Abstract
Background
Life satisfaction, one promising health asset, is associated with reduced risk of several chronic diseases and mortality. Mental health conditions and quality of life (QoL) are important aspects of well-being in late life and are significantly associated with life satisfaction. Despite the complex interrelationships between mental health, QoL and life satisfaction, the current literature has evaluated the simple association between them and failed to consider the complex pathways among these variables, especially among the older population. Hence, this study explores the pathways between mental health conditions (depression, anxiety, and stress), QoL and life satisfaction among older adults in eastern Nepal.
Methods
This cross-sectional study was conducted in eastern Nepal via face-to-face interviews with 847 older adults selected by multi-stage cluster sampling. The 5-item Satisfaction with Life Scale and 13-item Older People’s QoL scale assessed life satisfaction and QoL, respectively. The 21-item Depression, Anxiety and Stress scale measured mental health conditions. The relationship between QoL, depression, anxiety, and stress with life satisfaction was first evaluated using linear regression, subsequently by path analysis.
Results
The mean (± SD) life satisfaction and QoL score were 19.7 (± 5.3) and 42.9 (± 7.1), respectively. More than one-fifth of the participants had moderate to severe depression (30%), anxiety (34%), and stress (20%). In adjusted regression analysis, QoL was positively associated (β: 0.44; 95% CI: 0.40 to 0.48) with life satisfaction, whereas depression, anxiety, and stress were inversely associated. In the path analysis, the relationship between depression and stress with life satisfaction was mediated by QoL. Depression was indirectly related to life satisfaction (mediated by QoL, β = -0.25), whereas stress was both directly (β = -0.11) and indirectly (mediated by QoL, β = -0.08) related to life satisfaction.
Conclusions
Given the high mental health burden among the older Nepali population and its potential impact on life satisfaction and QoL, routine screening for mental health should be encouraged in clinical practice. Additionally, community-based interventions and mental health promotion programs should be launched at regional and local levels.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12877-024-05618-6.
Keywords: Anxiety, Depression, Stress, Quality of life, Life satisfaction, Nepal, Older adults
Introduction
Globally, the proportion of older adults is increasing, with the World Health Organization (WHO) estimating that by 2050, 80% of the aging population will be in low- and middle-income countries [1]. In Nepal, a South Asian country between India and China, adults aged 60 and over make up 8.1% (2.5 million) of the population [2]. Life expectancy in Nepal has increased drastically over the past few decades, from 54 years in 1990 to 71 years in 2020 [3]. National data shows the older population is growing at 3.5%, outpacing the national growth rate of 1.35% [4], and projections suggest 10.8% of the population will be 60 or older by 2030 [5]. This demographic shift calls for investments in social, economic, and healthcare initiatives tailored to older adults. Nepal currently offers some support, including a monthly allowance of Rs 4,000 (U.S. $29.74) for seniors over 68, a social security budget, and the 2006 Senior Citizen Act, which prioritizes older adult’s healthcare [6–8].However, program sustainability and coverage remain challenges, especially in rural areas where over 80% of older Nepalis live [9], and there is limited research on the health and well-being of this population.
Life satisfaction is a broad social construct to assess the overall subjective well-being of an individual that measures the coherence between the people’s life goals and their present state of affairs [10, 11]. It is one promising health asset associated with reduced risk of several chronic diseases and mortality [12–14]. Furthermore, the WHO and the United Nations are urging nations to use life satisfaction as an indicator for informing policy decisions, and several countries have moved in that direction [15–18]. Although Nepal has not yet adopted such measures, initial studies have examined life satisfaction among older Nepali adults [19–21]. Given the varied ways individuals evaluate their lives based on social, health, and economic factors, further research on life satisfaction among older Nepalis is warranted [22, 23], more studies on the life satisfaction of Nepali older adults are required.
Evidence suggests that depression and quality of life (QoL) are important predictors of life satisfaction among older adults [24–26], with depressive symptoms strongly associated with lower life satisfaction even after adjustment for physical health [19, 27]. Similarly, higher QoL is linked to greater life satisfaction [24, 25]. While life satisfaction and QoL are related, they are distinct constructs within well-being research [28, 29], as seen in frameworks like bottom-up and top-down theories [28, 29], which suggest that improved QoL enhances life satisfaction, and vice versa [24, 25, 28–30]. However, while life satisfaction is shown to predict QoL [30], there is less research on the reverse relationship, especially in older adults. Although there is a plausible complex interaction between mental health, QoL, and life satisfaction, existing literature typically examines these variables in isolation without addressing their complex pathways, particularly in older populations. To the best of our knowledge, previous studies have not considered a pathway approach to understanding the mediating role of QoL in the relationship between mental health and life satisfaction among older adults. This study, therefore, explores the pathways between mental health (depression, anxiety, and stress), QoL, and life satisfaction among older adults in eastern Nepal.
Methods
Study design, sample, and sampling
A cross-sectional study was conducted between July and September 2020 in rural settings of two districts (Morang and Sunsari) of Province 1 in eastern Nepal. The sample size of 847 was calculated based on an unknown prevalence of stress at 50%, a 5% margin of error at 95% significance and a 10% non-response rate [31]. Sampling included multi-stage cluster sampling, whereby two rural municipalities from each district were randomly selected in the first step. Subsequently, four wards in each municipality were selected randomly based on probability proportional to size. The sampling frame was obtained from ward offices of the respective municipalities. Eligibility criteria were: Nepali nationals aged 60 and above, at least one year of residence in the study area, and the ability to understand survey instructions. The details of the subjects’ recruitment are published elsewhere [31].
Data collection and variables
Eight trained enumerators collected data via face-to-face interviews using the KoBo Toolbox application, which is pre-installed on tablets and synchronized online [32]. Standard validated tools, as described below, measured dependent and independent variables. Initially prepared in English, the questionnaire was translated into Nepali and then independently back-translated into English to check its face validity. Due to the onset of COVID-19 at the time of this survey, questionnaires were pre-tested on volunteers similar to the anticipated cohort, and minor editorial revisions were made.
