Abstract
Background
Children with disabilities worldwide experience disparities in oral health. Parents and children encounter challenges in accessing quality dental care. Similar challenges are experienced in Saudi Arabia. This study aimed to explore the barriers and facilitators of oral healthcare for children with disabilities in Saudi Arabia.
Methods
This was an ethnographic study. The sample size was 25 participants, comprising of 12 pediatric dentists and 13 parents of children with disabilities. Data were collected through in-depth interviews, employing a topic guide. A pre-defined analytical framework was developed from the study objectives and framework analysis used to analyse data.
Results
The study identified significant barriers and facilitators to oral healthcare for children with disabilities. Barriers included long travel distances, inadequate clinic facilities, a shortage of specialist pediatric dentists, inefficiencies in referral systems, and financial constraints. Other challenges were related to physical barriers in clinics, cultural norms, and socioeconomic inequalities. Facilitators, though fewer, included personal connections, specialized disability friendly clinics, and the Priority Card Program, albeit with limited effectiveness. Suggestions for improvement highlighted the need for better training for dental professionals, enhanced clinic accessibility, and greater financial support for families.
Conclusion
Accessibility of dental care for children with disabilities in Saudi Arabia remains a significant challenge due to systemic barriers and individual-level obstacles. The study underscores the need for policy reforms, enhanced professional training, and the improvement of physical and financial accessibility to dental services. Addressing these issues through comprehensive educational programs and targeted interventions is essential for reducing oral health disparities and improving care for children with disabilities.
Keywords: Access, Disability, Children, Oral healthcare, Dental care, Saudi Arabia
Background
The United Nations Children’s International Emergency Fund (UNICEF) estimates the number of children with disabilities worldwide is approximately 240 million [1]. In the Kingdom of Saudi Arabia (KSA), individuals with disabilities account for 5.1% of the population, totalling 1,349,585 people, according to the 2022 Population and Housing Census [2]. This population includes those with mobility impairments (304,787 individuals), visual impairments (181,728 individuals), hearing impairments (84,025 individuals), intellectual disabilities (327,431 individuals), self-care challenges (157,977 individuals), and other physical disabilities (293,637 individuals) [2]. This diverse range of disabilities highlights the importance of understanding and addressing the specific healthcare needs of this population, particularly in the context of oral health.
Children with disabilities often face significant disparities in health outcomes compared to their non-disabled peers [3, 4]. These disparities extend to oral health, where children with disabilities experience a higher prevalence of dental issues like tooth decay, gingivitis, and severe periodontal disease [5–7]. Previous research emphasizes that individuals with disabilities, particularly those with intellectual disabilities, exhibit a greater prevalence and severity of periodontal disease compared to the general population [8]. While the prevalence of dental caries in children with intellectual disabilities is similar to that of the general population [7, 9], their oral health deteriorates more rapidly as they transition into adulthood. Studies indicate that adults with intellectual disabilities have more missing teeth, untreated dental decay, and fewer dental restorations compared to the general population [8, 10].
Moreover, individuals with disabilities, including children, have more complex oral healthcare needs compared to those without disabilities [11]. Research on the clinical oral health condition of children with disabilities reveals significant oral healthcare needs compared to the general population [12, 13]. These disparities are attributed to various risk factors, such as the need for assistance in basic oral hygiene tasks, communication barriers, behavioural issues, higher prevalence of poor nutrition, and challenges in accessing quality oral healthcare [14, 15].
Global research on oral healthcare accessibility for children with disabilities highlights substantial barriers which exacerbate existing oral health disparities [16–21]. One primary obstacle is the lack of reasonable adjustments for children with disabilities, such as accessible dental facilities [16]. Transportation difficulties create further challenges [16, 20]. Communication barriers also create challenges, especially for individuals with sensory impairments or communication disorders, particularly when the practitioner has little experience in adjusting the communication environment [17]. Financial constraints pose challenges, because treatment costs for individuals with disabilities are typically higher due to the need for specialized care [18, 21]. Negative past experiences or fear associated with dental visits can be a barrier to seeking regular dental care [21]. A lack of awareness among dental professionals about the specific needs of patients with disabilities can lead to inadequate care and create barriers to accessing essential dental services [18, 19, 21].
In KSA, the Saudi government has introduced various health policies to improve healthcare access for individuals with disabilities. Programs like the Priority Card aim to reduce waiting times through electronic registration [22]. Additionally, the King Salman Center for Disability Research’s Access Program fosters inclusivity in healthcare facilities and public spaces, adhering to international accessibility standards [22].
Despite these efforts, challenges remain. Research in KSA identifies key barriers to oral healthcare for children with disabilities, including difficulties in finding appropriate clinics [23–26]. Other barriers include dentists’ reluctance to treat children with special needs [24, 26], inadequate provision of oral health advice [24], the cost-prohibitive nature of dental care [24–26], difficulties with transportation [27], geographically distant dental clinics [27], fear of the dentist, and child uncooperativeness [25, 26]. These cross-sectional studies in KSA provide valuable insights, but because of their design, fail to explore reasons why these barriers occur. In contrast, qualitative studies offer a deeper understanding of the lived experiences, perspectives, and socio-cultural contexts surrounding oral healthcare access for this population. As such, qualitative research designs can therefore contribute to the development of targeted interventions and policies aimed at improving oral healthcare for children with disabilities. The present study aimed to explore the perceptions of dental professionals and parents about oral healthcare for children with disabilities in KSA.
Materials and methods
Study design
This study was about exploring experiences in a particular cultural context and therefore uses ethnography as the methodology to address the research aim. The main question for the study was: How do dental professionals and parents view barriers and facilitators of oral healthcare for children with disabilities in KSA?
The objectives were to: (i) Explore dental professionals’ perceptions of the barriers and facilitators in providing oral healthcare to children with disabilities, (ii) Investigate parents’ experiences in accessing oral healthcare for children with disabilities, (iii) Identify cultural, social, and systemic factors that influence access to and the quality of oral healthcare for children with disabilities and (iv) Provide evidence-based recommendations to improve dental care practices and policies.
Ethics
Ethical approval
for this study was obtained from the Institutional Review Board of King Saud University (Ref. No. 23/0475/IRB). To ensure participant anonymity, pseudonyms were assigned and identifiable characteristics modified. During the interviews, the researcher restated the study aim and invited participants to ask questions before signing a consent form. Participants were also informed that they had the option to voluntarily decide their participation in the study, withdraw up to two weeks after interview, and choose not to answer particular questions.
Study context
This research was conducted in Riyadh Province, the capital city of KSA. Study participants were recruited from hospitals and disability centres. These locations were selected for their known high patient volume and specialized services for children with disabilities. The recruitment process aimed to ensure a diverse representation of experiences across various healthcare settings. To maintain confidentiality, place names were not identified.
Sampling strategy and recruiting
In this study, two sampling methods were employed: purposive sampling and snowball sampling for participant recruitment. Purposive sampling involved recruiting self-selecting pediatric dentists and parents of children with disabilities. The researchers asked the initial participants to suggest others interested in participating, forming a snowball sample. Parents were approached through the head of the disability centers who facilitated introductions to interested parties, while pediatric dentists were directly approached at their workplaces by the researchers (MW or AJ) to invite their participation. The researchers gave them a brief overview of the study, gathered their contact information for interview scheduling, and then provided them with an information sheet, a topic guide to aid in interview preparation, and a consent form before the interview. The information sheet provided to participants included details about the study’s objectives, the voluntary nature of participation, confidentiality measures, and contact information for further inquiries or concerns. Two weeks later, the researcher contacted potential participants and asked if they would consent to an interview. The concept of information power guided sample size [28]. This meant that an iterative approach was taken to data collection, with interviews continuing until no new themes or insights emerged from the data, at which point it was determined that enough data had been collected. Following theoretical guidance, the research team discussed the content of the data at intervals during collection and reached a collective decision as to when to halt recruitment of participants [29]. This study was part of a broader project focusing on oral healthcare for children with disabilities, involving 12 dentists, 13 parents, and 5 policymakers. The current study specifically explored access to oral healthcare from the perspectives of parents and dentists, using a sample of 25 participants (12 dentists and 13 parents). This sample size was considered sufficient to capture diverse perspectives and provide a comprehensive understanding of the oral healthcare experiences of parents of children with disabilities and the perspectives of dentists treating this particular group.
