Abstract
Meniscal root tears are recognized as an important pathology. Failure to recognize and to treat this pathology could lead to early-onset osteoarthritis, similar to a total meniscectomy. Surgical treatment is essential to restore meniscal function and to normalize compartment contact pressures, whenever there is joint overload and not severe cartilaginous damage. Still, the biological healing property of the medial meniscus is poor, and failure of the surgical procedure may occur. This Technical Note proposes a technical procedure for revision of medial meniscus posterior root reconstruction with a split-gracilis autograft tendon anatomical transtibial pullout technique.
Technique Video
Meniscus root tears are defined as complete radial tears or avulsion of the anterior or posterior tibial attachments of the meniscus.1 Despite accounting for only 7% to 9% of meniscal injuries, meniscus root tears are notorious because they lead to a nonfunctioning meniscus, which means if they are left untreated, degenerative arthritis changes can occur similar to those seen in a knee with complete meniscectomy.2,3 Medial meniscus posterior root tear (MMPRT) can alter normal knee kinematics, can increase tibiofemoral contact pressure in the medial compartment up to 25%, and can lead to rapid progression of degenerative changes. The surgical options available to treat MMPRT include meniscectomy, meniscus repair, and meniscal root reconstruction, depending on the chronicity of the tear, stability of knee, and degree of existing arthrosis.4
Although the ideal surgical technique for MMPRT is still debatable, the transtibial pullout technique is popular for MMPRT repair, with promising results reported.5,6 Feucht et al.7 reviewed the transtibial pullout technique for medial meniscus posterior root repairs and concluded that 62% of patients had complete healing, 34% had partial healing, and 10% had a retear. Similarly, LaPrade et al.8 reported a 9.7% failure rate and need for revision after repair of MMPRT using the transtibial pullout technique. Recently, MMPRT repair with biological augmentation has gained popularity: the first case series shows lower rate of failure compared with the traditional techniques. Biological augmentation seems to be tempting, as meniscal surgery is burdened of high failure rate.9, 10, 11
There is a scarcity of literature that describes the best way to treat a cut-through of a MMPRT repair by the transtibial pullout technique. Herein, we describe a technique that uses a split-gracilis autograft reconstruction with a pullout through the tibia fixed with an interference screw to treat a failed MMPRT repair (Fig 1).
Fig 1.
Magnetic resonance, Sagittal view - Left knee, short tau inversion recovery sequence. The asterisk shows the typical “ghost sign” caused by the posterior horn avulsion of the medial meniscus. The white arrow points to the tibial tunnel, which was created to perform a pullout technique for the MMPR repair. The presence of the “ghost sign” suggests that the previous surgery has failed, and another MMPR avulsion has occurred. (MMPR, medial meniscus posterior root.)
Surgical Technique
Details of the technique are shown in the Video 1. Pearls and pitfalls and the advantages and disadvantages of this approach are described in Tables 1 and 2, respectively. Video 1 describes a case of a failed MMPR repair using a pullout with a nonresorbable suture, in which the decision was made to attempt a revision with a posterior root reconstruction with split gracilis tendon.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
| Releasing the superficial MCL, using the “pie-crust” technique, may be needed. Identify the anatomical footprint with an ACL tibial guide compass, opened at 60°. Check the position of the K-wire, and if it’s satisfying, proceed with the drilling To avoid cartilage damage, the ACL tibial guide needs to be inserted in horizontal position and to be turned in vertical position once it has reached the posterior rim of the TP. Dilate the “meniscus tunnel” with a knotted suture tape before passing the graft. Pass the graft from superior to inferior. |
In case of revision surgery of MMPR repair, the posterior margin of the meniscus could be damaged; it may be necessary to place the tunnel in the toward the meniscus body. During autograft harvesting, excessive pulling of the tendon may result in premature rupture of the graft. No dedicated instrumentation is available; an ACL tibial guide may be too bulky to reach the MMPR footprint. |
ACL, anterior cruciate ligament; MCL, medial collateral ligament, MMPR, medial meniscus posterior root; TP, tibial plateau.