Dependent variable
Life satisfaction
Satisfaction with Life Scale (SWLS), a widely used standard tool, measured participants’ satisfaction with life [10]. The scale captures participants’ agreement or disagreement on five items on subjective well-being on a 7-point Likert scale (1 = strongly disagree and 7 = strongly agree). In this study, the cumulative score (range 5 to 35) was calculated, where a higher score indicates higher levels of life satisfaction. The tool is previously validated and widely used across countries and cultures [10]. The tool, previously used in Nepal [19], has a Cronbach’s alpha of 0.89 in the current study, suggesting the scale is reliable among our participants.
Independent variables of interest
Quality of life was measured using the short version of the Older People’s Quality of Life (OPQOL) tool [33]. The OPQOL questionnaire comprises 13 items that capture participants’ agreement/disagreement on a 5-point Likert response scale (1 = strongly disagree to 5 = strongly agree). The scores for the 13 items are summed to obtain the total OPQOL score, which ranged between 13 and 65, whereby higher scores represent higher QoL. The tool has been used widely and validated across cultures [34, 35]. The tool was highly reliable in our study, as indicated by a Cronbach alpha of 0.91.
Depression, anxiety, and stress
The 21-item Depression, Anxiety, and Stress Scale (DASS-21) [36] measured the three independent variables of interest: depression, anxiety, and stress. Each sub-scale (i.e., depression, anxiety, and stress) contains seven items on a four-point Likert scale (0 = did not apply to me at all and 3 = applied to me very much, or most of the time). Briefly, the depression scale assesses dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest/involvement, anhedonia, and inertia. The anxiety scale assesses autonomic arousal, skeletal muscle effects, situational anxiety, and subjective experience of anxious affect. The stress scale assesses difficulty relaxing, nervous arousal, easily upset/agitated, irritable/over-reactive, and impatient. The items relevant to each of the three subscales are summed up to obtain the cumulative scores for depression (ranges: 0–21), anxiety (ranges: 0–21), and stress (ranges: 0–21), respectively. The cumulative score for each was used in the path analysis. However, for the linear regression, depression, anxiety, and stress were each classified into normal, moderate, and severe following the recommended cutoff [37]. The Nepali version of DASS-21 has been validated by two previous studies that demonstrated adequate psychometric properties of the scale [38, 39]. In the current study, the Cronbach alpha for the depression, anxiety, and stress subscales were 0.93, 0.87, and 0.87, respectively, indicating the scales to be reliable among our participants.
Control variables
In analyzing the relationships between QOL, depression, anxiety, stress, and life satisfaction, controlling for age, sex, marital status, education level, ethnicity, religion, occupation, family type, and dependency on family (for living and daily activities) is essential. Age and sex are foundational demographic factors influencing psychological well-being, as different life stages present unique challenges, and sex differences are observed in the prevalence of depression and anxiety [40, 41]. Marital status and family type shape social support networks, directly impacting life satisfaction [41]. Education level and occupation are indicators of socioeconomic status, which significantly influence mental health and quality of life [42]. Additionally, ethnicity and religion contribute to cultural values and coping mechanisms, shaping individuals’ perceptions of life satisfaction [41]. Lastly, dependency on family for living and daily activities, measures of social support, affects autonomy and plays a crucial role in understanding available social support, directly influencing both mental health and life satisfaction [40].
The responses for each control variable are provided in Table 1. Briefly, marital status was dichotomized into being married and without a partner; the latter included those widowed, separated, and never married. Education variable had three categories: “no education” (could not read or write), “informal” (those who attended some informal classes or training and could read and write in Nepali), and “formal education” (those attending formal schools). Ethnic groups were identified using Nepal’s Health Management Information System (HMIS) classification [43]. They were recategorized into three groups: Dalit and religious minority, disadvantaged group, and upper caste. Nepal’s local context considers the first two ethnic groups relatively disadvantaged.
Table 1.
Characteristics of participants- overall and by average life satisfaction score
| Characteristics | n (%) | Life satisfaction (Mean ± SD) |
p-value |
|---|---|---|---|
| Overall | 847 | 19.7 ± 5.3 | |
| Age, years | |||
| 60–64 | 290 (34.2) | 20.3 ± 4.8 | < 0.001 |
| 65–69 | 283 (33.4) | 20.1 ± 5.1 | |
| 70 and above | 274 (32.3) | 18.7 ± 5.7 | |
| Sex | |||
| Male | 469 (55.4) | 19.7 ± 5.1 | 0.833 |
| Female | 378 (44.6) | 19.8 ± 5.4 | |
| Marital status | |||
| Married | 647 (76.4) | 19.9 ± 5.2 | 0.114 |
| 1Without a partner | 200 (23.6) | 19.2 ± 5.3 | |
| Education status | |||
| No education | 472 (55.7) | 19.7 ± 5.5 | 0.008 |
| Informal education | 284 (33.5) | 19.4 ± 4.6 | |
| Formal education | 91 (10.7) | 21.3 ± 5.6 | |
| Ethnicity | |||
| Dalit & minority | 164 (19.4) | 18.2 ± 5.5 | < 0.001 |
| Disadvantaged | 554 (65.4) | 20.1 ± 4.9 | |
| Upper caste groups | 129 (15.2) | 19.9 ± 6.0 | |
| Religion | |||
| Hindu | 808 (95.4) | 19.7 ± 5.2 | 0.591 |
| Non-Hindu | 39 (4.6) | 20.2 ± 5.4 | |
| Occupation | |||
| Agriculture | 167 (19.7) | 20.2 ± 4.9 | < 0.001 |
