Abstract
Objective To determine whether the radiographic parameter at the epiphyseal tubercle region (peritubercle lucency sign) on the unaffected side can predict slipped capital femoral epiphysis (SCFE).
Methods We retrospectively reviewed patients who received an initial diagnosis of unilateral SCFE between 1995 and 2020 at a pediatric hospital in a Brazilian state's capital. The patients were monitored for at least 18 months. Two reviewers independently and blindly assessed the radiographs for the presence or absence of the sign. Disagreements were resolved by a third senior reviewer.
Results Out of the 115 cases reviewed, the peritubercle lucency sign was observed in 21 of the 30 patients who developed the disease in the contralateral hip. The sign was observed on an average of 21 days after the diagnosis on the initial side, and approximately 301 days prior to the condition affecting the contralateral hip. It was present in 95% and 85% of the cases on the lateral (frog-leg) and anteroposterior (AP) views, respectively. Interobserver reliability was measured using the Kappa test (k = 0.0801). There was a significant relationship between the presence of the sign and SCFE ( p < 0.001).
Conclusions: We propose that the peritubercle lucency sign can be used as a supplementary tool in early diagnosis, for it is beneficial in the therapeutic planning.
Level Of Evidence: Level III – Diagnostic Study In Nonconsecutive Patients (Without Consistently Applied ‘Gold Standard’ As Reference)
Keywords: early diagnosis, hip, radiography, slipped capital femoral epiphysis
Introduction
During the rapid growth phase of adolescence, increased fragility and shear stress can result in the slippage of the capital femoral epiphysis off the femoral neck, a condition known as slipped capital femoral epiphysis (SCFE). 1 2 The exact pathophysiology remains unclear, but the epiphyseal tubercle is thought to play a crucial role in disease development. The suggested mechanism involves a rotation during SCFE, so the tubercle would act as a fulcrum located eccentrically in the posterosuperior quadrant of the physis. 3 This is the most pronounced bony structure observed on the physeal surface of the capital femoral epiphysis. 4 Liu et al. 5 suggested that the epiphyseal tubercle is primarily responsible for stabilizing the capital femoral epiphysis and safeguarding the lateral epiphyseal vessels. During adolescence, the tubercle undergoes a reduction in height and perimeter, potentially leading to local instability and an increased risk of necrosis. 6 The disease has an incidence rate of 1 to 7 cases per 100 thousand people, and it predominantly affects boys, typically around the age of 14. 7 Skeletal maturity, metabolic disorders, femoral morphology, and body mass index can influence the development of the disease, which is often associated with increased body weight. 8 9 The disease more frequently impacts the left side and may affect both sides in up to 80% of the cases. It can occur simultaneously or at different times, usually within the first 18 months after the occurrence on one side. 10 11 Surgical intervention is a well-established treatment for the disease, and monitoring of the contralateral hip is crucial. In recent years, various radiographic parameters have been examined to identify early signs of SCFE in the contralateral hip; they include the Southwick angle, which indicates increased epiphyseal inclination, 12 the posterior inclination angle, 13 the alpha angle, 14 and the epiphyseal inclination. 15 While some authors 16 17 advocate for prophylactic fixation based on a combination of clinical data, radiographic evidence, and social indicators, assessment of the unaffected hip remains a subject of study. 18 Recently, a new objective imaging parameter, known as the peritubercle lucency sign, has been proposed. 19 This sign is believed to be evident on radiographs since the first changes that occur in the epiphyseal tubercle and the corresponding metaphysis. However, its practical application in clinical settings remains uncertain.
The present study aims to determine whether the peritubercle lucency sign could be used as a reliable radiographic parameter for early diagnosis and as a predictor of disease in the contralateral hip among patients with unilateral SCFE. Additionally, we aim to assess if the absence of this sign can serve as a predictor of the absence of SCFE. Finally, the study evaluates the interobserver agreement in radiographic analyses.
