Abstract
Chronic Osgood-Schlatter disease can cause significant knee pain and can result in severe functional deficits. For large, painful Osgood-Schlatter disease ossicles refractory to conservative management, surgical ossicle excision can provide resolution of symptoms. After diagnostic arthroscopy and intra-articular debridement, our preferred excision technique uses an open incision for direct visualization and removal of intratendinous ossicles, followed by distal patellar tendon repair and subsequent fixation with FiberTape sutures and knotless anchors to the tibial tubercle.
Technique Video
Osgood-Schlatter disease (OSD) is a common cause of anterior knee pain in skeletally immature adolescent athletes. Also known as traction apophysitis, osteochondrosis, or tibial tubercle apophysitis, OSD presents with the insidious onset of atraumatic functional knee pain and swelling, localizing to the tibial tubercle in the skeletally immature athlete.1 Symptoms are exacerbated with kneeling, running, jumping, and squatting and often resolve with rest. On examination, tenderness is present at the patellar tendon insertion on the tibial tubercle, and a large bony prominence may be noted as well.2
OSD occurs secondary to repetitive extensor mechanism forces applied at the patellar tendon insertion into a relatively soft apophysis of the tibial tubercle,3,4 resulting in chronic avulsion of that secondary ossification center.5 The etiology and risk factors for OSD remain a matter of debate, and rectus femoris tightness6, 7, 8 and repetitive sports activities9,10 have been well described.11 OSD occurs more commonly in male patients and is associated with participation in repetitive running and jumping sports. It typically presents during the peak growth velocity years of 8 to 12 for girls and 12 to 15 for boys,1,12,13 and 20% to 30% of cases are bilateral.14,15 In a cross-sectional study of 956 adolescent students (mean age: 13.7 years), de Lucena et al.10 found an OSD prevalence of 9.8% (11% in male patients and 8.3% in female patients), whereas Kujala et al.16 in a retrospective survey found a prevalence of 12.9% (mean age: 13.1 years), with OSD roughly 4 times more common in athletes versus nonathletes. Male patients have OSD more often than female patients, at a ratio of 3:1.11,17
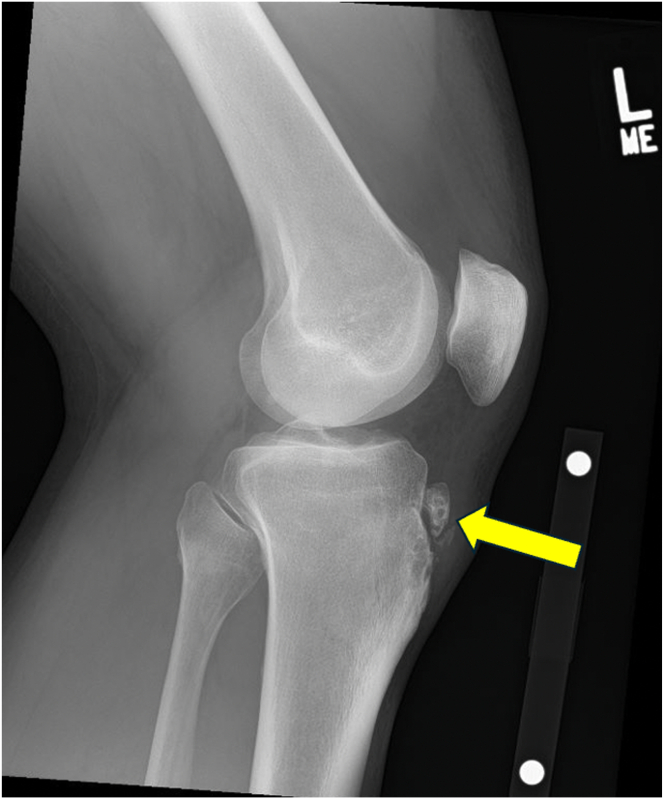
OSD is self-limiting in 90% of cases and resolves at skeletal maturity with fusion of the tibial tubercle apophysis.17 Knee radiographs show nonunited tibial tubercle ossicles, such as in the case described in this Technical Note (Fig 1), and magnetic resonance imaging can be used to assess whether ossicles are located within the patellar tendon. Treatment recommendations include hamstring and quadriceps stretches, relative rest and activity modification to reduce pain, as well as nonsteroidal anti-inflammatory drugs and ice application.2,18 In up to 10% of cases, symptoms fail to resolve with conservative measures and persist beyond skeletal maturity, and these patients may benefit from open or arthroscopic surgical excision of ossicles to eliminate the chronic mechanical patellar tendon irritation of OSD.15,19, 20, 21, 22, 23, 24, 25
Fig 1.