Study participants
Participants in the study included a total of 25 individuals, including 12 pediatric dentists, and 13 parents of children with disabilities. The characteristics of these participants (anonymized) are detailed in Table 1.
Table 1.
Participant characteristics
| Pediatric Dentists (DR) | ||||
|---|---|---|---|---|
| Participant | Age range | Sex | Specialist description | |
| DR1 | 30–35 | Female | Consultant in Pediatric dentistry | |
| DR2 | 25–30 | Female | Pediatric Dentist - First Deputy / Clinical Doctorate in Pediatric Dentistry | |
| DR3 | 30–35 | Male | Pediatric Dentist with recent completion of the Saudi Board in Pediatric Dentistry | |
| DR4 | 30–35 | Male | Pediatric Dentist with recent completion of the Saudi Board in Pediatric Dentistry | |
| DR5 | 25–30 | Female | Pediatric dentist | |
| DR6 | 30–35 | Female | Pediatric dentist / Assistant consultant | |
| DR7 | 30–35 | Male | Pediatric dentist / Assistant professor / DClinDent Pediatric Dentistry, MPaed Dent (RCSEd) | |
| DR8 | 25–30 | Male | Pediatric Dentist - First Deputy / Clinical Doctorate in Pediatric Dentistry | |
| DR9 | 30–35 | Female | Consultant in Pediatric dentistry | |
| DR10 | 30–35 | Male | Consultant in Pediatric dentistry | |
| DR11 | 45–55 | Female | Consultant in Pediatric dentistry | |
| DR12 | 45–55 | Male | Consultant in Pediatric dentistry | |
| Parents of Children with Disabilities (P) | ||||
| Participant | Parent | Age of Children | Sex of Children | Type of Disability |
| P1 | Mother | 9 years | Girl | Physical disability |
| P2 | Mother | 17 years | Boy | Fragile X Syndrome / Autism |
| P3 | Mother | 10 years | Boy | Fragile X Syndrome / Autism |
| P4 | Mother | 12 years | Boy | Intellectual disability (Moderate) |
| P5 | Mother | 15 years | Girl | Intellectual disability (Mild) |
| P6 | Mother | 17 years | Boy | Intellectual disability (Moderate), and Epilepsy |
| P7 | Mother | 9 years | Boy | Down syndrome |
| P8 | Mother | 11 years | Girl | Autism, and physical disability |
| P9 | Mother | 7 years | Boy | Autism |
| P10 | Father | 6 years | Boy | Down syndrome |
| P11 | Mother | 7 years | Girl | Intellectual disability (Mild), and physical disability |
| P12 | Mother | 9 years | Girl | Intellectual disability (Moderate) |
| P13 | Mother | 5 years | Girl | Autism |
Data collection methods
Data was gathered through semi-structured interviews conducted either in-person or via Zoom, depending on participants’ preferences for the method they felt most convenient. Parents showed a preference for virtual interviews, while dentists preferred face-to-face interaction at their workplace. The meeting link was sent to parents approximately one week before the session, with a reminder email sent one day before. The primary language of the interviews was Arabic, although participants had the option to also speak in English. Data collection took place from July 2023 to January 2024, by two researchers (MW and AJ), both dental professionals experienced in qualitative research.
Before initiating the interviews, participants were reminded of the study’s aims. They were informed about the voluntary nature of their participation and their right to withdraw from the study without consequences if they felt uncomfortable with the topics being discussed. Participants were also informed about the expected duration of the interview, which was estimated to be between 45 and 90 min. They were informed that the session would be recorded using an audio-recorder, and the interviewer would take notes during and after the interview. They were assured of anonymity. Subsequently, the interviews ranged in duration from 30 to 45 min. All interviews were digitally recorded and transcribed verbatim by the researchers.
Interview guides were developed in collaboration with research team members and were informed by frameworks of access to healthcare and key studies on barriers and facilitators to healthcare services for children with disabilities [16–21, 30, 31]. Separate guides were tailored for pediatric dentists and parents of children with disabilities. Despite the differences in target groups, the questions were intentionally designed to elicit similar information from various perspectives. Each guide comprised open-ended questions aimed at exploring diverse views on oral healthcare accessibility, challenges, and experiences with dental services. For detailed information on the interview guides, see Supplementary file 1.
Data analysis
Framework analysis is a robust method for organizing, synthesizing, and presenting qualitative data [32]. The analytical framework was guided by themes or categories that mirror the study’s objectives, ensuring the analysis is closely aligned with the research questions. This is a deductive approach. Analysis includes five stages: familiarization, identifying a coding framework, coding, charting, mapping and interpretation, this was conducted iteratively [32]. Two researchers (MW, AJ) employed verification techniques by checking the analysis against the original data and then comparing it against the accounts of other participants and existing theoretical evidence. The analysis therefore moved between deductive and inductive approaches.
Initially, the primary researcher, a native Arabic speaker, transcribed, redacted, and translated the interviews into English. A second researcher, also a native Arabic speaker proficient in English, independently reviewed the transcripts. This dual-verification process ensured accuracy by comparing the translations and resolving discrepancies through discussion. Afterwards, familiarization with the data occurred by reviewing transcriptions to gain a comprehensive understanding of participants’ perceptions. Following familiarization, the coding framework identification stage was undertaken. During this stage, emerging themes and concepts were identified through detailed discussions among the research team. As part of the coding framework identification process, a codebook was developed to ensure consistency and transparency in coding the data. The codebook defined each theme and associated codes with clear examples from the data. It served as a guiding tool for subsequent stages of indexing and charting. An example of the codebook is provided in Table 2.
Table 2.
Codebook example: professional skills and training in dental care
| Theme | Code | Definition | Example from Data |
|---|---|---|---|
|
Professional Skills and Training (This theme refers to the level of skills, training, and personal abilities of dental professionals, impacting the quality of care they can provide to children with disabilities) |
Lack of Confidence | Dental professionals expressing uncertainty or discomfort in treating children with disabilities | “A pediatric dentist declined to treat my son solely because he’s autistic…” (P9) |
| Insufficient Training | Inadequate training provided during dental education, particularly in dealing with complex cases involving disabilities | “During a visit, the staff seemed uncomfortable handling my son’s special needs…” (P6) | |
| Interpersonal Skills | Challenges in effectively communicating with parents and children with special needs. | “Parents with children who have health issues can be sensitive. Choosing the right words and approach is essential to avoid adding to their distress.” (Dr 3) | |
| Positive Engagement | Dentists exhibiting effective interpersonal skills, leading to better experiences for the children. | “During one visit, the doctor used engaging distractions, making the experience enjoyable for my child.” (P7) |
Once the thematic framework was established, the data was systematically indexed, ensuring that each piece of information was appropriately assigned to the relevant themes within the framework. This rigorous process of indexing facilitated the organization and categorization of the extensive dataset. Following indexing, the indexed data was summarized and synthesized into coherent representations using Microsoft Office Excel as the platform for analysis. Subsequently, the stage of mapping was followed, where analysis and interpretation of the data occurred within the context of the thematic framework. Connections, contradictions, and nuances within the dataset were explored, leading to deeper insights into the underlying meanings and implications of the data. Finally, interpretation was undertaken, where conclusions were drawn, and insights generated based on the analysis. Throughout these phases, the research team engaged in frequent discussions to resolve any disagreements. Also, an iterative analytical process was engaged, with the approach continually revisited and refined in light of new insights and developments. The thoroughness, validity, and reliability of the findings were ensured by this iterative nature of the analysis. O’Brien’s [33] guidance on how to present qualitative research is applied in this manuscript, as applicable.
