Abstract
Multiple open and endoscopic techniques have been described for recalcitrant cases of plantar fasciitis. Compared with open techniques, endoscopic plantar fasciotomy has been shown to be safe and effective with decreased postoperative pain and quicker recovery, as well as decreased risk of soft tissue and neurovascular injury, while retaining the ability to provide direct visualization of the plantar fascia to facilitate proper release. Single-portal endoscopic techniques may offer additional advantages including less portal site and postoperative pain, earlier return to activities, and cost-effectiveness and higher patient satisfaction when performed in the office setting. This Technical Note describes the authors’ technique for nanoscopic plantar fasciotomy using a single-portal needle arthroscopy system, as well as advantages and limitations of this technique.
Technique Video
Plantar fasciitis (plantar fasciopathy) remains a common cause of heel pain in adults. Approximately 1 million patients each year undergo treatment of plantar fasciitis in the United States, making up approximately 1% of all patient visits to orthopaedic surgeons.1 Diagnosis of plantar fasciitis is made clinically, with patients reporting insidious onset of heel pain with ambulation after periods of rest. On physical examination, patients will have tenderness along the plantar fascia and reproduction of pain with stretching of the plantar aponeurosis.2 Treatment of plantar fasciitis begins with at least 6 months of conservative management, with strategies including nonsteroidal anti-inflammatory drugs, physical therapy and stretching, orthoses, night splints, casting, corticosteroid injections, and extracorporeal shock wave therapy.2,3 Despite high overall success rates with conservative management, recalcitrant cases of plantar fasciitis may be treated operatively. Surgery typically consists of partial or complete plantar fasciotomy, with both open and endoscopic techniques described. Other recently described surgical options include plantar fascia debridement, percutaneous partial plantar fasciotomy, and bipolar radiofrequency microtenotomy.4, 5, 6
Advantages of open plantar fascia release, with or without limited incision (“mini-open”), include the ability to perform concomitant nerve decompression and resection of any heel spurs. However, open surgery can be associated with longer postoperative recovery and the risk of secondary heel pain caused by plantar incision scar.7 Endoscopic plantar fasciotomy, first described in 1991 by Barrett et al.8 offered the ability for patients to return to immediate weightbearing, with studies demonstrating overall shorter recovery time, and possibly lower complication rates and similar long-term outcomes as open fasciotomy.9, 10, 11, 12, 13 Traditional 2-portal endoscopic techniques use a medial and lateral portal, although use of 2 medial portals has also been described.7,14 Despite minimally invasive technique, portal-site pain can still occur after endoscopic release, with 2 studies reporting a 15% and 16% incidence of portal-related pain within their cohorts, respectively.12,15
Endoscopic fasciotomy with a single-portal technique, subsequently described in 1997 by Jeran et al., offers direct visualization and portal placement adjacent to the medial aspect of the plantar fascia while avoiding sharp instrumentation on the lateral aspect of the foot, thereby preventing injury to neurovascular structures and iatrogenic pain of the lateral column.16, 17, 18 Single-portal endoscopic plantar fasciotomy may also confer advantages of less portal site pain, less postoperative pain, and earlier return to activities, which has been the anecdotal experience of the senior authors. Single-portal fasciotomy may also be performed in the office setting for select patients, which may further contribute to improved cost-effectiveness and patient satisfaction.19 However, larger scale studies would be needed to compare outcomes after 2-portal versus single portal endoscopic fasciotomy.
