Abstract
Background:
Flexible flatfoot is a normal finding in infants and the arch is shaped spontaneously in most children before the age of 10 years. Flexible flatfoot is a common deformity in both adolescent and adult populations.
Objective:
This prospective study aims to assess the functional and radiological outcomes of subtalar arthroereisis in adolescent patients with symptomatic flexible flatfoot.
Methods:
This is a prospective study and included 26 feet in 19 patients who underwent subtalar arthroereisis for symptomatic flexible flatfeet deformity. Preoperative and postoperative functional assessment based on the American Orthopedic Foot and Ankle Society (AOFAS) hindfoot scale. Radiographic parameters included preoperative and postoperative Kite`s angle, talonavicular coverage angle, Anterior-Posterior talo-1st metatarsal angle, Meary`s angle, talar declination angle, calcaneal inclination angle and lateral talocalcaneal angle.
Results:
The mean follow-up period was 22.5±9.4 months and the mean preoperative AOFAS score was 54.6±6.0, while the mean AOFAS score at the last follow-up visit was 86.3±3.9 (P<0.001).The mean preoperative and postoperative radiological measurements were 19.0°±8.2° and 7.4°±3.9° for the AP Talo-1st metatarsal angle (P<0.001); 23.6°±9.1° and 8.0°±4.0° for talonavicular coverage angle (P<0.001); 35.4°±3.7° and 24.1°±3.4° for Kite`s angle (P<0.003); 22.4°±6.1° and 7.5°±3.7° for Meary`s angle (P<0.001); 41.0°±4.4° and 25.2°±7.1° for talar declination angle (P<0.001); 13.5°±3.7° and 21.3°±3.6° for calcaneal inclination angle (P<0.001) and 52.4°±7.2° and 42.9°±4.8° for lateral talocalcaneal angle (P<0.041) respectively.
Conclusion:
Subtalar arthroereisis is an effective and minimally invasive procedure that showed clinical and radiological improvement for symptomatic flexible flatfoot in our study group.
Keywords: Arthroereisis, flexible Flatfoot, pesplanovalgus, sinus tarsi implant
1. BACKGROUND
The term flatfoot is generally used to describe a foot deformity with loss or decrease of the medial longitudinal arch, eversion of the heel and forefoot abduction (1). So it is a three-dimensional deformity with subtalar joint external rotation, midfoot abduction and forefoot supination in relation to the hindfoot (1,2)
Flexible flatfoot is a normal finding in infants and the arch is shaped spontaneously in most children before age of 10 years (3-5). Flexible flatfoot is a common deformity in both adolescents and adults (6,7).
Staheli divided flatfoot into two groups, physiologic and pathologic flatfoot, in the flexible (physiologic, hypermobile) flatfoot, the arch collapses during weight bearing, but it appears with tiptoeing or dorsiflexion of the big toe, in contrast to pathologic (rigid, fixed) flatfoot (5,8).
There are two principal theories for the pathogenesis of flexible flatfoot, the first one explains this deformity by muscle weakness in the foot and ankle (9), and this theory was weakened by later electromyographic studies (10).
The second theory is bone-ligament complex integrity, in which the shape of bones and the strength and flexibility of the ligaments are needed to maintain the longitudinal arch, with excessive ligamentous laxity as the primary pathology (11).
Mann and Inman confirmed that intrinsic muscle activity is necessary for arch support during propulsion, but not in the static phase (12).
There is a controversy about the risk factors that may be associated with flexible flatfoot which include obesity (13) and hyperlaxity of the ligaments that causes hypermobility of the joints with excessive eversion motion at the subtalar joint (14).
Various treatment methods have been defined for symptomatic flexible flatfoot, these methods are divided into conservative and surgical procedures (7). Conservative treatment includes shoe modification, analgesia, braces, and physiotherapy (15).
Surgical treatment is indicated after failure of conservative management and can be categorized into tendon lengthening and transfer, osteotomies, arthrodesis of one or more joints and subtalar arthroereisis (7,16-19).
Soft tissue procedure alone is not sufficient in most cases and usually, it is accompanied by bony procedure(s)(7). There are different osteotomy techniques such as medial shift calcaneus osteotomy, lateral column lengthening osteotomy and dorsal open wedge medial cuneiform osteotomy (20,21).