Materials and Methods
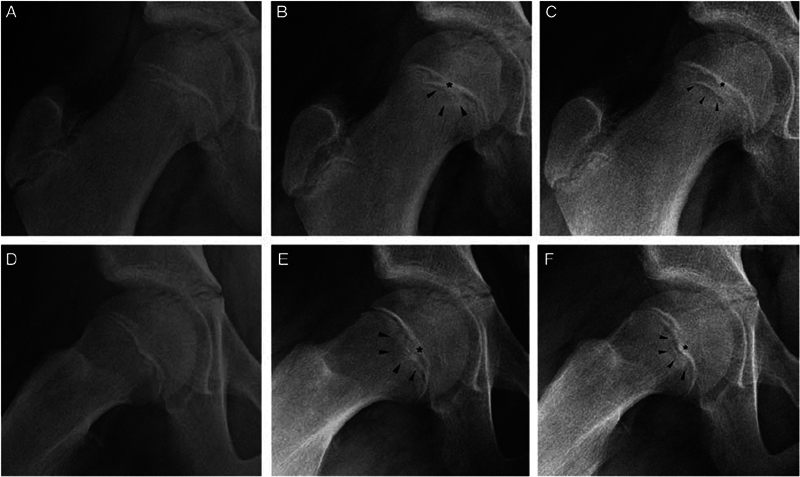
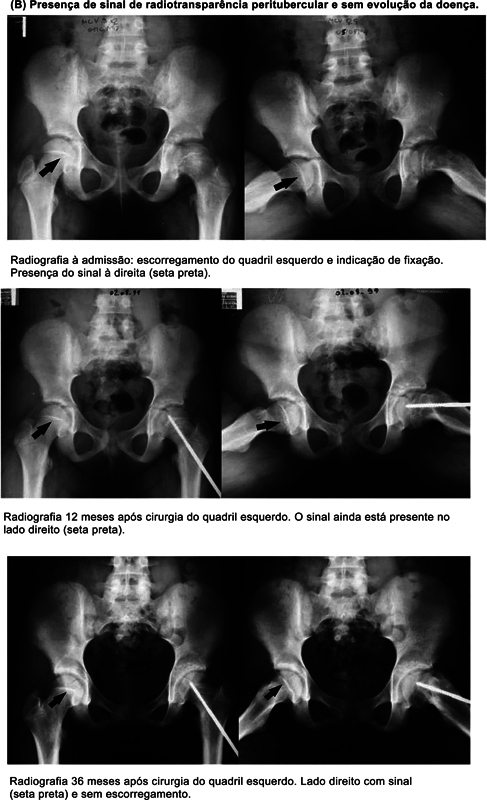
The current retrospective longitudinal study was conducted at Hospital Infantil Joana de Gusmão, in the city of Florianópolis, State of Santa Catarina, Brazil. The study population was composed of patients initially diagnosed with unilateral SCFE who had not previously undergone surgery on the opposite side and had a minimum outpatient follow-up of 18 months with the Orthopedics Service between 1995 and 2020. Patients who did not exhibit physeal closure during this period were monitored until the complete closure of the triradiate cartilage, ensuring that all were followed up until they attained skeletal maturity. The selected patients were numbered sequentially according to their inclusion in the study. Data were collected retrospectively from electronic and physical medical records, according to the research instrument described in Annex 1 . Radiographs obtained during the follow-up period were classified chronologically for each case and reviewed by two early-career orthopedic surgeons (reviewers 1 and 2). They searched for the peritubercle lucency sign as described in 2018 by Maranho et al. 19 ( Fig. 1 ). Only radiographs taken in the anteroposterior (AP) and lateral (frog -leg) views were considered valid. Reviewers 1 and 2 assessed the presence or absence of the sign in all radiographs. The sign was considered present if it appeared in at least one radiograph, and absent if it was not found in any. The responses were considered valid when both reviewers agreed on the presence or absence of the sign. In cases of disagreement, a third evaluator, a senior orthopedic surgeon referred to as reviewer 3, was consulted for a final analysis. All reviewers conducted their analyses independently and blinded. Previously, all 3 reviewers completed intra- and interobserver reliability tests, conducted in 2 rounds, analyzing 10% (15/115 cases) of the total sample size.