The purpose of this technique article is to describe a technique for single-portal endoscopic plantar fascia release using needle arthroscopy for the treatment of recalcitrant plantar fasciitis. Specifically, the authors describe their preferred technique using the Arthrex NanoScopic Resection System (Naples, Florida), which consists of a 1.9-mm-diameter arthroscope and 2.0-mm sheath, with an optic chip at the camera tip to provide high-definition imaging.20
Surgical Technique
Positioning, Local Anesthesia, and Room Setup
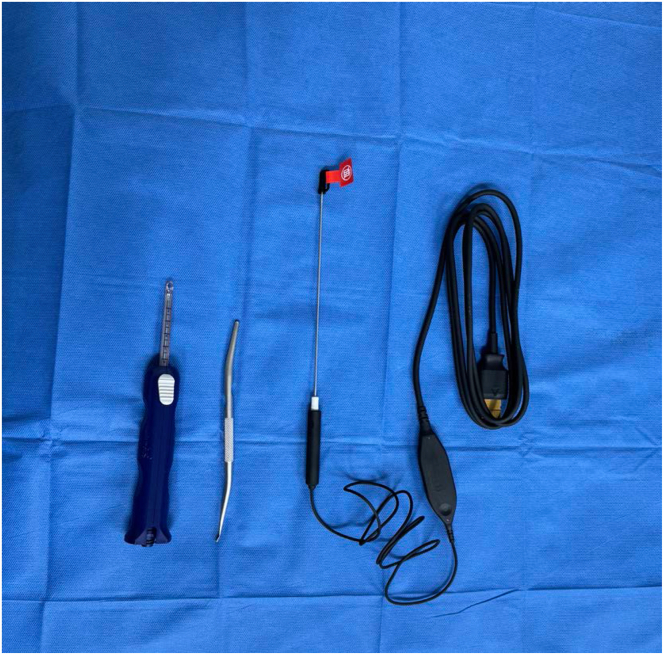
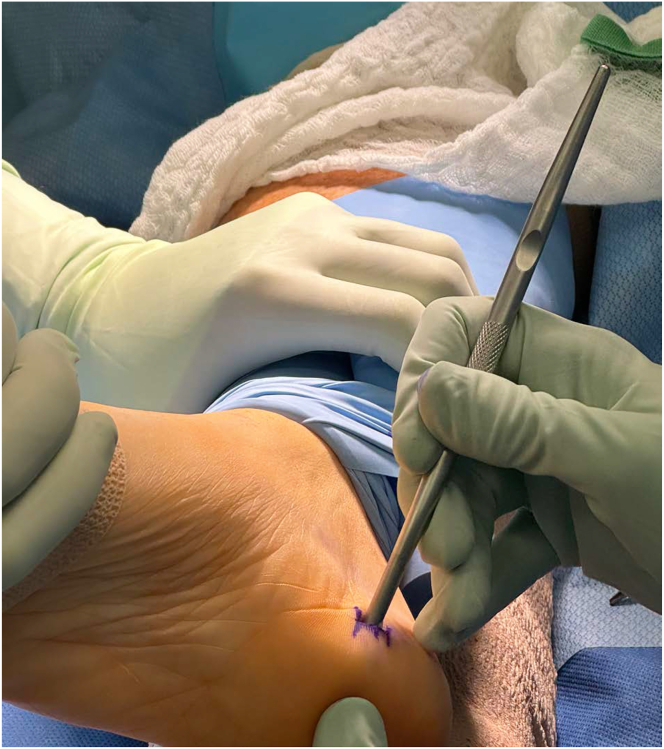
Instrumentation setup for the nanoscopic plantar fascia release consists of the needle scope, dilator, and a periosteal elevator (Fig 1). The patient is placed supine on the operating room table. A soft towel bump is placed under the leg to elevate the heel (Fig 2). Local anesthetic (with 1% lidocaine and 0.25% Marcaine) can be used for pain control but may not be necessary depending on other methods of anesthesia used. An ankle or thigh tourniquet may be placed for hemostasis but is not required.
Fig 1.
Instrumentation for nanoscopic plantar fascia release right side of patient. From left to right: NanoScopic release device with adapter (on back end) for NanoNeedle Scope, double-ended synovial scraper and dilator, NanoNeedle Scope (180 mm). Notably, this system does not require a light cable or scope coupler.
Fig 2.
The patient should be positioned supine with a soft bump under the leg to elevate the heel. An ankle or thigh tourniquet may be used but is not required. Patient right leg with elevator marking landmark of plantar fascia insertion.