These osteotomies in flexible flatfoot correct the deformity but it does not change the excessive eversion at the subtalar joint and usually need a long time to recover and there is a risk of nonunion (22,23).
Subtalar arthroereisis refers to the use of a subtalar implant to decrease excessive eversion and overpronation at the subtalar joint (2,18,19,23-26), previously these implants were bone grafts (27), currently, there are special implants designed for this purpose.
The advantages of this procedure include fast recovery, minimally invasive, three-dimensional correction, low infection rate and can be reverted by removal of implants (19,28).
Contraindications for this procedure are rigid flatfoot, infection at the surgical site, and subtalar arthritis (29,30).
One of the most common complications of this procedure is sinus tarsi pain (31), which is reported at different rates in different studies, and may require implant removal (25).
2. OBJECTIVE
The purposes of this study are to evaluate the functional and radiological outcomes in adolescent patients with flexible flatfoot treated by subtalar arthroereisis and document the complications of this procedure in this group of patients.
3. PATIENTS AND METHODS
The study included 26 feet (12 right, 14 left) in 19 patients (12 Females, 7 males) treated by subtalar arthroereisis for symptomatic flexible flatfoot deformity in our institution between July 2020 and January 2023.
Inclusion criteria were patients with symptomatic flexible flatfoot deformity between the ages 14 and 19 years at the time of operation, that did not respond to conservative management such as orthosis, analgesia and physiotherapy for at least 6 months. Patients complained of pain in the midfoot, hindfoot or calf during standing or walking and also complained of difficulty wearing shoes.
Patients who had flexible flatfoot deformity with previous surgery for flatfoot or secondary to a congenital condition, accessory navicular, trauma, genetic syndromes and neuromuscular disease, were excluded.
Table 1 summarizes the socio-demographic characteristics of the study population.
Table 1. Socio-demographic characteristics of the study population.
| Gender, n (%) | |
| Male Female |
12 (63.2) 7 (36.8) |
| Age, years, mean ± SD (range) | 15.3±1.4 (14-19) |
| Follow-up period/month, mean ± SD (range) | 22.5±9.4 (10-36) |
| Number of patients (feet) | 19 (26) |
| Operated foot, n (%) | |
| Right Left |
12 (46.2) 14 (53.8) |
| Family history, n (%) | |
| No yes |
5 (26.3) 14 (73.7) |
The clinical evaluation pre and postoperatively was based on the American Orthopedic Foot and Ankle Society (AOFAS) hindfoot score (32). This scale mainly consists of three aspects: pain, function and alignment and it had a maximum of 100 points. A mark of less than 50 is considered poor, 50-74 is fair, 75-89 is good and 90-100 is excellent.
Radiographic evaluation:
For radiographic assessment, the patients had pre and postoperative weight-bearing foot X-rays with two views, dorsoplantar (DP) and lateral views. The analysis was done by Picture Archiving and Communication System (PACS) and the following measurements were done:
On lateral view: Figure 1 shows these measurements on the lateral view
Figure 1. The angle formed between illustrated lines is for Meary`s angle (A), the talar declination angle (B), the lateral talocalcaneal angle (C) and the calcaneal inclination angle (D).

* The Calcaneal Inclination Angle:
Defined as the angle formed between a line parallel to the floor and a line connecting the two most inferior points of the calcaneus, normal values (20°-30°).
*. The Meary`s angle: the angle between the longitudinal axis of the talus and the longitudinal axis of the first metatarsal, normal values (0-5°)
* The lateral talocalcaneal angle: the angle formed between the longitudinal axis of the talus and the line connecting the most inferior points of the calcaneus, normal values (25°-40°).
* The Talar declination angle: the angle between the longitudinal axis of the talus and the line parallel to the supporting floor, normal values (15°-25°).
On dorsoplantar view: Figure 2 shows these angles
Figure 2. The angle formed between illustrated lines is for the talo-1st metatarsal angle (A), the talonavicular coverage angle (B) and Kite`s angle (C).

* AP talo-1st metatarsal angle (AP talo-1st metatarsal angle): defined as the angle between the longitudinal axis of the talus and the longitudinal axis of the first metatarsal, normal values (0-6°).