Preoperative lateral radiograph of the left knee with a nonunited Osgood-Schlatter ossicle at the tibial tubercle (yellow arrow).
Excellent patient outcomes have been described after surgical intervention for unresolved OSD, with resolution of pain and return to preoperative levels of sports participation.20, 21, 22,24,26, 27, 28 In this Technical Note, we describe our preferred technique for open excision of large symptomatic intratendinous Osgood-Schlatter ossicles in an adult patient, followed by knotless FiberTape suture anchor fixation of the patellar tendon to the tibial tubercle.
Surgical Technique
Patient Positioning and Anesthesia
After placement of adductor and sciatic nerve blocks under ultrasound guidance, the patient is placed in the supine position on the operating table with all bony prominences well padded. General anesthesia is then induced, and a well-padded tourniquet is insufflated. A knee examination under anesthesia is performed, which confirms a normal and intact ligamentous examination as well as full range of motion of the right knee.
Knee Arthroscopy
Knee arthroscopy is performed using low anteromedial and anterolateral portals. Medial and lateral meniscus structures are noted to be intact, as well as most of the cartilage within the knee, with the exception of grade 1 and grade 2 chondromalacia of the medial patellar facet. Extensive synovitis is noted in the superior gutter, suprapatellar pouch, and inferior patellar space, and this is debrided with a combination of arthroscopic shaver and radiofrequency ablation. A scarred and thickened pseudocapsule is noted medially, as well as a large plica, and these also are debrided. A chondroplasty of the medial patellar facet is performed, and the cartilage is brought back to a stable rim without loose fragments.
Open OSD Ossicle Excision
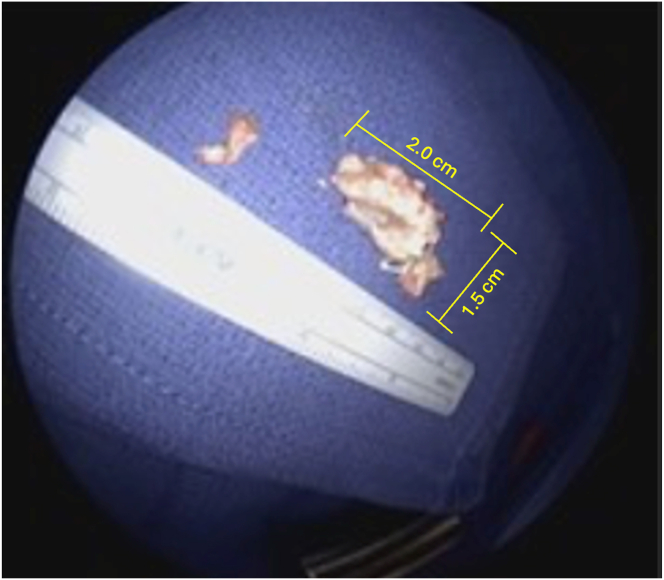
Attention is then turned to the open part of the procedure. A 7-cm incision is made directly over the palpable Osgood-Schlatter ossicle with the knee positioned in 30 degrees of flexion with a bump under the knee, and dissection is carried down to the patellar tendon with a No. 15 blade and electrocautery. The paratenon is incised using Metzenbaum scissors, and flaps of the paratenon are elevated for later repair. The patellar tendon is then incised in a longitudinal fashion over the Osgood-Schlatter ossicle using a No. 15 blade. The ossicle is identified and sharply dissected out of the patellar tendon using a combination of sharp dissection and Metzenbaum scissors, with care taken to preserve the patellar tendon at all times. A 1.5-cm × 2-cm Osgood-Schlatter ossicle is removed (Fig 2). The remaining calcific portions of the tendon insertion are also debrided using a rongeur.
Fig 2.
Excised Osgood-Schlatter ossicles from the left knee of a 43-year-old male patient with adult-onset Osgood-Schlatter disease. The ossicle was taken to the back table and measured at 1.5 cm × 2 cm.