Portal Placement
A 5-mm incision is made directly over the medial aspect of the plantar fascia insertion, just distal to the medial calcaneal tubercle and proximal to the border of the glabrous tissue (Fig 3, Video 1). Careful dissection down to the plantar fascia insertion is performed using a hemostat, taking care to avoid dissection dorsal to the fascia to prevent iatrogenic injury to Baxter’s (first branch of the lateral plantar) nerve. The dilator is then introduced and gently advanced plantar to the medial aspect of the fascial band to create a portal and potential space for the 1.9-mm endoscope and endoscopic plantar fascia resection system. A synovial scraper is then used to clear off residual soft tissue over the area of the plantar fascia insertion (Fig 4).
Fig 3.
A 5-mm incision is made over the medial aspect of the plantar fascia insertion at the junction of glabrous skin (g) and normal skin (n). The medial aspect of the calcaneal tubercle (mCT) can also be palpated, with the incision placed just distal to this bony landmark. Image depicting right foot incision site.
Fig 4.
After blunt dissection of the fascia insertion using a hemostat, the dilator end of the double-sided tool is introduced to create a portal space just plantar to the fascial band. Once the portal space is created, a synovial scraper, as shown here (similarly, a freer or periosteal elevator can be used) is used to clear off any residual tissue over the plantar aspect of the fascia. Image demonstrating right foot.
Operative Technique
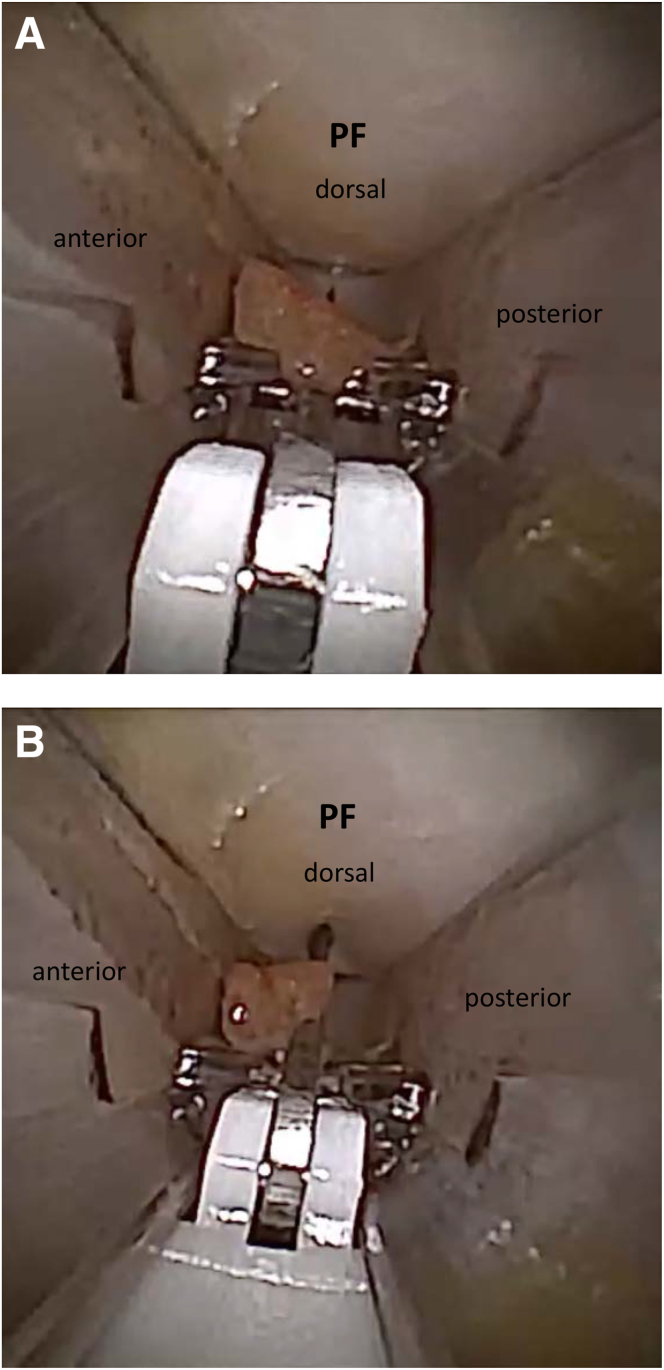
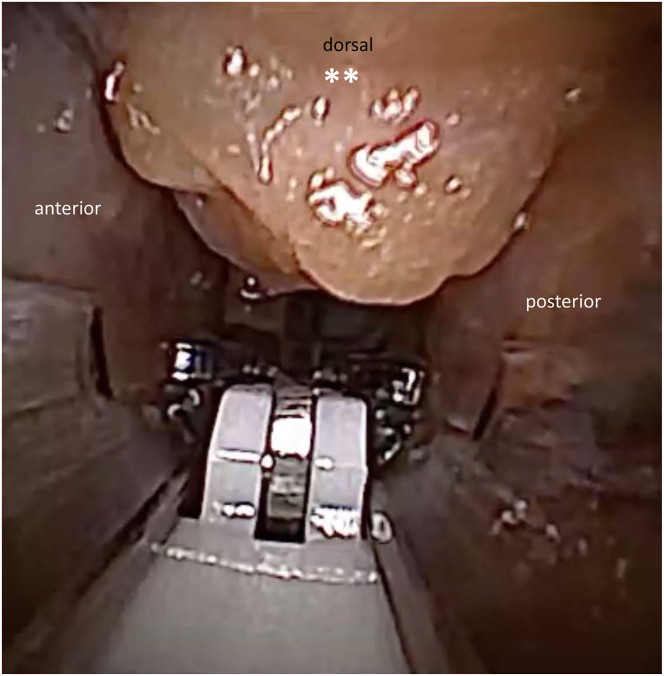
