0075) and National Natural Science Foundation of China (82201752) . The funder had no role in the study design, data collection, analysis, data interpretation or manuscript preparation.
Data availability
The datasets of the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the ethical community of West China Hospital, Sichuan University. We confirmed that all methods were performed in accordance with relevant guidelines and regulations to protect human subjects. All participants read and signed written informed consent forms.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Abbreviations
PPF poor pulmonary function.
NPF normal pulmonary function.
MCI mild cognitive impairment.
COPD chronic obstructive pulmonary disease.
FVC Forced Vital Capacity.
FEV1 Forced Expiratory Volume in one second.
MMEF25 − 75% Maximal Mid-Expiratory Flow between 75% and 25% of the FVC.
MEF50% Maximal Expiratory Flow at 50% of the FVC.
MEF25% Maximal Expiratory Flow at 25% of the FVC.
MMSE Mini-Mental State Examination.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Aging. and Health [https://www.who.int/zh/news-room/fact-sheets/detail/ageing-and-health]
- 2.Wortmann M. Dementia: a global health priority - highlights from an ADI and World Health Organization report. Alzheimers Res Ther. 2012;4(5):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dementia. [ https://www.who.int/zh/news-room/fact-sheets/detail/dementia]
- 4.Estimation of the global prevalence of dementia. In 2019 and forecasted prevalence in 2050: an analysis for the global burden of Disease Study 2019. Lancet Public Health. 2022;7(2):e105–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.2024 ALZHEIMER’S DISEASE FACTS AND FIGURES. [https://www.alz.org/media/Documents/alzheimers-facts-and-figures.pdf] [DOI] [PMC free article] [PubMed]
- 6.Impairment CSoDaC. [Chinese expert consensus on the diagnosis and treatment of mild cognitive impairment due to Alzheimer′s disease 2021]. Chin J Neurol 2022, 55(5).
- 7.Wang J, Dove A, Song R, Qi X, Ma J, Bennett DA, Xu W. Poor pulmonary function is associated with mild cognitive impairment, its progression to dementia, and brain pathologies: a community-based cohort study. Alzheimer’s Dement J Alzheimer’s Assoc. 2022;18(12):2551–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhou L, Yang H, Zhang Y, Li H, Zhang S, Li D, Ma Y, Hou Y, Lu W, Wang Y. Association of impaired lung function with dementia, and brain magnetic resonance imaging indices: a large population-based longitudinal study. Age Ageing 2022, 51(11). [DOI] [PubMed]
- 9.Liao KM, Ho CH, Ko SC, Li CY. Increased risk of dementia in patients with Chronic Obstructive Pulmonary Disease. Medicine. 2015;94(23):e930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liao WC, Lin CL, Chang SN, Tu CY, Kao CH. The association between chronic obstructive pulmonary disease and dementia: a population-based retrospective cohort study. Eur J Neurol. 2015;22(2):334–40. [DOI] [PubMed] [Google Scholar]
- 11.Donahue PT, Xue QL, Carlson MC. Peak Expiratory Flow Predicts Incident Dementia in a Representative Sample of U.S. older adults: the National Health and Aging trends Study (NHATS). Journals Gerontol Ser Biol Sci Med Sci. 2023;78(8):1427–35. [DOI] [PMC free article] [PubMed]
- 12.Duong M, Usman A, Ma J, Xie Y, Huang J, Zaman M, Dragoman A, Jiatong Chen S, Farooqi M, Raina P. Associations between lung function and physical and cognitive health in the Canadian longitudinal study on aging (CLSA): a cross-sectional study from a multicenter national cohort. PLoS Med. 2022;19(2):e1003909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dodd JW. Lung disease as a determinant of cognitive decline and dementia. Alzheimers Res Ther. 2015;7(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Higbee DH, Granell R, Hemani G, Smith GD, Dodd JW. Lung function, COPD and cognitive function: a multivariable and two sample mendelian randomization study. BMC Pulm Med. 2021;21(1):246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sibbett RA, Russ TC, Allerhand M, Deary IJ, Starr JM. Physical fitness and dementia risk in the very old: a study of the Lothian Birth Cohort 1921. BMC Psychiatry. 2018;18(1):285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ye Z, Li X, Lang H, Fang Y. Long-term PM2.5 exposure, lung function, and cognitive function among Middle-aged and older adults in China. Journals Gerontol Ser Biol Sci Med Sci. 2023;78(12):2333–41. [DOI] [PubMed] [Google Scholar]