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| The procedure provides reattachment of the MMPR to its anatomical footprint. The autograft provides primary and secondary fixation of the posterior root of the meniscus, thanks to tendon-bone healing process. Split-gracilis tendon allows a less-invasive “tunnel” in the meniscus. The diameter of the tibial tunnel is decreased to the minimum. A lower rate of donor-site morbidity is expected since part of the gracilis tendon remains attached. Screw fixation provides modular tensioning of the meniscus root. The procedure does not require additional arthroscopic portals. |
The procedure is complex, extensive skills are required, and the operative time may be variable prolonged. Split gracilis tendon harvesting is more complicated, and premature tendon rupture may occur. Using screw fixation, a longer graft is required to ensure the graft itself engages with the screw. |
MMPR, medial meniscus posterior root.
Patient Positioning
The patient is positioned supine with dangling leg, and thigh tourniquet at 250 mmHg. An eletric leg holder (Maquet, Rastatt, Germany) has been used; the positioning allows knee motion between 0° and 120° of ROM.
Arthroscopic Debridement of the Meniscal Tear and MMPR Preparation
Standard anterolateral and anteromedial (AM) portals are created. The posterior horn meniscal tear is identified, and its mobility is tested with an arthroscopic hook (Fig 2). The degenerated meniscal tissue is shaved off (Fig 3).
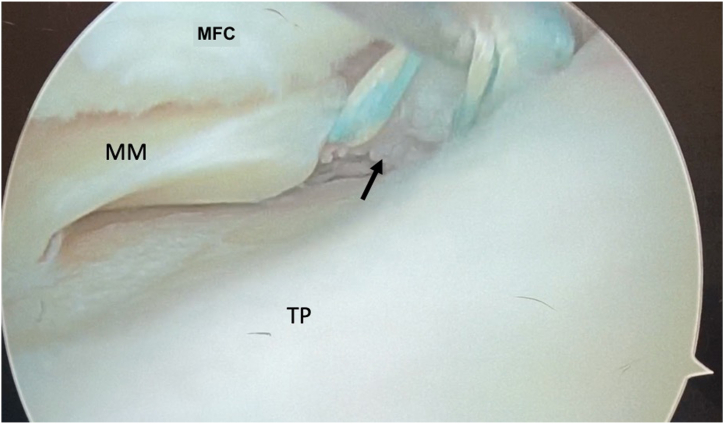
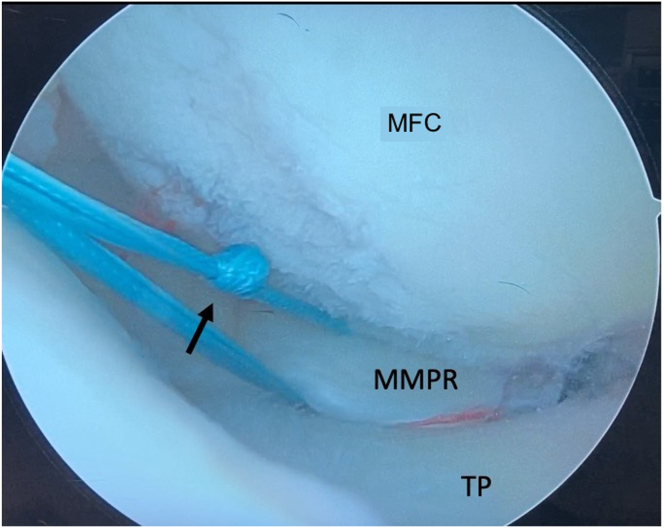
Fig 2.
Intraoperative arthroscopic image. The camera is on the anterolateral portal. It is possible to see whether the previous sutures, pointed out by the black arrow, are no longer tightened and so the sutures can be pulled by the hook. The medial meniscus posterior root is so detached, and this intraoperative finding comes along with the hypothesis made by the magnetic resonance imaging. (MFC, medial femoral condyle; MM, medial meniscus; TP, tibial plateau.)
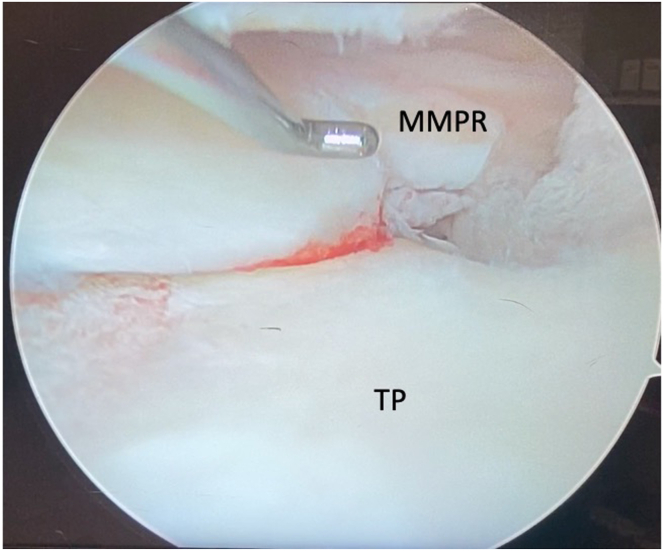
Fig 3.