| Business or job | 95 (11.2) | 20.5 ± 5.3 | |
| Retired and others | 231 (27.3) | 18.5 ± 4.6 | |
| Unemployed | 354 (41.8) | 20.1 ± 5.7 | |
| District | |||
| Morang | 438 (51.7) | 19.8 ± 5.6 | 0.786 |
| Sunsari | 409 (48.3) | 19.7 ± 4.8 | |
| Family type | |||
| Single | 155 (18.3) | 20.3 ± 5.7 | 0.113 |
| Joint | 692 (81.7) | 19.6 ± 5.2 | |
| Dependency on family for living | |||
| No | 193 (22.8) | 20.3 ± 6.0 | 0.076 |
| Yes | 653 (77.2) | 19.6 ± 5.0 | |
| Dependency on family for daily activities | |||
| No | 456 (53.8) | 20.9 ± 5.7 | < 0.001 |
| Yes | 391 (46.2) | 18.4 ± 4.3 | |
| Depression | |||
| Normal | 593 (70.0) | 20.4 ± 4.8 | < 0.001 |
| Moderate | 162 (19.1) | 18.2 ± 5.8 | |
| Severe | 92 (10.9) | 18.4 ± 5.9 | |
| Anxiety | |||
| Normal | 559 (66.0) | 20.3 ± 4.8 | < 0.001 |
| Moderate | 140 (16.5) | 18.9 ± 6.9 | |
| Severe | 148 (17.5) | 18.3 ± 4.8 | |
| Stress | |||
| Normal | 670 (79.1) | 20.2 ± 5.0 | < 0.001 |
| Moderate | 151 (17.8) | 17.9 ± 5.7 | |
| Severe | 26 ( 3.1) | 19.5 ± 6.6 |
1 Includes widowed, separated, and never married. Significant p-values are bolded
Statistical analyses
SAS Version 9.4 [44] was used for data analyses. Univariate statistics (frequency, proportion, mean and standard deviation) were generated to summarize the variables depending on their type. Bivariate analyses summarized differences in life satisfaction scores across independent variables. Pearson correlation coefficients were calculated between the independent variables of interest (QoL, depression, anxiety, and stress) and outcome (life satisfaction). The relationship between QoL, depression, anxiety, and stress with life satisfaction was first evaluated using linear regression, subsequently by path analysis. Stepwise regression based on the Akaike information criterion (AIC) criteria was used for model selection. The initial model began with all the control variables listed in Table 1, and the final model was adjusted for age, ethnicity, religion, occupation, and family dependency for daily activities. Adjusted and unadjusted beta coefficients and 95% confidence intervals from linear regressions are reported in Table 2. Multicollinearity was tested in terms of the variance influence factor (VIF). All the variables in the model had VIF less than 2.5 suggesting that multicollinearity was not concerning. Statistical significance was set at 0.05.
Table 2.
Means, standard deviations, and intercorrelations (Pearson correlation coefficients) between variables in path analysis
| Mean | SD | Pearson correlation coefficients*** | ||||
|---|---|---|---|---|---|---|
| Life satisfaction | QoL | Depression | Anxiety | |||
| QoL | 42.9 | 7.1 | 0.61 | |||
| Depression | 3.6 | 4.3 | -0.20 | -0.35 | 0.88 | |
| Anxiety | 3.4 | 3.6 | -0.18 | -0.33 | ||
| Stress | 4.4 | 3.8 | -0.24 | -0.35 | 0.86 | 0.86 |
Abbreviation- QoL: Quality of life, SD: standard deviation. *** All correlation coefficients were significant at p < 0.001
For the path analysis, the CALIS procedure in SAS was used. Path analysis is a valuable analytical method when the goal is to examine both direct and indirect relationships among observed variables in a simple and intuitive manner. Unlike structural equation modeling (SEM), which involves latent variables and adds complexity, path analysis focuses solely on measured variables, making the results easier to interpret. It also efficiently handles mediation by capturing direct and indirect effects within a single framework, offering a more streamlined alternative to conducting separate mediation analyses. Additionally, path analysis requires smaller sample sizes compared to SEM, while providing clearer insights into causal pathways through its more straightforward model. The initial model assumed an interrelationship between all independent variables of interest and life satisfaction (Supplemental Fig. 1). However, the final model was developed based on the Lagrange Multiplier test and the Wald test. The path models were assessed using chi-square goodness of fit, standardized root mean square residual (SRMR), root mean square error of approximation (RMSEA), and Bentler comparative fit index (CFI). The chi-square statistic tests the null hypothesis that the theoretical model fits the data. Thus, a larger p-value (> 0.05) suggests a close fit. Likewise, RMSEA and SRMR values less than 0.09 suggest a fair fit or adequate approximation error. In contrast, values less than 0.055 suggest a small error or better fit. CFI values greater than 0.94 suggest a good fit between data and hypothesized models [45].
Results
Descriptive statistics of sociodemographic profile
The mean age of participants was 68.0 ± 7.1 years. The majority of the participants were males (55.4%), married (76.4%), without any education (55.7%), belonged to a disadvantaged ethnic group (65.4%), and followed the Hindu religion (95.4%). Four in five lived in a joint family (81.7%), and about 77% and 46% of the participants depended on family for living and daily activities, respectively. About 30% of the participants had moderate to severe depression, 34% had moderate to severe anxiety, and about 20% had moderate to severe stress (Table 1).
Descriptive statistics of dependent and independent variables
The mean life satisfaction score (± SD) was 19.7 ± 5.3. In bivariate analyses, the average life satisfaction score was significantly associated with age, ethnicity, education, occupation, family dependence on daily activities, morbidity status, depression, anxiety, and stress (p < 0.001) (Table 1).The results in Table 3 show that life satisfaction was significantly and positively correlated with QoL (r = 0.61, p < 0.001), whereas depression (r = − 0.20, p < 0.001), anxiety (r = − 0.18, p < 0.001) and stress (r = − 0.24, p < 0.001) showed a weak negative correlation.