* Talonavicular coverage angle: the angle between the articular surface of the talar head and the articular surface of the navicular bone, with normal values less than 7°.
* Kite’s angle: the angle between the longitudinal axis of the talus and the longitudinal axis of the calcaneus, normal values (25°-40°).
Postoperative complications were recorded and included sinus tarsi pain and infection.
The study was conducted in accordance with the ethical guidelines of the Declaration of Helsinki and informed consent was obtained from all the patients.
Prosthesis: Talar fit implants were used, 15 screws were Prostop (Arthrex, Naples, FL, USA) and 11 screws were subtalar screws (ChM, Bialystock, Poland).
Surgical technique: All patients were operated on at our institution by the same foot and ankle surgeon.
The patient was supine with an ipsilateral hip sandbag and tourniquet. the soft spot at the sinus tarsi just distal to the tip of the fibula was palpated, a 1-2 cm incision was made, deep dissection was blunt by hemostat, and the guidewire from anterolateral to posteromedial was inserted in the sinus tarsi. Trial testers with gradual increments in diameter were inserted under fluoroscopic guidance on the guidewire to choose the most suitable implant size by assessment of the subtalar motion and the purchase grip of the tester. Then the final implant with the appropriate size was inserted under fluoroscopic guidance. The incision was closed routinely. No other procedures were added.
Figure 3 is for a postoperative weight-bearing x-ray of a patient at week 12 and figure 4 is for a clinical picture of the same patient pre and postoperative.
Figure 3. Weight-bearing postoperative x-ray.
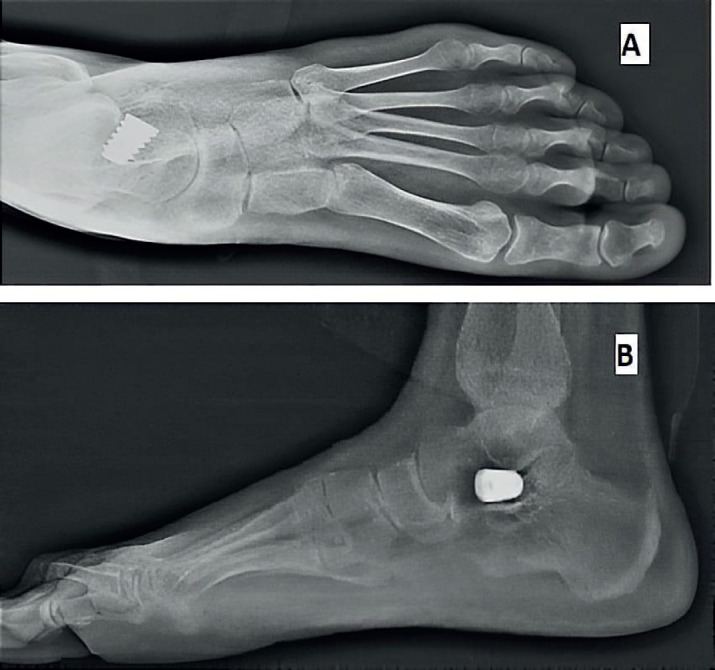
Figure 4. A clinical picture of pre and postoperative of the patient treated by subtalar arthroereisis showing correction of the forefoot abduction and heel valgus deformities.

The patient was discharged home on the same day and kept in a non-walking cast for 4 weeks, then the cast was removed and the patient started weight bearing as tolerated.
Statistical analysis
Statistical analysis was performed using SPSS v20.0 software (SPSS Inc., Chicago, IL, USA). Descriptive statistics analysis was performed to calculate Means and standard deviations. A paired sample’s t-test was used to compare means, and a P-value of 0.05 was considered statistically significant.
4. RESULTS
The study included 19 patients with 26 feet, 12 were male and 7 were female, the evaluated feet were 12 right and 14 left. The mean age was 15.3±1.4 (range, 14-19) years and the mean follow-up was 22.5±9.4 (range, 10-36) months. 1st-degree family history of flatfoot was positive in 14 patients (73.7%).
The mean preoperative AOFAS score was 54.6±6.0 (range, 40-67), while the mean AOFAS score at the last follow-up visit was 86.3±3.9 (range, 77-92) (P<0.001).