Annex 1. Research instrument used in the study.
| Name |
|---|
| Medical record |
| Date of birth – day/month/year |
| Age – in years |
| Sex – male/female |
| City of origin |
| Comorbidity – description |
| Percentile on the weight x age chart |
| Time of symptom evolution – in days |
| Trauma – present or absent |
| Location of the onset of symptoms – description |
| Date of first evaluation – day/month/year |
| First side – right/left |
| Degree of the first side – 0/1/2/3 |
| Surgery in the first side – day/month/year |
| First side: fixation type – in situ /reduction |
| First side: material – description |
| Second side – right/left |
| Degree of the second side – 0/1/2/3 |
| Second side: fixation type – in situ /reduction |
| Second side: material – description |
| Lucency sign – present/absent |
| Sign presence – yes/no |
| Follow-up time – in months |
| Complication – description |
| Material withdrawal – yes/no |
Fig. 1.
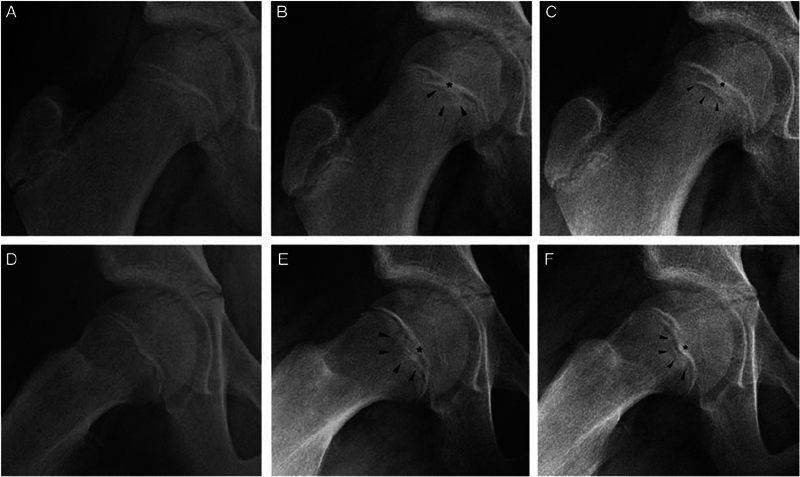
Peritubercle lucency sign 19 .
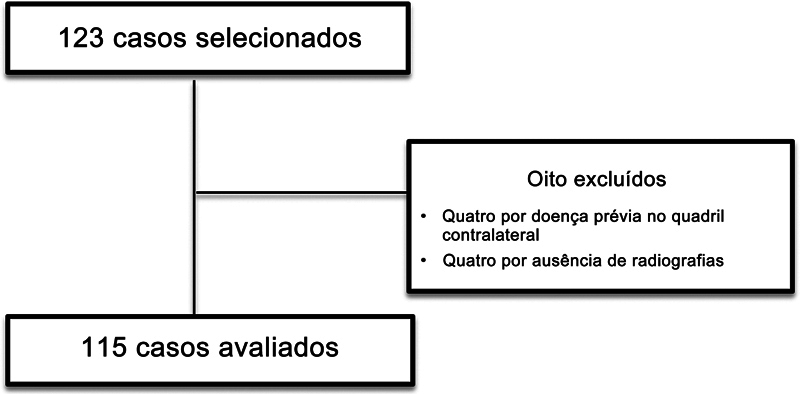
We excluded patients who had previously undergone fixation in a different service or prophylactic fixation of the unaffected hip, as well as those who did not have adequate radiographs for review and those who were diagnosed with another disease in the contralateral hip. Cases that have already presented disease in both hips from the beginning (bilateral) were not considered. A flowchart of the patient selection process is shown in Fig. 2 .
Fig. 2.
Flowchart of the patient selection process. A total of 115 cases were selected based on the inclusion criteria.