Table 3.
Linear regression for the association between independent variables of interest and life satisfaction
| Independent variables of interest | Unadjusted β1 (95% CI) | Adjusted β2 (95% CI) |
|---|---|---|
| Quality of life | 0.45 (0.41, 0.49) *** | 0.44 (0.40, 0.48) *** |
| Depression | ||
| Normal | Reference | Reference |
| Moderate | -2.19 (-3.09, -1.29) *** | -2.81 (-3.72, -1.90) *** |
| Severe | -1.94 (-3.08, -0.81) *** | -2.64 (-3.75, -1.52) *** |
| Anxiety | ||
| Normal | Reference | Reference |
| Moderate | -1.48 (-2.44, -0.52) ** | -1.49 (-2.41, -0.56) ** |
| Severe | -2.00 (-2.94, -1.06) *** | -2.71 (-3.68, -1.74) *** |
| Stress | ||
| Normal | Reference | Reference |
| Moderate | -2.31 (-3.23, -1.39) *** | -2.74 (-3.66, -1.82) *** |
| Severe | -0.71 (-2.74, 1.33) | -1.68 (-3.64, 0.27) |
Significant coefficients are bolded. **p < 0.01, ***p < 0.001. 1β is the regression coefficient indicating the change in life satisfaction for each one-unit increase in the predictor, with other variables held constant. A positive β means satisfaction increases, while a negative β signals a decrease. 2Based on the Akaike information criterion, the model was adjusted for age, ethnicity, religion, occupation, and family dependency for daily activities
Factors associated with life satisfaction
In the final adjusted model, controlling for age, ethnicity, religion, occupation, and family dependency for daily activities, all independent variables of interest, i.e., QoL, depression, anxiety, and stress, were significantly associated with life satisfaction (Table 2).
After adjusting control variables, a unit increase in QoL score increased life satisfaction by 0.44 units (adjusted β: 0.44; 95% CI: 0.40 to 0.48, p < 0.001). Depression, anxiety, and stress were inversely associated with life satisfaction. Older adults with moderate and severe symptoms of depression had 2.81 (adjusted β: -2.81; 95% CI: -3.72 to -1.90, p < 0.001) and 2.64 (adjusted β: -2.64; 95% CI: -3.75 to -1.52, p < 0.001) times lower life satisfaction score respectively than those without depressive symptoms. Likewise, those with moderate (adjusted β: -1.49; 95% CI: -2.41 to -0.56, p < 0.001) and severe (adjusted β: -2.71; 95% CI: -3.68 to -1.74, p < 0.001) score of anxiety and moderate stress (adjusted β: -2.74; 95% CI: -3.66, -1.82, p < 0.001) had lower life satisfaction score than their counterparts (Table 2).
Path analysis
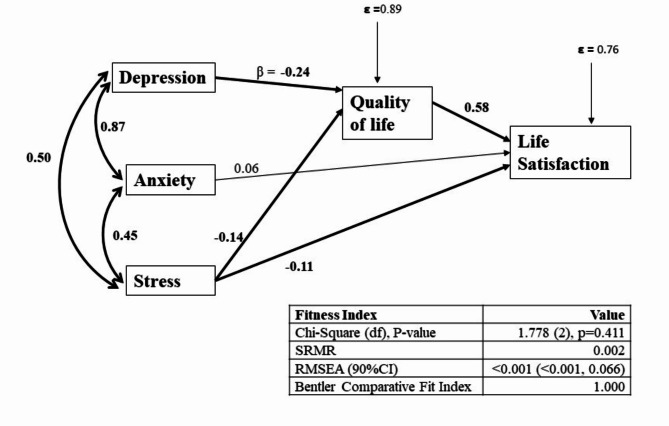
Figure 1 shows significant pathways of the final model and their goodness-of-fit indices. All goodness of fit indices, i.e., non-significant chi-square test (χ2 = 1.778, df = 2, p = 0.411), smaller values of residual (RMSEA < 0.001 and SRMR = 0.002), and CFI greater than 0.94, suggesting that the final model reasonably fits the data.
Fig. 1.
Pathway between depression, anxiety, stress, quality of life and life satisfaction (final model). Single-headed arrows indicate directional relationships, showing the hypothesized influence of one variable on another. Bold arrows highlight pathways found to be statistically significant in the path analysis. The final model is adjusted for age, ethnicity, marital and educational status, and family dependency for daily activities. β (Beta) represents the standardized regression coefficient, indicating the strength and direction of the relationship between the variables. Positive values indicate a direct relationship, while negative values indicate an inverse relationship. ε (Epsilon): Denotes the error term, which accounts for the unexplained variance in quality of life and life satisfaction. Fitness Index Values: Chi-Square tests the fit of the model to the data, with a non-significant p-value suggesting good model fit. SRMR (Standardized Root Mean Square Residual) indicates the average discrepancy between observed and predicted correlations, with values closer to 0 showing a better fit. RMSEA (Root Mean Square Error of Approximation) reflects the model’s goodness-of-fit, with values < 0.05 indicating a close fit. Bentler Comparative Fit Index compares the model’s fit to a baseline model, with values closer to 1 indicating a better fit
All path coefficients shown in Fig. 1, except the path between anxiety and life satisfaction were statistically significant (Table 4; Fig. 1). QoL (β = 0.58; p < 0.001) and stress (β = -0.11; p = 0.040) had a significant direct relationship with life satisfaction, whereas the direct pathway between depression and life satisfaction was not supported. Depression indirectly contributed to life satisfaction through QoL (β = -0.25; p < 0.001). In addition to significant direct effects, the relationship between stress and life satisfaction was also mediated by QoL (β = -0.08; p < 0.05) (Fig. 1).
Table 4.