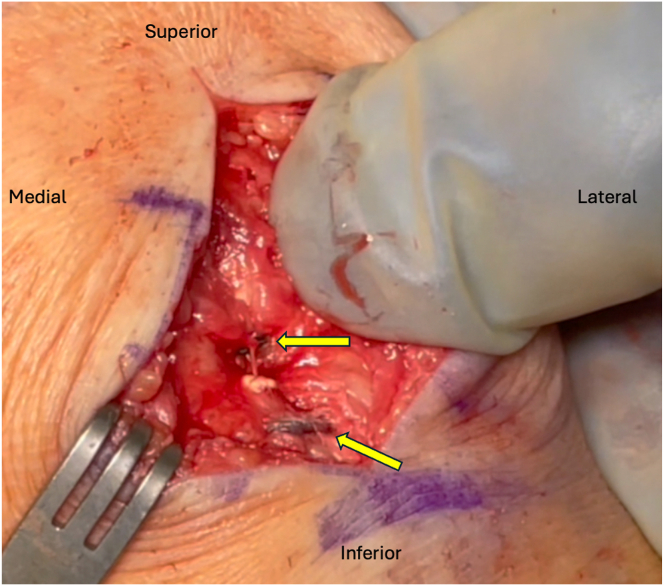
Suture Anchor Patellar Tendon Fixation
A high-speed burr is used to create a bed of bleeding bone at the tibial tubercle to repair the tendon. Two high-strength sutures (FiberTape; Arthrex, Naples, FL) are used in a horizontal, everted mattress fashion to repair the patellar tendon side to side. Two suture anchors (4.75-mm PEEK [polyether ether ketone] SwiveLock; Arthrex) are then placed into the bed of bleeding bone, and sutures from these anchors are used to repair the central aspect of the tendon back down to the tibial tubercle (Fig 3). The patellar incision is copiously irrigated and closed in a layered fashion using 2-0 and 3-0 absorbable subcuticular sutures (MONOCRYL; Ethicon, Cornelia, GA). The portal incisions are closed using the same 3-0 subcuticular suture.
Fig 3.
Suture anchor fixation for patellar tendon repair using 2 PEEK (polyether ether ketone) SwiveLock suture anchors (Arthrex, Naples, FL) (yellow arrows). The anchors are placed into the bed of bleeding bone, and the sutures are used to repair the central aspect of the patellar tendon back down to the tibial tubercle.
Postoperative Rehabilitation
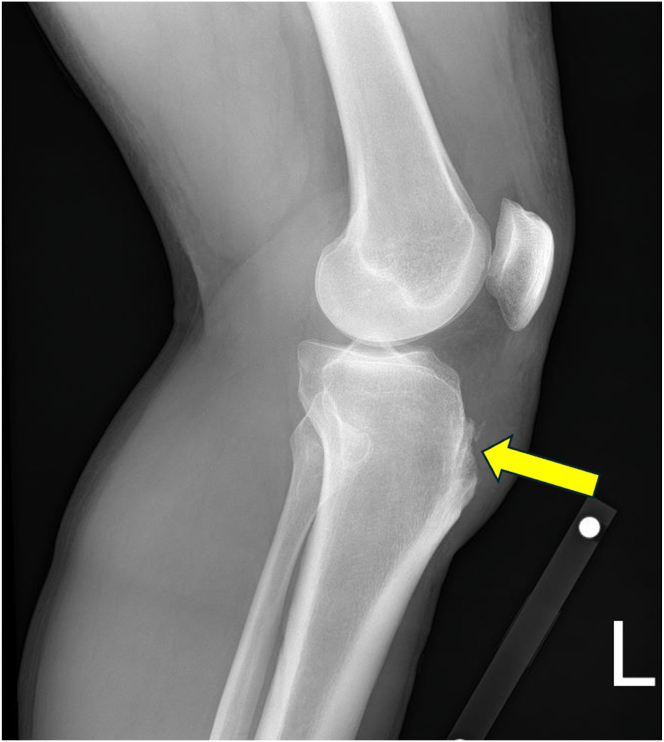
The patient is toe-touch weight-bearing for 2 weeks after surgery. A hinged knee brace is worn for 2 weeks, with the knee range of motion set to between 0 and 45° of knee flexion. A standard postoperative knee arthroscopy physical therapy protocol is prescribed. A postoperative lateral knee radiograph confirms the successful excision of the OSD ossicle (Fig 4). Return to full activity is expected 3 months postoperatively.