Intraoperative arthroscopic image, left knee with camera in the anterolateral portal; the hook goes through the anteromedial portal. The medial meniscus has been debrided from any residual scar tissue due to previous operation, and it is clear that the new point of suture attachment must be toward the posterior meniscus horn and meniscus body to avoid any biological failure of the procedure. The circle underlines the previous bone tunnel intra-articular exit point, which appears to be in desirable position, so in this circumstance, the old tunnel trajectory may be reused. (MMPR, medial meniscus posterior root; TP, tibial plateau.)
Because it is a revision of pullout meniscus suture, the wire that was fixing the meniscus is carefully removed by using a hook to untie the knot. Once the wire is separated from the meniscus, arthroscopic scissors are used to cut the wire. The MMPR is armed with a No. 2 FiberWire (Arthrex, Naples, FL) using the FIRSTPASS suture passer (Smith & Nephew, London, UK) (Fig 4). This FiberWire is passed though the meniscus and the ends of the suture are retrieved through the AM portal.
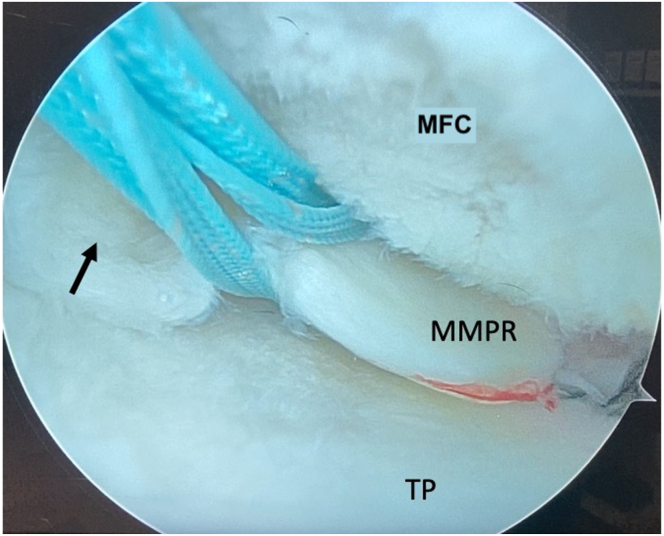
Fig 4.
Intraoperative arthroscopic image, left knee, camera in the anterolateral portal. Dedicated instrumentation has been used to let a unabsorbable wire (black arrow) to pass through the medial meniscus. The suture comes out from the anteromedial portal. Since the created hole is going to be enlarged to let the tendon pass through it, it’s utmost important to choose a safe zone in healthy meniscal tissue, not too close to the edge of the posterior horn, toward the body of the meniscus. (MFC, medial femoral condyle; MMPR, medial meniscus posterior root; TP, tibial plateau.)
Graft Harvesting and Preparation
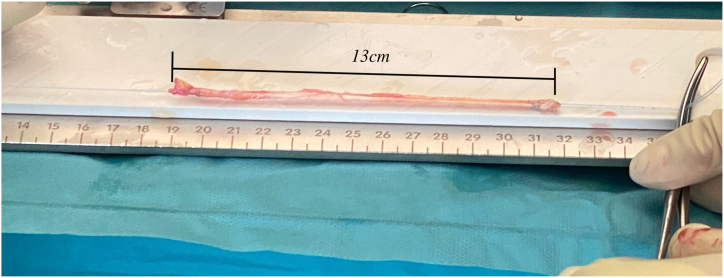
A 3-cm longitudinal skin incision is made on the medial side of the tibia. The sartorius fascia is incised and the gracilis just below is confirmed and isolated along its course. With a scalpel, the gracilis tendon is split until a 5-mm width graft is obtained. With an open tendon stripper, the split gracilis is harvested. The final length of the graft should be at least 10 cm. The muscular remnants are peeled off the graft, and at both ends 3 series of Krachow stiches are placed with No. 2-0 FiberWire (Arthrex) (Fig 5).
