Abstract
Background
Vasoepididymostomy (VE) is an important surgical treatment to achieve natural conception for patients with obstructive azoospermia (OA), and only unilateral VE can be performed under certain conditions, such as OA patients with congenital unilateral absence of the vas deferens (CUAVD) and some acquired OA. There is a lack of relevant reports assessing the clinical outcomes of unilateral VE in OA patients with different causes. This study is aimed to describe the clinical features and evaluate treatments and outcomes of unilateral single-armed VE in OA patients.
Methods
From December 2015 to June 2021, 46 OA patients (including 13 CUAVD-associated OA and 33 acquired OA) underwent unilateral single-armed VE in Shanghai General Hospital (Shanghai, China). Patient information, semen analysis, hormone profiles, and treatment information were collected, and the clinical outcomes were evaluated.
Results
Obstruction in distal of unilateral vas deferens (16/46) was the most common cause for OA patients underwent unilateral VE, and CUAVD accounts for 28.4% (13/46). The overall patency rate was 50.0% (23/46), with 38.5% (5/13) for the CUAVD group and 54.5% (18/33) for the acquired group (p > 0.05). The natural pregnancy rates in CUAVD group and acquired group were 20.0% and 33.3%, respectively (p > 0.05).
Conclusions
These findings suggest unilateral single-armed VE can achieve high patency and pregnancy rates in OA patients, whether for CUAVD or acquired OA patients.
Keywords: Unilateral vasoepididymostomy, Obstructive azoospermia, Patency, Pregnancy
Highlight Box
Key findings
• Unilateral single-armed vasoepididymostomy (VE) can achieve high patency and pregnancy rates in obstructive azoospermia (OA) patients, whether for congenital unilateral absence of the vas deferens (CUAVD) or acquired OA patients.
What is known and what is new?
• Bilateral VE exhibited higher risk ratio of patency rate than unilateral VE, however only unilateral VE can be performed under certain conditions, such as OA patients with CUAVD and some acquired OA.
• Unilateral VE can achieve high patency and pregnancy rates in both CUAVD and acquired OA patients.
What is the implication, and what should change now?
• Unilateral single-armed VE is a feasible option for OA patients with different causes.
Introduction
15% of the infertile population is identified as azoospermia, and can be classified into two general categories: obstructive azoospermia (OA) and nonobstructive azoospermia (NOA). Obstructive azoospermia is the result of blockage or loss of any segments of the male reproductive tract, and accounts for 40% of all azoospermia cases (1). Etiologically, OA may be acquired or congenital (2,3). Post-vasectomy obstruction, infection, iatrogenic injury or trauma are the main causes of acquired OA. While congenital OA is mainly caused by congenital absence of the vas deferens (CAVD).
Though with obstruction of any location, from the rete testis to the ejaculatory ducts, patients with OA are characterized by normal spermatogenesis. Thus, those patients can get their own offspring through surgical reconstruction or retrieval of sperm. Vasoepididymostomy (VE) is an important surgical treatment for epididymal obstructive azoospermia, with satisfactory patency and pregnancy rates (4,5). A recent systematic review and meta-analysis of microsurgical VE outcomes showed the overall patency and pregnancy rates of 64.1% and 31.1%, respectively (6). When compared with unilateral VE, the patency rate of bilateral VE exhibited higher risk ratio of 1.38% (6). However, only unilateral VE can be performed under certain conditions, such as OA patients with congenital unilateral absence of the vas deferens (CUAVD) and some acquired OA.
So far, although some successful microsurgical reconstruction of unilateral VE have been reported in case reports, large-sample and long-term follow-up cases have rarely been reported. The present study is aimed to summarize the clinical outcomes of unilateral single-armed VE, analyze the reasons to undergo unilateral single-armed VE and assess the potential application and value of unilateral VE in OA patients. This manuscript is written following STROBE checklist.
Methods
Patients
This study was approved by the Ethics Committee of Shanghai General Hospital (approval No. 2017KY020-2), and written informed consent was obtained from all the patients. Patients who underwent unilateral VE between December 2015 and June 2021 were included in this study. All the patients had normal karyotypes, and no Y chromosomal microdeletions were found. Their female partners had a normal fertility profile. Men with aspermia due to ejaculatory disorders such as anejaculation or retrograde ejaculation were not included in this study. Patient information and laboratory data were collected from the patient records.