Fig 4.
One-month postoperative lateral radiograph of the left knee after excision of an Osgood-Schlatter ossicle for a 43-year-old male patient who was diagnosed with adult-onset Osgood-Schlatter disease. The yellow arrow shows from where the ossicle was excised.
Discussion
This Technical Note and Video 1 describe our technique for ossicle excision in the setting of large, symptomatic OSD ossicles located within the patellar tendon. Recommendations for surgical planning include determining ossicle location—intratendinous versus intra-articular—to guide open versus arthroscopic excision, as well as using suture anchors for fixation of the distal patellar tendon after excision of the Osgood-Schlatter ossicle, as noted in the pearls and pitfalls of Table 1.
Table 1.
Pearls and Pitfalls of Osgood-Schlatter Ossicle Excision
| Pearls | Pitfalls |
|---|---|
| Open excision allows for direct visualization and safe excision of intratendinous OSD ossicles. | Damage to the patellar tendon should be carefully avoided during excision of intratendinous ossicles. |
| Suture anchor insertional repair of the distal patellar tendon to a bleeding bone bed on the tibial tubercle ensures strong fixation and promotes healing. | Not having anatomic tendon repair could lead to overconstraint of the patellar tendon. |
| Knotless decreases postoperative tendon pain/issues. | Avoid bulky knots. |
| Use knotless anchors and flat tapes. | |
| Start early rehabilitation. |
OSD, Osgood-Schlatter disease.
A number of techniques have been described for the surgical management of symptomatic chronic OSD, including drilling of the tibial tubercle, ossicle excision, bone peg insertion to induce fusion, open excision of loose fragments, and closing-wedge tubercle osteotomy.15 Open or arthroscopic techniques may be used, and knee arthroscopy is beneficial, as it allows additional intra-articular pathologies to be addressed. Regarding the excision of ossicles, arthroscopy does not violate the patellar tendon and avoids an incision directly over the patellar tendon and tibial tubercle, which could be painful with kneeling.27,29 With open techniques, complete reduction of pain and return to preoperative activity levels have been reported in multiple studies,25,27,28 and in this case, an open approach was used with a longitudinal incision through the patella tendon. This allowed for effective ossicle visualization and excision, which was followed by patellar tendon side-to-side repair. A recommendation from our technique is to repair the distal patellar tendon to the tibial tubercle with suture anchors. This closes the dead space resulting from the excision of OSD ossicles, reinforces the patellar tendon side-to-side repair, and protects the extensor mechanism by providing additional fixation of the patellar tendon to the tibial tubercle.
Our described OSD ossicle excision technique is an effective option for the treatment of chronic, symptomatic intratendinous ossicles. Suture anchor insertional repair of the distal patellar tendon to the tibial tubercle promotes healing and decreases the risk of postoperative extensor mechanism compromise.
Disclosures
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: M.T.P. reports consulting or advisory, funding grants, and travel reimbursement from Arthrex; consulting or advisory for Arthrosurface, Anika Therapeutics, and JRF Ortho; funding grants from the U.S. Department of Defense and National Institutes of Health; board membership for the Arthroscopy Association of North America, American Academy of Orthopaedic Surgeons, American Orthopaedic Society for Sports Medicine, American Shoulder and Elbow Surgeons, San Diego Shoulder Institute, and The Society of Military Orthopaedic Surgeons. M.T.P. is an editorial board member for Arthroscopy. All other authors (F.R.P., R.J.W., W.H.B., P.G., B.T.P.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supplementary Data