The variables were submitted to descriptive analyses. The relationships among the variables of interest were examined using the contingency coefficient C correlation test, with a significance level of p < 0.01. The interobserver agreement was verified using the Kappa coefficient of agreement, with a significance level of p < 0.01. Data were analyzed using the IBM SPSS Statistics Subscription for Windows, version Build 1.0.0.1406 (IBM Corp., Armonk, NY, United States).
The current study was conducted after we received approval from the Institutional Research Ethics Committee (opinion no. 42937121.2.0000.5361). The study was based on Resolution no. 500/16 of the Brazilian National Health Council (Conselho Nacional de Saúde, CNS, in Portuguese), and it adhered to the ethical principles of beneficence, non-maleficence, justice, and autonomy.
Results
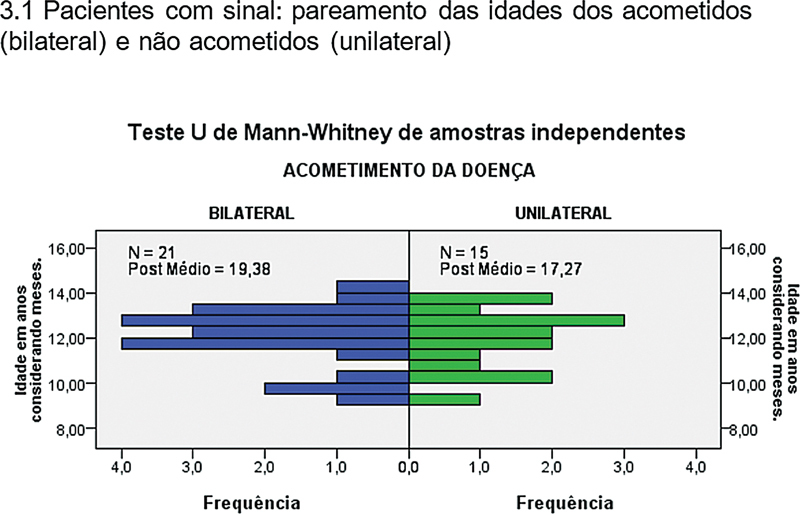
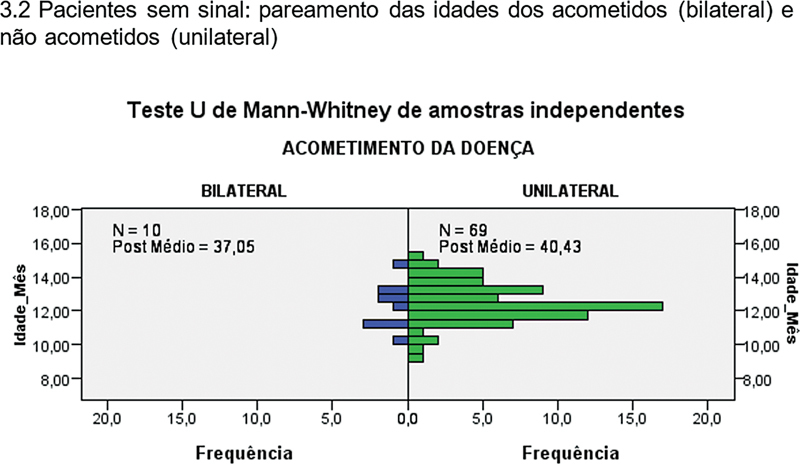
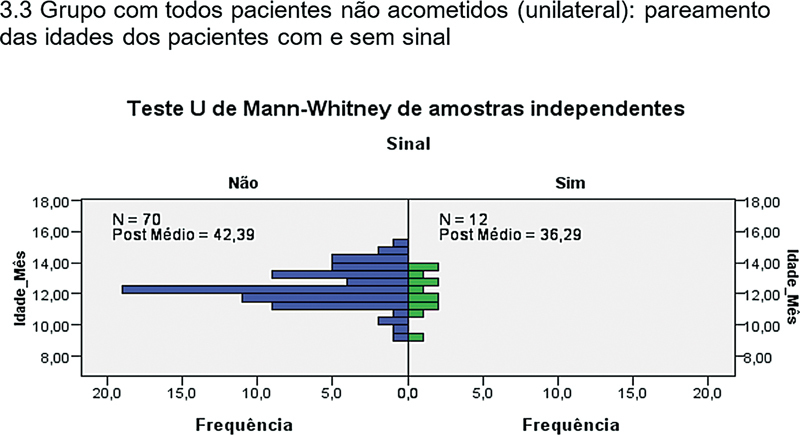
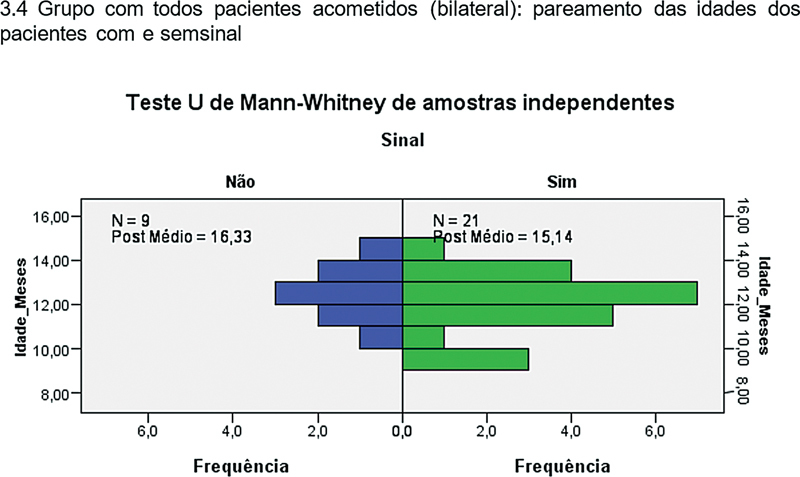
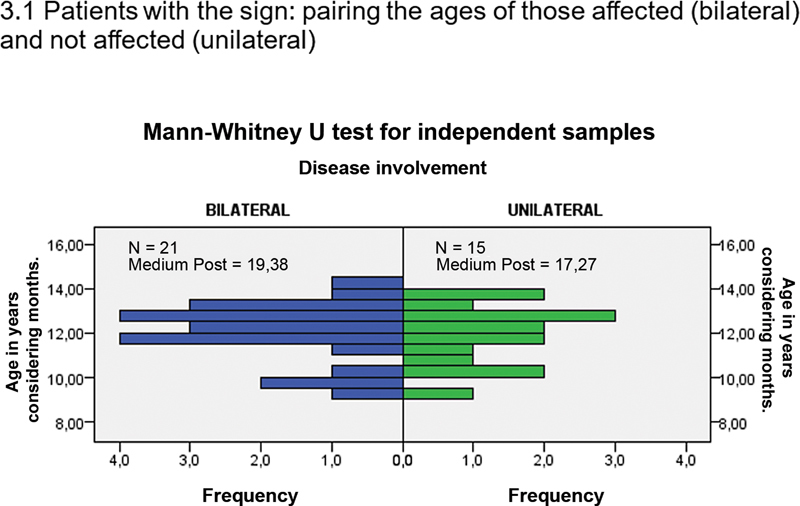
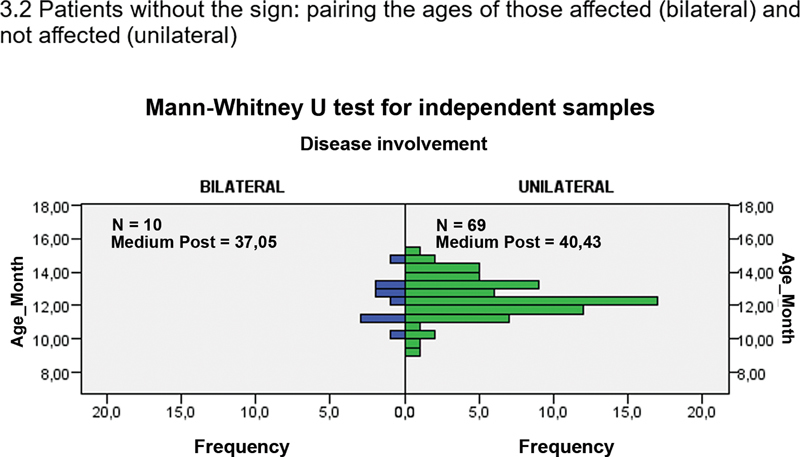
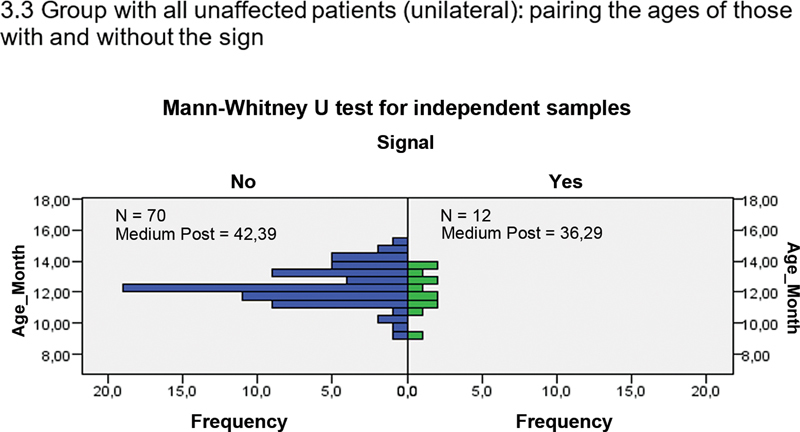
