Abstract
The posterior cruciate ligament (PCL) is the strongest ligament of the knee and plays an important role in stabilizing the knee joint posteriorly. PCL tears are common injuries in sports injuries and traffic accidents; however, clinical outcomes after PCL reconstruction have not yet met clinicians’ expectations, with a high postsurgery failure rate reported. Suture tape augmentation and supplementary fixation have shown ideal biomechanical properties in early studies. In this Technical Note, we describe a surgical technique to reconstruct the PCL with suture tape augmentation and transtibial tubercle fixation; the PCL remnant is also preserved. This technique is deemed to improve posterior stability and ultimate failure load for PCL graft over traditional techniques.
Technique Video
The posterior cruciate ligament (PCL) is an essential ligament for knee stability. The complexity of the PCL has generated challenges in the management of PCL injuries. Grade I and II PCL injuries usually can be treated with nonoperative management, but grade III injuries often require PCL reconstruction. Compared with anterior cruciate ligament reconstruction, PCL reconstruction has shown a greater rate of residual laxity and graft failure. In recent studies, suture tape augmentation has shown a positive effect on graft initial stability and posterior stability in long-term follow-up.1,2 Our technique uses suture tape as an internal brace to absorb the load that exceeds the physiological range and to protect the graft from elongation and failure in the ligamentization process. In tibial fixation, the transtibial tubercle fixation technique is used as an additional fixation, which can improve the ultimate failure load.3
Surgical Technique
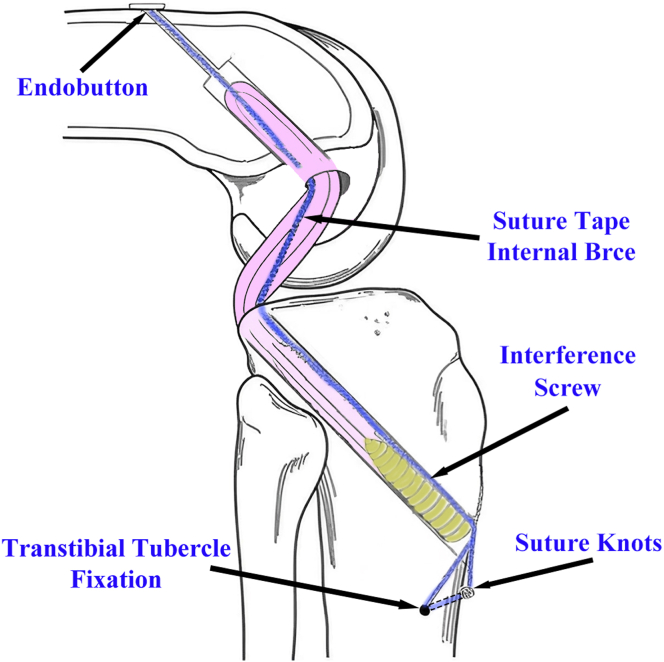
In Figure 1 and Video 1, the complete demonstration is described; the advantages and disadvantages of this technique are shown in Table 1.
Fig 1.
Diagrammatic sketch of posterior cruciate ligament graft fixation. Bule, suture tape internal brace; pink, graft; yellow, interference screw.
Table 1.
Advantages and Disadvantages
| Advantages |
| Preservation of femoral bone stock |
| Preserved PCL remnant protects graft from a killer turn |
| Preserved PCL remnant promotes vascular growth for graft healing, ligamentization, and the restoration of sensation |
| Better biomechanical property in ultimate failure load |
| Disadvantages |
| Longer operative time |
| Possible knee flexion constraint |
| Possible graft stress shielding |
PCL, posterior cruciate ligament.
Patient Positioning and Preparation
The patient is positioned in the supine position with a thigh tourniquet and receives general anesthesia, after which the patient undergoes a basic physical examination, posterior drawer, and anterior drawer and compared with the healthy side.