We present our technique for Osgood-Schlatter ossicle excision for the treatment of adult-onset Osgood-Schlatter disease. We are presenting the case of a 43-year-old male patient with chronic left knee pain at the site of a nonunioned Osgood-Schlatter ossicle proximal to his tibial tubercle. He had not responded to conservative therapy. Magnetic resonance imaging confirmed a large nonunioned ossicle in the distal aspect of the patellar tendon with surrounding edema. The patient has been indicated for adult-onset Osgood-Schlatter disease. He has had symptomatic knee pain and stiffness for >10 years. Kneeling causes significant pain for the patient, which is required for his job. He has tenderness on direct palpation of the tibial tubercle. The patient is placed in a supine position, and all bony prominences are well padded. A diagnostic knee arthroscopy and arthroscopic debridement are carried out using 2 inferior portals. The extensive synovitis in the superior gutter, suprapatellar pouch, and inferior patellar space is debrided. The scarred and thickened pseudocapsule and large plica are debrided, and a chondroplasty of the medial patellar facet is performed. The open portion of this procedure begins with a 7-mm incision made directly over the palpable Osgood-Schlatter ossicle, and the dissection is carried down to the patellar tendon with a No. 15 blade and Bovie. The paratenon is incised using Metzenbaum scissors, and flaps of the paratenon are elevated for later repair. The patellar tendon is then incised in a longitudinal fashion over the Osgood-Schlatter ossicle using a No. 15 blade. The ossicle is identified and sharply dissected out of the patellar tendon using a combination of sharp dissection and Metzenbaum scissors, with care taken to preserve the patellar tendon at all times. A 1.5-cm × 2-cm Osgood-Schlatter ossicle is removed. The remaining calcific portions of the tendon insertion are also debrided using a rongeur. A high-speed burr is used to create a good bed of bleeding bone at the proximal aspect of the tibial tubercle for repair of the tendon. Two Arthrex FiberTape sutures are used in a horizontal mattress fashion to repair the patellar tendon side to side. Two 4.75-mm PEEK SwiveLock anchors (Arthrex, Naples, FL) are then placed into the bed of bleeding bone using the 2 sutures to repair the central aspect of the tendon back down to the tibial tubercle. Skin and subcutaneous tissues are closed in a routine fashion. This patellar incision is copiously irrigated and closed in a layered fashion using 2-0 MONOCRYL (Ethicon, Cornelia, GA) and 3-0 MONOCRYL subcuticular sutures. The portal incisions are closed using a 3-0 MONOCRYL subcuticular suture. The patient is toe-touch weight-bearing for 2 weeks after surgery. A hinged knee brace is worn for 3 weeks with knee range of motion set to between 0 and 45° of knee flexion. A standard postoperative knee arthroscopy physical therapy protocol is prescribed. Postoperative lateral knee radiograph confirms successful excision of the OSD ossicle. Return to full activity is expected 3 months postoperatively.
References
- 1.Smith J.M., Varacallo M. StatPearls. Treasure Island (FL) StatPearls Publishing; 2024. Osgood-Schlatter disease.https://www.ncbi.nlm.nih.gov/books/NBK441995/ [PubMed] [Google Scholar]
- 2.Patel D.R., Villalobos A. Evaluation and management of knee pain in young athletes: Overuse injuries of the knee. Transl Pediatr. 2017;6:190–198. doi: 10.21037/tp.2017.04.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rathleff M.S., Straszek C.L., Blond L., Thomsen J.L. Knee pain in children and adolescents. Ugeskr Laeger. 2019;181 [in Danish] [PubMed] [Google Scholar]
- 4.Haines M., Pirlo L., Bowles K.A., Williams C.M. Describing frequencies of lower-limb apophyseal injuries in children and adolescents: A systematic review. Clin J Sport Med. 2022;32:433–439. doi: 10.1097/JSM.0000000000000925. [DOI] [PubMed] [Google Scholar]
- 5.Pagenstert G., Wurm M., Gehmert S., Egloff C. Reduction osteotomy of the prominent tibial tubercle after Osgood-Schlatter disease. Arthroscopy. 2017;33:1551–1557. doi: 10.1016/j.arthro.2017.02.012. [DOI] [PubMed] [Google Scholar]
- 6.Enomoto S., Oda T., Sugisaki N., Toeda M., Kurokawa S., Kaga M. Muscle stiffness of the rectus femoris and vastus lateralis in children with Osgood-Schlatter disease. Knee. 2021;32:140–147. doi: 10.1016/j.knee.2021.08.001. [DOI] [PubMed] [Google Scholar]