- 17.Shang X, Scott D, Chan RK, Zhang L, He M. Association of pulmonary function with Cognitive decline in older adults: a Nationwide Longitudinal Study in China. Journals Gerontol Ser Biol Sci Med Sci. 2021;76(8):1423–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiao T, Wijnant SRA, Licher S, Terzikhan N, Lahousse L, Ikram MK, Brusselle GG, Ikram MA. Lung function impairment and the risk of Incident Dementia: the Rotterdam Study. J Alzheimer’s Disease: JAD. 2021;82(2):621–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tong H, Cong S, Fang LW, Fan J, Wang N, Zhao QQ, Wu J. [Performance of pulmonary function test in people aged 40 years and above in China, 2019–2020]. Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua liuxingbingxue zazhi 2023, 44(5):727–34. [DOI] [PubMed]
- 20.Prevalence of chronic obstructive pulmonary. Disease (COPD) in Chinese residents aged 40 years and above [https://ncncd.chinacdc.cn/xwz/zxdt/201812/t20181203_197848.htm]
- 21.Lung Cancer Risk Factors. [https://www.cancer.org/cancer/types/lung-cancer/causes-risks-prevention/risk-factors.html]
- 22.Chronic obstructive pulmonary disease. Risk factors and risk reduction [https://www.uptodate.com/contents/zh-Hans/chronic-obstructive-pulmonary-disease-risk-factors-and-risk-reduction]
- 23.Jia L, Du Y, Chu L, Zhang Z, Li F, Lyu D, Li Y, Li Y, Zhu M, Jiao H, et al. Prevalence, risk factors, and management of dementia and mild cognitive impairment in adults aged 60 years or older in China: a cross-sectional study. Lancet Public Health. 2020;5(12):e661–71. [DOI] [PubMed] [Google Scholar]
- 24.World COPD, Day. The lung is life [https://www.sccdc.cn/Article/View?id=32426]
- 25.Wang C, Xu J, Yang L, Xu Y, Zhang X, Bai C, Kang J, Ran P, Shen H, Wen F, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet (London England). 2018;391(10131):1706–17. [DOI] [PubMed] [Google Scholar]
- 26.Fan P, Zhang S, Wang W, Yang Z, Tan W, Li S, Zhu C, Hu D, Zhou X, Tian Z, et al. The design and implementation of natural population cohort study Biobank: a multiple-center project cooperation with medical consortia in Southwest China. Front Public Health. 2022;10:996169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhu L, Chen RC. [Chinese experts’ consensus on the standardization of adult lung function diagnosis]. J Clin Pulmonary Med 2022, 27(7).
- 28.Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, Coates A, van der Grinten CP, Gustafsson P, Hankinson J, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005;26(5):948–68. [DOI] [PubMed] [Google Scholar]
- 29.Association CM, House CMJP, Practice CSG. Society PFGoCT, Association EBoCJoGPOCM, Disease EGoGoGfPCoRS: [Guidelinefor pulmonary function testing in primary care (2018)]. Chin J Gen Pract 2019, 18(6).
- 30.2024 GOLDREPORT. [https://goldcopd.org/2024-gold-report/]
- 31.Stanojevic S, Kaminsky DA, Miller MR, Thompson B, Aliverti A, Barjaktarevic I, Cooper BG, Culver B, Derom E, Hall GL et al. ERS/ATS technical standard on interpretive strategies for routine lung function tests. Eur Respir J 2022, 60(1). [DOI] [PubMed]
- 32.Jian W, Gao Y, Hao C, Wang N, Ai T, Liu C, Xu Y, Kang J, Yang L, Shen H, et al. Reference values for spirometry in Chinese aged 4–80 years. J Thorac Disease. 2017;9(11):4538–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Folstein MF, Folstein SE, McHugh PR. Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. [DOI] [PubMed] [Google Scholar]
- 34.Gao MY, Yang M, Kuang WH, Qiu PY. [Factors and validity analysis of Mini-mental State examination in Chinese elderly people]. Beijing Da Xue Xue bao Yi xue ban = J Peking Univ Health Sci. 2015;47(3):443–9. [PubMed] [Google Scholar]
- 35.O’Donnell M, Teo K, Gao P, Anderson C, Sleight P, Dans A, Marzona I, Bosch J, Probstfield J, Yusuf S. Cognitive impairment and risk of cardiovascular events and mortality. Eur Heart J. 2012;33(14):1777–86. [DOI] [PubMed] [Google Scholar]
- 36.Lutsey PL, Chen N, Mirabelli MC, Lakshminarayan K, Knopman DS, Vossel KA, Gottesman RF, Mosley TH, Alonso A. Impaired lung function, Lung Disease, and risk of Incident Dementia. Am J Respir Crit Care Med. 2019;199(11):1385–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Obstructive and Restrictive Lung Disease. [https://www.webmd.com/lung/obstructive-and-restrictive-lung-disease]