Fig 5.
A dedicated graft-preparing station has been used, and the split-gracilis tendon has been harvested, at both ends 3 series of Krachow stiches has been made, using an unabsorbable wire. The obtained length (13 cm) is enough to pass through the meniscus and to be pulled in the tibial tunnel in double strand. The diameter of the graft is less than 2 mm, so it’s possible to use the smallest drilling size to make the tibial tunnel and to let the autograft pass in double strand.
Tibial Tunnel Preparation
A tibial anterior cruciate ligament guide (ACUFEX PINPOINT; Smith & Nephew), opened at 60°, is introduced through the AM portal, and the tunnel entry point in the joint is determined. A 2.4-mm K-wire is drilled through the tibia until the tip of the wire appears in the joint.
If the MMPR has been repositioned in the anatomical position from the previous repair, the original tibial tunnel is exploited. Otherwise, a new tunnel is created.
If the original tibial tunnel is being reused, first the suture material used to fix the MMPR tear has to be removed. A 2.4-mm K-wire is inserted through the old tunnel to get the right direction.
In either case, the incision used for graft harvesting can be exploited to point the anterior cruciate ligament guide to the bone. Once the K-wire is positioned in the tibia, a cannulated 4.5-mm traumatic drill (the tip of the drill is sharp) is used to create the tibial tunnel to allow graft passage.
Graft Passage
The FiberWire, which passes through the meniscus, is knotted and is passed back and forth several times through the meniscus until the perforation is enlarged and it will be appropriate to accept the diameter of the gracilis graft (Fig 6). The graft is linked to the FiberWire and pulled from the AM portal through the medial meniscus from superior to inferior. The graft is pulled until both ends are at equal length (Fig 7).
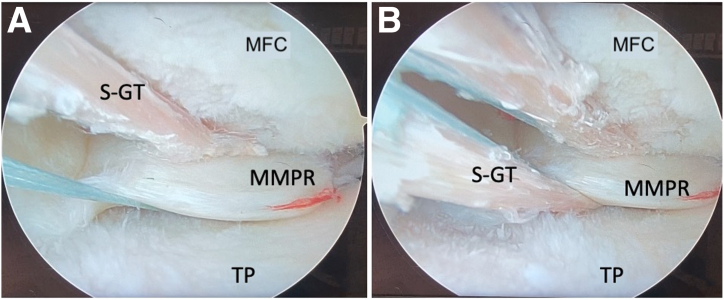
Fig 6.
Intraoperative arthroscopic image, left knee, camera in the anterolateral portal. A knot (black arrow) is made in the wire that goes through the MMPR. The wire is passed through the meniscus in such a way as to enlarge the hole, so that the later graft can pass through it, lowering the risk of iatrogenic meniscus rupture. (MFC, medial femoral condyle; MMPR, medial meniscus posterior root; TP, tibial plateau.)
Fig 7.
Intraoperative images. Left knee, camera goes through the anterolateral portal. (a) The graft is passed through the meniscus from superior to inferior. (b) The graft is pulled until the ends are at equal length. It can be seen that the graft passes more medial than the posterior root; the choice has been made to ensure the graft passes through a healthy meniscus, especially after the previous failure. (MFC, medial femoral condyle; MMPR, medial meniscus posterior root; S-GT, split-gracilis tendon TP, tibial plateau.)
Nitinol wire with an eyelet at its end is passed through the tibial tunnel and retrieved from the AM portal. Then, a No. 2 VICRYL suture is passed through the nitinol eyelet. Since the graft passage is made in 2 steps, the VICRYL is needed for retrieving the nitinol wire after the first end of the graft has been pulled in the tibial tunnel, without loosing the former and it’s time saving, since there is no need for the tibial guide to be repositioned for passing the nitinol wire.