Relationship between independent and dependent variables in path analyses
| Independent variables | Dependent variables | Estimate (β) | 95% CI | p-value | |
|---|---|---|---|---|---|
| Quality of life | ----- -> | Life satisfaction | 0.58 | 0.53, 0.63 | < 0.001 |
| Depression | ----- -> | Quality of life | -0.24 | -0.37, -0.12 | < 0.001 |
| Anxiety | ----- -> | Life satisfaction | 0.06 | -0.04, 0.17 | 0.233 |
| Stress | ----- -> | Life satisfaction | -0.11 | -0.21, -0.01 | 0.040 |
| Depression | ----- -> | Anxiety | 0.87 | 0.85, 0.89 | < 0.001 |
| Depression | ----- -> | Stress | 0.50 | 0.44, 0.56 | < 0.001 |
| Anxiety | ----- -> | Stress | 0.45 | 0.39,0.51 | < 0.001 |
| Stress | ----- -> | Quality of life | -0.14 | -0.27,-0.02 | 0.021 |
The arrow (----- ->) represents the direct causal path from the independent variable to the dependent variable. “Standardized Estimate (β)” represents the standardized regression coefficient, indicating the strength and direction of the relationship between the independent and dependent variables
Table 5 shows the direct, indirect and total effects of depression, anxiety, and stress on life satisfaction. Depression (β = -0.25) and anxiety (β = -0.09) were found to be indirectly related to life satisfaction (mediated by QoL), whereas stress was both directly (β = -0.11) and indirectly (mediated by QoL, β = -0.08) related to life satisfaction.
Table 5.
Total, direct and indirect effects of independent variables on life satisfaction
| Total Effect | Direct Effect | Indirect Effect | |
|---|---|---|---|
| Depression | -0.25*** | 0.00 | -0.25*** |
| Anxiety | -0.02 | 0.06 | -0.09*** |
| Stress | -0.19*** | -0.11* | -0.08* |
*p < 0.05, ***p < 0.001. “Total Effect” is the sum of direct and indirect effects and indicates the overall influence of the independent variable on life satisfaction. “Direct Effect” represents the immediate impact of the independent variable on life satisfaction, without mediation. “Indirect Effect” shows the impact of the independent variable on life satisfaction that is mediated through other variables
Discussion
Nepal’s National Health Policy (2014) aims to deliver quality health services to all citizens and provide basic health services free of cost [46], and the National Mental Health Strategy and Action Plan (2020) describes the provision of free primary care mental health services for all parts of the country [47]However, the government of Nepal’s commitment to addressing the unmet needs of the aging population is not up to par. This research found that higher QoL scores were associated with better life satisfaction, whereas higher depression, anxiety, and stress scores were associated with lower life satisfaction. Furthermore, in the path analysis, QoL mediated the relationship between depression and life satisfaction.
Better QoL was associated with better life satisfaction, a finding consistent with the literature [24, 25, 30, 48]. Those with the highest levels of QoL reported being satisfied with their life [24, 25]. Among Turkish older adults, life satisfaction positively predicted QoL [30]. The plausible reason could be that older adults in community settings have emotional stability, engagement, positive emotion and relationships, productivity, resilience and self-esteem that might have uniquely flourished their QoL. This could have influenced the perception that life is going well, positively impacting subjective happiness on the life satisfaction scale.
Our finding of an inverse association between mental health conditions and life satisfaction, i.e., poor mental health leads to lower life satisfaction, is consistent with the literature [19, 27, 49–51]. Lower life satisfaction in older adults is attributed to poor mental health [19, 27, 50]. Even after adjustment for physical health characteristics, depressive symptoms are strongly associated with lower life satisfaction [27]. A previous study from Nepal reported older adults with higher depression scores had lower life satisfaction [19]. Likewise, among older adults with chronic pain in Sweden, anxiety or depression disorders had a negative relationship with life satisfaction [51]. In fact, life satisfaction is negatively associated with depression, anxiety, and/or stress for all age groups, including the oldest old [49], young adults [52, 53] and adolescents [54]. Depressive symptoms impact perceived subjective feelings, self-esteem and self-worth, as well as health behaviors such as physical activity, healthy diet, and medication adherence [55]. They also induce higher levels of distress and loneliness, all of which ultimately impact an individual’s satisfaction with life [56]. Another possible explanation could be that depression in older adults impairs daily functional activity and increases their dependency on caregivers or family members [57, 58]. This, in turn, deteriorates their state of well-being, which may have contributed to the decreased perceived self-worth of our participants on the life satisfaction scale. Moreover, in Nepal, the mental health and life satisfaction of marginalized communities, such as Madhesi, Dalits, and Indigenous groups, is often affected by limited access to socioeconomic and cultural resources. However, cultural factors like family support, community networks, and participation in cultural events (e.g., Dashain, Deepawli, Joorshital, Chaath) can enhance mental health and life satisfaction. Social activities, such as community gatherings, arts, ceremonies, and volunteering, foster a sense of belonging and inclusion, ultimately improving well-being among older adults. These activities were partially disrupted during COVID-19, though marginalized communities demonstrated resilience. Future research should explore the relationships between mental health (e.g., depression, anxiety) and life satisfaction in older adults, while identifying protective factors.
Furthermore, in addition to directly affecting life satisfaction, QoL mediated the pathway between depression and life satisfaction. The potential link between depression and QoL is well evident in the literature, as depression in older population is one of the prime factors that determine the QoL in that population. Consistent with our findings, poor mental health decreases QoL in older populations [59–61]. A previous finding from urban Nepal also reported that depression score was negatively associated with QoL among Nepali older adults [61]. Notably, one component of the OPQOL tool is social support and previous literature support that social support buffers the impact of depressive symptoms on life satisfaction in old age [59]. In later life, support from friends and family helps adapt to physical, biological, and social changes. It also acts as a buffer to help older adults cope with symptoms of depression and/or the impact of depression on perceived well-being and life satisfaction [59].
