Abstract
Background
In the current era of rapid technological development, digital technology is progressively transforming the medical field. In palliative care, its integration is an inevitable trend, offering new possibilities for improving care delivery and patient outcomes.
Objective
This study aimed to review the application of digital technologies in palliative care, focusing on their advantages, challenges, and measurable impacts across diverse care settings.
Methods
A scoping review was conducted, evaluating studies published between January 1, 2000, and August 1, 2024. Searches were performed across PubMed, CINAHL, Web of Science, Scopus, and the Cochrane Library. Original studies assessing digital interventions within palliative care settings were included. Data extraction included study design, sample size, setting, intervention type, and outcomes. Methodological quality was appraised using appropriate tools for randomized controlled trials (RCTs), non-randomized studies, mixed-methods studies, and qualitative studies. Two independent reviewers conducted the data extraction and quality appraisal, resolving disagreements through discussion.
Results
Twenty-four studies were included, examining digital technologies such as computer systems, virtual reality (VR), and wearable devices. Key interventions supported information provision, symptom monitoring, psychological support, and communication feedback. Digital tools demonstrated positive impacts on pain management, symptom distress, quality of life, and patient acceptability. Despite methodological strengths in most studies, limitations such as small sample sizes and inconsistent outcome measures were noted.
Conclusion
Digital technologies in palliative care demonstrate significant potential to improve patients’ quality of life and alleviate symptom burden through remote monitoring, real-time feedback, and personalized interventions. These innovations address limitations of the traditional biomedical model, enhancing the accessibility and overall quality of palliative care.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12904-024-01626-w.
Keywords: Digital technology, Palliative care, Computers, VR, Wearable device
Introduction
Palliative care seeks to improve the quality of life for patients with life-threatening illnesses and their families by alleviating physical, psychological, social, and spiritual suffering [1]. This care model is applicable at any stage of illness, not limited to end-of-life care, and is particularly essential for patients facing complex treatments or psychological distress [2].
As global aging accelerates and chronic illnesses such as cancer and dementia rise, the demand for palliative care is increasing dramatically. An estimated 56.8 million people currently require palliative care annually, a number expected to nearly double by 2060 [3]. However, only about 14% of those in need receive such services, reflecting a significant global care gap [4]. Studies predict that by 2060, around 48 million people worldwide will die from serious health-related suffering [5]. This indicates that the traditional biomedical model of institutionalized healthcare may not be sufficient to meet the growing demand for palliative care. Moreover, access to palliative care remains inadequate, especially in resource-limited regions, leading to a lack of essential support and care for many patients. This imbalance between supply and demand has prompted the medical community to explore new methods to expand the reach and quality of palliative care services.
In this context, the rapid development of digital technology presents new opportunities for palliative care. Digital technology encompasses fields such as computers, virtual reality (VR), and wearable devices, and its use in healthcare has demonstrated considerable potential. For instance, Gustafson et al. [6] used computers to establish social communication channels for advanced cancer patients and monitor symptoms with real-time feedback, finding that online support systems reduced symptom distress. Guenther et al. [7] employed immersive 360° VR interventions for palliative care patients, including videos for travel, relaxation, and meditation, which resulted in significant pain reduction. Wright et al. [8] utilized wearable devices to continuously monitor physiological indicators, such as heart rate and steps, in patients with advanced gynecologic cancer, enabling timely adjustments to treatment plans, and improving symptom management.
Despite promising outcomes, barriers such as high costs, limited accessibility, user acceptance, and data privacy concerns hinder the widespread adoption of digital technologies in palliative care. This review aims to systematically analyze the current state of digital technology in palliative care, focusing on intervention types, their impact on patient outcomes, and the challenges to their implementation. These insights will inform future research and guide the development of innovative, patient-centered approaches to palliative care.
Materials and methods
This study followed the scoping review framework by Arksey and O’Malley [9], with reporting guided by the PRISMA-ScR extension [10]. The research protocol was registered on the Open Science Framework (10.17605/OSF.IO/A4B3J).
Define the research questions
The primary research questions were:
① What digital technologies are currently applied in palliative care, and what are their functional domains?
② How do these technologies impact patient outcomes and care quality?
③ What barriers and facilitators affect the implementation of digital technologies in diverse palliative care settings?
Literature search strategy
Databases including PubMed, CINAHL, Web of Science, Scopus, and Cochrane Library were searched from January 1, 2000, to August 1, 2024. A combination of Medical Subject Headings (MeSH) and free-text terms was used to ensure comprehensive retrieval. MeSH terms included “Digital Technology,” “Palliative Care,” “Hospice Care Nursing,” “Terminal Care,” and “End-of-Life Care,” tailored for databases such as PubMed and CINAHL that support controlled vocabularies. Free-text terms, including “digital technology,” “internet,” “computers,” “virtual reality,” “VR,” “web,” “platform,” “wearable devices,” and “intelligent robot,” were used in databases without MeSH indexing, such as Scopus and Web of Science. Boolean operators (AND/OR) were used to combine terms, and search strategies were adjusted for the indexing systems of each database. Detailed search strategies are provided in Appendix 1.
Inclusion and exclusion criteria
Inclusion criteria:
① Studies involving adults (≥ 18 years) receiving palliative care.
② Original research assessing digital technologies in palliative care (RCTs, observational studies, qualitative studies, and mixed-methods).
Exclusion criteria:
① Reviews, conference abstracts, and inaccessible full texts.
② Study protocols, guidelines, opinions, or policy documents.
Literature screening
The EndNote X9™ bibliographic software (Clarivate Analytics, USA) was used to store and deduplicate the retrieved articles. Covidence systematic review software (Veritas Health Innovation, Australia) was utilized for screening titles and abstracts against the inclusion and exclusion criteria. Two reviewers (YHT, XL) independently screened the titles and abstracts, with a third reviewer (YW) resolving potential conflicts. The final selection of studies proceeded to full-text review.
Data extraction and analysis
Full-text articles selected during the screening stage were reviewed independently by two reviewers (YHT, HMX). Extracted data included author, country, publication year, study type, study population, sample size, intervention measures (technology, specific applications, content elements), intervention duration, outcome measures, and measurement tools. Any discrepancies were resolved through discussion with a third reviewer (YW).
Quality appraisal of studies
This study selected appropriate quality appraisal tools based on the study design of the included articles to ensure the scientific rigor and reliability of the evaluations. For randomized controlled trials (RCTs), the Cochrane Risk of Bias Tool [11] was used to assess potential biases. Non-randomized quantitative studies were evaluated using the Newcastle-Ottawa Scale (NOS) [12] to appraise cohort selection, comparability, and outcome measurement quality. Mixed-methods studies were assessed using the Joanna Briggs Institute (JBI) [13] checklist for mixed methods, focusing on the integration of quantitative and qualitative data. Qualitative studies were appraised with the Critical Appraisal Skills Programme (CASP) [14] tool, which evaluates the clarity of research questions and the trustworthiness of the data.