Quality indicators
To ensure the credibility of the data analysis, the study employed several strategies, including an audit trail, triangulation, and member-checking, as commonly recommended in qualitative research methodology [34, 35]. An audit trail was diligently maintained to document the researchers’ decision-making process, along with the collection and analysis of data. This documentation served as a transparent record of the research steps, facilitating scrutiny of the researchers’ methods. Various forms of triangulation, such as analyst and sources triangulation, were then utilized to enhance the trustworthiness of the findings. Analyst triangulation engaged multiple researchers in analyzing and reviewing the data, offering diverse perspectives to the analysis [35]. The study also gathered insights from a range of sources, including parents, and pediatric dentists, reinforcing the solidity of the analysis. Finally, random member-checking was undertaken to validate the accuracy and completeness of the researchers’ interpretations and the study’s findings, following guidelines from Lincoln and Guba (1985) [34]. Through these strategies, the study aimed to enhance the quality and trustworthiness of the data analysis, providing a solid foundation for the conclusions.
Results
The analysis revealed several themes concerning oral healthcare accessibility for children with disabilities, each encompassing both barriers and facilitators. An overview of these themes is presented in Table 3.
Table 3.
Overview of themes related to accessing oral healthcare for children with disabilities
| Main theme | Subthemes |
|---|---|
| Facility and service accessibility |
Geographical distance Inadequate facilities System inefficiencies Reasonable adjustments Transport challenges Personal connections (Wasta) Specialized clinics and support programs |
| Professional skills and training in dental care |
Lack of confidence Training Interpersonal and communication skills Positive engagement Specialist courses and practical experience in postgraduate studies |
| Socioeconomic inequalities |
Financial strain Limited insurance coverage Availability of subsidized services |
| Information and oral health education |
Lack of awareness about dental services Difficulty interpreting children’s pain Insufficient oral health education resources Absence of standardized guidelines |
| Culture norms and gender dynamics |
The challenges of segregated facilities The cultural perception for same sex professionals |
Theme 1: facility and service accessibility
This theme explores the physical and systemic barriers that families face in accessing oral healthcare for children with disabilities, including long travel distances, inadequate facilities, and a shortage of specialist dentists. For many families, navigating the dental care system for children with disabilities involves long trips from remote areas to urban centres, where specialized care is more readily available.
“We often see that syndromes and disabilities in patients come from families in remote areas… They must travel to urban centres like Riyadh for treatment due to a lack of necessary services in their local regions” (Dr 2).
For further details of participants, see Table 1.
Upon reaching urban centres, families encounter additional challenges. Most primary care clinics lack the necessary equipment for children with disabilities, often resulting in referrals to larger hospitals, which delay care.
“Not all clinics are equipped to assist children with disabilities; many are not qualified. Consequently, they are referred to larger hospitals, which takes a long time” (Dr 6).
The shortage of specialist pediatric dentists further exacerbates accessibility issues.
“Specialist pediatric dentists are scarce in primary care clinics and private practices, being mostly concentrated in larger hospitals” (Dr 6).
Moreover, a decline in the number of pediatric dentists’ limits access to specialized dental care, creating additional barriers for families seeking timely treatment for their children with disabilities.
“There is a decline in pediatric dentists even in government and private hospitals, and the ratio of pediatric dentists to the population is still low” (Dr 1).
Inefficiencies in the healthcare system, especially in referral processes, increase these challenges. Poorly organized referrals, diverse management practices, and a lack of communication lead to increased burdens on overworked medical staff and treatment delays.
“The on-call system for dental care is poorly organized… Some hospitals have easier referrals, while others cause patients to get lost in the system” (Dr 1).
Long waits for treatment also add emotional stress for children and their families. One parent shared:
“My child has been on the waiting list for a year and a half for dental surgery, using painkillers while we’re stuck with the public system’s long waits” (P5).
Scheduling inefficiencies and unfriendly clinic environments further contribute to anxiety for children.
“Delays are particularly hard on children because they don’t understand long waits, and it can be distressing for them to be in unfamiliar places” (P2).
A pediatric dentist pointed out the inadequacies in clinic design: “Some clinics lack appropriate tools, and their design isn’t suitable for special needs patients. An open or busy space can negatively affect patients with autism” (Dr 7). Parents emphasized the need for more engaging clinic environments: “An ordinary dental clinic is not necessarily suitable for children with special needs. The clinic must have engaging items beyond smartphones to distract them” (P3). Suggestions include enhancing decor with engaging characters: “They could have characters, and the chair could be decorated to make it more inviting” (P1).
Physical barriers further complicate clinic visits, as many clinics, especially private ones, lack proper accommodations for individuals with disabilities, often providing only stairs at their entrances.
“A clinic without ramps or elevators is inaccessible, and without nearby parking, those with mobility issues struggle to return for follow-up care” (Dr 4).
Reliable transportation also poses a significant barrier, often leading to missed or delayed appointments due to limited parking and long distances.
“Living in the south of Riyadh and needing to reach the main hospital in the east is challenging, as family schedules, limited parking, and safe transportation can cause delays” (P3).
Despite these barriers, personal connections within the healthcare system can sometimes facilitate access to timely care. One parent recounted her experience:
“Two years ago, when my child began showing signs of tooth decay despite maintaining good oral hygiene, I struggled to find suitable care. After much effort and watching my son’s condition worsen, I used my connections to seek attention at [hospital’s name]. What was initially a four-year wait turned into just five weeks thanks to a dentist who expedited our appointment. We received comprehensive dental treatment, including extractions and fillings. The dentist even offered to see my child directly for future visits, making the process smoother” (P3).
This highlights how social networks can play a crucial role in overcoming systemic barriers, enabling families to access timely and appropriate care despite the challenges posed by healthcare structures. Specialized clinics for patients with autism offer additional hope. These clinics provide a controlled and sensory-friendly environment tailored to the unique needs of children with autism. Services include quiet rooms, structured routines, and staff trained to manage sensory sensitivities and behavioral challenges. Such environments help reduce anxiety and improve the overall dental experience for children with autism.
“ Children with autism require specialized management. On designated days, clinics are reserved exclusively for them, ensuring a quieter environment” (Dr 4).
One government initiative, the priority card program, aimed to improve dental care access. However, both parents and doctors reported its ineffectiveness: “Honestly, this card has been of no use to me… It’s useless” (P6). A doctor noted a lack of awareness about the card among staff and parents: “I haven’t heard of the priority card in hospitals or from parents” (Dr 3). Here, the card’s potential benefits appeared undermined by poor implementation and a general lack of awareness.
Theme 2: professional skills and training in dental care
This theme refers to the skills, training, and abilities of dental professionals, which directly impact the care quality they provide to children with disabilities. A significant issue is the gap in training and willingness to treat these children, often resulting in referrals to other practitioners.