- 7.Nakase J., Goshima K., Numata H., Oshima T., Takata Y., Tsuchiya H. Precise risk factors for Osgood-Schlatter disease. Arch Orthop Trauma Surg. 2015;135:1277–1281. doi: 10.1007/s00402-015-2270-2. [DOI] [PubMed] [Google Scholar]
- 8.Nakase J., Aiba T., Goshima K., et al. Relationship between the skeletal maturation of the distal attachment of the patellar tendon and physical features in preadolescent male football players. Knee Surg Sports Traumatol Arthrosc. 2014;22:195–199. doi: 10.1007/s00167-012-2353-3. [DOI] [PubMed] [Google Scholar]
- 9.Gaulrapp H., Nuhrenborger C. The Osgood-Schlatter disease: A large clinical series with evaluation of risk factors, natural course, and outcomes. Int Orthop. 2022;46:197–204. doi: 10.1007/s00264-021-05178-z. [DOI] [PubMed] [Google Scholar]
- 10.de Lucena G.L., dos Santos Gomes C., Guerra R.O. Prevalence and associated factors of Osgood-Schlatter syndrome in a population-based sample of Brazilian adolescents. Am J Sports Med. 2011;39:415–420. doi: 10.1177/0363546510383835. [DOI] [PubMed] [Google Scholar]
- 11.Lucenti L., Sapienza M., Caldaci A., Cristo C., Testa G., Pavone V. The etiology and risk factors of Osgood-Schlatter disease: A systematic review. Children (Basel) 2022;9(6) doi: 10.3390/children9060826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Indiran V., Jagannathan D. Osgood-Schlatter disease. N Engl J Med. 2018;378:e15. doi: 10.1056/NEJMicm1711831. [DOI] [PubMed] [Google Scholar]
- 13.Zonfrillo M.R., Spicer R.S., Lawrence B.A., Miller T.R. Incidence and costs of injuries to children and adults in the United States. Inj Epidemiol. 2018;5:37. doi: 10.1186/s40621-018-0167-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Corbi F., Matas S., Alvarez-Herms J., et al. Osgood-Schlatter disease: Appearance, diagnosis and treatment: A narrative review. Healthcare (Basel) 2022;10:1011. doi: 10.3390/healthcare10061011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McDonough G.R., Rossi M.J. Arthroscopic resection of symptomatic tibial tubercle ossicles for recalcitrant Osgood-Schlatter disease using a 2-portal technique. Arthrosc Tech. 2022;11:e813–e818. doi: 10.1016/j.eats.2021.12.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kujala U.M., Kvist M., Heinonen O. Osgood-Schlatter's disease in adolescent athletes. Retrospective study of incidence and duration. Am J Sports Med. 1985;13:236–241. doi: 10.1177/036354658501300404. [DOI] [PubMed] [Google Scholar]
- 17.Gholve P.A., Scher D.M., Khakharia S., Widmann R.F., Green D.W. Osgood Schlatter syndrome. Curr Opin Pediatr. 2007;19:44–50. doi: 10.1097/MOP.0b013e328013dbea. [DOI] [PubMed] [Google Scholar]
- 18.Midtiby S.L., Wedderkopp N., Larsen R.T., Carlsen A.F., Mavridis D., Shrier I. Effectiveness of interventions for treating apophysitis in children and adolescents: Protocol for a systematic review and network meta-analysis. Chiropr Man Therap. 2018;26:41. doi: 10.1186/s12998-018-0209-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Binazzi R., Felli L., Vaccari V., Borelli P. Surgical treatment of unresolved Osgood-Schlatter lesion. Clin Orthop Relat Res. 1993;(289):202–204. [PubMed] [Google Scholar]
- 20.Zhi-Yao L.I. Arthroscopic excision of a huge ununited ossicle due to Osgood-Schlatter disease in an adult patient. J Orthop Case Rep. 2013;3:4–7. doi: 10.13107/jocr.2250-0685.092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsakotos G., Flevas D.A., Sasalos G.G., Benakis L., Tokis A.V. Osgood-Schlatter lesion removed arthroscopically in an adult patient. Cureus. 2020;12:e7362. doi: 10.7759/cureus.7362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flowers M.J., Bhadreshwar D.R. Tibial tuberosity excision for symptomatic Osgood-Schlatter disease. J Pediatr Orthop. 1995;15:292–297. doi: 10.1097/01241398-199505000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Choi W., Jung K. Intra-articular large ossicle associated to Osgood-Schlatter disease. Cureus. 2018;10 doi: 10.7759/cureus.3008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pihlajamaki H.K., Visuri T.I. Long-term outcome after surgical treatment of unresolved Osgood-Schlatter disease in young men: Surgical technique. J Bone Joint Surg Am. 2010;92:258–264. doi: 10.2106/JBJS.J.00450. [DOI] [PubMed] [Google Scholar]