Results
Results of literature screening
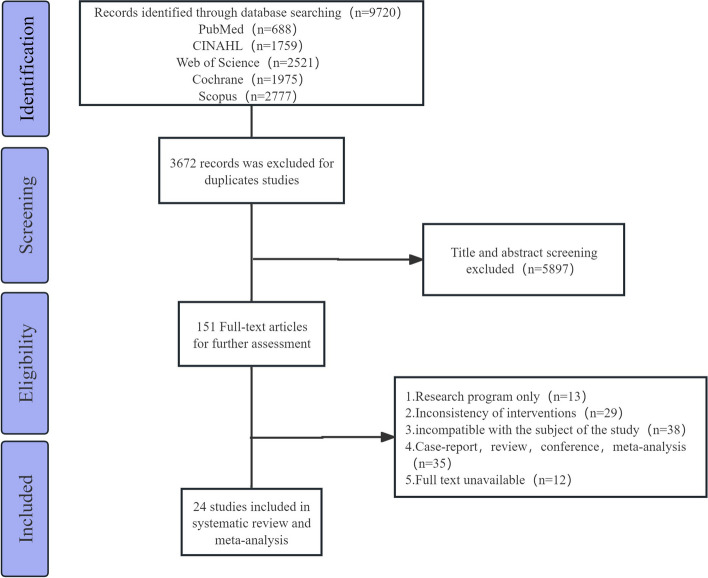
A total of 9,720 articles were initially retrieved. After removing duplicates, 6,048 articles remained. Following title and abstract screening, 5,897 articles were excluded. After full-text review, 127 articles were further excluded, resulting in the inclusion of 24 articles [6–8, 15–35]. See Fig. 1.
Fig. 1.
Flowchart of study selection
Basic characteristics of included studies
A total of 24 studies were included in this review after applying the inclusion and exclusion criteria. These studies were published between 2009 and 2024. Nine studies [6, 8, 17, 18, 20, 23, 30, 32, 34] were conducted in the United States, three in the United Kingdom [22, 27, 29], two in Australia [15, 33], two in Canada [19, 21], and two in Switzerland [28, 31]. The remaining six studies were conducted in China [35], Japan [26], Tanzania [25], India [16], Germany [7], and Italy [24]. The studies included six randomized controlled trials [6, 15, 22, 23, 29, 32], eleven quantitative non-randomized studies [7, 16, 20, 24, 26–28, 30, 33–35], six mixed-methods studies [8, 17–19, 21, 31], and one qualitative study (22). Five studies [16, 24, 28, 30, 32] were conducted in home settings, while the others [6–8, 15, 17–23, 25–27, 29, 31, 33–35] were conducted in hospitals or palliative care institutions. The basic characteristics of the included studies are presented in Table 1. A summary of digital technology applications in palliative care is provided in Table 2.
Table 1.
Basic characteristics of the studies
| Author & Year | Country | Study Type | Study Population | Sample Size | Intervention Measures | Outcome Measures and Instruments | ||
|---|---|---|---|---|---|---|---|---|
| Technology | Specific Application | Content | ||||||
| Wilkie et al. [34] 2009 | USA | Quantitative Non-Randomized Study | Advanced Cancer | 131 | Computer | PAINReportIt® | Symptom Assessment and Documentation | A①; B①; F①; G① |
| Gustafson et al. [6] 2013 | USA | RCT | Advanced Cancer | 246 | Computer | CHESS Coping with Lung Cancer website | Social Communication Channels, Symptom Monitoring, and Feedback | B② |
| Steel et al. [32] 2016 | USA | RCT | Advanced Cancer | 261 | Computer | A psychoeducational web site and a collaborative care coordinator | psychoeduca-tional、self-management(record symptoms and monitor、Communication、Relaxation Techniques and Educational Videos、Resource Library) | A②; B③④; C①; E①② |
| Tieman et al. [33] 2016 | Australia | Quantitative Non-Randomized Study | Advanced Cancer | 43 | Computer | Ipad, CareSearch Website, FitBit®™ | Video Conferencing、Virtual Case Conferences、Self-Report Assessment Tools、Remote Activity Monitoring | B⑤; D①; E③④; F① |
| Guo et al. [19] 2017 | Canada | Mixed-Methods Study | Not Reported | 13 | Computer | IPAD/Lenovo ThinkPad laptop | Keeping in touch with someone、entertainment、Search for information、Remote Monitoring |
C②; D②; G② H |
| Wright et al. [8] 2018 | USA | Mixed-Methods Study | Advanced Cancer | 10 | Wearable Devices | Fitbit Zip, Fitbit Charge 2, Beiwe research platform | Remote Monitoring、Providing Customized Symptom Management | E⑤⑥; F②③; G②③; H |
| Niki et al. [26] 2019 | Japan | Quantitative Non-Randomized Study | Advanced Cancer | 20 | VR | Google Earth VR, HTC VIVE | Immersive Virtual Reality Travel | A③; B②; F④; G②③ |
| Ferguson et al. [18] 2020 | USA | Mixed-Methods Study | Advanced Dementia | 25 | VR | YouTube VR | Immersive 360° Ocean View Video | A④; G②③; H |
| Johnson et al. [20] 2020 | USA | Quantitative Non-Randomized Study | Not Reported | 12 | VR | Samsung Gear VR, Oculus Software |
Watching Animated Videos and Realistic Static Images via VR Applications(The nine applications were as follows: 360 Photos, Meditation, Apollo 11, Bait!, Feel: The Must of the Sea, Bear Island, theBlu, Coaster, and Hello Mars. ) |
B② |
| Kabir et al. [21] 2020 | Canada | Mixed-Methods Study | Not Reported | 27 | Computer |
TV/ touchscreen laptop |
Virtual Travel with Music Playback | B②; C③; E⑤⑦; F②③④⑤⑥; H |
| Pavic et al. [28] 2020 | Switzerland | Quantitative Non-Randomized Study | Advanced Cancer | 30 | Wearable Devices | Samsung Galaxy S5, bracelet Ecerion® | Remote Monitoring、Symptom Reporting | A⑤; B②; D③ |
| Schoppee et al. [30] 2020 | USA | Quantitative Non-Randomized Study | Advanced Cancer | 234 | Computer | computer tablet, PAINReportIt® | Symptom Assessment and Documentation | G① |
|
Brungardt et al. [17] 2021 |
USA | Mixed-Methods Study | Not Reported | 23 | VR | Facebook Oculus Go | Nature Scenery Videos with Music Therapy | F①⑦⑧; G②④; H |
| Lloyd et al. [22] 2021 | United Kingdom | Qualitative Study | Not Reported | 19 | VR | Room Scale VR | immersed in a simulated underwater environment | H |