All radiographic angles improved significantly, the mean AP talo-1st metatarsal angles were 19.0°±8.2° (range, 6°-36°) degrees preoperatively and improved to 7.4°±3.9° (range, 0°-16°) degrees postoperatively (P<0.001). The mean preoperative and postoperative talonavicular angles were 23.6°±9.1° (range, 12°-48°) and 8.0°±4.0° (range, 3°-20°) respectively (P<0.001). The mean preoperative and postoperative Kite`s angles were 35.4°±3.7° (range, 28°-42°) and 24.1°±3.4° (range, 18°-30°) respectively (P<0.003).
The mean preoperative and postoperative Meary`s angles were 22.4°±6.1° (range, 12°-35°) and 7.5°±3.7° (range, 2°-16°) respectively (P<0.001), the mean preoperative and postoperative talar declination angles were 41.0°±4.4° (range, 30°-49°) and 25.2°±7.1° (range, 12°-38°) respectively (P<0.001).
The mean preoperative and postoperative calcaneal inclination angles were 13.5°±3.7° (range, 5°-19°) and 21.3°±3.6° (range, 10°-30°) respectively (P<0.001), the mean preoperative and postoperative lateral talocalcaneal angles were 52.4°±7.2° (range, 35°-65°) and 42.9°±4.8° (range, 31°-51°) respectively (P<0.041).
Table 2 summarizes the statistical results of the variables in the current study.
Table 2. Statistical results of the variables in the current study.
| Variable | Preoperative | Postoperative | p.value |
|---|---|---|---|
| AOFAS | |||
| Mean ± SD Range |
54.6±6.0 40-67 |
86.3±3.9 77-92 |
<0.001 |
| AP talo-1st metatarsal angle | |||
| Mean ± SD Range |
19.0±8.2 6-36 |
7.4±3.9 0-16 |
<0.001 |
| Talonavicular angle | |||
| Mean ± SD Range |
23.6±9.1 12-48 |
8.0±4.0 3-20 |
<0.001 |
| Meary`s angle | |||
| Mean ± SD Range |
22.4±6.1 12-35 |
7.5±3.7 2-16 |
<0.001 |
| Kite`s angle | |||
| Mean ± SD Range |
35.4±3.7 28-42 |
24.1±3.4 18-30 |
0.003 |
| Talar declination angle | |||
| Mean ± SD Range |
41.0±4.4 30-49 |
25.2±7.1 12-38 |
<0.001 |
| Calcaneal inclination angle | |||
| Mean ± SD Range |
13.5±3.7 5-19 |
21.3±3.6 10-30 |
<0.001 |
| Lateral talocalcaneal angle | |||
| Mean ± SD Range |
52.4±7.2 35-65 |
42.9±4.8 31-51 |
0.041 |
Sinus tarsi pain occurred in two feet (7.7%) and was treated with nonsteroidal anti-inflammatory drugs for two weeks, without implant removal and did not affect patients’ daily activities, another foot developed a surgical site infection treated with antibiotics and regular dressings. In this study, no patient necessitated implant removal for any reason in the follow-up period.
5. DISCUSSION
There are a lot of controversies in the literature about the surgical options for the treatment of symptomatic flexible flatfoot, these treatments include soft tissue procedures, osteotomies, arthrodesis and arthroereisis (7, 14, 16-19) (interposition of bone or special implants into the sinus tarsi).
Arthroereisis was introduced in 1946 by the insertion of a bone block in the sinus tarsi to decrease excessive subtalar eversion (27), the bone block might undergo resorption with recurrent deformity or might cause pseudoarthrosis and pain.
Arthroereisis by special implants was introduced later on with a variety of implants and different surgical techniques (33,34). This procedure allows quick recovery and less pain in comparison to other surgical procedures (19,28). Other advantages include the small surgical wound, minimally invasive technique, low infection risk, preserving bone and cartilage, the simplicity of the procedure, can be combined with other added procedures if needed, and the possibility for implant removal, if required, with a full and painless range of motion at the subtalar joint after removal (25,35).