Graft Harvesting and Preparation
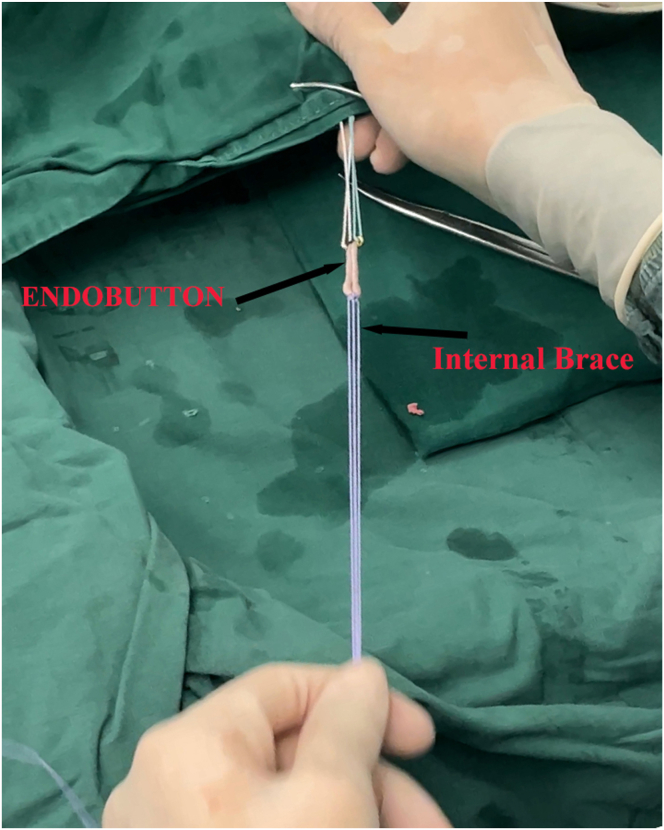
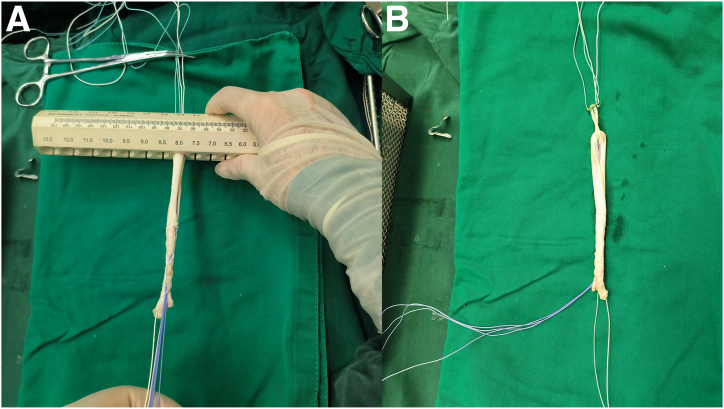
The knee is positioned at 90° of flexion, and a 2- to 3-cm oblique incision between the tibial tubercle and the posteromedial edge of the tibia is made. The semitendinosus tendon and gracilis tendon are separated bluntly and harvested by a tendon stripper. Using an oblique incision can reduce the risk of damage to the infrapatellar branch of the saphenous nerve. Two No. 2-0 OrthoCord sutures (DePuy Mitek, Raynham, MA) are looped through a suspension device (15-mm ENDOBUTTON; Smith & Nephew, Andover, MA) as an internal brace (Fig 2), and then the semitendinosus tendon and gracilis tendon are looped through and quadrupled into 4 strands. Both ends of tendons are stitched together for 6 loops using a whipstitch with a No. 2 ULTRABRAID suture (Smith & Nephew). The graft is trimmed to 8 mm in diameter. Notably, the stitched free ends of the tendon should be preserved as little as possible to prevent the ends from curling up when the graft is pulled into the tibia tunnel. The internal brace is incorporated into the 4-strand autograft (Fig 3).
Fig 2.
Two No. 2-0 OrthoCord sutures (DePuy Mitek, Raynham, MA) are looped through a suspension device (15 mm ENDOBUTTON; Smith & Nephew, Andover, MA) as internal brace.
Fig 3.
(A) The graft is trimmed to 8 mm. (B) The prepared graft with the internal brace (blue).