| Moscato et al. [24] 2021 | Italy | Quantitative Non-Randomized Study | Advanced Cancer | 14 | VR | Mirage Solo VR, wearable wristband | Non-Interactive 360° Nature Scenery Videos (Ocean View, Parks, Waterfalls, London Bridge, Mountain Views) and Interactive Basic Skill Games(Yuma’s World) | A②; B②; C④; E③⑤⑧⑨ |
| Ngoma et al. [25] 2021 | Tanzania | RCT | Advanced Cancer | 98 | Computer | CommCare platform, mPalliative Care Link | Symptom and QoL reporting、Synoptic clinical record and PC plan generation、Follow-up clinical interactions、SMS、Educational module 、Emergency phone contact | B⑥; G⑤ |
| Nwosu et al. [27] 2021 | United Kingdom | Quantitative Non-Randomized Study | Not Reported | 15 | VR | Samsung Gear VR, Sony WH-CH500 | Choose any one of the following options:①A five-minute beach relaxation video;②A ten-minute meditation in a simulated forest environment③A five-minute roller coaster ride | F④; G③ |
| Perna et al. [29] 2021 | United Kingdom | RCT | Not Reported | 20 | VR | Google Daydream VR, Google Pixel XL | Immersive VR Video Experiences (e.g., Opera, Flying an Airplane) | B②; F③; G② |
| Austin et al. [15] 2022 | Australia | RCT | Advanced Cancer | 13 | VR | Oculus Rift® headset | Immersive 360° VR Non-Interactive Audio-Visual Experience (Enjoying an Alpine Meadow Environment) | A③; B②; F③④; G②⑥ |
| Balasubramanian et al. [16] 2022 | India | Quantitative Non-Randomized Study | Advanced Cancer | 120 | Computer | a camera integrated laptop and e-PC software application | Online Communication with Healthcare Providers | G⑦ |
| Guenther et al. [7] 2022 | Germany | Quantitative Non-Randomized Study | Not Reported | 45 | VR | Samsung Gear VR, PICO G2 4 K VR | Immersive 360° Videos (Three Categories: 1: Travel: Iceland and London, Relaxation: Various Beaches and Secluded Spots, Meditation and Animals: Dolphin Therapy, Seal Hospital, Wild West, Farm Sanctuary) | A③⑤; D④ |
| Seiler et al. [31] 2022 | Switzerland | Mixed-Methods Study | Not Reported | 6 | VR | Oculus Quest 2 Software, NatureTreks VR, You Tube VR, Occulus TV, Tripp VR | Immersive VR Experiences (Landscape Exploration, Mindfulness Meditation-Supportive Environments, etc.) | A⑥; B②; F④⑨; G②③; H |
| Mirshahi et al. [23] 2024 | USA | RCT | Advanced Heart Failure | 22 | Computer | Skyroom, WhatsApp® | weekly webinars、engage patients with case scenarios and empower them to make appropriate decisions when facing similar situations、learn from other patients | C④; D⑤⑥; F③⑨; G②③⑧ |
| Guo et al. [35] 2024 | China | Quantitative Non-Randomized Study | Advanced Cancer | 61 | VR | Intelligent Virtual Reality Mind-Body Interaction Training System | Immersive Nature Scenery Photos Combined with Audio Experience (Ocean, Forest, Beach, Valley, Prairie, Glacier, etc.) | A③; B② |
A is the pain level: ①McGill Pain Questionnaire (MPQ), ②Brief Pain Inventory (BPI), ③Numerical Rating Scale (NRS), ④Pain Assessment IN Advanced Dementia Scale (PAIN-AD), ⑤Visual Analog Scale (VAS), ⑥National Comprehensive Cancer Network (NCCN)
B is plagued by symptoms: ①Symptom Distress Scale (SDS), ②Edmonton Symptom Assessment Scale (ESAS), ③Functional Assessment of Cancer Therapy-General (FACT-G), ④Functional Assessment of Cancer Therapy–Fatigue (FACT-Fatigue), ⑤Symptom Assessment Scale (SAS), ⑥Palliative care Outcome Scale (POS)
C for psychological or mental health: ①Center for Epidemiologic Studies Depression Scale (CES-D), ②the UCLA loneliness Scale, ③Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being scale (FACIT-Sp-12), ④Hospital Anxiety and Depression Scale (HADS)
D for quality of life: ①Australia-modified Karnofsky Performance Status (AKPS), ②Self-administered questionnaires, ③Euro-pean Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30 (EORTC QLQ-C30), ④European Quality of Life Five Dimension Five Level Health Questionnaire(EQ-5D-5 L), ⑤Persian version of the Kansas City Cardiomyo-pathy Questionnaire (PKCCQ), ⑥Functional Assessment of Chronic Ill-ness Therapy–Palliative-14 questionnaire (FACIT PAL-14)
E is a physiological parameter: ①Serum Cytokine Levels, ②Natural Killer(NK) cell numbers, ③Activity index, ④Weight, ⑤Pulse rate, ⑥Number of steps, ⑦Cholesterol, ⑧Picoelectricity, ⑨Skin temperature
F for feasibility: ①Usage time, ②Patient enrollment rate, ③Patient intervention completion rate, ④Side effects, ⑤Burden of intervention, ⑥The Greater Cincinnati Chapter Well-Being Observation Tool©, ⑦Patient mortality rate, ⑧Patient discontinuation rate, ⑨Patient turnover
G for acceptability: ①Computer Acceptability Scale (CAS), ②Patient satisfaction, ③Willingness to use, ④System Usability Scale(SUS), ⑤Homemade Quality of Care Scale, ⑥iGroup Presence Questionnaire (IPQ), ⑦e-Palliative Patient Satisfaction Questionnaire, ⑧Compliance
H for semi-structured interviews
Table 2.