Patients with symptomatic flexible flatfoot usually complain of medial foot pain, the clinical improvement post subtalar arthroereisis may be due to the effect of the implant that redistributes the forces toward normal and decreases the load on the medial column of the foot (2,36). In their study with a biomedical model, Arangio et al found that there is a force shifting to the medial column in flatfoot deformity, and subtalar arthroereisis with 6 mm substantially reduced these forces to normal (2).
Moreover, Franz et al in their study about the effects on pedobarographic outcome post subtalar arthroereisis on 39 patients with juvenile flexible flatfoot reported that arthroereisis induces medial to lateral load shift under the mid and forefoot (36).
In the current study, the clinical outcome as measured by the AOFAS hindfoot scale significantly improved postoperatively, as the mean increased from 54.6±6.0 preoperatively to 86.3±3.9 postoperatively (P<0.001), a similar finding was reached by other studies, as Wang et al reported improvement in AOFAS from 55.5 preoperatively to 86.3 postoperatively in 46 feet for 31 children and adolescents treated with subtalar arthroereisis (24). Also, this improvement was observed in the study performed by Needleman et al, as the AOFAS score increased from 52 preoperatively to 87 postoperatively (19).
There are also other studies that showed improvement in the AOFAS hindfoot scale post subtalar arthroereisis (25,37).
Regarding radiographic outcomes in the current study, we observed a significant improvement in the talar declination angle, Meary`s angle, calcaneus inclination angle, lateral talocalcaneal angle, AP talo-1st metatarsal angler, Kite`s angle and talonavicular coverage angle.
Similarly, Megremis et al in their study on 14 patients with 28 symptomatic flatfeet treated by subtalar arthroereisis combined with percutaneous Achilles lengthening, found a radiographic improvement as the Meary`s angle, Kite`s angle, talus declination angle and talonavicular coverage angle were significantly improved postoperatively, whereas the calcaneal inclination angle was slightly improved, which means slightly restoration of the medial arch (38).
Furthermore, in a retrospective study conducted by Indiano et al for the effectiveness of subtalar arthroereisis for pediatric flexible flatfoot with follow-up till skeletal maturity, their study included 112 feet, they noticed an improvement in radiographic parameters (lateral talocalcaneal angle, calcaneal inclination angle, Meary’s angle, anteroposterior talonavicular angle, talonavicular uncoverage percent) of the foot in pediatric flexible flatfoot and giving satisfactory outcomes at the end of skeletal maturity (39). This radiographic improvement has also been reported in other studies (26,40).
Overall these findings are in accordance with findings reported by Inn Tan et al in a systemic review and meta-analysis of the outcomes of subtalar arthroereisis in symptomatic flexible flatfoot, which included 17 publications and 1563 feet, they found that subtalar arthroereisis could mitigate pain and correct radiological abnormalities (Meary`s angle, calcaneal inclination angle, kite`s angle and lateral talocalcaneal angle) (31).
However, there are different complications reported for subtalar arthroereisis, the most frequent one is sinus tarsi pain, the incidence of this complication is widely different among many studies, and it varies from 3% to 40% (24,31,41). The cause of postoperative sinus tarsi pain is multifactorial and not fully understood. The explanation for this pain includes overcorrection, under-correction, soft tissue irritation and impingement between the implant and posterior subtalar articular surfaces (24,43).
Treatment of postoperative sinus tarsi pain starts with non-steroidal anti-inflammatory drugs, local cold immersions and physiotherapy, and in refractory cases, it may require implant removal (31,42).
Other complications, that it is reported in the literature for this procedure, are wound infection, under-correction, subtalar arthritis, overcorrection, broken metal, fracture and implant migration (31).
In the current study, sinus tarsi pain occurred in two feet (7.7%), treated by oral non-steroidal anti-inflammatory drugs for a couple of weeks with local ice, the patient’s symptoms improved and no limitation to daily activity or sports occurred, also no need for implant removal.
Another complication that occurred in one foot was wound infection in the second week postoperatively, treated with simple debridement, regular dressings and antibiotics, not necessitated implant removal. No other complications have been reported in our study.
The limitations of this study include the small sample size, lack of a control group, measurement bias and the short-term follow-up for the patients.