The NanoNeedle scope is then introduced into the release device (Fig 5). The plantar fascia can be viewed using the nanoscope. The foot should be held in a dorsiflexed position to tension the plantar fascia and surrounding tissues (Fig 6). Once the plantar fascia is visualized, the scope is advanced to the lateral-most extent of the fascia, and the endoscopic cutting blade is released with the tip of the blade directed upward. The blade is then directed from lateral to medial while applying upward pressure for a complete release of the fascia (Fig 7 A and B). The release is complete when fat and underlying intrinsic musculature is visualized across the width of the release (Fig 8). The wound is then irrigated, and the skin is closed with nylon sutures (Fig 9). A bulky sterile soft dressing and a postoperative shoe is applied. The patient is made protected weightbearing on the operative leg for 2 to 3 days and then progresses to weightbearing as tolerated once sutures are removed. Patients are permitted to return to sports within 2 weeks, using a cushioned arch support. Table 1 contains a brief summary of these steps for performing nanoscopic fasciotomy.
Fig 5.
The needle scope is then introduced into the release device. Image demonstrating right foot.
Fig 6.
With the foot manually dorsiflexed to tension the fascia, the needle scope is used to visualize and localize the medial and lateral extents of the overlying plantar fascia. Image demonstrating right foot.
Fig 7.
The endoscopic cutting blade with the overlying plantar fascia (PF) is demonstrated here as visualized from the medial portal. While applying steady upward pressure, the blade is directed from lateral (far side of medial incision, as shown) to medial for a complete fasciotomy. (A) and (B) show the direction of release.
Fig 8.
Fat and underlying intrinsic musculature (∗∗) are seen protruding from the dorsal extent of the portal tract, indicating complete release of the plantar fascia.
Fig 9.
After irrigating the wound, the skin is closed with 1-2 nylon sutures. A bulky, soft dressing and postoperative shoe are applied. Image demonstrating right foot.
Table 1.