Summary of digital technology applications in palliative care
| Author & Year | Main Research Content and Results |
|---|---|
| Wilkie et al. [34] 2009 | Developed and evaluated an interactive pentablet software, “PAINReportIt-Plus,” designed to assist cancer patients in home hospice care to report pain and related symptoms. The findings demonstrated high acceptability of the tool (mean score 10.3/13), significantly enhancing symptom visibility and reducing symptom distress, thereby optimizing symptom management processes. |
| Gustafson et al. [6] 2013 | Studied and evaluated an online support system called CHESS (Comprehensive Health Enhancement Support System) designed to assist patients with non-small cell lung cancer (NSCLC) and their caregivers in managing symptoms and accessing social support. The findings demonstrated that CHESS significantly reduced patient symptom distress (e.g., Cohen’s d = 0.61 at 6 months) compared to the Internet and showed potential for enhancing caregiver satisfaction and patient survival. |
| Steel et al. [32] 2016 | Investigated and evaluated a web-based stepped collaborative care intervention designed to reduce depression, pain, and fatigue in patients with advanced cancer while improving quality of life. The findings demonstrated that, compared to enhanced usual care, the intervention significantly reduced depression (Cohen’s d = 0.71), pain (Cohen’s d = 0.62), and fatigue (Cohen’s d = 0.26) and markedly improved quality of life (Cohen’s d = 0.99) at six months. Additionally, the intervention lowered levels of inflammatory markers (e.g., IL-6 and IL-1b), increased natural killer (NK) cell numbers, and reduced caregiver stress and depression. |
| Tieman et al. [33] 2016 | Evaluated a telehealth-based intervention designed to support palliative care patients and their caregivers in the community. The findings indicated that the intervention demonstrated high feasibility, with patients and caregivers effectively managing the technology to report symptom data, significantly enhancing the responsiveness and overall quality of community-based care services. |
| Guo et al. [19] 2017 | Investigated and evaluated an internet-based communication and information technology intervention called “Keep in Touch (KIT)” to support in-patient palliative care patients and their family members. The findings indicated high feasibility of the intervention, significantly enhancing patients’ social connectedness, reducing loneliness, and improving overall well-being and quality of life. |
| Wright et al. [8] 2018 | Investigated and evaluated a mobile health intervention named “HOPE” (Helping Our Patients Excel), which incorporated wearable devices (Fitbit Zip and Fitbit Charge 2) to monitor physical activity and biometric data for improving symptom management in patients with advanced gynecologic cancers. The study demonstrated high feasibility and acceptability, with participants achieving an average daily step count of 3,973, indicating a significant increase in physical activity. Additionally, most participants reported that the wearable devices motivated their physical activity, enhanced communication with their care team, and improved their overall symptom management, ultimately contributing to better quality of life. |
| Niki et al. [26] 2019 | Investigated and evaluated a VR-based intervention aimed at alleviating symptom burden in terminal cancer patients through simulated travel experiences. The study demonstrated significant reductions in pain (Cohen’s d = 0.57 d = 0.57d = 0.57), fatigue (Cohen’s d = 0.68 d = 0.68d = 0.68), depression (Cohen’s d = 1.08 d = 1.08d = 1.08), and anxiety (Cohen’s d = 0.86 d = 0.86d = 0.86), along with improved overall well-being. The intervention was found to be safe with no severe side effects, highlighting its feasibility and potential in palliative care settings. |
| Ferguson et al. [18] 2020 | Investigated a VR-based intervention to provide therapeutic recreational experiences for hospice patients living with dementia (hPLWD). Participants wore a VR headset to view a beach scene, with 56% reporting enjoyment and 48% expressing willingness to use it again. Although 8% experienced worsened behavioral and psychological symptoms, VR was generally deemed safe and beneficial, with potential to enhance patients’ quality of life. |
| Johnson et al. [20] 2020 | Evaluated a VR-based intervention aimed at improving symptom management for palliative care patients. Twelve patients participated in a one-time, 30-minute VR session. The study found that most participants reported ease of use, with 83% recommending the intervention to others. Symptom assessments (ESAS-r) indicated trends of improvement in pain, fatigue, drowsiness, depression, and anxiety, with a significant reduction in anorexia. Overall, VR was deemed a promising modality for palliative care interventions. |
| Kabir et al. [21] 2020 | Investigated an audiovisual technology called “LIFEView,” designed to support well-being and quality of life in palliative and end-of-life care patients through virtual travel experiences. The study found high feasibility and acceptability, with participants showing slight but positive trends in improving psychological, physical, and spiritual symptoms. The intervention was widely appreciated for fostering reminiscence and meaning-making, with potential value in reducing psychological distress. |
| Pavic et al. [28] 2020 | Investigated a wearable device-based mobile health technology designed to monitor the health of discharged palliative care cancer patients and predict health deterioration. The study demonstrated high feasibility, with 76% of patients finding the method beneficial and willing to recommend it to others. Data analysis revealed that resting heart rate, heart rate variability, and step speed effectively predicted unplanned emergency visits and readmissions, highlighting the potential of wearable technology as a digital biomarker for health deterioration. |
| Schoppee et al. [30] 2020 | Investigated the Wi-Fi-enabled PAINReportIt® tablet tool for real-time pain reporting by cancer patients in hospice care. Results showed high acceptability among patients (mean score 12.2/14) and caregivers (mean score 8.5/9), with no significant differences by gender or race. While older adults and those with limited computer experience scored slightly lower, overall feasibility was high, suggesting the tool’s potential as an effective method for pain management and communication in hospice care. |
| Brungardt et al. [17] 2021 | Investigated and evaluated a combined VR and music therapy (MT) intervention aimed at managing emotions and symptoms in hospitalized palliative care patients. Patients experienced a personalized music playlist within a VR environment. The intervention showed high feasibility and acceptability, with 74% of patients completing it and 53% giving the highest satisfaction rating. Participants reported emotional benefits, such as calmness and comfort, alongside physical responses, including pain relief and relaxation. |
| Lloyd et al. [22] 2021 | Investigated a VR-based intervention aimed at improving the overall well-being of hospice patients through immersive experiences. Nineteen patients participated in a 30-minute VR session, and findings demonstrated high acceptability. Most participants enjoyed the intervention and reported significant relief in symptoms such as pain and anxiety, along with improved emotional and psychological well-being. The study highlighted VR’s potential to help patients temporarily escape the constraints of reality and reconnect with meaningful experiences, enhancing their sense of life’s value. |
| Moscato et al. [24] 2021 | Investigated and evaluated a VR-based intervention aimed at alleviating symptoms in cancer patients receiving home palliative care. The study revealed that while long-term outcomes (e.g., anxiety, depression, pain) showed no significant improvement, the VR intervention significantly reduced pain (− 37.73%), anxiety (− 46.36%), depression (− 30.05%), and shortness of breath (− 36.32%), and enhanced overall well-being (+ 26.36%) in the short term after use. No adverse side effects were reported, indicating high feasibility and acceptability of the intervention. |
| Ngoma et al. [25] 2021 | Evaluated a smartphone application called “mPalliative Care Link (mPCL)” designed to enhance remote palliative care through community health workers for patients with advanced cancer. The study found that while symptom severity was higher in the mPCL group, care satisfaction was comparable to the phone-contact group. The app facilitated automated symptom assessment and response, showing promise as a scalable palliative care intervention, particularly in resource-limited settings. |