Strengths, limitations, and future research directions
This pioneering study explored the pathways between mental health, QoL and life satisfaction among Nepali older adults. To our knowledge, these pathways among older adults have not been previously explored in any context. Large sample size with a response rate of more than 90% and the involvement of locally trained enumerators who understand the local culture dynamics and language with years of experience in fieldwork as surveyors add to the strengths of this research. Notably, the research lead and few other research team members have lived marginalization experience similar to those of the studied population which ensures that findings are interpreted within local socio-cultural lens.
Nonetheless, this study has the following limitations: (i) Data collection was done during the COVID-19 pandemic, a period with unique challenges, such as social restrictions, economic uncertainty, and health concerns, that may have significantly influenced the participant’s response, findings should be interpreted with caution, (ii) cross-sectional study design; therefore, no causal inferences can be made, (iii) Although we used a validated tool to measure depression, anxiety and stress, given that mental health is highly stigmatized in Nepal [62], their measures may be underestimated due to the possibility of social desirability bias (iv) our study was limited to two districts with small geographic regions, which restricts the generalizability of the findings to other settings and ethnic groups (e.g., urban, hilly, or Himalayan regions and diverse ethnic groups).
Further prospective studies are needed to identify the direction of these pathways. While we conceptualized the pathway from QoL to life satisfaction, further rigorous large-scale research embedding a multimethod or mixed-method approach with an opportunity for participants to anonymously report well-being parameters required to investigate the interactions between QoL and life satisfaction from bidirectional perspectives.
Policy and practice implications
Despite the above-noted limitations, this study has significant clinical implications for older populations’ health and well-being, particularly in low-resource settings. As an important health indicator to assess the overall subjective well-being of an individual, understanding the determinants of life satisfaction is essential to promote overall well-being. Specifically, given the high mental health burden among the older Nepali population, as quantified by the current and previous studies [61], and its potential impact on life satisfaction and QoL; routine screening for mental health should be encouraged in primary health care for the ageing population. Training community health workers to identify and manage common mental health issues can improve access to care, especially in rural and underserved areas where specialized services are often unavailable. As a trusted community member, these workers can also serve as liaisons between traditional healing systems and modern mental health services, fostering culturally acceptable care. Additionally, as the government of Nepal is on the verge of devising a geriatric health policy, prioritizing the prevention and management of depression in a national health strategy is essential. This policy should include key performance indicators for primary healthcare services to address mental health effectively. Our findings emphasize the importance of mental health assessments at secondary and tertiary care levels, where healthcare providers can evaluate mental health using validated scales and tailor interventions to mitigate adverse mental health impacts, especially for marginalized groups who may face greater barriers to accessing care. Addressing mental health literacy, reducing stigma, and strengthening referrals are also critical and should be incorporated into national policy; empowering community health workers to support older adults could significantly enhance care accessibility. Public health campaigns and mental health literacy initiatives can help normalize conversations about mental health, thereby encouraging help-seeking behavior.
While Nepal’s Community Mental Health Care Package 2074 (2017) aims to integrate mental health into primary care, its implementation faces barriers, including limited human resources and funding [47, 63]. Additionally, Nepal’s robust traditional healing system, rooted in religious and cultural practices, should be considered in mental health program design, as traditional and faith-based healers use culturally specific spiritual practices to address psychological issues among diverse communities [47]. Mental health initiatives should also focus on reducing stereotypes and addressing the social and cultural determinants of mental health, enhancing social support and involving family members in care could help improve QoL. Specifically, strengthening social support systems through community-based programs and involving families and peers in mental health care can improve QoL and life satisfaction by diminishing perceived stress or emotional distress - a positive predictor of anxiety and depression. Finally, fostering connections between older adults and community or neighborhood groups can promote social connectedness, and enhance well-being.
Conclusions
Depression, anxiety, and stress had a negative relationship with life satisfaction, while QoL had a positive relationship. QoL mediated the relationship of depression and stress with life satisfaction. This study’s findings could be used in designing mental health services and programs that ultimately aim to enhance older adults’ life satisfaction and quality of life. Future studies may explore factors that interplay in the mediating role of QoL in the relationship between mental health and life satisfaction. Given the global trend of nationwide longitudinal aging studies, future research has an opportunity to expand the geographical boundaries to include a nationally representative sample of older adults in Nepal. Finally, social support plays an important role in the pathway between mental health and life satisfaction. Future research should explore these pathways by including social support in the pathways.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgements
We want to thank the local-level authorities of the government of Nepal for helping us collect the information from participants. The work would not have been completed without the support of District Health Officers. Moreover, we are indebted to all the study participants.
Author contributions
UNY, RM, SG, and SKM conceptualized and designed the study; SM, UNY, and OPY were responsible for field work; SG and UNY analyzed the data and interpreted the findings; SG, IK, and UNY were responsible for writing the first draft of the paper; all the authors made critical revisions and approved the final version of the manuscript.
Funding
UNY and RM secured provincial funding from the Nepal Health Research Council, Government of Nepal.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The Ethics Committee at the Nepal Health Research Council approved the study (Ref#114/2021P). Before the data collection, written informed consent was obtained from all participants, and participation was voluntary. Thumbprint impressions were obtained from participants who had no formal education (illiterate) and were approved by the ethics committee. The privacy and confidentiality of all study participants were maintained.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Uday Narayan Yadav and Saruna Ghimire contributed equally to this work.
References
- 1.WHO, Ageing. and health. 2021. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Accessed 14 Sep 2022.
- 2.Chalise HN. Provincial situation of elderly population in Nepal. Am J Aging Sci Res. 2020;1:9–11. [Google Scholar]
- 3.World Bank. Life expectancy at birth, total (years) - Nepal | Data. 2022. https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=NP. Accessed 14 Jun 2022.