Step-by-Step Guide to Performing Nanoscopic Plantar Fasciectomy
| Step 1: Inject local anesthetic (if desired) over incision site, directly over medial aspect of plantar fascia insertion and proximal to border of glaborous tissue. |
| Step 2: Make 5-mm incision. Insert hemostat to dissect down to plantar fascia insertion. |
| Step 3: Introduce dilator to create portal space. Remove dilator and use synovial scraper to clear off any residual soft tissue on the underside of the insertion. |
| Step 4: With the needle scope advanced into the endoscopic plantar fascia resection system, insert device to visualize plantar fascia across insertion site. |
| Step 5: With the foot dorsiflexed, use the endoscopic blade to release the fascial band, starting at the lateral aspect and traveling medially. Ensure complete release and visualization of intrinsic musculature across insertion site. |
| Step 6: Irrigate the wound, close incision, and apply soft dressings as indicated. |
Discussion
Minimally invasive surgery has gained significant attention in foot and ankle surgery in recent years, with percutaneous and arthroscopic techniques described for a multitude of foot and ankle pathologies.21 Although the goals of minimally invasive techniques in foot and ankle surgery include to lower complication rates, improved scar cosmesis, and quicker postoperative recovery, it is also important that the technique ensure adequate correction and/or release of the pathology involved. Over the past 30 years, plantar fasciotomy, traditionally performed as an open procedure, has also evolved with a multitude of endoscopic and percutaneous techniques described.7,8,14,18,22,23 Advantages of endoscopic plantar fasciotomy have included decreased postoperative pain with quicker recovery and decreased risk of soft tissue and neurovascular injury, all while retaining the ability to provide direct visualization of the plantar fascia to facilitate proper release.12,13,22
In this technique paper, we describe a minimally invasive approach to plantar fasciotomy using the NanoScopic Release System (Arthrex, Naples, Florida).20 This simple, single-portal technique, using a 1.9-mm endoscope, has been effective at allowing both senior authors the ability to perform plantar fasciotomy with minimal surgical risk and almost no downtime for patients. Prior work describing minimally invasive plantar fasciotomy with either single or dual portals have used incisions of up to 1 cm, with use of various size endoscopes ranging from 2.5 to 4.0 mm.14,16 The benefit of the nanoscopic plantar fasciotomy, as described in this technique report, lies in its smaller diameter system, as with other potential benefits reported with needle arthroscopy overall. These benefits include reduced risk of iatrogenic nerve and skin injury (along with theoretically reduced risk for bacterial entry and infection), and the option to perform needle arthroscopy procedures in the office setting as has been described in various anatomic areas.24, 25, 26, 27, 28, 29 A summary of the advantages and limitations, as well as pearls and pitfalls, of nanoscopic fasciotomy are provided in Tables 2 and 3.
Table 2.
Advantages and Limitations
| Advantages |
|
| Limitations |
|
Table 3.
Pearls and Pitfalls
| Pearls |
|
| Pitfalls |
|
In-office needle arthroscopy (IONA) for the treatment of recalcitrant PF has all the potential advantages of other IONA techniques previously described. Faster return to work, less time lost to injury with accelerated return to sport protocols, fewer complications, and the ability for the patient to see and understand the pathology, thereby helping with post-procedure rehabilitation, have all been described for other pathologies treated with IONA. The most obvious benefit is lack of any potential anesthetic complication as well as reduced cost when the procedure is performed in office or in a treatment room.
In conclusion, nanoscopic plantar fasciotomy is a safe and reproducible treatment option that may confer advantages inherent to traditional endoscopic fasciotomy as well as additional benefits of a single-portal needle arthroscopy system, with smaller incisions than required with traditional open and endoscopic techniques.
Disclosures
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: J.G.K. is a consultant for In2Bones; receives research support from Arthrex; is a paid consultant for Arthrex and CONMED Linvatec; is a board or committee member of American Orthopaedic Foot and Ankle Society, Arthroscopy Association of North America, European Society for Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA), Ankle and Foot Associates (AFAS), and International Society for Cartilage Repair of the Ankle; receives research support from Isto Biologics; and receives financial support from the Ohnell Family Foundation, Mr. Winston Fisher, and Ms. Tatiana Rybak. A.L.G. is a consultant for Arthrex. All other authors (E.C., J.J.B.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supplementary Data
Operative technique demonstrating the authors’ technique for nanoscopic plantar fasciotomy using a single-portal needle arthroscopy system, as well as advantages and limitations of this technique applied to right side of patient.