Portal Creation
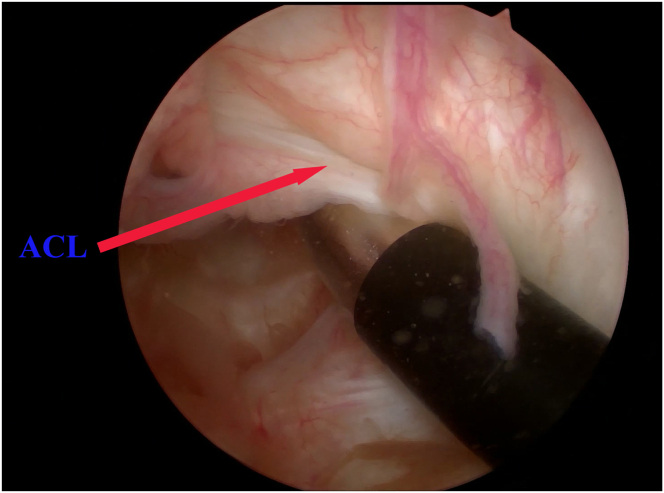
A standard anterolateral (AL) and anteromedial (AM) portal are established. Then, the anterior cruciate ligament (Fig 4) and meniscus are checked with arthroscopy. The PCL tear is confirmed by the posterior drawer test using a 30° arthroscope with the knee in 90° of flexion.
Fig 4.
The patient is placed supine, and his knee is in 90° of flexion. Pseudo-laxed anterior cruciate ligament in drawer test (anterolateral portal).
Femoral Tunnel Creation
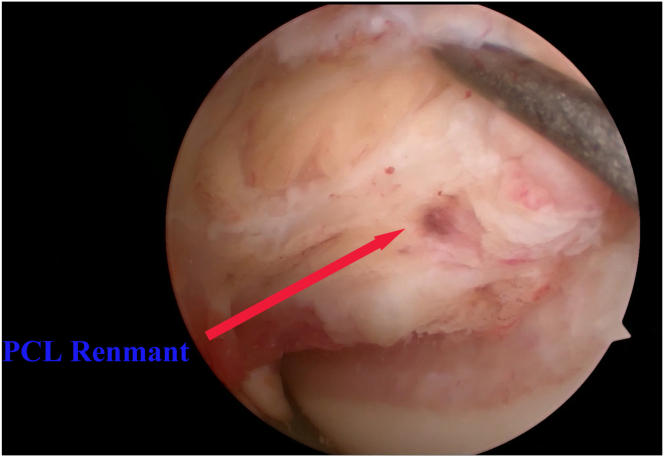
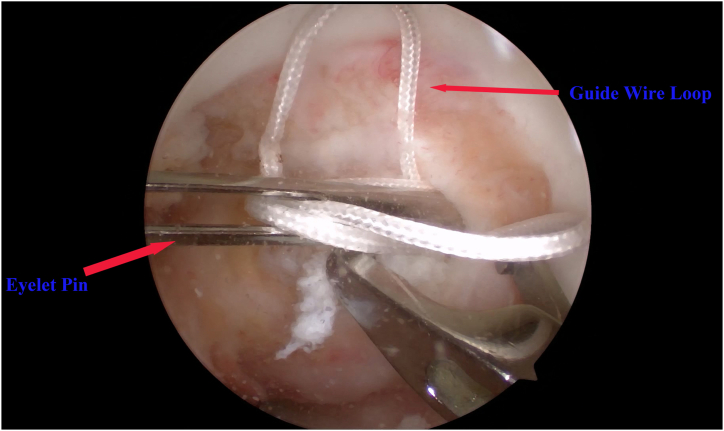
The femoral tunnel is drilled using an out-side in, retrograde technique. With the knee in 90° of flexion, the arthroscope is inserted via the AL portal, and the PCL remnant is separated and cauterized; care should be taken to minimize damage to the PCL remnant as much as possible (Fig 5). The femoral guide, set to l at an angle of 60° (FlipCutter drill guide system; Arthrex, Naples, FL), is inserted via the AM portal and targeted at the center of the footprint of the PCL remnant (Fig 6). The femoral guide is directed at the 1:30 clock face position on the right knee or 10:30 clock face position on the left knee of the medial femoral condyle. Then, the retro reamer is inserted into the guide sleeve and drilled into the joint space. After the retro reamer is drilled into the joint, the guide set is removed, and the guide sleeve is malleted to the bone. After confirming that the retro reamer tip can be flipped safely, create a tunnel for 30 mm and slide back the reamer after straightening the blade. Then, with the guide sleeve, a wire loop for graft passage is passed into the joint by an eyelet pin and pulled out via the AL portal (Fig 7).