Unilateral vasoepididymostomy
Unilateral single-armed VE was performed according to the procedures as described previously (6,7). Briefly, scrotal exploration and testicular biopsy was performed to confirm normal spermatogenesis. Then the saline or trypan blue was injected to the vas deferens using a 24-gauge angio catheter sheath to confirm the patency of the seminal vesicle side. According to intraoperative findings, a unilateral VE was finally underwent using the modified single-armed 2-suture longitudinal vasoepididymostomy (SA-LIVE) technique (7,8). Briefly, under a Carl Zeiss operating microscope, two single-armed 10–0 nylon sutures were sequentially placed outside-in through the mucosal layer of the vas deferens, parallelly through the epididymal tubule, then placed inside-out through the mucosal layer of the vas deferens. Then all the sutures were tied together, and the epididymal tubule was gently intussuscepted into the lumen of the vas deferens.
Follow-up
All the patients were followed up every 3–6 months. Semen analysis was performed at four weeks after surgery, and then at 2-month intervals until pregnancy was achieved. Patency was defined as the sperm concentration more than 1 million per milliliter in at least one post-operative ejaculate sample. Pregnancy was defined as an identified gestational sac by ultrasound examination.
Statistical analysis
Parameters are described as the mean ± standard deviation (SD). The patency and pregnancy rates were calculated. The statistical analysis was conducted using SPSS software, version 19.0 (SPSS Inc., Chicago, IL, USA). P value < 0.05 was considered to be statistically significant.
Results
Demographics
A total of 46 OA patients underwent unilateral VE between December 2015 and June 2021, including 13 patients with CUAVD and 33 patients with acquired OA. The ages (mean ± SD) of the male patients and their female partners in the CUAVD group and acquired group were 28.2 ± 3.0, 26.1 ± 1.8 and 30.8 ± 5.9, 27.3 ± 3.1 years, respectively. The volume and pH of the semen sample in CUAVD group were lower than those of acquired group (1.7 ± 0.9 vs. 2.5 ± 1.1 ml, 7.1 ± 0.3 vs. 7.3 ± 0.1, respectively). While there were no significant differences in infertility duration, testicular size and hormone levels between the two groups (Table 1).
Table 1.
Characteristics of patients underwent unilateral vasoepididymostomy
| Characteristics | Total | CUAVD group | Acquired group | p value |
|---|---|---|---|---|
| Patients, n | 46 | 13 | 33 | |
|
Age (year), Mean ± SD Patients Female partners |
30.1 ± 5.4 26.9 ± 2.8 |
28.2 ± 3.0 26.1 ± 1.8 |
30.8 ± 5.9 27.3 ± 3.1 |
0.060 0.116 |
| Infertility duration (month), Mean ± SD | 34.2 ± 32.1 | 32.2 ± 22.1 | 35.0 ± 35.5 | 0.788 |
| Testicular size, ml | ||||
| Left | 14.3 ± 5.8 | 15.1 ± 4.2 | 14.0 ± 6.4 | 0.594 |
| Right | 15.0 ± 6.8 | 13.1 ± 5.5 | 15.7 ± 7.2 | 0.234 |
| Semen Volume, ml | 2.2 ± 1.1 | 1.7 ± 0.9 | 2.5 ± 1.1 | 0.028 |
| Semen pH | 7.2 ± 0.2 | 7.1 ± 0.3 | 7.3 ± 0.1 | 0.032 |
| Semen fructose | 0.075 | |||
| Negative | 2 | 2 | 0 | |
| Positive | 44 | 11 | 33 | |
| FSH, IU/L | 5.0 ± 2.4 | 4.7 ± 1.8 | 5.1 ± 2.7 | 0.597 |
| LH, IU/L | 4.8 ± 1.8 | 4.9 ± 1.4 | 4.8 ± 2.0 | 0.951 |
| T, ng/ml | 4.4 ± 3.0 | 3.5 ± 2.1 | 4.7 ± 3.3 | 0.218 |
FSH normal range: 1.27–19.26 IU/L; LH normal range: 1.24–8.62 IU/L; T normal range: 1.75–7.81 µg/L. CUAVD: congenital unilateral absence of the vas deferens; FSH: follicle‑stimulating hormone; LH: luteinizing hormone; SD: standard deviation; T: testosterone
Intraoperative findings and treatments
Unilateral single-armed VE was performed in all the 46 patients. The causes for performing unilateral single-armed VE in acquired group were as follows: obstruction in distal of unilateral vas deferens (n = 16), unilateral testicular atrophy caused by cryptorchidism (n = 6), unilateral epididymal dysplasia (n = 4), idiopathic (n = 3), unilateral testicular atrophy caused by epididymo-orchitis (n = 2) and unilateral intratesticular obstruction (n = 2) (Table 2). Three patients in the CUAVD group underwent unilateral cross VE due to obstruction in contralateral caput of epididymis, and one patient in the acquired group underwent unilateral cross VE due to obstruction in distal of unilateral vas deferens and contralateral testicular atrophy. There were no significant differences in the side and site of anastomosis between the two groups (Table 3).