Participants frequently mentioned the lack of confidence and expertise among dentists. One parent described a pediatric dentist refusing care due to discomfort treating an autistic child:
“A pediatric dentist refused to treat my son simply because he’s autistic… He said, ‘Neither I nor my assistant can examine him as the child is not cooperative…” (P9).
Similarly, another parent described a situation where a dentist’s unfamiliarity with disabilities was evident.
“During a visit, the staff seemed uncomfortable handling my son’s special needs. The dentist even asked me to help him get my son to open his mouth.” (P6).
Other participants discussed the qualifications of healthcare professionals in treating children and suggested that doctors in government hospitals are more experienced.
“Private clinic dentists often refer children with disabilities elsewhere, while government hospital doctors have more experience handling these cases. " (Dr 2).
Dental professionals acknowledged this gap, expressing reluctance to handle rare or complex cases because of limited exposure and lack of confidence:
“Sometimes, cases or syndromes are so rare that even doctors haven’t heard of them, leading to a reluctance to take on such cases due to fear or a lack of confidence.” (Dr 5).
Concerns also extended to interpersonal skills. Effective communication is crucial when dealing with sensitive cases, and shortcomings in this area exacerbated the challenges families faced:
“Parents with children who have health issues can be sensitive. Choosing the right words and approach is essential to avoid adding to their distress.” (Dr 3).
Families report experiences where inadequate understanding and patience from dental staff led to traumatic outcomes. One parent described how a dismissive approach from the dentist led to their child developing a fear of dental visits:
“The dentist’s inability to engage with my child led to a traumatic experience that escalated to anaesthesia for a minor decay. Now, she’s scared of dentists and reluctant to attend even routine check-ups.” (P1).
In contrast, positive interactions with dentists who engaged with children in a friendly manner significantly improved their comfort and willingness to receive care:
“During one visit, the doctor used engaging distractions, making the experience enjoyable for my child. A cooperative and light-hearted approach made all the difference.” (P7).
Dentists further acknowledged gaps in undergraduate training for treating children with disabilities, stressing the need for specialist courses and practical experience, as recommended by the Saudi Board.
“Our undergraduate training lacked hands-on experience. The specialized training provided by the Saudi Board was essential in boosting our confidence and competence.” (Dr 1).
Another dentist shared how postgraduate studies addressed these gaps by offering valuable experience and emphasizing Interprofessional collaboration:
“Undergraduate training didn’t prepare me well for treating patients with disabilities. Postgraduate studies in pediatrics changed that, providing hands-on experience in weekly clinics, especially with patients who had learning disabilities.“(Dr 3).
Theme 3: socioeconomic inequalities
This theme highlights the financial and social barriers that limit access to oral healthcare for families with children with disabilities. Participants shared experiences of significant socioeconomic barriers affecting dental care access, primarily focused on the cost of private services and socioeconomic status.
Many participants emphasized the prohibitive costs of private dental care. One dentist noted,
“Getting dental work done privately is really expensive, which is a huge problem for a lot of people. The costs are a big reason why some families can’t get the care they need for their kids” (Dr 5).
This high cost often forces families to forgo necessary care or seek private services as a last resort when public services fall short. Another participant explained:
“The issue with government hospitals is the long wait for appointments. This often leaves no choice but to seek treatment at private clinics, where the prices are a major worry. For those with disabilities, treatments can be even pricier” (Dr 1).
A parent also shared their struggle with covering high costs without insurance, highlighting the difficult choices families must make between different healthcare needs:
“The high cost of dental services is a major barrier for us. We pay out of pocket for everything, including my child’s therapies. Long wait lists for public services forced us to seek costly private care, making dental expenses another burden we can’t afford. It feels like all our money goes into just one aspect of her care” (P1).
The influence of socioeconomic status extends to securing routine dental appointments. A dentist observed that economically disadvantaged families often prioritize other medical needs over dental care:
“Parents’ socioeconomic status complicates their situation. Traveling to the hospital can be exhausting, especially with children who have disabilities, leading them to prioritize urgent medical needs over dental care and miss appointments due to time or resource constraints” (Dr 4).
The hierarchy within institutional policies also exacerbated the divide. A participant mentioned how scheduling inequalities further disadvantaged patients:
“At our university hospital, there’s a system that favours staff members, giving them quicker dental appointments for routine check-ups and general dental procedures. In contrast, the average patient can wait as much as a year for the same services.” (Dr 1).
Despite these barriers, participants identified facilitators that could improve access to oral healthcare, notably financial and insurance support. One dentist involved in a committee on ‘access to care’ questioned whether financial constraints hinder access, especially for children:
“I was part of a committee focused on ‘access to care’ and ‘quality.’ We noticed that many services are free, so I’m not sure financial constraints are a significant issue for children” (Dr 11).
Another dentist pointed out that most workplaces provide insurance, suggesting the primary obstacle might be a lack of parental awareness regarding dental health:
“Most workplaces offer insurance, enabling access to big hospitals. I don’t see money as a barrier; rather, it may be a lack of parental desire or dental education” (Dr 7).
This study emphasises the importance of addressing both financial barriers and educational gaps to improve access to oral healthcare.
Theme 4: information and oral health education
This theme outlines various obstacles related to a lack of awareness and education regarding dental services for children with disabilities, as faced by parents and caregivers. It reveals the complexity of accessing proper dental care and sheds light on potential facilitators that could improve access.
Parents expressed a lack of knowledge about dental services tailored for their children’s needs.
“I searched, went from one clinic to another… because I didn’t know where to find a clinic with the right facilities, like laughing gas” (P7).
Another parent expressed uncertainty about finding a dentist equipped to meet their child’s needs and communicate effectively.
“[.] I want to take my child for a check-up, but I’m unsure who the right dentist is. I don’t know any dentists who can communicate and persuade effectively” (P2).
Parents often struggled to recognize and interpret their children’s expressions of dental pain. “Their sense of pain is weak so they don’t express it, but I would notice his face swollen or fingers in his mouth all the time” (P3). This difficulty, due to communication impairments, hinders timely care.
Parents and professionals agreed on the lack of oral health education, especially about primary teeth. One parent shared their confusion:
“When my child’s tooth decayed, I questioned the need for treatment since it was a baby tooth. The dentist reassured me it would fall out, so no extraction was needed, and advised fluoride for protection. So, I’m waiting for the new tooth to emerge.” (P7).
A dentist corroborated the need for increased awareness, but contradicted the information given to the previous parent:
“I always try to start early to increase awareness. Many parents think baby teeth aren’t important since they’ll fall out. We need to raise awareness about this” (Dr 1).
The data also reveal a lack of collaboration between healthcare departments, hindering oral health awareness efforts. A parent said, “I’ve never had a pediatrician talk to me about dental care” (P3). This was supported by a dentist’s remark on the lack of routine dental health advice in general medical care:
“[…] unfortunately, there’s a lack of coordination between medical and dental departments, and patients are only referred when serious issues like infections arise " (Dr 1).
One oral healthcare provider suggested the absence of standardized guidelines for children with disabilities in Saudi Arabia contributes to the lack of support for dental professionals:
“No consistent guideline exists for special needs children’s dental care. I often rely on British guidelines and personal materials, as we lack Arabic guidelines with visuals for at-home care. I use my phone to show patients how to brush properly, but hospitals provide no official support in this regard” (Dr 7).
Theme 5: cultural norms and gender dynamics in healthcare access
This theme explores how cultural expectations, such as gender segregation and preferences for same-gender dentists, affect access to dental care for children with disabilities. It highlights the discomfort some caregivers feel in mixed-gender settings and the impact of cultural attire on the clinic atmosphere. These norms often conflict with the healthcare needs of children, emphasizing the need for inclusive, culturally sensitive settings.