References
- 1.Riddle D.L., Schappert S.M. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: A national study of medical doctors. Foot Ankle Int. 2004;25:303–310. doi: 10.1177/107110070402500505. [DOI] [PubMed] [Google Scholar]
- 2.Neufeld S.K., Cerrato R. Plantar fasciitis: Evaluation and treatment. J Am Acad Orthop Surg. 2008;16:338. doi: 10.5435/00124635-200806000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Crawford F., Thomson C. Interventions for treating plantar heel pain. Cochrane Database Syst Rev. 2003;(3):CD000416. doi: 10.1002/14651858.CD000416. [DOI] [PubMed] [Google Scholar]
- 4.Cottom J.M., Wolf J.R., Sisovsky C.A. Midterm outcomes of endoscopic plantar fascia debridement in 125 patients: A 5-year follow-up. J Foot Ankle Surg. 2023;62:444–447. doi: 10.1053/j.jfas.2022.11.001. [DOI] [PubMed] [Google Scholar]
- 5.Cottom J.M., Maker J.M., Richardson P., Baker J.S. Endoscopic debridement for treatment of chronic plantar fasciitis: An innovative technique and prospective study of 46 consecutive patients. J Foot Ankle Surg. 2016;55:748–752. doi: 10.1053/j.jfas.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 6.Sorensen M.D., Hyer C.F., Philbin T.M. Percutaneous bipolar radiofrequency microdebridement for recalcitrant proximal plantar fasciosis. J Foot Ankle Surg. 2011;50:165–170. doi: 10.1053/j.jfas.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Feng S.M., Song R.L., Wang A.G., Sun Q.Q., Zhang S.C. Endoscopic partial plantar fasciotomy via 2 medial portals vs mini-open procedure for refractory plantar fasciitis. Foot Ankle Int. 2021;42:458–463. doi: 10.1177/1071100720964805. [DOI] [PubMed] [Google Scholar]
- 8.Barrett S.L., Day S.V. Endoscopic plantar fasciotomy for chronic plantar fasciitis/heel spur syndrome: Surgical technique—Early clinical results. J Foot Surg. 1991;30:568–570. [PubMed] [Google Scholar]
- 9.Bader L., Park K., Gu Y., O’Malley M.J. Functional outcome of endoscopic plantar fasciotomy. Foot Ankle Int. 2012;33:37–43. doi: 10.3113/FAI.2012.0037. [DOI] [PubMed] [Google Scholar]
- 10.Mao D.W., Chandrakumara D., Zheng Q., Kam C., Kon Kam King C. Endoscopic plantar fasciotomy for plantar fasciitis: A systematic review and network meta-analysis of the English literature. Foot (Edinb) 2019;41:63–73. doi: 10.1016/j.foot.2019.08.001. [DOI] [PubMed] [Google Scholar]
- 11.Ward L., Mercer N.P., Azam M.T., et al. Outcomes of endoscopic treatment for plantar fasciitis: A systematic review. Foot Ankle Spec. 2022 doi: 10.1177/19386400221129167. Published online November 27, 2022. [DOI] [PubMed] [Google Scholar]
- 12.Kinley S., Frascone S., Calderone D., Wertheimer S.J., Squire M.A., Wiseman F.A. Endoscopic plantar fasciotomy versus traditional heel spur surgery: A prospective study. J Foot Ankle Surg. 1993;32:595–603. [PubMed] [Google Scholar]
- 13.Fallat L.M., Cox J.T., Chahal R., Morrison P., Kish J. A retrospective comparison of percutaneous plantar fasciotomy and open plantar fasciotomy with heel spur resection. J Foot Ankle Surg. 2013;52:288–290. doi: 10.1053/j.jfas.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 14.Al-Ashhab M.E., HEDA Elbegawy, Hasan H.A.A. Endoscopic plantar fasciotomy through two medial portals for the treatment of recalcitrant plantar fasciopathy. J Foot Ankle Surg. 2018;57:264–268. doi: 10.1053/j.jfas.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 15.O’Malley M.J., Page A., Cook R. Endoscopic plantar fasciotomy for chronic heel pain. Foot Ankle Int. 2000;21:505–510. doi: 10.1177/107110070002100610. [DOI] [PubMed] [Google Scholar]