Table 2.
Causes for performing unilateral single-armed VE
| Causes | n (%) |
|---|---|
| Obstruction in distal of unilateral vas deferens | 16 (34.8) |
| Unilateral testicular atrophy caused by cryptorchidism | 6 (13.0) |
| Unilateral epididymal dysplasia | 4 (8.7) |
| Idiopathic | 3 (6.5) |
| Unilateral testicular atrophy caused by epididymo-orchitis | 2 (4.3) |
| Unilateral intratesticular obstruction | 2 (4.3) |
| CUAVD | 13 (28.4) |
CUAVD: congenital unilateral absence of the vas deferens; VE: vasoepididymostomy
Table 3.
Clinical outcomes of patients underwent unilateral VE in CUAVD-associated or acquired OA group
| Variables | CUAVD group | Acquired group | p value |
|---|---|---|---|
| Side of anastomosis, n (%) | 0.161 | ||
| Left | 10 (76.9%) | 18 (55.5%) | |
| Right | 3 (23.1%) | 15 (44.5%) | |
| Site of anastomosis, n (%) | 1.000 | ||
| Caput | 4 (30.7%) | 9 (27.3%) | |
| Corpus or caudal | 9 (69.3%) | 24 (72.7%) | |
| Patency, n (%) | 5/13 (38.5%) | 18/33 (54.5%) | 0.326 |
| Pregnancy, n (%) | 6/13 (46.2%) | 11/33 (33.3%) | 0.637 |
| Natural Pregnancy, n (%) | 1/5 (20%) | 6/18 (33.3%) | 1.000 |
CUAVD: congenital unilateral absence of the vas deferens; OA: obstructive azoospermia
Patency and pregnancy
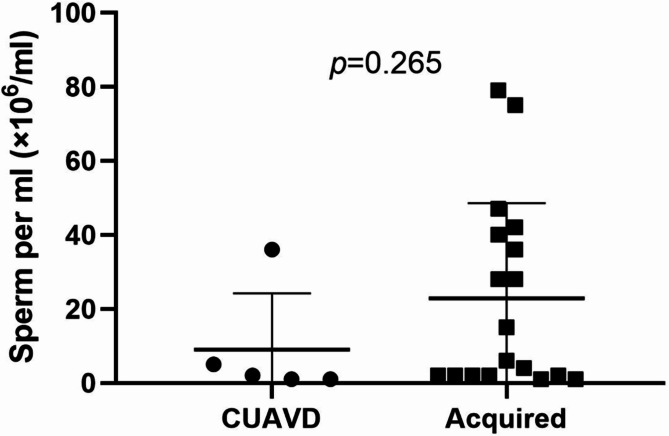
Sperm was detected in the ejaculate between 1 and 6 months after surgery. The overall patency rate was 50.0% (23/46), with 38.5% (5/13) for the CUAVD group and 54.5% (18/33) for the acquired group. There was no statistical significance of the sperm concentration after recanalization in CUAVD group and acquired group (p = 0.265) (Fig. 1). Five patients underwent assisted reproductive technology (ART) after surgery in CUAVD group, and 8 patients in acquired group. Notably, there was 1 couple in each group achieved pregnancy through intracytoplasmic sperm injection (ICSI) using the sperm in the fresh ejaculate. The natural pregnancy rate was 20.0% (1/5) for CUAVD group and 33.3% (6/18) for acquired group (p = 1.000) (Table 3).
Fig. 1.
Sperm concentration after recanalization in CUAVD group and acquired group
Discussion
Vasoepididymostomy (VE) is one of representative methods of vasal repair to get natural conception for patients with obstructive azoospermia (OA). The surgical procedures and techniques of VE are constantly innovated and improved. Several modified single-armed VE techniques with high patency and pregnancy rates have been reported (8–11). In our center, we also attempted to explore modified surgical techniques to improve the rate of spontaneous pregnancy rate (7,8,12).