One parent expresses the difficulties faced due to gender segregation, especially when accompanying a child who looks older than they are.
“Waiting is challenging for my son. People stare, which makes both him and others uncomfortable. There’s no suitable waiting area for us. I can’t sit in either the men’s or women’s sections. Women feel awkward, and I can’t go into the men’s area, which is uncomfortable for me. This often leaves us sitting outside. The setup just isn’t accommodating.” (P6).
Moreover, caregivers frequently express a preference for male doctors for their sons, which they believe contributes to a more comfortable treatment experience:
“Honestly, we prefer male doctors because they often have a good way of handling people with disabilities, and my son feels comfortable with them. They know when to be strict but also how to be gentle” (P6).
These preferences are deeply rooted in cultural norms and significantly influence the trust and comfort levels caregivers experience while seeking treatment for their children.
Discussion
This study provides insights from parents and dental professionals regarding the barriers and facilitators to accessing oral healthcare for children with disabilities in KSA. The findings reveal complex challenges in accessing care, with barriers existing at both systemic and individual levels.
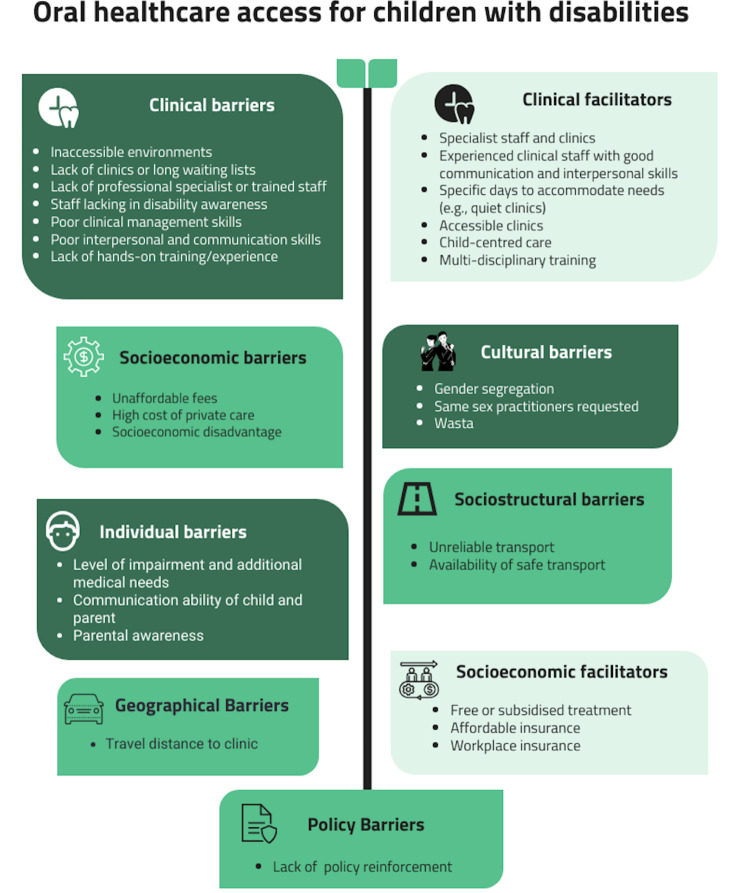
Figure 1 highlights the broad categories of factors that worked as either barriers or facilitators to oral healthcare access for children with disabilities from participants’ perspectives. They are presented in different themes that were shown in results to simplify the complex and systemic nature of the problem. For example, as seen in the “clinical factor”, accessibility can be a barrier if the existing dental clinic does not accommodate the need for children with disabilities but can also be a facilitator if it is built in an accessible and inclusive way to welcome children with disabilities. And as shown in the figure, it is clear that barriers outweigh the facilitators, proving that access to oral healthcare of children with disabilities is a significant issue that mandate interventions at different levels and across different sectors “health, education, etc.” to help mitigate this problem and ultimately improve their oral health, general health and wellbeing.
Fig. 1.
Overview of factors associated with accessibility to oral healthcare for children with disabilities
These challenges align with findings from local [26, 27, 36] and global studies [16–21], highlighting significant barriers that exacerbate oral health disparities for children with disabilities. Recurring issues identified in this study are the systemic inefficiencies in appointment booking, clinic management, and coordination among staff, which significantly impact the quality of care. These systemic challenges were consistently pointed out by participants as key obstacles to timely and effective routine treatment.
One challenge highlighted by this study is the difficulty families’ face in accessing dental care for children with disabilities. Families in remote areas struggle with long travel distances, and primary care clinics often lack the necessary infrastructure “ramps, elevators, etc.”, resulting in delays and frequent referrals to larger “distanced” hospitals. Physical barriers within clinics and transportation challenges further hinder access. Although KSA has implemented an access program for people with disabilities, it still requires reinforcement, particularly in rural region [37]. Improving access through accommodating, better-equipped clinics, and reduced fees remains essential [38].
Another significant barrier is the lack of sufficient professional skills and training among dental practitioners, a challenge evident in both national and international contexts. Studies in KSA [24, 39, 40]; and globally [21] report that a shortage of trained special care dentists limits access to essential dental services. One study found that dental care providers in KSA, especially those who had treated patients with special needs, felt more prepared to offer care, underscoring the importance of hands-on experience in improving preparedness [41]. General dentists’ reluctance to treat children with disabilities, often due to insufficient training, underscores the urgent need for reforms in dental education. These include integrating relevant courses into undergraduate and postgraduate curricula and expanding continuing education opportunities. Despite the Saudi Board’s efforts to introduce specialized training, pediatric dentists remain the primary caregivers for children with disabilities, as general dentists rarely provide these services. For example, a study conducted in KSA, found that only 12% of children with special healthcare needs (CSHCN) received dental care from general dentists, while 72.9% were treated by pediatric dentists [25]. Similarly, Nayak et al. (2022) revealed that many general dentists in Saudi Arabia face considerable challenges in treating CSHCN, reinforcing the reliance on pediatric dentists and highlighting training and resource gaps in the dental workforce [42]. Globally, comparable trends persist; Casamassimo et al. (2004) reported that only 10% of general dentists in a sample of 1,251 U.S. general practitioners frequently treated children with disabilities. However, dentists with hands-on dental school experience were more inclined to seek further education and perceived disability-related challenges as less of a barrier [43]. Expanding training and continuing education could enhance the competence and availability of the dental workforce, reducing reliance on specialized centers and addressing the shortage of trained professionals [44].
Enhancing provider willingness to treat children with disabilities, along with promoting empathy and understanding, could alleviate the sense of rejection often felt by their families. Research indicates that provider self-efficacy, empathy, and positive communication are closely associated with improved patient-cantered care [45]. Dentists with more experience and training in managing children with disabilities are more likely to communicate effectively and empathetically, while those lacking such experience may struggle with both communication and treatment completion [45].
Socioeconomic barriers also significantly complicate access to dental care for children with disabilities. The high cost of private care and lack of insurance are major challenges. While some institutions in KSA offer free services, participants reported that these services are often inadequate to meet the high demand. Managing a child’s disabilities adds further financial strain, leading caregivers to deprioritize dental care. This aligns with research linking costs to difficulties in accessing dental care [19, 24, 25, 46]. Enhancing financial support and improving the educational system to raise awareness about available services are critical to mitigating these barriers. However, systemic barriers, such as clinic inefficiencies and resource shortages, must also be addressed to ensure sustainable improvements. A comprehensive approach is needed, including strengthening healthcare infrastructure, expanding professional training, and implementing systemic reforms to eliminate inequities in oral healthcare for children with disabilities.