| Nwosu et al. [27] 2021 | Investigated the feasibility and potential applications of a VR intervention in palliative care settings. Conducted in two UK specialist palliative care units, 15 participants (patients and caregivers) engaged in immersive therapy using the Samsung Gear VR system. Findings revealed that 93.3% of participants reported a positive experience and expressed willingness to use the intervention again, with no significant adverse effects observed. The study highlighted critical considerations for VR implementation, such as equipment selection, infection control, and session configuration, emphasizing the need for further research to integrate VR into palliative care practices. |
| Perna et al. [29] 2021 | Investigated the feasibility and effects of a personalized VR intervention for repeated use in palliative care patients. The study included 26 participants, 77% of whom completed all four 4-minute VR sessions. Results showed significant symptom score reductions in the intervention group after the first session (from 26.3 to 11.5), compared to a decrease from 37.9 to 25.5 in the control group. While personalized VR did not significantly outperform non-personalized VR (P = 0.60), repeated VR sessions demonstrated high feasibility and acceptability, with potential benefits for psychological well-being. |
| Austin et al. [15] 2022 | Investigated a VR intervention for managing cancer pain in palliative care. Thirteen participants underwent a crossover trial using 3D head-mounted (HMD VR) and 2D screen applications. Results demonstrated significant reductions in cancer pain intensity for both methods (3D HMD VR: −1.9, P = 0.00, 2D screen: −1.5, P = 0.007), though no significant differences were observed between the two. The study highlighted VR as a feasible and safe adjunctive approach for pain management. |
| Balasubramanian et al. [16] 2022 | Evaluated an e-Palliative Care (e-PC) homecare service model that utilizes virtual doctor consultations to enhance patient and caregiver satisfaction and care outcomes for advanced cancer patients. The study found high overall satisfaction (mean score 4.39/5), with notable benefits in reducing financial burdens and improving time convenience. e-PC was deemed a feasible and cost-effective solution for delivering high-quality palliative care in resource-limited settings. |
| Guenther et al. [7] 2022 | Evaluated a single VR experience for alleviating pain and improving symptom control in palliative care patients. The study included 40 participants and demonstrated significant pain reduction during and up to one hour after the VR session (from a baseline VAS of 2.25 to 0.7 during use, P < 0.0001). 85% of patients rated the experience as “very good” or “good,” and 82.5% expressed willingness to use it again. Despite minor side effects such as dry eyes and headaches, VR was found to be a highly acceptable and effective non-pharmacological intervention for pain relief in palliative care. |
| Seiler et al. [31] 2022 | Investigated a VR-based intervention to assess its feasibility and acceptability among palliative care patients. Six patients participated in a single 20 to 60-minute VR session, experiencing content such as nature landscapes and specific locations. The study revealed significant reductions in overall symptom burden (ESAS total score decreased by 8.4 points) and psychological distress (DT decreased by 0.6 points). Participants widely reported relaxation and psychological relief, with most expressing willingness to use VR again. Although a few patients faced discomfort with equipment use, the overall feasibility and acceptability were high, highlighting VR’s potential application in palliative care. |
| Mirshahi et al. [23]2024 | Investigated the feasibility and acceptability of an early telehealth-based palliative care intervention aimed at improving the quality of life in heart failure patients. Conducted in Iran, the study involved six weeks of nurse-led webinars and WhatsApp group activities. Results indicated high feasibility and acceptability, with 78% of participants willing to join again or recommend it to others. While trends for anxiety and depression improvement were not statistically significant, quality-of-life scores (PKCCQ and FACIT-PAL-14) improved significantly in the intervention group (PKCCQ: P < 0.001; FACIT-PAL-14:P = 0.001). The study highlights the potential of this approach in resource-limited settings. |
| Guo et al. [35] 2024 | Explored the application of VR technology in symptom management for patients with advanced cancer. Sixty-one patients participated in a 30-minute VR relaxation session, and results indicated significant improvements in symptoms such as pain, fatigue, nausea, anorexia, anxiety, and depression (P < 0.05). The intervention showed high patient acceptability, although 15% experienced mild dizziness, which resolved spontaneously. The study concluded that VR is a safe and effective adjunctive treatment with potential for broader implementation in palliative care for advanced cancer patients. |
Literature quality assessment
The quality appraisal of the 24 included studies was conducted based on their study design. Six RCTs [6, 15, 23, 25, 29, 32] were assessed using the Cochrane Risk of Bias Tool. The overall risk of bias showed that three studies [6, 15, 29] were rated as low risk, while three studies [23, 25, 32] were rated as moderate risk due to insufficient blinding, which may have introduced performance bias. Ten non-randomized quantitative studies [7, 16, 20, 26–28, 30, 33–35] were evaluated using the NOS. The overall quality showed that five studies [16, 26, 28, 33, 34] were rated as moderate quality due to robust participant selection and outcome measurement, although comparability was limited. Five studies [7, 20, 27, 30, 35] were rated as low quality due to insufficient sample size and inadequate outcome measurement. Seven mixed-methods studies [8, 17–19, 21, 24, 31]were appraised using the JBI checklist for mixed methods. The overall quality showed that two studies [8, 24] were rated as high quality due to comprehensive integration of quantitative and qualitative data. Five studies [17–19, 21, 31] were rated as moderate quality due to insufficient transparency in data integration and unclear methodological rigor. One qualitative study [22] was assessed using the CASP tool. It was rated as high quality, although it had limitations in data saturation.
Types and specific applications of digital technologies in palliative care
Ten studies [6, 16, 19, 21, 23, 25, 30, 32–34] applied computer-based technologies, such as websites, platforms, and apps, including PAINReportIt®, CHESS Coping with Lung Cancer website, FitBit®™, mPalliative Care Link, CommCare platform, e-PC software, and WhatsApp®, to palliative care. In palliative care, computer technologies enhance the quality of care and patient experience by improving data access and sharing efficiency, providing psychological support, entertainment, communication, and monitoring functions. Twelve studies [7, 15, 17, 18, 20, 22, 24, 26, 27, 29, 31, 35] applied virtual reality (VR) to palliative care, utilizing devices like Google Earth VR, YouTube VR, Samsung Gear VR, Facebook Oculus Go, Room Scale VR, Mirage Solo VR, Google Daydream VR, Oculus Rift® headset, PICO G2 4 K VR, and Tripp VR. Patients used head-mounted displays and stereoscopic glasses for a 360° immersive experience in a virtual world, with options to choose different themes based on personal needs, including relaxation (beach, music, meditation), travel experiences (Iceland and London), and animal therapy (dolphin therapy, western farm, nature reserve), as well as interactive games. Through non-invasive simulation technology, patients could interact with virtual objects in real-time, enhancing psychological support and overall quality of life by simulating a realistic environment. Two studies [8, 28] employed wearable devices in palliative care, including Fitbit Zip, Fitbit Charge 2, and bracelet Ecerion®. In palliative care, wearable devices provide continuous data streams by monitoring physiological parameters, such as heart rate, blood pressure, and activity levels, to optimize care decisions and personalized treatment plans. Their advantages include improved continuity and accuracy of monitoring, reduced hospital visits, enhanced patient self-management, and early warning mechanisms to prevent potential complications.