Nevertheless, many studies performed with a small number of patients showed clinical and radiological improvement. In future studies, the number of patients and the follow-up periods can be increased. We believe that our study will add to other studies in the literature on the treatment of symptomatic flexible flatfoot in adolescents.
6. CONCLUSION
In conclusion, subtalar arthroereisis is an effective, minimally invasive and easy procedure for treatment of symptomatic flexible flatfoot in adolescents with good clinical and radiological outcomes in our study group.
Ethics approval and consent to participate:
Ethical approval was obtained from the University Research Committee of the Jordan University of Science and Technology; the number is (700-2021). Consent forms were obtained from all participants.
Availability of data and materials:
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Author’s contribution:
MA Corresponding author participated in study design, review of the literature, writing the manuscript. AR participated in the study design and review of the literature. SBE participated in the study design. MK participated in statistical analysis. AY, MA, YA and JA participated in the clinical data collection from the patients. NO, HA and JA participated in the radiological evaluation.
Conflict of interest:
The authors declare that they have no competing interests.
Financial support and sponsorship:
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
REFERENCES
- 1.Michaudet C, Edenfield KM, Nicolette GW, Carek PJ. Foot and Ankle Conditions: Pes Planus. FP Essent. 2018;465:18–23. [PubMed] [Google Scholar]
- 2.Arangio GA, Reinert KL, Salathe EP. A biomechanical model of the effect of subtalar arthroereisis on the adult flexible flat foot. Clin Biomech (Bristol, Avon) 2004;19(8):847–852. doi: 10.1016/j.clinbiomech.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Gould N, Moreland M, Alvarez R, Trevino S, Fenwick J. Development of the child's arch. Foot Ankle. 1989;9(5):241–245. doi: 10.1177/107110078900900506. [DOI] [PubMed] [Google Scholar]
- 4.Tong JW, Kong PW. Medial Longitudinal Arch Development of Children Aged 7 to 9 Years: Longitudinal Investigation. Phys Ther. 2016;96(8):1216–1224. doi: 10.2522/ptj.20150192. [DOI] [PubMed] [Google Scholar]
- 5.Staheli LT, Chew DE, Corbett M. The longitudinal arch. A survey of eight hundred and eighty-two feet in normal children and adults. J Bone Joint Surg Am. 1987;69(3):426–428. [PubMed] [Google Scholar]
- 6.Benedetti MG, Ceccarelli F, Berti L, et al. Diagnosis of flexible flatfoot in children: a systematic clinical approach. Orthopedics. 2011;34(2):94. doi: 10.3928/01477447-20101221-04. Published 2011 Jan 1. [DOI] [PubMed] [Google Scholar]
- 7.Mosca VS. Flexible flatfoot in children and adolescents. J Child Orthop. 2010;4(2):107–121. doi: 10.1007/s11832-010-0239-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Staheli LT. Evaluation of planovalgus foot deformities with special reference to the natural history. J Am Podiatr Med Assoc. 1987;77(1):2–6. doi: 10.7547/87507315-77-1-2. [DOI] [PubMed] [Google Scholar]
- 9.Jones Russell. The human foot. An experimental study of its mechanics, and the role of its muscles and ligaments in the support of the arch. American Journal of Anatomy. 1941;68:1–39. doi: 10.1002/aja.1000680102. [DOI] [Google Scholar]
- 10.BASMAJIAN JV, STECKO G. THE ROLE OF MUSCLES IN ARCH SUPPORT OF THE FOOT. J Bone Joint Surg Am. 1963;45:1184–1190. [PubMed] [Google Scholar]
- 11.HARRIS RI, BEATH T. Hypermobile flat-foot with short tendo achillis. J Bone Joint Surg Am. 1948;30A(1):116–140. [PubMed] [Google Scholar]