In addition, the policies of some hospitals where they prioritise staff members for dental appointments inadvertently contributes to prolonged wait times for the general patient population, highlighting a systemic issue. Our findings suggest that such scheduling inequalities may exacerbate healthcare disparities. Suggestions for addressing this challenge could involve strategies like increasing service capacity, allocating designated slots for staff, or implementing scheduling systems that prioritize based on urgency instead of affiliation.
A lack of oral health education further contributes to inadequate care for children with disabilities. Integrating early dental assessments into routine well-child healthcare, supported by pediatricians and allied health professionals, can bridge the gap between general and specialized dental care [47, 48]. In KSA, the Ministry of Health prioritized maternal and child health through initiatives like the Mother & Child Healthcare program, which includes oral health awareness and child nutrition education [49]. The Child Health Passport, which documents children’s medical history, examinations, investigations, and follow-ups, serves as a primary reference for healthcare providers, promoting integrated care that includes necessary screenings [49]. While these initiatives lay a foundation for improved integration, oral health within routine child healthcare practices continues to be an area of ongoing development. The effectiveness of these policies in enhancing access to dental care for children may depend on their consistent implementation and the adequacy of training provided to healthcare professionals, who are often the first point of contact for mothers and children.
Research highlights significant gaps in oral health knowledge among Saudi healthcare providers, which impact the quality of care for children. Zakirulla et al. (2021) found that nurses in pediatric intensive care units recognized the importance of oral care but struggled with barriers like insufficient education, time constraints, and heavy workloads [50]. Similarly, Alshathri et al. (2020) reported that only 7% of family physicians had received oral health training, leading to low referral rates to dental clinics [51]. Almazrooa et al. (2021) further identified that only 42% of family physicians would request dental consultations before bisphosphonate therapy, demonstrating a lack of awareness about the oral health risks associated with certain treatments [52].
These gaps in training and awareness can be addressed by the Saudi Commission for Health Specialties, which mandates continuous medical education (CME) but currently does not account for CME hours outside healthcare providers’ practice scope [53], limiting opportunities for oral health education. Expanding CME to focus on oral health topics such as disease identification, risk assessment, and appropriate referrals could improve early detection and management of oral health issues by all healthcare professionals. Strengthening the integration of oral health training into CME programs and ensuring consistent policy implementation would be critical in enhancing access to dental care for children, particularly those with disabilities. Internationally, the Colorado Medical–Dental Integration Project incorporates dental hygiene services into medical settings, promoting collaboration between medical providers and dental hygienists to enhance access to preventive oral health services for vulnerable populations, demonstrating the integration of dental care into general healthcare [54].
Cultural norms in KSA, such as gender segregation and preferences for same-gender providers, complicate access to dental care for children with disabilities, limiting families’ options and increasing challenges. Addressing these barriers through inclusive and culturally competent healthcare environments can enhance access and improve care for diverse patient populations.
While the study identified significant barriers to accessing oral healthcare for children with disabilities, it also highlighted resilience and facilitators in overcoming these challenges. One such facilitator is the use of personal connections, referred to as wasta, which some parents relied on to expedite care. Wasta is described as “[…]an unwritten social contract based on the cooperation and obligation between members of various social groups such as families and tribes” (p.1) [55]. While individual dentists may be willing to help, broader systemic factors, such as scheduling difficulties and lack of coordination, often hinder efforts to provide timely care and may worsen oral health outcomes for children in need. Additionally, systemic challenges, including a shortage of trained professionals and limited resources, contribute to delays in care [56, 57]. To address these structural barriers, it is essential to improve healthcare staffing, infrastructure, and inter-departmental coordination. Eliminating the need for personal connections to access services would ensure that care is based on clinical need rather than social ties, ultimately ensuring more equitable and timely care for children with disabilities.
Beyond personal connections, specialized clinics for children with autism show promise. These clinics provide sensory-adapted environments (e.g., dimmed lighting, soundproofing, calming colors) and use visual aids, social stories, and structured routines. Trained professionals address sensory and behavioral needs, ensuring patient-centered care. Research confirms these adaptations improve cooperation and reduce distress in children with autism during dental treatments [58–60]. However, the limited availability of such clinics may ultimately increase disparities by extending wait times and restricting access to general dental services. This aligns with concerns raised in the UK dental literature, which warn against the potential pitfalls of creating separate services for disabled individuals, because it may exacerbate existing inequalities [61]. Within KSA, the ineffectiveness of the priority card program in expediting care reveals a gap between policy and practice, emphasizing the need for better implementation and awareness among healthcare providers. Balancing specialized care with broader accessibility would appear essential to ensure that children with disabilities are not further marginalized within the healthcare system.
Strengths and limitations
Qualitative research, using ethnography as the methodology, provided rich insights into accessing oral healthcare for children with disabilities within one province in KSA. While the sample size was sufficient for the qualitative nature of the study, and guided by the concept of information power, there are potential limitations to consider. Selection bias may have arisen due to self-selecting participants, and participant bias is possible, with responses potentially influenced by personal experiences or social desirability. The study also occurred in one discrete geographical area in KSA, and each region differs in terms of population density, resources and health care availability. Therefore, this study may not necessarily reflect the challenges of other regions. Whilst the study incorporated diverse perspectives; certain factors might have influenced the results. Differences in the type and level of disabilities among the children, as well as variations in the professional experience of the participating pediatric dentists (e.g., first deputies versus consultants), could have impacted the findings.
Although generalizability is not the primary goal of qualitative research, these findings provide valuable insights specific to the context of the study. Future research could aim to include larger and more varied participant groups, explore different regions, and incorporate both qualitative and quantitative methods to offer a more comprehensive understanding of the issues at hand. Despite these limitations, the study’s strengths include rigorous framework analysis, adherence to ethical standards, and input from various stakeholders. Although the analysis was thorough, it still relied on the subjective interpretations of the researchers. However, quality indicators like audit trails and triangulation further enhanced the credibility and reliability of the findings, laying a solid foundation for understanding the complex issues surrounding oral healthcare access.
Implications and future recommendations
The study underscores the need for reforms to improve oral healthcare access for children with disabilities in KSA. It recommends integrating comprehensive training on managing children with disabilities into both undergraduate and postgraduate dental education. This training should cover practical skills, communication, and empathy to better prepare general dentists for treating people with disabilities, reducing dependence on specialized centres and improving access to dental services.
Improving cultural competence in dental care is essential. Training should address local cultural norms to create inclusive environments where all patients feel comfortable. Regular workshops or seminars could be implemented in dental schools and professional development programs to enhance cultural awareness among dental practitioners. Strengthening collaboration between dental professionals, pediatricians, and allied health providers will also help ensure early detection and timely care for children with disabilities.
Continuous reinforcement of policies to improve accessibility, especially in rural and underserved areas, is needed. Key steps include ensuring clinics are physically accessible, expanding transportation options, and introducing mobile or home care services to support families who face difficulties traveling. Additionally, providing financial support through expanded subsidized services, broader insurance coverage, and financial aid programs can alleviate the burden on families, ensuring that cost does not become a barrier to necessary care.
Limited knowledge among caregivers and the community regarding oral health importance highlighted the limited levels of awareness. Public health campaigns could be launched to raise awareness. These campaigns might include community-based workshops, the distribution of educational materials, and direct engagement with caregivers in settings such as clinics and schools to enhance their understanding of oral health and encourage preventive care.
This study adds to the literature by including various stakeholders’ perspectives on the challenges parents of children with disabilities face in accessing oral healthcare. Future research could also incorporate the voices of children and adults with disabilities to better inform the pathways through care alongside the progress and pitfalls to improving their oral health and overall well-being.