Content elements of digital technologies in palliative care
(1) Information Collection [6, 8, 19, 25, 26, 28, 30, 32–34]: Platforms or software are used to monitor patients’ health data, including self-monitoring of symptoms and signs, continuous tracking of pain, fatigue, anxiety, depression, and sleep, as well as remote monitoring of vital signs. (2) Information Provision [6, 23, 32]: Health education is provided through videos, courseware, and online tutorials, offering disease knowledge, care guidance, and relaxation techniques. (3) Decision Support [6, 8, 34]: Based on patient data, healthcare providers can remotely offer decision-support information, serving as a reference for patient decisions. (4) Communication Feedback [6, 16, 23, 25, 33]: Services include online text or video communication, patient messaging, and feedback. (5) Psychological Support [7, 15, 17, 18, 20–22, 24, 27, 29, 31, 32, 35]: Psychological relaxation is facilitated through immersive VR, video watching, and audio listening. Online cognitive behavioral therapy and psychological education websites are also used to provide psychological support. (6) Alerts and Warnings [8, 33]: The system analyzes patient-uploaded data, and when the data exceeds preset thresholds, it sends alerts to relevant healthcare professionals. It also assists patients in seeking help by sending distress signals to healthcare providers.
Outcome measures and effectiveness of digital technologies in palliative care
Outcome measures mainly include pain levels, symptom distress, psychological or mental health, quality of life, physiological parameters, feasibility indicators, and acceptability indicators. Pain levels were assessed using tools such as MPQ [34], BPI [24, 32], NRS [7, 15, 26, 35], PAIN-AD [18], VAS [7, 28], and NCCN [31]. Symptom distress was evaluated using SDS [34], ESAS [6, 15, 20, 21, 24, 26, 28, 29, 31, 35], FACT-G [32], FACT-Fatigue [32], SAS [33], and POS [25]. Psychological or mental health was assessed through CES-D [32], the UCLA Loneliness Scale [19], FACIT-Sp-12 [21], and HADS [23, 24]. Quality of life was measured using AKPS [33], self-made questionnaires [19], EORTC QLQ-C 30 [28], EQ-5D-5 L [7], PKCCQ [23], and FACIT PAL-14 [23]. Physiological parameters were evaluated by serum cytokine levels [32], Natural Killer (NK) cell numbers [32], activity index [24, 33], weight [33], heart rate [8, 21, 24], step count [8], blood pressure [21], electrodermal activity [24], and skin temperature [24]. Feasibility was assessed by usage time [17, 33, 34], patient enrollment rate [8, 21], intervention completion rate [8, 15, 21, 23], side effects [15, 21, 26, 27, 31], intervention burden [21], The Greater Cincinnati Chapter Well-Being Observation Tool© [21], patient mortality [17], discontinuation rate [17], and dropout rate [23, 31]. Acceptability was evaluated using CAS [30, 34], patient satisfaction [8, 15, 17–19, 23, 26, 29, 31], willingness to use [8, 18, 23, 26, 27, 31], SUS [17], self-made nursing quality scales [25], IPQ [15], e-Palliative Patient Satisfaction Questionnaire [16], and patient compliance [23]. Additionally, seven studies [8, 17–19, 21, 22, 31] conducted semi-structured interviews with patients to discuss their experiences.
Discussion
Digital technologies have promising applications in palliative care patients
The studies included in this review indicate that digital technologies have high feasibility and acceptability among palliative care patients, with only a small number of patients experiencing mild adverse effects, such as dizziness and dry eyes, during use [7]. Most patients provided positive feedback after using the technologies, with no serious adverse events reported and overall high intervention completion rates. However, based on the study periods and content, the application of digital technologies in palliative care remains in its early exploratory stage, with most research focusing on basic feasibility rather than in-depth clinical efficacy validation.
These studies primarily emphasize patient experiences and the practical utility of the technologies in real-world settings, but lack comprehensive evaluation of their long-term effects and clinical outcomes. For example, several studies [7, 18, 20–22, 26, 27, 31, 35] involved only a single exposure to the intervention. Additionally, limitations in study design, such as small sample sizes, lack of control groups, and insufficient follow-up periods, have impacted the accuracy and generalizability of the results, making it challenging to widely apply and thoroughly validate the findings.
Notably, 13 studies [6, 8, 15, 16, 24–26, 28, 30, 32–35] included in this review focused on patients with advanced cancer, while the other studies targeted patients with advanced dementia [18], advanced heart failure [23], or unspecified diseases [7, 17, 19–22, 27, 29, 31]. The complexity and diversity of the palliative care patient population pose significant challenges for research, as these patients often experience multiple symptoms and complications with rapidly changing conditions. This requires highly personalized and adaptable digital technologies. Current studies have not adequately addressed these complexities, limiting the ability to fully demonstrate the potential clinical benefits of these technologies. Future research should focus more on refining study design, validating long-term effects, and exploring personalized applications to fully assess and showcase the potential value of digital technologies in palliative care.
Limiting factors of digital technologies in palliative care
Although digital technologies hold substantial potential for advancing palliative care, their widespread adoption and sustained effectiveness face several significant barriers.
One key challenge is the complexity of hardware and software operation. Most studies [6–8, 15, 17–23, 25–27, 29, 31, 33–35] have been conducted in hospitals or palliative care institutions, where professional operators provide guidance and support. However, research has shown that home care is the preferred setting for many palliative care patients [36]. In this context, many elderly patients face difficulties in learning and adapting to new technologies due to limited digital literacy and reduced adaptability. For example, Kabir et al. [21] highlighted that introducing the LIFEView audiovisual technology in hospice care required professional teams to provide extensive training, with some patients needing repeated instructions to achieve basic usability. Thus, the ability of healthcare professionals to deliver effective training, coupled with the adaptability of patients, directly influences the practical implementation of these technologies. To fully realize their potential, it is crucial to address these challenges through patient-centered training programs, simplified user interfaces, and robust technical support systems.
Access to digital technologies in resource-limited settings remains a critical challenge. Recent data from the World Bank reveals that the internet penetration rate in low-income countries is only 28%, significantly lower than the global average of 63% [37]. Additionally, a report from the World Health Organization (WHO) highlights that many low-income countries lack reliable electricity supplies and basic network connectivity, which poses significant constraints on the use of telemedicine and VR technologies [38]. For instance, Ngoma et al. [25] found that the mobile palliative care solution “mPalliative Care Link” in Tanzania faced significant limitations due to unstable networks and equipment shortages, restricting its reach to only a limited number of patients. Addressing these issues requires the development of technologies tailored to low-resource settings, such as remote monitoring systems that operate on low bandwidth or offline-capable data collection devices.