Epididymal obstruction is considered as a common cause of OA, and quite a large part of these patients have an epididymitis history. In a cohort of 110 patients underwent VE, 42% of the patients had a history of epididymitis (13). What’s worse, Binsaleh reported that 83.3% (10/12) of the patients could only underwent unilateral VE due to genitourinary infection (14). With surgical techniques modified and improved, high patency can be also achieved in patients underwent unilateral VE. Recently, multiple reports have showed a patency rate of 45.8–66.7% in unilateral VE (10,13,15). In the present study, an overall patency rate of 50.0% (23/46) was achieved, which was consistent with previous studies.
To date, most studies upon unilateral VE have been conducted with small samples. And seldom studies focused on intraoperative findings for unilateral VE. In 2017, Peng et al. reported a retrospective study including 51 patients underwent unilateral VE. Contralateral intratesticular obstruction (n = 26) was the main cause of unilateral reconstruction, followed by distal vas deferens obstruction (n = 14), contralateral absent vas deferens (n = 6) and cryptorchidism (n = 5) (16). Different from their research, the current study showed that obstruction in distal of unilateral vas deferens (16/46) was the most common cause, while unilateral intratesticular obstruction was found in only two patients. Notably, 28.4% (13/46) of the OA patients performing unilateral single-armed VE presented with CUAVD, suggesting that CUAVD patients with OA seeking for natural conception is not a small population.
Several studies have compared the clinical outcomes between unilateral VE and bilateral VE (13,17,18), however no studies have focused on the efficacy of unilateral VE in OA of different causes. To the best of our knowledge, this is the first study reporting the clinical outcomes of unilateral VE between congenital and acquired OA patients. Our results showed the patency and natural pregnancy rates in CUAVD group and acquired group were 38.5% and 54.5%, 20.0% and 33.3%, respectively. There was no statistical significance of patency and pregnancy rates between the two groups (p > 0.05). These findings suggest unilateral single-armed VE is a feasible option for OA patients with different causes.
Apart from high rates of patency and natural pregnancy, VE has potential benefits over assisted reproductive technology (ART), including low costs, no additional risks to the female partner and fetus and can achieve multiple pregnancies (13,19). It is suggested that VE should be the first option for epididymal obstruction, not an alternative treatment after ART failure (16). Our results showed unilateral VE could also achieve a satisfactory result, whether in patients with CUAVD-associated or acquired OA. However, ART should be taken into account when making intraoperative and postoperative decisions. In the current study, the epididymal and testicular sperms were cryopreserved during VE as a backup of the procedure. And 13 patients underwent ART after surgery, including 2 couples achieved pregnancy through ICSI using the sperm in the fresh ejaculate. Thus, ART can be a remedy after unilateral single-armed VE for patients.
Our study has several limitations. Given the retrospective design, potential information bias is possible. We failed to collect some important surgical variables, such as operation and patency time. The short follow-up period is also a limitation. A prolonged observation period is beneficial in the comparison of patency and natural pregnancy. Due to the low incidence of CUAVD, this study contained a small number of patients in CUAVD group. Thus, a prospective, multicenter, and large sample cohort study is needed.
Conclusions
In summary, unilateral single-armed VE can achieve high patency and pregnancy rates in OA patients, whether for CUAVD or acquired OA patients. When considering the treatments, unilateral single-armed VE is a feasible option to OA patients with different causes.
Acknowledgements
Not applicable.
Author contributions
(I) Conception and design: YZ, PL and ZE. (II) Administrative support: JD, CY and LZ. (III) Provision of study materials or patients: YH, TR. (IV) Collection and assembly of data: YZ and EZ. (V) Data analysis and interpretation: YD, YT and FZ. (VI) Manuscript writing: All authors. (VII) Final approval of manuscript: All authors.
Funding
This work was supported by grants from Shanghai science and technology innovation action plan project (20Y11907600), National Natural Science Foundation of China (82171586,82001530), Clinical Research Innovation Plan of Shanghai General Hospital (CTCCR-2021C17) and Strategic Priority Research Program of the Chinese Academy of Sciences (XDA16020701).
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study obtained approval from the Ethics Committee of Shanghai General Hospital (No.: 2017KY020-2) and informed consent was obtained from all individual participants.
Consent for publication
All authors have completed the ICMJE uniform disclosure form. The authors have no conflicts of interest to declare.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yihong Zhou and Jianjun Dong are contributed equally to this work.
Contributor Information
Peng Li, Email: fengzhongjiezou@163.com.