- 12.MANN R, INMAN VT. PHASIC ACTIVITY OF INTRINSIC MUSCLES OF THE FOOT. J Bone Joint Surg Am. 1964;46:469–481. [PubMed] [Google Scholar]
- 13.Pourghasem M, Kamali N, Farsi M, Soltanpour N. Prevalence of flatfoot among school students and its relationship with BMI. Acta Orthop Traumatol Turc. 2016;50(5):554–557. doi: 10.1016/j.aott.2016.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bordelon RL. Hypermobile flatfoot in children. Comprehension, evaluation, and treatment. Clin Orthop Relat Res. 1983;(181):7–14. [PubMed] [Google Scholar]
- 15.Basta N.W, Mital M.A, Bonadio O, et al. A comparative study of the role of shoes, arch supports, and navicular cookies in the management of symptomatic mobile flat feet in children. International Orthopaedics. 1977;1:143–148. doi: 10.1007/BF00576318. [DOI] [Google Scholar]
- 16.McCall RE, Lillich JS, Harris JR, Johnston FA. The Grice extraarticular subtalar arthrodesis: a clinical review. J Pediatr Orthop. 1985;5(4):442–445. doi: 10.1097/01241398-198507000-00011. [DOI] [PubMed] [Google Scholar]
- 17.Saltzman CL, Fehrle MJ, Cooper RR, Spencer EC, Ponseti IV. Triple arthrodesis: twenty-five and forty-four-year average follow-up of the same patients. J Bone Joint Surg Am. 1999;81(10):1391–1402. [PubMed] [Google Scholar]
- 18.Lanham RH Jr. Indications and complications of arthroereisis in hypermobile flatfoot. J Am Podiatry Assoc. 1979;69(3):178–185. doi: 10.7547/87507315-69-3-178. [DOI] [PubMed] [Google Scholar]
- 19.Needleman RL. Current topic review: subtalar arthroereisis for the correction of flexible flatfoot. Foot Ankle Int. 2005;26(4):336–346. doi: 10.1177/107110070502600411. [DOI] [PubMed] [Google Scholar]
- 20.Kim JR, Shin SJ, Wang SI, Kang SM. Comparison of lateral opening wedge calcaneal osteotomy and medial calcaneal sliding-opening wedge cuboid-closing wedge cuneiform osteotomy for correction of planovalgus foot deformity in children. J Foot Ankle Surg. 2013;52(2):162–166. doi: 10.1053/j.jfas.2012.12.007. [DOI] [PubMed] [Google Scholar]
- 21.Sangeorzan BJ, Mosca V, Hansen ST Jr. Effect of calcaneal lengthening on relationships among the hindfoot, midfoot, and forefoot. Foot Ankle. 1993;14(3):136–141. doi: 10.1177/107110079301400305. [DOI] [PubMed] [Google Scholar]
- 22.Jara ME. Evans Osteotomy Complications. Foot Ankle Clin. 2017;22(3):573–585. doi: 10.1016/j.fcl.2017.04.006. [DOI] [PubMed] [Google Scholar]
- 23.Li B, He W, Yu G, et al. Treatment for Flexible Flatfoot in Children With Subtalar Arthroereisis and Soft Tissue Procedures. Front Pediatr. 2021;9:656178. doi: 10.3389/fped.2021.656178. Published 2021 May 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang S, Chen L, Yu J, et al. Mid-term Results of Subtalar Arthroereisis with Talar-Fit Implant in Pediatric Flexible Flatfoot and Identifying the Effects of Adjunctive Procedures and Risk Factors for Sinus Tarsi Pain. Orthop Surg. 2021;13(1):175–184. doi: 10.1111/os.12864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ozan F, Doğar F, Gençer K, et al. Symptomatic flexible flatfoot in adults: subtalar arthroereisis. Ther Clin Risk Manag. 2015;11:1597–1602. doi: 10.2147/TCRM.S90649. Published 2015 Oct 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Scharer BM, Black BE, Sockrider N. Treatment of painful pediatric flatfoot with Maxwell-Brancheau subtalar arthroereisis implant a retrospective radiographic review. Foot Ankle Spec. 2010;3(2):67–72. doi: 10.1177/1938640010362262. [DOI] [PubMed] [Google Scholar]
- 27.CHAMBERS EF. An operation for the correction of flexible flat feet of adolescents. West J Surg Obstet Gynecol. 1946;54:77–86. [PubMed] [Google Scholar]