Third, data security and privacy issues present critical challenges. According to a U.S. cybersecurity report [39], the healthcare sector accounted for 21% of all reported data breaches between 2019 and 2021, involving substantial amounts of patient health information. These breaches not only compromise patient privacy but also undermine trust in digital technologies among patients and healthcare providers. In palliative care, where privacy-sensitive information such as psychological states and medical histories is involved, these risks are heightened. To mitigate these concerns, robust encryption protocols, such as end-to-end encryption, must be implemented. Additionally, digital tools should comply with international privacy regulations, such as the General Data Protection Regulation (GDPR) [40], and local laws. Regular cybersecurity training should also be integrated into healthcare institutions’ digital management strategies to ensure robust protection.
Lastly, the insufficient personalization and adaptability of digital technologies requires more attention. For instance, Seiler et al. [31] observed that palliative care patients exhibited diverse preferences for VR experiences, with some preferring tranquil natural landscapes while others opted for dynamic, stimulating environments. Designing technologies with greater flexibility, such as using AI algorithms for personalized recommendations, could better accommodate the varied needs of patients.
Implications for future research and practice
Future research should focus on addressing the key barriers identified in this review to optimize the implementation and integration of digital technologies in palliative care. To overcome accessibility challenges in resource-limited settings, priority should be given to developing innovative infrastructure solutions, such as portable satellite-based internet systems and solar-powered devices, to mitigate connectivity and power limitations. Collaboration among governments, non-governmental organizations, and private stakeholders will be essential to subsidize equipment costs, ensuring affordability for healthcare providers and patients. Furthermore, pilot studies should be conducted to assess the feasibility and effectiveness of these tools in resource-constrained environments, providing evidence for wider adoption.
While digital technologies show considerable promise, their integration into palliative care remains challenging, particularly in regions lacking designated palliative care units. The complexity of both hardware and software presents an additional obstacle. To minimize these barriers, future efforts should focus on developing simplified user interfaces and user-friendly systems tailored to elderly patients, who often struggle with limited digital literacy. Remote training programs, virtual tutorials, and AI-guided assistance can further facilitate the adoption of technology in home settings. Establishing community-based support networks and remote technical assistance will also be crucial in ensuring ongoing guidance and troubleshooting.
Data privacy and security are key concerns, necessitating the establishment of internationally recognized standards, such as those aligned with the General Data Protection Regulation (GDPR). Advanced solutions, including end-to-end encryption and blockchain technology, should be integrated into digital platforms to protect sensitive patient information. Additionally, regular cybersecurity training within healthcare institutions is vital to minimize vulnerabilities and foster trust in digital solutions.
To address the economic challenges associated with digital tools, governments and international organizations should establish dedicated funding mechanisms and encourage cross-sector partnerships to share costs and optimize resource allocation. Moreover, collaboration between healthcare professionals, technology developers, and policymakers is essential to create scalable solutions that meet the diverse needs of palliative care settings. Finally, future technologies should aim to enhance personalization by leveraging artificial intelligence to dynamically adapt to patient preferences and clinical conditions. Flexible, customizable features should also be incorporated to accommodate diverse user needs.
By prioritizing these actionable directions, digital technologies can overcome existing barriers, improve patient outcomes, expand access to care, and ensure trust and security within palliative care systems.
Conclusion
This scoping review systematically examined the current state of digital technology applications in palliative care, their potential impacts, and the challenges associated with their implementation. The findings suggest that, although digital technologies are still in the early stages of exploration, tools such as computer systems, virtual reality (VR), and wearable devices show significant potential in improving patients’ quality of life, alleviating symptom burden, and providing psychological support. Unlike the traditional biomedical model, which primarily relies on institution-based, clinician-led care, digital technologies enable remote monitoring, real-time feedback, and personalized interventions. These innovations expand the reach of palliative care, enhancing its accessibility and overall quality.
Supplementary Information
Acknowledgements
This study has no acknowledgements.
Authors' contributions
Contributions to conception and writing: YHT, XL, WM. Drafting thearticle or revising it critically for important intellectual content: HMX, YW, YG.
Funding
This study did not receive specific funding from any funding agencies in the public, commercial, or non-profit sectors.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kvale PA, Simoff M, Prakash UB. Palliative care. Chest. 2003;123(1):S284–311. [DOI] [PubMed] [Google Scholar]
- 2.Sepúlveda C, Marlin A, Yoshida T, Ullrich A. Palliative care: the World Health Organization’s global perspective. J Pain Symptom Manag. 2002;24(2):91–6. [DOI] [PubMed] [Google Scholar]
- 3.Knaul FM, Farmer PE, Krakauer EL, De Lima L, Bhadelia A, Kwete XJ, Arreola-Ornelas H, Gómez-Dantés O, Rodriguez NM, Alleyne GA. Alleviating the access abyss in palliative care and pain relief—an imperative of universal health coverage: the Lancet Commission report. Lancet. 2018;391(10128):1391–454. [DOI] [PubMed] [Google Scholar]
- 4.Care H. Clinical practice guidelines for quality palliative care. Third National Consensus Project for Quality Palliative Care; 2013. [Google Scholar]
- 5.Sleeman KE, De Brito M, Etkind S, Nkhoma K, Guo P, Higginson IJ, Gomes B, Harding R. The escalating global burden of serious health-related suffering: projections to 2060 by world regions, age groups, and health conditions. Lancet Global Health. 2019;7(7):e883-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gustafson DH, DuBenske LL, Namkoong K, Hawkins R, Chih MY, Atwood AK, Johnson R, Bhattacharya A, Carmack CL, Traynor AM. An eHealth system supporting palliative care for patients with non–small cell lung cancer: a randomized trial. Cancer. 2013;119(9):1744–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guenther M, Görlich D, Bernhardt F, Pogatzki-Zahn E, Dasch B, Krueger J, Lenz P. Virtual reality reduces pain in palliative care–a feasibility trial. BMC Palliat Care. 2022;21(1):169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wright A, Raman N, Staples P, Schonholz S, Cronin A, Carlson K, Keating N, Onnela J. The HOPE pilot study: harnessing patient-reported outcomes and biometric data to enhance cancer care. JCO Clin Cancer Inf. 2018;2:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 10.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73. [DOI] [PubMed] [Google Scholar]