Conclusion
The study identifies barriers at various levels to accessing oral healthcare for parents of children with disabilities in KSA. An important component of access is ensuring adequate training for dental professionals, addressing financial constraints to enable parents to access care with greater ease, and improving physical accessibility to oral health care services. Providing solutions involves enhanced dental education, improved accessibility to oral health care, better Interprofessional collaboration with other medical and health related disciplines and developing sustainable financial support schemes. Addressing these areas appears crucial when the aim is to reduce disparities and improve the overall health and well-being of children with disabilities.
Acknowledgements
The authors would like to acknowledge the King Salman Center for Disability Research for funding this study through Research Group no. KSRG-2024-052.
Abbreviations
- (UNICEF)
The United Nations Children’s International Emergency Fund
- KSA
Kingdom of Saudi Arabia
- CSHCN
Children with Special Healthcare Needs
Author contributions
M.A. and J.O. conceived the ideas and designed the methods. M.A. conducted data collection and analysis, wrote the manuscript, and led the writing process. A.J. conducted data collection and contributed to both the analysis and writing. J.O. contributed to the analysis, participated in the writing, and offered feedback. S.B. provided insights on methods, supported data analysis, and offered feedback on the draft. All authors contributed to manuscript revisions.
Funding
The authors extend their appreciation to the King Salman Center For Disability Research for funding this work through Research Group no KSRG-2024-052.
Data availability
All data analyzed during this study are included in this manuscript.
Declarations
Ethics approval and consent to participate
Ethical approval for this study was obtained from the Institutional Review Board of King Saud University (Ref. No. 23/0475/IRB). The study adhered to relevant ethical guidelines and regulations. Informed consent was obtained from all participants prior to their involvement in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.UNICEF, Seen. Counted, Included: Using data to shed light on the well-being of children with disabilities. 2021. https://data.unicef.org/resources/children-with-disabilities-report-2021/. Accessed 7 July 2024.
- 2.Population and Housing Census, the Kingdom of Saudi Arabia. 2024. Available: https://www.apd.gov.sa/en/statistics. Accessed 1 December 2024.
- 3.Allerton LA, Welch V, Emerson E. Health inequalities experienced by children and young people with intellectual disabilities: A review of literature from the United Kingdom. J Intellect Disabil. 2011;15(4):269–78. [DOI] [PubMed] [Google Scholar]
- 4.Gréaux M, Moro MF, Kamenov K, Russell AM, Barrett D, Cieza A. Health equity for persons with disabilities: a global scoping review on barriers and interventions in healthcare services. Int J Equity Health. 2023;22(1):236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lam PPY, Du R, Peng S, McGrath CPJ, Yiu CKY. Oral health status of children and adolescents with autism spectrum disorder: A systematic review of case-control studies and meta-analysis. Autism. 2020;24(5):1047–66. [DOI] [PubMed] [Google Scholar]
- 6.Wilson NJ, Lin Z, Villarosa A, George A. Oral health status and reported oral health problems in people with intellectual disability: A literature review. J Intell Dev Disabil. 2019;44(3):292–304. [Google Scholar]
- 7.Robertson MD, Schwendicke F, de Araujo MP, Radford JR, Harris JC, McGregor S, et al. Dental caries experience, care index and restorative index in children with learning disabilities and children without learning disabilities; a systematic review and meta-analysis. BMC Oral Health. 2019;19(146):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anders PL, Davis EL. Oral health of patients with intellectual disabilities: a systematic review. Spec Care Dentist. 2010;30(3):110–7. [DOI] [PubMed] [Google Scholar]
- 9.Whelton H, Crowley E, Nunn J, Murphy A, Guiney H, Cronin M et al. Oral health of children attending special needs schools and day care centres. 2008.
- 10.Ward LM, Cooper S-A, Hughes-McCormack L, Macpherson L, Kinnear D. Oral health of adults with intellectual disabilities: a systematic review. J Intellect Disabil Res. 2019;63(11):1359–78. [DOI] [PubMed] [Google Scholar]
- 11.Horwitz SM, Kerker BD, Owens PL, Zigler E. The health status and needs of individuals with mental retardation. New Haven, Connecticut: Department of Epidemiology and Public Health, Yale University School of Medicine; 2000. [Google Scholar]
- 12.Hsiao S-Y, Chen P-H, Huang S-S, Yen C-W, Huang S-T, Yin S-Y, et al. Dental treatment needs and related risk factors among school children with special needs in Taiwan. J Personalized Med. 2021;11(6):452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ajami BA, Shabzendedar M, Rezay YA, Asgary M. Dental treatment needs of children with disabilities. J Dent Res Dent Clin Dent prospects. 2007;1(2):93–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alwadi MA, AlJameel AH, Baker SR, Owens J. Access to oral health care services for children with disabilities: a mixed methods systematic review. BMC Oral Health. 2024;24(1):1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson NJ, Lin Z, Villarosa A, Lewis P, Philip P, Sumar B, et al. Countering the poor oral health of people with intellectual and developmental disability: a scoping literature review. BMC Public Health. 2019;19:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abduludin DMA, Rahman NA, Adnan MM, Yusuf A. Experience of caregivers caring for children with cerebral palsy in accessing oral health care services: A qualitative study. Archives Orofac Sci. 2019;14(2):133–46. [Google Scholar]
- 17.Parry JA, Newton T, Linehan C, Ryan C. Dental visits for autistic children: a qualitative focus group study of parental perceptions. JDR Clin Translational Res. 2023;8(1):36–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Du RY, Yiu CKY, King NM. Oral health behaviours of preschool children with autism spectrum disorders and their barriers to dental care. J Autism Dev Disord. 2019;49:453–9. [DOI] [PubMed] [Google Scholar]
- 19.Junnarkar VS, Tong HJ, Hanna KMB, Aishworiya R, Duggal M. Qualitative study on barriers and coping strategies for dental care in autistic children: Parents’ perspective. Int J Pediatr Dent. 2023;33(2):203–15. [DOI] [PubMed] [Google Scholar]
- 20.Kachwinya SM, Kemoli AM, Owino R, Okullo I, Bermudez J, Seminario AL. Oral health status and barriers to oral healthcare among children with cerebral palsy attending a health care center in Kampala, Uganda. BMC Oral Health. 2022;22(1):656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu N, Drake M, Kruger E, Tennant M. Determining the barriers to access dental services for people with a disability: A qualitative study. Asia Pac J Health Manage. 2022;17(1):75–83. [Google Scholar]
- 22.GOV.SA. 2024. Rights of People with Disabilities. https://my.gov.sa/wps/portal/snp/careaboutyou/RightsOfPeopleWithDisabilities. Accessed 2 December 2024.