Fig 5.
The patient is placed supine, and his knee is in 90° of flexion. The PCL remnant is preserved (anterolateral portal).
Fig 6.
The patient is placed supine, and his knee is in 90° of flexion. (A) The femoral guide set (FlipCutter drill guide system; Arthrex, Naples, FL) is inserted via anteromedial portal. (B) The femoral guide is directed at 1:30-o’clock position on the right knee (view of anterolateral portal).
Fig 7.
The patient is placed supine, and his knee is in 90° of flexion. With an eyelet pin, a wire loop is passed into joint space via femoral tunnel and pulled out via anterolateral portal (anterolateral portal).
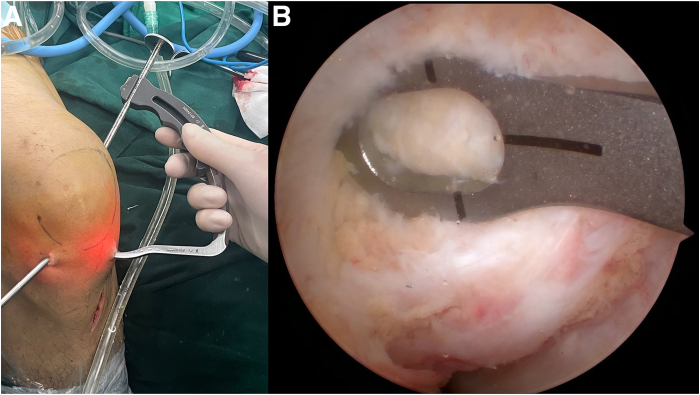
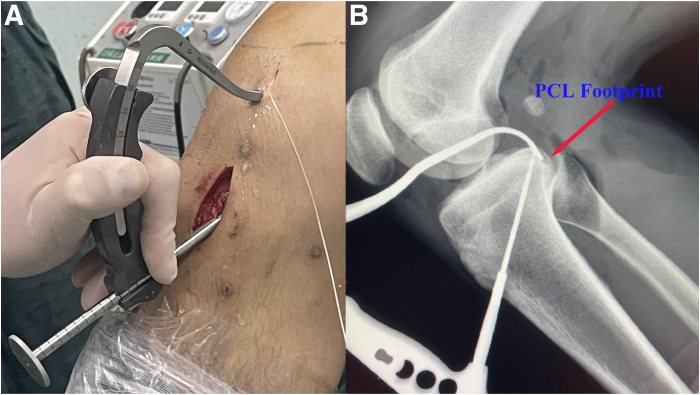
Tibia Tunnel Creation
The tibia tunnel is created using an appropriate guide system (Smith & Nephew). After a 3-cm incision is made medial proximal tibial for guide sleeve to reach the bone, the guide at an angle of 65° is inserted into joint space via the AM portal, and the guide pin is set approximately 10 to 12 mm below the joint line in the PCL facet to reduce the infusion of killer turn. Intraoperative radiography is used to confirm guide pin has been set in the proper location (Fig 8). A guide pin is drilled from anterior to the posterior and exited through the center of the PCL footprint, and then a cannulated reamer according to the graft diameter is drilled over the guide pin to create the tibial tunnel. Then, a wire loop is passed into with same procedure of the femoral tunnel.
Fig 8.
The patient is placed supine, and his knee is in 90° of flexion. (A) The guide system (Smith & Nephew; Andover, MA) at an angle of 65° is inserted into joint space via anteromedial portal. (B) A radiograph is used to confirm guide pin has set in proper location. (PCL, posterior cruciate ligament.)