Erlei Zhi, Email: zhzzer1985@126.com.
References
- 1.Wosnitzer MS, Goldstein M. Obstructive azoospermia. Urol Clin North Am 2014;41:83–95. [DOI] [PubMed]
- 2.Fogle RH, Steiner AZ, Marshall FE, et al. Etiology of azoospermia in a large nonreferral inner-city population. Fertil Steril 2006;86:197-9. [DOI] [PubMed]
- 3.Practice. The management of obstructive azoospermia: a committee opinion. Fertil Steril 2019;111:873 − 80. [DOI] [PubMed]
- 4.Chan PT, Brandell RA, Goldstein M. Prospective analysis of outcomes after microsurgical intussusception vasoepididymostomy. BJU Int 2005;96:598–601. [DOI] [PubMed]
- 5.Tanrikut C, Goldstein M. Obstructive azoospermia: a microsurgical success story. Semin Reprod Med 2009;27:159 − 64. [DOI] [PubMed]
- 6.Yoon YE, Lee HH, Park SY, et al. The role of vasoepididymostomy for treatment of obstructive azoospermia in the era of in vitro fertilization: a systematic review and meta-analysis. Asian J Androl 2018;21:67–73. [DOI] [PMC free article] [PubMed]
- 7.Li P, Liu N, Zhi E, et al. Vasal vessel-sparing microsurgical single-armed vasoepididymostomy to epididymal obstructive azoospermia: A retrospective control study. Andrologia 2021;53:e14133. [DOI] [PubMed]
- 8.Liu N, Li P, Zhi E, et al. A modified single-armed microsurgical vasoepididymostomy for epididymal obstructive azoospermia: intraoperative choice and postoperative consideration. BMC Urol 2020;20:121. [DOI] [PMC free article] [PubMed]
- 9.Yuan Y, Fang D, Lei H, et al. Rat model and validation of a modified single-armed suture technique for microsurgical vasoepididymostomy: Guo’s SA-LIVE. Andrology 2021;9:361-7. [DOI] [PubMed]
- 10.Lyu KL, Zhuang JT, Li PS, et al. A novel experience of deferential vessel-sparing microsurgical vasoepididymostomy. Asian J Androl 2018;20:576 − 80. [DOI] [PMC free article] [PubMed]
- 11.Zhao L, Tu XA, Zhuang JT, et al. Retrospective analysis of early outcomes after a single-armed suture technique for microsurgical intussusception vasoepididymostomy. Andrology 2015;3:1150-3. [DOI] [PubMed]
- 12.Li P, Liu NC, Zhi EL, et al. 3D digital image microscope system-assisted vasovasostomy and vasoepididymostomy in rats. Asian J Androl 2021;23:396-9. [DOI] [PMC free article] [PubMed]
- 13.Shiraishi K, Matsuyama H. Outcomes of partial intussusception and endo-to-side vasoepididymostomy in men with epididymal obstructive azoospermia. Int J Urol 2020;27:1124-9. [DOI] [PubMed]
- 14.Binsaleh S. Two-suture single-armed longitudinal intussusception vasoepididymostomy for obstructive azoospermia: report of patients characteristics and outcome. Int Urol Nephrol 2014;46:2271-7. [DOI] [PubMed]
- 15.Li JP, Zhang XZ, Wu JG, et al. Seminal plasma neutral alpha-glucosidase activity as an early predictor of patency and natural pregnancy after microsurgical vasoepididymostomy. Andrologia 2019;51:e13235. [DOI] [PubMed]
- 16.Peng J, Zhang Z, Yuan Y, et al. Pregnancy and live birth rates after microsurgical vasoepididymostomy for azoospermic patients with epididymal obstruction. Hum Reprod 2017;32:284-9. [DOI] [PubMed]
- 17.Wang SY, Fang YY, Zhang HT, et al. The effect of BMI and age on the outcomes of microsurgical vasoepididymostomy: a retrospective analysis of 181 patients operated by a single surgeon. Asian J Androl 2022. [DOI] [PMC free article] [PubMed]
- 18.Basourakos SP, Lewicki P, Punjani N, et al. Practice patterns of vasal reconstruction in a large United States cohort. Andrologia 2021;53:e14228. [DOI] [PubMed]
- 19.Meng MV, Greene KL, Turek PJ. Surgery or assisted reproduction? A decision analysis of treatment costs in male infertility. J Urol 2005;174:1926-31; discussion 31. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.