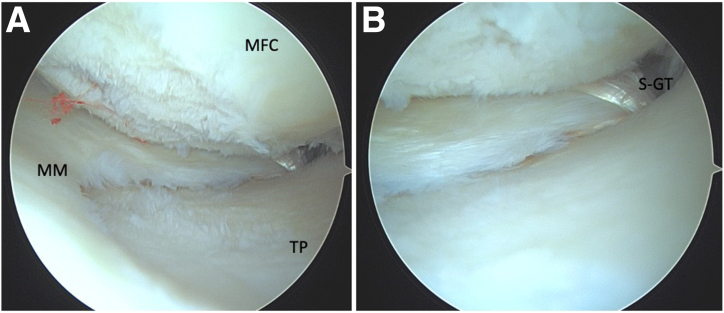
Both of the ends of the gracilis graft are pulled through the tibial tunnel and tightened. The graft is fixed to the tunnel with 5 × 20-mm resorbable interference screw. The medial meniscus will consequently be tightened toward the tunnel the more the screw will be advanced. The interference screw is advanced until anatomical reinsertion of the MMPH and the C-shape of medial meniscus is visualized (Fig 8).
Fig 8.
Intraoperative images. Left knee. Camera goes through the anterolateral portal. The final result is shown: the medial meniscus has regained the native C-shape (a), and the graft has been tightened through the tibial tunnel and the exposed intra-articular portion of the graft is reduced to the minimum, as it can be seen in the zoomed image (b). (MFC, medial femoral condyle; MMPR, medial meniscus posterior root; S-GT, split-gracilis tendon TP, tibial plateau.)
Postoperative Rehabilitation
Postoperatively, the patient is touch weight-bearing for 6 weeks in a hinged brace. Patient is allowed to 0° to 90° range of motion for the first 4 weeks, which is gradually increased as tolerated with the physical therapist but no passive flexion beyond 120° is allowed in the first 6 weeks. The patient is allowed progressive weight-bearing as tolerated after 6 weeks, and knee brace is weaned off.
Discussion
MMPR plays a crucial role in maintaining the function of the meniscus. Since the effect of the MMPR tear is comparable with total meniscectomy, surgical repair is the preferred option, even if initial stages of cartilaginous degeneration have begun, to protect the joint from accelerated osteoarthritis.3,5 It is well known that surgeries of the menisci are burdened with a high rate of complications, especially the medial meniscus, which has a low biological potential to heal. At present, there is neither a consensus regarding the ideal indications for treating MMPR tear nor regarding the best surgical technique. The transtibial pullout technique is a highly rated choice of surgical treatment for MMPR tear, because it ensures anatomical reinsertion of the posterior horn, allowing the medial meniscus to regain its shape and thus physiological knee joint biomechanics can be restored.8 Despite this technique’s theoretical advantages, Li et al.,11 in a cohort of 35 patients, reported a failure rate of 50% in pullout technique repair of MMPR within 2 years. Recently, MMPR repair with biological augmentation is gaining popularity, as it is reported to have lower failure rate compared with traditional pullout techniques, as per Holmes et al.9
Biological augmentation requires more arduous surgical skills, but it is a tempting option, as biological grafts may ligamentize over time, leading to more physiological attachment of the menisci. This in turn makes it more resistant to failure than synthetic material, as secondary fixation occurs.12 In the revision cases of meniscal tear, biological augmentation seems to be a valuable solution.
The choice of a split-gracilis tendon autograft is dictated by the necessity of a thin graft so as to not induce iatrogenic damage to the MMPR. The properties of an autograft are preferable to those of an allograft.
The limitations of the described technique are multiple: fine surgical skills are required both for the arthroscopy and to harvest the tendons. The MMPR is difficult to reach with arthroscopic devices, and pie-crusting of the medial collateral ligament often is required. The presented technique did not require a posteromedial portal, differently to which can be found in literature, since thanks to the FIRSTPASS Suture Passer, or similar products, and the retrieving carrier suture from the tibial tunnel, the procedure may be managed just from the anterior portals.
The use of an interference screw is recommended, as it guarantees stable fixation and when it is advanced through the tunnel, it pulls down on the graft and consequently the meniscus. This allows the surgeon to recreate the anatomical C-shape of the medial meniscus under vision while the screw is advanced. This can better restore the functionality of the medial meniscus and maybe prevent meniscal extrusion over time.