Graft Passage and Transtibial Tubercle Fixation
The graft is passed into the joint via the AL portal (Fig 9) and first passed into the femoral tunnel with the aid of a prepassed wire loop and fixed by an Endobutton (Smith & Nephew). Then, the graft is passed into the tibia tunnel and cycled 20 times before tibial fixation to minimize graft elongation. With the knee in 70° flexion and an anterior drawer force applied, the graft is fixed in the tibial tunnel with an interference screw (Smith & Nephew) (Fig 10). An eyelet pin is used to drill transversely into the tibial tubercle, the suture tape internal brace is passed to the lateral side and fixed at tubercle independently, then the Ultrabraid sutures (Smith & Nephew) are passed and fixed in the same way (Fig 11).3 Finally check the graft with arthroscopy and perform a posterior drawer test (Fig 12).
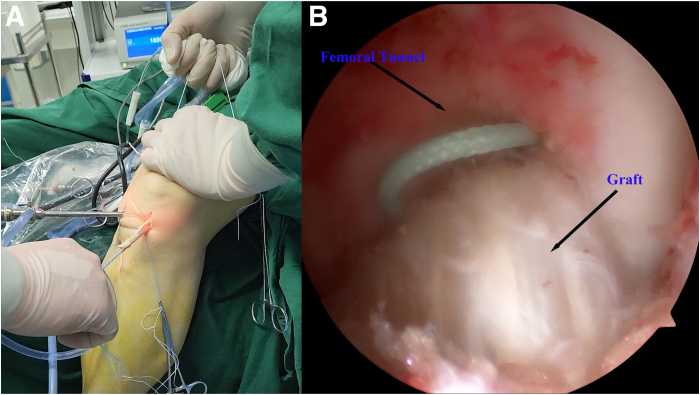
Fig 9.
(A) The graft is passed into femoral tunnel via anterolateral portal by pre-passed wire loop. (B) Confirm proper passage of the graft and ENDOBUTTON (Smith & Nephew) into the femoral tunnel through arthroscopy (anteromedial portal).
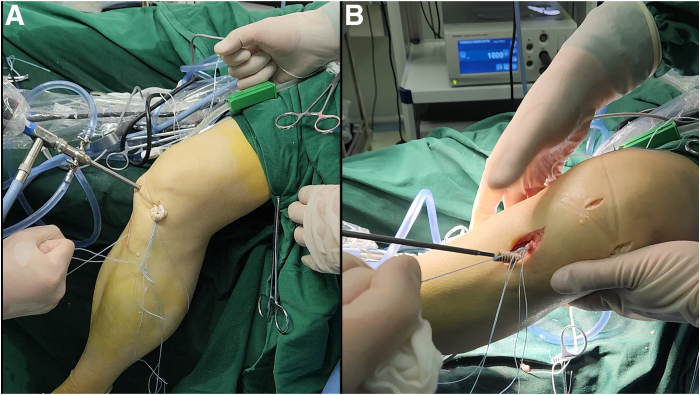
Fig 10.
(A) The graft is passed into tibia tunnel by pre-passed wire loop. (B) The graft is fixed by an interference screw (Smith & Nephew).
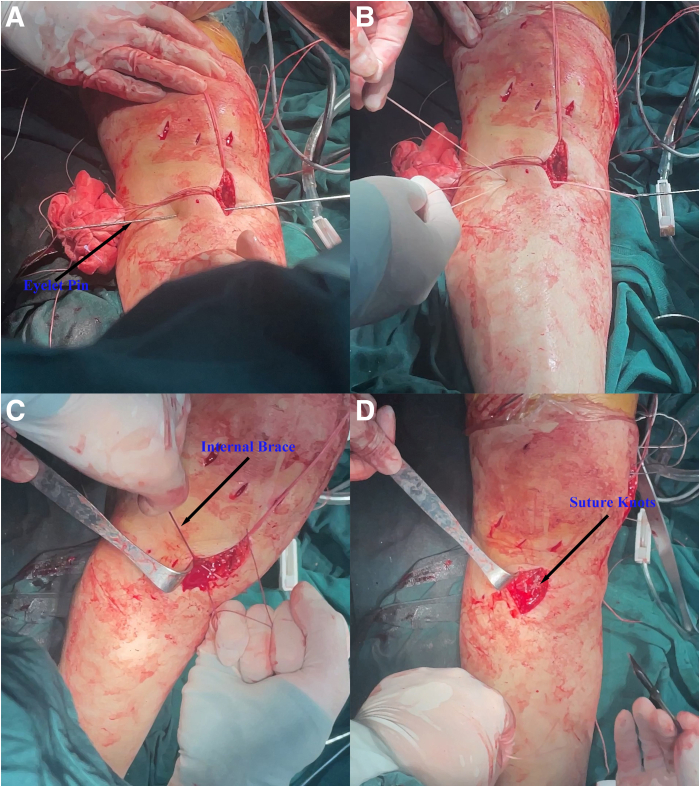
Fig 11.