- 38.Zhou M, Wang H, Zeng X, Yin P, Zhu J, Chen W, Li X, Wang L, Wang L, Liu Y, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet (London England). 2019;394(10204):1145–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhou Y, Zhong NS, Li X, Chen S, Zheng J, Zhao D, Yao W, Zhi R, Wei L, He B, et al. Tiotropium in Early-Stage Chronic Obstructive Pulmonary Disease. N Engl J Med. 2017;377(10):923–35. [DOI] [PubMed] [Google Scholar]
- 40.Heaton RK, Grant I, McSweeny AJ, Adams KM, Petty TL. Psychologic effects of continuous and nocturnal oxygen therapy in hypoxemic chronic obstructive pulmonary disease. Arch Intern Med. 1983;143(10):1941–7. [PubMed] [Google Scholar]
- 41.Guan PP, Wang P. Integrated communications between cyclooxygenase-2 and Alzheimer’s disease. FASEB Journal: Official Publication Federation Am Soc Experimental Biology. 2019;33(1):13–33. [DOI] [PubMed] [Google Scholar]
- 42.Au A, Feher A, McPhee L, Jessa A, Oh S, Einstein G. Estrogens, inflammation and cognition. Front Neuroendocr. 2016;40:87–100. [DOI] [PubMed] [Google Scholar]
- 43.Bettcher BM, Yaffe K, Boudreau RM, Neuhaus J, Aizenstein H, Ding J, Kritchevsky SB, Launer LJ, Liu Y, Satterfield S, et al. Declines in inflammation predict greater white matter microstructure in older adults. Neurobiol Aging. 2015;36(2):948–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Altamura C, Scrascia F, Quattrocchi CC, Errante Y, Gangemi E, Curcio G, Ursini F, Silvestrini M, Maggio P, Beomonte Zobel B, et al. Regional MRI Diffusion, White-Matter Hyperintensities, and cognitive function in Alzheimer’s Disease and Vascular Dementia. J Clin Neurol (Seoul Korea). 2016;12(2):201–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.van Straaten EC, Harvey D, Scheltens P, Barkhof F, Petersen RC, Thal LJ, Jack CR Jr., DeCarli C. Periventricular white matter hyperintensities increase the likelihood of progression from amnestic mild cognitive impairment to dementia. J Neurol. 2008;255(9):1302–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Infurna FJ, Gerstorf D. Linking perceived control, physical activity, and biological health to memory change. Psychol Aging. 2013;28(4):1147–63. [DOI] [PubMed] [Google Scholar]
- 47.Grenville J, Granell R, Dodd J. Lung function and cognitive ability in children: a UK birth cohort study. BMJ open Respiratory Res 2023, 10(1). [DOI] [PMC free article] [PubMed]
- 48.Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, Brayne C, Burns A, Cohen-Mansfield J, Cooper C, et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet (London England). 2020;396(10248):413–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hirano T, Doi K, Matsunaga K, Takahashi S, Donishi T, Suga K, Oishi K, Yasuda K, Mimura Y, Harada M et al. A novel role of growth differentiation factor (GDF)-15 in overlap with sedentary lifestyle and cognitive risk in COPD. J Clin Med 2020, 9(9). [DOI] [PMC free article] [PubMed]
- 50.Leisure. Life in Sichuan.
- 51.Li X, Peng A, Li L, Chen L. Association between walking and square dancing-oriented leisure-time physical activity and cognitive function among middle-aged and elderly people in Southwest China. BMC Geriatr. 2023;23(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhou Y, Chen Z, Shaw I, Wu X, Liao S, Qi L, Huo L, Liu Y, Wang R. Association between social participation and cognitive function among middle- and old-aged Chinese: a fixed-effects analysis. J Global Health. 2020;10(2):020801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bloomberg M, Muniz-Terrera G, Brocklebank L, Steptoe A. Healthy lifestyle and cognitive decline in middle-aged and older adults residing in 14 European countries. Nat Commun. 2024;15(1):5003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xiao D, Chen Z, Wu S, Huang K, Xu J, Yang L, Xu Y, Zhang X, Bai C, Kang J, et al. Prevalence and risk factors of small airway dysfunction, and association with smoking, in China: findings from a national cross-sectional study. Lancet Respiratory Med. 2020;8(11):1081–93. [DOI] [PubMed] [Google Scholar]
- 55.Stockley JA, Cooper BG, Stockley RA, Sapey E. Small airways disease: time for a revisit? Int J Chronic Obstr Pulm Dis. 2017;12:2343–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lan F, Lyu J, Guo Y, Bian Z, Yu C, Zhou H, Tan Y, Pei P, Cao W, Chen J, et al. [Area specific differences in lung function indices and prevalence of airflow obstruction in adults: findings from people in 10 areas in China]. Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua Liuxingbingxue Zazhi. 2015;36(11):1205–9. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets of the current study are available from the corresponding author upon reasonable request.