- 11.Moseley AM, Rahman P, Wells GA, Zadro JR, Sherrington C, Toupin-April K, Brosseau L. Agreement between the Cochrane risk of bias tool and Physiotherapy Evidence Database (PEDro) scale: a meta-epidemiological study of randomized controlled trials of physical therapy interventions. PLoS ONE. 2019;14(9): e0222770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5. [DOI] [PubMed] [Google Scholar]
- 13.Munn Z, Aromataris E, Tufanaru C, Stern C, Porritt K, Farrow J, Lockwood C, Stephenson M, Moola S, Lizarondo L, et al. The development of software to support multiple systematic review types: the Joanna Briggs Institute System for the Unified Management, Assessment and Review of Information (JBI SUMARI). Int J Evid Based Healthc. 2019;17(1):36–43. [DOI] [PubMed] [Google Scholar]
- 14.Long HA, French DP, Brooks JM. Optimising the value of the critical appraisal skills programme (CASP) tool for quality appraisal in qualitative evidence synthesis. Res Methods Med Health Sci. 2020;1(1):31–42. [Google Scholar]
- 15.Austin PD, Siddall PJ, Lovell MR. Feasibility and acceptability of virtual reality for cancer pain in people receiving palliative care: a randomised cross-over study. Supportive care cancer: official J Multinational Association Supportive Care Cancer. 2022;30(5):3995–4005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Balasubramanian S, Biji MS, Ranjith MK, Abhina SS. Patient satisfaction in home care services through e-palliative care -an experience of tertiary cancer centre from Kerala. Indian J Palliat Care. 2022;28(3):250–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brungardt A, Wibben A, Tompkins AF, Shanbhag P, Coats H, LaGasse AB, Boeldt D, Youngwerth J, Kutner JS, Lum HD. Virtual reality-based music therapy in palliative care: a pilot implementation trial. J Palliat Med. 2021;24(5):736–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferguson C, Shade MY, Blaskewicz Boron J, Lyden E, Manley NA. Virtual reality for therapeutic recreation in dementia hospice care: a feasibility study. Am J Hospice Palliat Medicine®. 2020;37(10):809–15. [DOI] [PubMed] [Google Scholar]
- 19.Guo Q, Cann B, McClement S, Thompson G, Chochinov HM. Keep in Touch (KIT): feasibility of using internet-based communication and information technology in palliative care. BMC Palliat care. 2017;16:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnson T, Bauler L, Vos D, Hifko A, Garg P, Ahmed M, Raphelson M. Virtual reality use for symptom management in palliative care: a pilot study to assess user perceptions. J Palliat Med. 2020;23(9):1233–8. [DOI] [PubMed] [Google Scholar]
- 21.Kabir M, Rice JL, Bush SH, Lawlor PG, Webber C, Grassau PA, Ghaedi B, Dhuper M, Hackbusch R. A mixed-methods pilot study of ‘LIFEView’audiovisual technology: virtual travel to support well-being and quality of life in palliative and end-of-life care patients. Palliat Med. 2020;34(7):954–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lloyd A, Haraldsdottir E. Virtual reality in hospice: improved patient well-being. BMJ supportive Palliat care. 2021;11(3):344–50. [DOI] [PubMed] [Google Scholar]
- 23.Mirshahi A, Bakitas M, Khoshavi M, Khanipour-Kencha A, Riahi SM, Wells R, Odom JN, Ghiyasvandian S, Zakerimoghadam M. The impact of an integrated early palliative care telehealth intervention on the quality of life of heart failure patients: a randomized controlled feasibility study. BMC Palliat Care. 2024;23(1):22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moscato S, Sichi V, Giannelli A, Palumbo P, Ostan R, Varani S, Pannuti R, Chiari L. Virtual Reality in Home Palliative Care: Brief Report on the Effect on Cancer-Related Symptomatology. Front Psychol. 2021;12:709154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ngoma M, Mushi B, Morse RS, Ngoma T, Mahuna H, Lambden K, Quinn E, Sagan SB, Ho YX, Lucas FL, et al. mPalliative care link: examination of a mobile solution to palliative care coordination among Tanzanian patients with cancer. JCO global Oncol. 2021;7:1306–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Niki K, Okamoto Y, Maeda I, Mori I, Ishii R, Matsuda Y, Takagi T, Uejima E. A novel palliative care approach using virtual reality for improving various symptoms of terminal cancer patients: a preliminary prospective, multicenter study. J Palliat Med. 2019;22(6):702–7. [DOI] [PubMed] [Google Scholar]
- 27.Nwosu AC, Mills M, Roughneen S, Stanley S, Chapman L, Mason SR. Virtual reality in specialist palliative care: a feasibility study to enable clinical practice adoption. BMJ supportive Palliat care. 2021;14(1):47–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pavic M, Klaas V, Theile G, Kraft J, Tröster G, Blum D, Guckenberger M. Mobile health technologies for continuous monitoring of cancer patients in palliative care aiming to predict health status deterioration: a feasibility study. J Palliat Med. 2020;23(5):678–85. [DOI] [PubMed] [Google Scholar]
- 29.Perna MML, Lund S, White N, Minton O. The Potential of Personalized Virtual Reality in Palliative Care: A Feasibility Trial. Am J Hosp palliat Care. 2021;38(12):1488–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schoppee TM, Dyal BW, Scarton L, Ezenwa MO, Singh P, Yao Y, Suarez ML, Wang ZJ, Molokie RE, Wilkie DJ. Patients and caregivers rate the PAINReportIt wireless internet-enabled tablet as a method for reporting pain during end-of-life cancer care. Cancer Nurs. 2020;43(5):419–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seiler A, Schettle M, Amann M, Gaertner S, Wicki S, Christ SM, Theile G, Feuz M, Hertler C, Blum D. Virtual reality therapy in palliative care: A case series. J Palliat Care. 2022. Epub ahead of print. 10.1177/08258597221086767. [DOI] [PubMed]
- 32.Steel JL, Geller DA, Kim KH, Butterfield LH, Spring M, Grady J, Sun W, Marsh W, Antoni M, Dew MA. W eb-based collaborative care intervention to manage cancer‐related symptoms in the palliative care setting. Cancer. 2016;122(8):1270–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tieman JJ, Swetenham K, Morgan DD, To TH, Currow DC. Using telehealth to support end of life care in the community: a feasibility study. BMC Palliat care. 2016;15:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilkie DJ, Kim YO, Suarez ML, Dauw CM, Stapleton SJ, Gorman G, Storfjell J, Zhao Z. Extending computer technology to hospice research: interactive pentablet measurement of symptoms by hospice cancer patients in their homes. J Palliat Med. 2009;12(7):599–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guo YY, Yu XY, Xie SP. Application of virtual reality in palliative care for terminal cancer patients. J Nurs. 2024;31(11):58–62. [Google Scholar]
- 36.Lundereng ED, Nes AAG, Holmen H, Winger A, Thygesen H, Jøranson N, Borge CR, Dajani O, Mariussen KL, Steindal SA. Health care professionals’ experiences and perspectives on using telehealth for home-based palliative care: scoping review. J Med Internet Res. 2023;25: e43429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World B. Individuals using the internet (% of population) – low-income countries 2021. Available from: https://data.worldbank.org/indicator/IT.NET.USER.ZS.
- 38.World Health O: Global report on digital health. 2023. Available from: https://www.who.int.
- 39.Journal H. Healthcare data breach statistics 2022. https://www.hipaajournal.com.
- 40.European P, Council of the European U. General data protection regulation (GDPR) 2016. Available from: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A32016R0679.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.