- 25.El-Husseini T.F., Abdelgawad A.A. Results of surgical treatment of unresolved Osgood-Schlatter disease in adults. J Knee Surg. 2010;23:103–107. doi: 10.1055/s-0030-1267474. [DOI] [PubMed] [Google Scholar]
- 26.Weiss J.M., Jordan S.S., Andersen J.S., Lee B.M., Kocher M. Surgical treatment of unresolved Osgood-Schlatter disease: Ossicle resection with tibial tubercleplasty. J Pediatr Orthop. 2007;27:844–847. doi: 10.1097/BPO.0b013e318155849b. [DOI] [PubMed] [Google Scholar]
- 27.Pihlajamaki H.K., Mattila V.M., Parviainen M., Kiuru M.J., Visuri T.I. Long-term outcome after surgical treatment of unresolved Osgood-Schlatter disease in young men. J Bone Joint Surg Am. 2009;91:2350–2358. doi: 10.2106/JBJS.H.01796. [DOI] [PubMed] [Google Scholar]
- 28.Circi E., Beyzadeoglu T. Results of arthroscopic treatment in unresolved Osgood-Schlatter disease in athletes. Int Orthop. 2017;41:351–356. doi: 10.1007/s00264-016-3374-1. [DOI] [PubMed] [Google Scholar]
- 29.Circi E., Atalay Y., Beyzadeoglu T. Treatment of Osgood-Schlatter disease: Review of the literature. Musculoskelet Surg. 2017;101:195–200. doi: 10.1007/s12306-017-0479-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
We present our technique for Osgood-Schlatter ossicle excision for the treatment of adult-onset Osgood-Schlatter disease. We are presenting the case of a 43-year-old male patient with chronic left knee pain at the site of a nonunioned Osgood-Schlatter ossicle proximal to his tibial tubercle. He had not responded to conservative therapy. Magnetic resonance imaging confirmed a large nonunioned ossicle in the distal aspect of the patellar tendon with surrounding edema. The patient has been indicated for adult-onset Osgood-Schlatter disease. He has had symptomatic knee pain and stiffness for >10 years. Kneeling causes significant pain for the patient, which is required for his job. He has tenderness on direct palpation of the tibial tubercle. The patient is placed in a supine position, and all bony prominences are well padded. A diagnostic knee arthroscopy and arthroscopic debridement are carried out using 2 inferior portals. The extensive synovitis in the superior gutter, suprapatellar pouch, and inferior patellar space is debrided. The scarred and thickened pseudocapsule and large plica are debrided, and a chondroplasty of the medial patellar facet is performed. The open portion of this procedure begins with a 7-mm incision made directly over the palpable Osgood-Schlatter ossicle, and the dissection is carried down to the patellar tendon with a No. 15 blade and Bovie. The paratenon is incised using Metzenbaum scissors, and flaps of the paratenon are elevated for later repair. The patellar tendon is then incised in a longitudinal fashion over the Osgood-Schlatter ossicle using a No. 15 blade. The ossicle is identified and sharply dissected out of the patellar tendon using a combination of sharp dissection and Metzenbaum scissors, with care taken to preserve the patellar tendon at all times. A 1.5-cm × 2-cm Osgood-Schlatter ossicle is removed. The remaining calcific portions of the tendon insertion are also debrided using a rongeur. A high-speed burr is used to create a good bed of bleeding bone at the proximal aspect of the tibial tubercle for repair of the tendon. Two Arthrex FiberTape sutures are used in a horizontal mattress fashion to repair the patellar tendon side to side. Two 4.75-mm PEEK SwiveLock anchors (Arthrex, Naples, FL) are then placed into the bed of bleeding bone using the 2 sutures to repair the central aspect of the tendon back down to the tibial tubercle. Skin and subcutaneous tissues are closed in a routine fashion. This patellar incision is copiously irrigated and closed in a layered fashion using 2-0 MONOCRYL (Ethicon, Cornelia, GA) and 3-0 MONOCRYL subcuticular sutures. The portal incisions are closed using a 3-0 MONOCRYL subcuticular suture. The patient is toe-touch weight-bearing for 2 weeks after surgery. A hinged knee brace is worn for 3 weeks with knee range of motion set to between 0 and 45° of knee flexion. A standard postoperative knee arthroscopy physical therapy protocol is prescribed. Postoperative lateral knee radiograph confirms successful excision of the OSD ossicle. Return to full activity is expected 3 months postoperatively.