(A) An eyelet pin is drilled transversely into the tibial tubercle. (B) The sutures are passed to the lateral side. (C) The internal brace is fixed independently. (D) The knots after transtibial tubercle fixation.
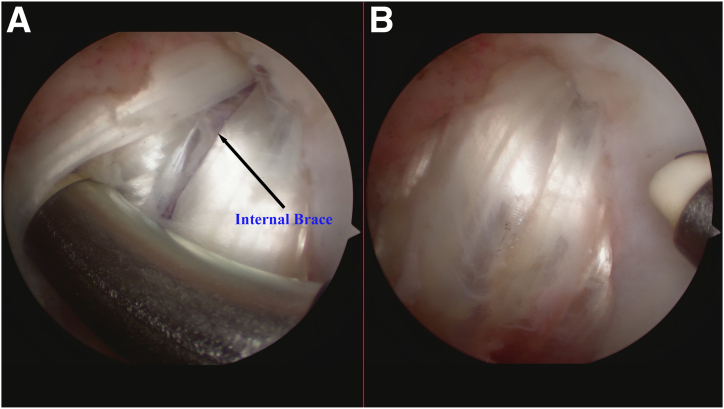
Fig 12.
The patient is placed supine, and his knee is in 90° of flexion. (A) The suture tape internal brace in graft. (B) Reconstructed posterior cruciate ligament is shown (anterolateral portal).
Rehabilitation
Quadriceps sets and straight-leg raises are preformed from day 1 postoperatively. Range-of-motion movements began on day 2 postoperatively; an increase of 30° in the range of motion is allowed every 2 weeks. Partial weight-bearing activities are allowed 4 weeks after surgery, and full weight-bearing activities at 8 weeks.
Discussion
In previous studies, using suture tape as internal brace to augment the graft has been demonstrated to be effective.4 After the graft is fixed, the graft needs time to remodel; in the remodeling phase, the biomechanical properties decline compared with initial implantation. Therefore, using independent suture tape to augment the graft results in lower elongation, greater ultimate load, and a reduction in the risk of graft failure during the ligamentization process.4, 5, 6 Compared with using an interference screw alone, using transtibial tubercle fixation as a supplement can improve ultimate failure load. In addition, compared with using metallic anchors, push-lock screws, and other supplementary fixation techniques, our technique needs no supplementary implants and therefore results in reduced medical costs.3,7 However, there are also risks to this technique; if the internal brace is tensioned excessively, it may constrain knee flexion and graft stress shielding.
In this technique, we also try to reduce the damage to the PCL remnant. The preserved remnant can act like a cushion pad to protect the graft from abrasion or attenuation as the result of a killer turn.8 Preserving the PCL remnant promotes vascular growth for graft healing, ligamentization, and the sensation for joint motion and position.9 The disadvantage of preserving the remnant is the poor visualization of the joint space, which requires additional surgical experience and longer time to master this technique.
The main purpose of this PCL reconstruction technique is using an augmented graft and supplementary fixation to reduce the risks of graft failure in the early stages of ligamentization, improve fixation stability, and start rehabilitation activities early to reduce influence on quadriceps strength and range of motion.
Disclosures
All authors (Y.W., H.L., S.C., H.Z.) declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. This work was financially supported by the Liaoning Applied Basic Research Program (No. 2023JH2/101300018); the National Natural Science Foundation of China (No. 8247090461); the Shenyang Sports Medicine Clinical Medical Research Center (L230117) and the Youth Science and Technology Talent Project of Shenyang (RC230857).