- 28.Brancheau SP, Walker KM, Northcutt DR. An analysis of outcomes after use of the Maxwell-Brancheau Arthroereisis implant. J Foot Ankle Surg. 2012;51(1):3–8. doi: 10.1053/j.jfas.2011.10.019. [DOI] [PubMed] [Google Scholar]
- 29.Schon LC. Subtalar arthroereisis: a new exploration of an old concept. Foot Ankle Clin. 2007;12(2):329–vii. doi: 10.1016/j.fcl.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 30.Needleman RL. A surgical approach for flexible flatfeet in adults including a subtalar arthroereisis with the MBA sinus tarsi implant. Foot Ankle Int. 2006;27(1):9–18. doi: 10.1177/107110070602700103. [DOI] [PubMed] [Google Scholar]
- 31.Tan JHI, Tan SHS, Lim AKS, Hui JH. The outcomes of subtalar arthroereisis in pes planus: a systemic review and meta-analysis. Arch Orthop Trauma Surg. 2021;141(5):761–773. doi: 10.1007/s00402-020-03458-8. [DOI] [PubMed] [Google Scholar]
- 32.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 33.Graham ME, Jawrani NT. Extraosseous talotarsal stabilization devices: a new classification system. J Foot Ankle Surg. 2012;51(5):613–619. doi: 10.1053/j.jfas.2012.05.030. [DOI] [PubMed] [Google Scholar]
- 34.Vescio A, Testa G, Amico M, et al. Arthroereisis in juvenile flexible flatfoot: Which device should we implant? A systematic review of literature published in the last 5 years. World J Orthop. 2021;12(6):433–444. doi: 10.5312/wjo.v12.i6.433. Published 2021 Jun 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chong DY, Macwilliams BA, Hennessey TA, Teske N, Stevens PM. Prospective comparison of subtalar arthroereisis with lateral column lengthening for painful flatfeet. J Pediatr Orthop B. 2015;24(4):345–353. doi: 10.1097/BPB.0000000000000179. [DOI] [PubMed] [Google Scholar]
- 36.Franz A, Herz D, Raabe J, Seeberger U, Bollmann C. Pedobarographic outcome after subtalar screw arthroereisis in flexible juvenile flatfoot. Foot Ankle Surg. 2021;27(4):389–394. doi: 10.1016/j.fas.2020.05.003. [DOI] [PubMed] [Google Scholar]
- 37.García Bistolfi M, Avanzi R, Buljubasich M, Bosio S, Puigdevall M. Subtalar arthroereisis in pediatric flexible flat foot: Functional and radiographic results with 5 years of average follow-up. Foot (Edinb) 2022;52:101920. doi: 10.1016/j.foot.2022.101920. [DOI] [PubMed] [Google Scholar]
- 38.Megremis P, Megremis O. Arthroereisis for Symptomatic Flexible Flatfoot Deformity in Young Children: Radiological Assessment and Short-Term Follow-Up. J Foot Ankle Surg. 2019;58(5):904–915. doi: 10.1053/j.jfas.2019.01.012. [DOI] [PubMed] [Google Scholar]
- 39.Indino C, Villafañe JH, D'Ambrosi R, et al. Effectiveness of subtalar arthroereisis with endorthesis for pediatric flexible flat foot: a retrospective cross-sectional study with final follow up at skeletal maturity. Foot Ankle Surg. 2020;26(1):98–104. doi: 10.1016/j.fas.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 40.Husain ZS, Fallat LM. Biomechanical analysis of Maxwell-Brancheau arthroereisis implants. J Foot Ankle Surg. 2002;41(6):352–358. doi: 10.1016/s1067-2516(02)80080-1. [DOI] [PubMed] [Google Scholar]
- 41.Suh DH, Park JH, Lee SH, et al. Lateral column lengthening versus subtalar arthroereisis for ped flatfeet: a systematic review. Int Orthop. 2019;43(5):1179–1192. doi: 10.1007/s00264-019-04303-3. [DOI] [PubMed] [Google Scholar]
- 42.Fernández de Retana P, Alvarez F, Bacca G. Is there a role for subtalar arthroereisis in the management of adult acquired flatfoot? Foot Ankle Clin. 2012;17(2):271–281. doi: 10.1016/j.fcl.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 43.Cook EA, Cook JJ, Basile P. Identifying risk factors in subtalar arthroereisis explantation: a propensity-matched analysis. J Foot Ankle Surg. 2011;50(4):395–401. doi: 10.1053/j.jfas.2011.03.01. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.