- 23.AlHammad KAS, Hesham AM, Zakria M, Alghazi M, Jobeir A, AlDhalaan RM, et al. Challenges of autism spectrum disorders families towards oral health care in Kingdom of Saudi Arabia. Pesquisa Brasileira em Odontopediatria e Clínica Integrada. 2020;20(e5178):1–7. [Google Scholar]
- 24.Alshihri AA, Al-Askar MH, Aldossary MS. Barriers to Professional Dental Care among Children with Autism Spectrum Disorder. J Autism Dev Disord. 2021;51(8):2988–94. [DOI] [PubMed] [Google Scholar]
- 25.Zahran SS, Bhadila GY, Alasiri SA, Alkhashrami AA, Alaki SM. Access to dental care for children with special health care needs: a cross-sectional community survey within Jeddah, Saudi Arabia. J Clin Pediatr Dentistry. 2023;47(1):50–7. [DOI] [PubMed] [Google Scholar]
- 26.Al-Shehri SAM. Access to dental care for persons with disabilities in Saudi Arabia (Caregivers’ perspective). J Disabil Oral Health. 2012;13(2):51–61. [Google Scholar]
- 27.Alfaraj A, Halawany HS, Al-Hinai MT, Al-Badr AH, Alalshaikh M, Al-Khalifa KS. Barriers to dental care in individuals with special healthcare needs in Qatif, Saudi Arabia: a caregiver’s perspective. Patient Prefer Adherence. 2021:15:69–76. [DOI] [PMC free article] [PubMed]
- 28.Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–60. [DOI] [PubMed] [Google Scholar]
- 29.Ritchie J, Spencer L. Qualitative data analysis for applied policy research. Analyzing qualitative data: Routledge; 2002. pp. 173–94. [Google Scholar]
- 30.Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19(2):127–40. [DOI] [PubMed] [Google Scholar]
- 32.Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative research practice. London: Sage; 2003. [Google Scholar]
- 33.O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–51. [DOI] [PubMed] [Google Scholar]
- 34.Lincoln YS, Guba EG. Naturalistic Inquiry. Beverly Hills, CA: Sage Publications, Inc; 1985. [Google Scholar]
- 35.Denzin NK. The research act: A theoretical introduction to sociological methods. New York: Routledge; 2017. [Google Scholar]
- 36.Alumran A, Almulhim L, Almolhim B, Bakodah S, Aldossary H, Alakrawi Z. Preparedness and willingness of dental care providers to treat patients with special needs. Clinical, cosmetic and investigational dentistry. 2018:231–6. [DOI] [PMC free article] [PubMed]
- 37.Unified National Platform. Rights of People with Disabilities. 2002. https://www.my.gov.sa/wps/portal/snp/careaboutyou/RightsOfPeopleWithDisabilities#header2_10. Accessed 10 August 2024.
- 38.Vertel N, Harrison RL, Campbell KM. Access to dental services for children with special health care needs: A pilot study at the dental department of BC Children’s Hospital. J Can Dent Assoc. 2017;83(h6):1488–2159. [PubMed] [Google Scholar]
- 39.Alwadi MAM, Baker SR, Owens J. Oral health experiences and perceptions of children with disabilities in the Kingdom of Saudi Arabia. Int J Pediatr Dent. 2022;32(6):856–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Alwadi MAM, Baker SR, Owens J. Ethnographic perspectives of mothers and professionals on including children with disabilities in oral health in the Kingdom of Saudi Arabia. Int J Pediatr Dent. 2024;34(6):832-842 [DOI] [PubMed]
- 41.Alumran A, Almulhim L, Almolhim B, Bakodah S, Aldossary H, Alrayes SA. Are dental care providers in Saudi Arabia prepared to treat patients with special needs? J Multidisciplinary Healthc. 2019;12:281–90. [DOI] [PMC free article] [PubMed]
- 42.Nayak UA, Hijji RB, Aljuhani MA, Aljuhani LA, Almarwani RN, Nayak PA. Dentists’ Knowledge, Attitude and Practices Regarding Dental Care for Children with Special Healthcare Needs in Saudi Arabia. J Clin Diagn Res. 2022;16(10):ZC11–6. [Google Scholar]
- 43.Casamassimo PS, Seale NS, Ruehs K. General dentists’ perceptions of educational and treatment issues affecting access to care for children with special health care needs. J Dent Educ. 2004;68(1):23–8. [PubMed] [Google Scholar]
- 44.O’Rourke S, Dougall A, O’Sullivan M. Does education in special care dentistry increase people’s confidence to manage the care of a more diverse population? Spec Care Dentist. 2023;43(6):743–50. [DOI] [PubMed] [Google Scholar]
- 45.Michael K, Dror MG, Karnieli-Miller O. Students’ patient-centered-care attitudes: The contribution of self-efficacy, communication, and empathy. Patient Educ Couns. 2019;102(11):2031–7. [DOI] [PubMed] [Google Scholar]
- 46.Como DH, Florindez-Cox LI, Stein Duker LI, Cermak SA. Oral Health Barriers for African American Caregivers of Autistic Children. Int J Environ Res Public Health. 2022;19(24):17067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Committee USDoHaHSOHC. US Department of Health and Human Services oral health strategic framework, 2014–2017. Public Health Rep. 2016;131(2):242–57. [PMC free article] [PubMed] [Google Scholar]
- 48.Dwiel K, Hesketh M, Alpert J, Cellini J, Goodell K, Phillips R, et al. The impact of oral health training for primary care clinicians: a systematic review. Fam Med. 2019;51(3):251–61. [DOI] [PubMed] [Google Scholar]
- 49.GOV.SA. 2024. Healthcare. https://www.my.gov.sa/wps/portal/snp/aboutksa/HealthCareInKSA/?lang=en. Accessed 2 December 2024.
- 50.Zakirulla M, Laheq MT, Assiri MNM, Al–Alhinyah SAN, Aldowsari M, Alzakari FI, et al. Oral health care knowledge among nurses in the pediatric intensive care units in Abha, Saudi Arabia. J Res Med Dent Sci. 2021;9(6):7–14. [Google Scholar]
- 51.Alshathri B, Aljasser N, Kofi M. Knowledge of oral health among family medicine physicians in Riyadh, Saudi Arabia 2020. J Family Med Prim Care. 2020;9(9):4761–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Almazrooa SA, Binmadi NO. The knowledge and attitude of physicians’ toward the oral medicine specialty. J Oral Maxillofacial Surg Med Pathol. 2021;33(1):83–8. [Google Scholar]
- 53.Saudi Commission for Health Specialties. CPD Activities Accreditation. 2024. https://scfhs.org.sa/en/cpds-activities-accreditation. Accessed 2 December 2024.
- 54.Braun PA, Cusick A. Collaboration between medical providers and dental hygienists in pediatric health care. J Evid Based Dent Pract. 2016;16:59–67. [DOI] [PubMed] [Google Scholar]
- 55.Alsarhan F, Valax M. Conceptualization of wasta and its main consequences on human resource management. Int J Islamic Middle East Finance Manage. 2021;14(1):114–27. [Google Scholar]
- 56.Star JM, Flores A, Leyva E, Foertsch C. Barriers to routine dental care for children with special health care needs. Spec Care Dentist. 2024;44(2):592–9. [DOI] [PubMed] [Google Scholar]
- 57.Alshatrat SM, Al-Bakri IA, Al-Omari WM. Dental Service Utilization and Barriers to Dental Care for Individuals with Autism Spectrum Disorder in Jordan: A Case-Control Study. Int J Dent. 2020;2020(1):3035463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cermak SA, Stein Duker LI, Williams ME, Lane CJ, Dawson ME, Borreson AE, et al. Feasibility of a sensory-adapted dental environment for children with autism. Am J Occup Therapy. 2015;69(3):p69032200201–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fallea A, Zuccarello R, Calì F. Dental anxiety in patients with borderline intellectual functioning and patients with intellectual disabilities. BMC Oral Health. 2016;16:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shapiro M, Melmed RN, Sgan-Cohen HD, Eli I, Parush S. Behavioural and physiological effect of dental environment sensory adaptation on children’s dental anxiety. Eur J Oral Sci. 2007;115(6):479–83. [DOI] [PubMed] [Google Scholar]
- 61.Owens J, Dyer TA, Mistry K. People with learning disabilities and specialist services. Br Dent J. 2010;208(5):203–5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data analyzed during this study are included in this manuscript.