Supplementary Data
A single-bundle PCL reconstruction with suture tape augment and transtibial tubercle fixation is shown. The patient is positioned in the spine position, and a drawer test is performed to the injured knee and compared with the healthy side. A standard anterolateral and anteromedial portal are established. Via anterolateral portal, the anterior cruciate ligament, meniscus, and posterior ligament are checked, The drawer test is performed again; then, pseudo-laxed, the anterior ligament can be seen. The knee is positioned at 90° of flexion, and an oblique incision between the tibial tubercle and the posteromedial edge of tibia is made. The semitendinosus tendon and gracilis tendon are separated bluntly and harvested by a tendon stripper. Two No. 2-0 OrthoCord sutures are looped through a ENDOBUTTON as an internal brace, then the semitendinosus tendon and gracilis tendon are looped through and quadrupled into 4 strands. The graft is trimmed to 8 mm in diameter and stitched for 6 loops using whipstitch with a No. 2 Ultrabraid. Via the anterolateral portal, the PCL remnant is separated and cauterized minimally. A retrograde technique is used to drill femoral tunnel. The femoral guide, set at an angle of 60°, is inserted via anteromedial portal and located at the central of the footprint of the PCL. The femoral guide is directed at 1:30-o’clock position. The retro reamer is inserted into guide sleeve and drilled into joint space. After the retro reamer is drilled into the joint and the laser mark is exposed, the guide set is removed, and the guide sleeve is malleted to the bone. The reamer tip is flipped, and a 30-mm tunnel is made. The reamer is then removed and an eyelet pin with a wire loop for femoral passage is insert via guide sleeve. After making femoral tunnel, an incision is made on medial proximal tibial, the guide system at an angle of 65° is inserted via anteromedial portal, guide pin is set approximately 10 to 12 mm below the joint line on the PCL facet. A guide pin is drilled into joint space and an intraoperative radiograph is used to confirm guide pin has set in proper location. An 8-mm diameter cannulated reamer is drilled over the guide pin to create the tibial tunnel. Then, a wire loop is passed into with same procedure of femoral tunnel. The graft is passed into joint via the anterolateral portal and first passed into femoral tunnel with the aid of pre-passed wire loop and fixed by ENDOBUTTON. Then the graft is passed into tibia tunnel and cycled 20 times before tibial fixation to minimize graft elongation. With the knee in 70° flexion and an anterior drawer force applied, the graft is fixed in tibial tunnel with an interference screw. An eyelet pin is used to drill transversely into the tibial tubercle, and the suture tape internal brace is passed to the lateral side and fixed at tibial tubercle independently. Then, the ULTRABRAID suture is passed and fixed in the same way to fix the free ends of graft. Finally check the graft with arthroscopy and perform a posterior drawer test. (PCL, posterior cruciate ligament.)
References
- 1.EA Mackenzie C., Huntington L.S., Tulloch S. Suture tape augmentation of anterior cruciate ligament reconstruction increases biomechanical stability: A scoping review of biomechanical, animal, and clinical studies. Arthroscopy. 2022;38:2073–2089. doi: 10.1016/j.arthro.2021.12.036. [DOI] [PubMed] [Google Scholar]
- 2.Zhang H., Wang J., Gao Y., Zheng P., Gong L. Suture tape augmentation improves posterior stability after isolated posterior cruciate ligament reconstruction using hamstring tendon autograft with single-bundle transtibial technique. Arthroscopy. 2024;40:2045–2054. doi: 10.1016/j.arthro.2023.12.007. [DOI] [PubMed] [Google Scholar]
- 3.Duan M.Y., Sun R., Zhuang L.T., Zhang H.Z. Biomechanical evaluation of a novel transtibial posterior cruciate ligament reconstruction using high-strength sutures in a porcine bone model. Chin Med J (Engl) 2021;134:2316–2321. doi: 10.1097/CM9.0000000000001725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jackson G.R., Opara O., Tuthill T., et al. Suture augmentation in orthopaedic surgery offers improved time-zero biomechanics and promising short-term clinical outcomes. Arthroscopy. 2023;39:1357–1365. doi: 10.1016/j.arthro.2023.01.012. [DOI] [PubMed] [Google Scholar]