- 4.Central Bureau of Statistics. National Population and Housing Census 2011. 2012.
- 5.United Nations, Department of Economic and Social Affairs. Population Division. World Population Ageing 2015 (ST/ESA/SER.A/390). 2015.
- 6.Shrestha S, Aro AR, Shrestha B, Thapa S. Elderly care in Nepal: Are existing health and community support systems enough. SAGE Open Med. 2021;9:1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chalise HN, Bohara P, Khanal T. Older People and Social Security System in Nepal. Gerontol Geriatr Res. 2022;8.
- 8.Geriatric Center Nepal. Status report on elderly people (60+) in Nepal on health, nutrition and social status focusing on research needs. 2010.
- 9.Chalise HN. Socio-Demographic and Health Status of Nepalese Elderly. Indian J Gerontol. 2012;26:151–60. [Google Scholar]
- 10.Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. 1985;49:71–5. [DOI] [PubMed] [Google Scholar]
- 11.Nemitz J. Increasing longevity and life satisfaction: is there a catch to living longer? J Popul Econ. 2022;35:557–89. [Google Scholar]
- 12.Boehm JK, Peterson C, Kivimaki M, Kubzansky LD. Heart health when life is satisfying: evidence from the Whitehall II cohort study. Eur Heart J. 2011;32:2672–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feller S, Teucher B, Kaaks R, Boeing H, Vigl M. Life satisfaction and risk of chronic diseases in the European prospective investigation into cancer and nutrition (EPIC)-Germany study. PLoS ONE. 2013;8:e73462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martín-María N, Miret M, Caballero FF, Rico-Uribe LA, Steptoe A, Chatterji S, et al. The Impact of Subjective Well-being on Mortality: A Meta-Analysis of Longitudinal Studies in the General Population. Psychosom Med. 2017;79:565–75. [DOI] [PubMed] [Google Scholar]
- 15.Stiglitz JE. Measuring what counts: the global movement for well-being. The New Press; 2019.
- 16.Sachs JD. Introduction to the 2019 global happiness and wellbeing policy report. Glob Happiness Wellbeing. 2019.
- 17.World Health Organization. Joint meeting of experts on targets and indicators for health and well-being in Health 2020: Copenhagen, Denmark, 5–7 February 2013. 2013.
- 18.Jean-Paul F, Martine D, Beyond. GDP measuring what counts for economic and social performance: measuring what counts for economic and social performance. OECD Publishing; 2018.
- 19.Ghimire S, Baral BK, Karmacharya I, Callahan K, Mishra SR. Life satisfaction among elderly patients in Nepal: associations with nutritional and mental well-being. Health Qual Life Outcomes. 2018;16:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gautam R, Saito T, Kai I. Correlates of life satisfaction among older Nepalese adults living with a son. Biosci Trends. 2008;2:187–92. [PubMed] [Google Scholar]
- 21.Schwartz AE. We Are Left Alone: A Qualitative Study of Life Satisfaction of Older Adults in Rural Nepal. Yale University; 2021.
- 22.Alıcı B, Seçim G. The Psychometric Properties of the Turkish Version of the Riverside Life Satisfaction Scale–Adult Form. SAGE Open. 2020;10:1-8. [Google Scholar]
- 23.Lombardo P, Jones W, Wang L, Shen X, Goldner EM. The fundamental association between mental health and life satisfaction: results from successive waves of a Canadian national survey. BMC Public Health. 2018;18:342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Novianti LE, Wungu E, Purba F. Quality of Life as A Predictor of Happiness and Life Satisfaction. J Psikol. 2020;47:93. [Google Scholar]
- 25.López-Ruiz V-R, Huete-Alcocer N, Alfaro-Navarro J-L, Nevado-Peña D. The relationship between happiness and quality of life: A model for Spanish society. PLoS ONE. 2021;16:e0259528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khodabakhsh S. Factors affecting life satisfaction of older adults in Asia: A systematic review. J Happiness Stud. 2022;23:1289–304. [Google Scholar]
- 27.Puvill T, Lindenberg J, de Craen AJM, Slaets JPJ, Westendorp RGJ. Impact of physical and mental health on life satisfaction in old age: a population based observational study. BMC Geriatr. 2016;16:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pinto S, Fumincelli L, Mazzo A, Caldeira S, Martins JC. Comfort, well-being and quality of life: Discussion of the differences and similarities among the concepts. Porto Biomed J. 2017;2:6–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Veenhoven R. The study of life satisfaction. A comparative study of satisfaction with life in Europe. Eötvös University; 1996. pp. 11–48.
- 30.Aydiner Boylu A, Gunay G. Life satisfaction and quality of life among the elderly: Moderating effect of activities of daily living. Turk J Geriatr. 2017;20:61–9. [Google Scholar]
- 31.Shrestha A, Ghimire S, Kinney J, Mehta R, Mistry SK, Saito S, et al. The role of family support in the self-rated health of older adults in eastern Nepal: findings from a cross-sectional study. BMC Geriatr. 2024;24:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kobo Inc. KoBoToolbox | Data Collection Tools for Challenging Environments. 2021.