Disclosures
All authors (P.F., A.J., E.A., C.F., C.H.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supplementary Data
The described surgical technique is shown in a revision case of a MMPR repair. The presented case involves a 56-year-old woman who sustained a MMPR avulsion a year before, treated with a transtibial pullout technique using a unabsorbable suture, fixed with at the anteromedial tibial cortex with a button. One year later, the suture failed, and the MMPR was avulsed again, as can be seen in Figures 1 and 2. In a revision setting, it was decided to use a biological augmented procedure to reposition the meniscal root. (MMPR, medial meniscus posterior root.)
References
- 1.LaPrade R.F., Floyd E.R., Carlson G.B., Moatshe G., Chahla J., Monson J.K. Meniscal root tears: Solving the silent epidemic. J Arthrosc Surg Sports Med. 2021;2:47. [Google Scholar]
- 2.Bhatia S., LaPrade C.M., Ellman M.B., LaPrade R.F. Meniscal root tears. Am J Sports Med. 2014;42:3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 3.Lee DR, Lu Y, Reinholz AK, et al. Root repair has superior radiological and clinical outcomes than partial meniscectomy and nonoperative treatment in the management of meniscus root tears: A systematic review [Published online February 2024]. Arthroscopy. https://doi.org/10.1016/j.arthro.2024.02.017. [DOI] [PubMed]
- 4.Lee J.I., Kim D.H., Yoo H.J., Choi H.G., Lee Y.S. Comparison of the predicting performance for fate of medial meniscus posterior root tear based on treatment strategies: A comparison between logistic regression, gradient boosting, and CNN algorithms. Diagnostics. 2021;11:1225. doi: 10.3390/diagnostics11071225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moon H.S., Choi C.H., Jung M., Lee D.Y., Hong S.P., Kim S.H. Early surgical repair of medial meniscus posterior root tear minimizes the progression of meniscal extrusion: 2-year follow-up of clinical and radiographic parameters after arthroscopic transtibial pull-out repair. Am J Sports Med. 2020;48:2692–2702. doi: 10.1177/0363546520940715. [DOI] [PubMed] [Google Scholar]
- 6.Krych A.J., Boos A.M., Lamba A., Smith P.A. Clinical outcome of meniscus centralization with medial meniscus root repair for the extruded medial meniscus. Arthroscopy. 2024;40:1578–1587. doi: 10.1016/j.arthro.2023.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Feucht M.J., Kühle J., Bode G., et al. Arthroscopic transtibial pullout repair for posterior medial meniscus root tears: A systematic review of clinical, radiographic, and second-look arthroscopic results. Arthroscopy. 2015;31:1808–1816. doi: 10.1016/j.arthro.2015.03.022. [DOI] [PubMed] [Google Scholar]
- 8.LaPrade R.F., Matheny L.M., Moulton S.G., James E.W., Dean C.S. Posterior meniscal root repairs: Outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45:884–891. doi: 10.1177/0363546516673996. [DOI] [PubMed] [Google Scholar]
- 9.Holmes S.W., Huff L.W., Montoya K.J., Durkin M.W., Baier A.J. Arthroscopic medial meniscal root reconstruction with gracilis autograft is safe and improves 2-year postoperative patient-reported outcomes. Arthrosc Sports Med Rehabil. 2022;4:e1339–e1346. doi: 10.1016/j.asmr.2022.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ishikawa H., Okamura H., Ohno T., Fujita S., Akezuma H., Inagaki K. Arthroscopic medial meniscus posterior root reconstruction and pull-out repair combined technique for root tear of medial meniscus. Arthrosc Tech. 2022;11:e109–e114. doi: 10.1016/j.eats.2021.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li H., Nie S., Lan M. Medial meniscus posterior root tear reconstructed with gracilis autograft improve healing rate and patient reported outcome measures. BMC Musculoskelet Disord. 2022;23:1094. doi: 10.1186/s12891-022-06067-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li C., Hu X., Meng Q., et al. The potential of using semitendinosus tendon as autograft in rabbit meniscus reconstruction. Sci Rep. 2017;7:7033. doi: 10.1038/s41598-017-07166-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The described surgical technique is shown in a revision case of a MMPR repair. The presented case involves a 56-year-old woman who sustained a MMPR avulsion a year before, treated with a transtibial pullout technique using a unabsorbable suture, fixed with at the anteromedial tibial cortex with a button. One year later, the suture failed, and the MMPR was avulsed again, as can be seen in Figures 1 and 2. In a revision setting, it was decided to use a biological augmented procedure to reposition the meniscal root. (MMPR, medial meniscus posterior root.)