- 5.Pauzenberger L., Syré S., Schurz M. “Ligamentization” in hamstring tendon grafts after anterior cruciate ligament reconstruction: A systematic review of the literature and a glimpse into the future. Arthroscopy. 2013;29:1712–1721. doi: 10.1016/j.arthro.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 6.Root C., Braman M., Srinivas M., et al. Suture tape augmentation of posterior cruciate ligament reconstruction shows improved biomechanical stability with equivalent outcome and complication rates: A scoping review [published online March 25, 2024]. Arthroscopy. https://doi.org/10.1016/j.arthro.2024.03.025 [DOI] [PubMed]
- 7.Lee J.J., Otarodifard K., Jun B.J., McGarry M.H., Hatch G.F., Lee T.Q. Is supplementary fixation necessary in anterior cruciate ligament reconstructions? Am J Sports Med. 2011;39:360–365. doi: 10.1177/0363546510390434. [DOI] [PubMed] [Google Scholar]
- 8.Kopka M., Heard S.M., Buchko G.M., Hiemstra L.A., Lafave M.R., Kerslake S. Remnant-sparing anterior cruciate ligament reconstruction results in similar clinical, functional, and quality-of-life outcomes to anatomic single-bundle anterior cruciate ligament reconstruction. Arthrosc Sports Med Rehabil. 2024;6 doi: 10.1016/j.asmr.2024.100898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee D.W., Jang H.W., Lee Y.S., et al. Clinical, functional, and morphological evaluations of posterior cruciate ligament reconstruction with remnant preservation: Minimum 2-year follow-up. Am J Sports Med. 2014;42:1822–1831. doi: 10.1177/0363546514536680. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A single-bundle PCL reconstruction with suture tape augment and transtibial tubercle fixation is shown. The patient is positioned in the spine position, and a drawer test is performed to the injured knee and compared with the healthy side. A standard anterolateral and anteromedial portal are established. Via anterolateral portal, the anterior cruciate ligament, meniscus, and posterior ligament are checked, The drawer test is performed again; then, pseudo-laxed, the anterior ligament can be seen. The knee is positioned at 90° of flexion, and an oblique incision between the tibial tubercle and the posteromedial edge of tibia is made. The semitendinosus tendon and gracilis tendon are separated bluntly and harvested by a tendon stripper. Two No. 2-0 OrthoCord sutures are looped through a ENDOBUTTON as an internal brace, then the semitendinosus tendon and gracilis tendon are looped through and quadrupled into 4 strands. The graft is trimmed to 8 mm in diameter and stitched for 6 loops using whipstitch with a No. 2 Ultrabraid. Via the anterolateral portal, the PCL remnant is separated and cauterized minimally. A retrograde technique is used to drill femoral tunnel. The femoral guide, set at an angle of 60°, is inserted via anteromedial portal and located at the central of the footprint of the PCL. The femoral guide is directed at 1:30-o’clock position. The retro reamer is inserted into guide sleeve and drilled into joint space. After the retro reamer is drilled into the joint and the laser mark is exposed, the guide set is removed, and the guide sleeve is malleted to the bone. The reamer tip is flipped, and a 30-mm tunnel is made. The reamer is then removed and an eyelet pin with a wire loop for femoral passage is insert via guide sleeve. After making femoral tunnel, an incision is made on medial proximal tibial, the guide system at an angle of 65° is inserted via anteromedial portal, guide pin is set approximately 10 to 12 mm below the joint line on the PCL facet. A guide pin is drilled into joint space and an intraoperative radiograph is used to confirm guide pin has set in proper location. An 8-mm diameter cannulated reamer is drilled over the guide pin to create the tibial tunnel. Then, a wire loop is passed into with same procedure of femoral tunnel. The graft is passed into joint via the anterolateral portal and first passed into femoral tunnel with the aid of pre-passed wire loop and fixed by ENDOBUTTON. Then the graft is passed into tibia tunnel and cycled 20 times before tibial fixation to minimize graft elongation. With the knee in 70° flexion and an anterior drawer force applied, the graft is fixed in tibial tunnel with an interference screw. An eyelet pin is used to drill transversely into the tibial tubercle, and the suture tape internal brace is passed to the lateral side and fixed at tibial tubercle independently. Then, the ULTRABRAID suture is passed and fixed in the same way to fix the free ends of graft. Finally check the graft with arthroscopy and perform a posterior drawer test. (PCL, posterior cruciate ligament.)