- 16.Saxena A. Uniportal endoscopic plantar fasciotomy: a prospective study on athletic patients. Foot Ankle Int. 2004;25:882–889. doi: 10.1177/107110070402501207. [DOI] [PubMed] [Google Scholar]
- 17.Hofmeister E.P., Elliott M.J., Juliano P.J. Endoscopic plantar fascia release: an anatomical study. Foot Ankle Int. 1995;16:719–723. doi: 10.1177/107110079501601109. [DOI] [PubMed] [Google Scholar]
- 18.Jeran D., McElgun T., Mirza M.A., King E.T. Single-portal endoscopic plantar fascial release: Operative technique, with preliminary results. Lower Extremity. 1997;4:103–108. [Google Scholar]
- 19.Kanakamedala A., Chen J.S., Kaplan D.J., et al. In-office needle tendoscopy of the peroneal tendons. Arthrosc Tech. 2022;11:e365–e371. doi: 10.1016/j.eats.2021.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arthroscopy Nano. Arthrex. https://www.arthrex.com/imaging-resection/nano-arthroscopy
- 21.Lui T.H. Arthroscopy and endoscopy of the foot and ankle: Indications for new techniques. Arthroscopy. 2007;23:889–902. doi: 10.1016/j.arthro.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 22.Campillo-Recio D., Ibañez M., Jimeno-Torres E., et al. Two-portal endoscopic plantar fascia release: Step-by-step surgical technique. Arthrosc Tech. 2020;10:e15–e20. doi: 10.1016/j.eats.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oliva F., Piccirilli E., Tarantino U., Maffulli N. Percutaneous release of the plantar fascia. New surgical procedure. Muscles Ligaments Tendons J. 2017;7:338–340. doi: 10.11138/mltj/2017.7.2.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Colasanti C.A., Mercer N.P., Garcia J.V., Kerkhoffs G.M.M.J., Kennedy J.G. In-office needle arthroscopy for the treatment of anterior ankle impingement yields high patient satisfaction with high rates of return to work and sport. Arthroscopy. 2022;38:1302–1311. doi: 10.1016/j.arthro.2021.09.016. [DOI] [PubMed] [Google Scholar]
- 25.Colasanti C.A., Azam M.T., Bi A.S., et al. Reproducible and effective biceps tenodesis method utilizing in-office nano-arthroscopy. Arthrosc Tech. 2023;12:e1797–e1802. doi: 10.1016/j.eats.2023.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burt J., Smith V., Gee C.W., Clarke J.V., Hall A.J. The role of outpatient needle arthroscopy in the diagnosis and management of musculoskeletal complaints: A systematic review of the Arthrex NanoScope. Knee. 2023;42:246–257. doi: 10.1016/j.knee.2023.04.003. [DOI] [PubMed] [Google Scholar]
- 27.Butler J.J., Randall G.W., Schoof L., et al. Excellent clinical outcomes and rapid return to activity following in-office needle tendoscopy for chronic Achilles tendinopathy. Arthrosc Sports Med Rehabil. 2024 doi: 10.1016/j.asmr.2024.100937. Published online April 8, 2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stornebrink T., Walinga A.B., Stufkens S.A.S., Kerkhoffs G.M.M.J. Wide-awake needle arthroscopy of the anterior ankle: A standardized approach. Arthrosc Tech. 2024;13 doi: 10.1016/j.eats.2023.102901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gianakos A.L., Kennedy J.G. In-office needle arthroscopy: Indications, surgical techniques, tips, and tricks. J Am Acad Orthop Surg Glob Res Rev. 2024;8:e23–e00124. doi: 10.5435/JAAOSGlobal-D-23-00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Operative technique demonstrating the authors’ technique for nanoscopic plantar fasciotomy using a single-portal needle arthroscopy system, as well as advantages and limitations of this technique applied to right side of patient.