- 33.Bowling A, Hankins M, Windle G, Bilotta C, Grant R. A short measure of quality of life in older age: The performance of the brief Older People’s Quality of Life questionnaire (OPQOL-brief). Arch Gerontol Geriatr. 2013;56:181–7. [DOI] [PubMed] [Google Scholar]
- 34.Chen Y, Hicks A, While AE. Validity and reliability of the modified Chinese version of the Older People’s Quality of Life Questionnaire (OPQOL) in older people living alone in China. Int J Older People Nurs. 2014;9:306–16. [DOI] [PubMed] [Google Scholar]
- 35.Siette J, Knaggs GT, Zurynski Y, Ratcliffe J, Dodds L, Westbrook J. Systematic review of 29 self-report instruments for assessing quality of life in older adults receiving aged care services. BMJ Open. 2021;11:e050892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44:227–39. [DOI] [PubMed] [Google Scholar]
- 37.Thapa SB, Hauff E. Psychological distress among displaced persons during an armed conflict in Nepal. Soc Psychiatry Psychiatr Epidemiol. 2005;40:672–9. [DOI] [PubMed] [Google Scholar]
- 38.Thapa DK, Visentin D, Kornhaber R, Cleary M. Psychometric properties of the Nepali language version of the Depression Anxiety Stress Scales (DASS-21). Nurs Open. 2022;9:2608–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tonsing KN. Psychometric properties and validation of Nepali version of the Depression Anxiety Stress Scales (DASS-21). Asian J Psychiatry. 2014;8:63–6. [DOI] [PubMed] [Google Scholar]
- 40.Wilmer MT, Anderson K, Reynolds M. Correlates of Quality of Life in Anxiety Disorders: Review of Recent Research. Curr Psychiatry Rep. 2021;23:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nagargoje VP, James KS, Muhammad T. Moderation of marital status and living arrangements in the relationship between social participation and life satisfaction among older Indian adults. Sci Rep. 2022;12:1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang Y, Su D, Chen Y, Tan M, Chen X. Effect of socioeconomic status on the physical and mental health of the elderly: the mediating effect of social participation. BMC Public Health. 2022;22:605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lynn B, Dahal DR, Govindasamy P, Caste. Ethnic and Regional Identity in Nepal: Further Analysis of the 2006 Nepal Demogrpahic and Health Survey. Maryland, USA: Calverton; 2008. [Google Scholar]
- 44.SAS Institute Inc. Statistical Analysis Systems; 2016.
- 45.O’Rourke N, Hatcher LA. Step-By-Step Approach to Using SAS System for Factor Analysis and Structural Equation Modeling. 2013.
- 46.Balakrishnan SS, Caffrey M. Policy brief for Nepal. UNICEF; 2022.
- 47.World Health Organization. Nepal WHO Special Initiative for Mental Health Situational Assessment. 2022.
- 48.Yildirim Y, Kilic SP, Akyol AD. Relationship between life satisfaction and quality of life in Turkish nursing school students. Nurs Health Sci. 2013;15:415–22. [DOI] [PubMed] [Google Scholar]
- 49.Ng ST, Tey NP, Asadullah MN. What matters for life satisfaction among the oldest-old? Evidence from China. PLoS ONE. 2017;12:e0171799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim E, Delaney S, Tay L, Chen Y, Diener E, Vanderweele T. Life Satisfaction and Subsequent Physical, Behavioral, and Psychosocial Health in Older Adults. Milbank Q. 2021;99. [DOI] [PMC free article] [PubMed]
- 51.Dong H-J, Larsson B, Dragioti E, Bernfort L, Levin L-Å, Gerdle B. Factors Associated with Life Satisfaction in Older Adults with Chronic Pain (PainS65+). J Pain Res. 2020;13:475–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Koivumaa-Honkanen H, Kaprio J, Honkanen R, Viinamäki H, Koskenvuo M. Life satisfaction and depression in a 15-year follow-up of healthy adults. Soc Psychiatry Psychiatr Epidemiol. 2004;39:994–9. [DOI] [PubMed] [Google Scholar]
- 53.Strine TW, Chapman DP, Balluz LS, Moriarty DG, Mokdad AH. The associations between life satisfaction and health-related quality of life, chronic illness, and health behaviors among U.S. community-dwelling adults. J Community Health. 2008;33:40–50. [DOI] [PubMed] [Google Scholar]
- 54.Hoseini-Esfidarjani S-S, Tanha K, Negarandeh R. Satisfaction with life, depression, anxiety, and stress among adolescent girls in Tehran: a cross sectional study. BMC Psychiatry. 2022;22:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Whooley MA, de Jonge P, Vittinghoff E, Otte C, Moos R, Carney RM, et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300:2379–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lee SL, Pearce E, Ajnakina O, Johnson S, Lewis G, Mann F, et al. The association between loneliness and depressive symptoms among adults aged 50 years and older: a 12-year population-based cohort study. Lancet Psychiatry. 2021;8:48–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ghimire S, Paudel G, Mistry SK, Parvez M, Rayamajhee B, Paudel P, et al. Functional status and its associated factors among community-dwelling older adults in rural Nepal: findings from a cross-sectional study. BMC Geriatr. 2021;21:335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yadav UN, Tamang MK, Thapa TB, Hosseinzadeh H, Harris MF, Yadav KK. Prevalence and determinants of frailty in the absence of disability among older population: a cross sectional study from rural communities in Nepal. BMC Geriatr. 2019;19:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Adams TR, Rabin LA, Da Silva VG, Katz MJ, Fogel J, Lipton RB. Social Support Buffers the Impact of Depressive Symptoms on Life Satisfaction in Old Age. Clin Gerontol. 2016;39:139–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sivertsen H, Bjørkløf GH, Engedal K, Selbæk G, Helvik A-S. Depression and Quality of Life in Older Persons: A Review. Dement Geriatr Cogn Disord. 2015;40:311–39. [DOI] [PubMed] [Google Scholar]
- 61.Ghimire S, Baral BK, Pokhrel BR, Pokhrel A, Acharya A, Amatya D, et al. Depression, malnutrition, and health-related quality of life among Nepali older patients. BMC Geriatr. 2018;18:191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Gurung D, Poudyal A, Wang YL, Neupane M, Bhattarai K, Wahid SS, et al. Stigma against mental health disorders in Nepal conceptualised with a what matters most framework: a scoping review. Epidemiol Psychiatr Sci. 2022;31:e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Primary Health Care Revitalization Division. Community Mental Health Package, Nepal 2074. Teku, Kathmandu: Government of Nepal, Ministry of Health, Department of Health Services; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.