The present study included 115 patients diagnosed with unilateral SCFE at their first consultation. During the follow-up, 30 patients developed the condition in the contralateral hip. The average age was of 11.81 (range: 9–15) years, and the average follow-up period was of 32.8 (range: 4–96) months ( Table 1 ). For the obesity and overweight analysis, we used the weight-for-age index as a benchmark, referencing the percentile charts from the Centers for Disease Control and Prevention. 20 Two patients had multiple comorbidities (hypothyroidism and conditions associated with obesity). Regarding the duration of symptoms, we found that 33% of cases were acute, 62% were chronic, and 5% were chronic-acute, as per the Fahey and O'Brien classification. 21 The severity of each affected hip was measured according to the quantification classification of the slippage of the epiphysis relative to the femoral neck, as described by Wilson et al. 22 Of the two cases with a severity rating, one was diagnosed through scintigraphy, and the other was diagnosed based on pain symptoms and refusal to bear weight on the affected limb. The average time from the first consultation to the initial surgical procedure was 3.19 of (range: 0–30) days. For patients who, during follow-up, developed the disease in the contralateral hip and required fixation, the interval between the two surgeries was on average 312 (range: 26–810) days. In-situ fixation was the method of choice in 86.89% of the cases. The materials used for fixation were either a cannulated screw or a threaded metallic wire (Schanz pin). The choice of implant varied over the years, based on when the procedure was performed and the availability of the synthesis materials at the hospital. The evaluation of the peritubercle lucency sign is outlined in Table 2 and the sign was found to be present in 31.3% of all cases. Out of the 30 individuals who developed the disease, 21 exhibited this sign. The youngest patient who presented the sign and progressed to the disease was a male aged 9 years and 1 month, and the oldest patient was a boy aged exactly 14 years. When pairing the presence or absence of the sign with age, the null hypothesis must be retained since age behavior does not differ significantly between the groups that did or did not progress to the disease ( Table 3 ). A significant correlation between the presence of the peritubercle lucency sign and contralateral SCFE was found ( p < 0.001). The contingency coefficient C showed a p -value of 1.06 × 10 −7 ( p < 0.001). The upper limit of the contingency coefficient C is 0.707, and the correlation is 0.44. The data obtained from these analyses are described in Table 4 .
Table 1. Demographics and clinical characteristics of the study sample.
| n | Valid percentage** | |
|---|---|---|
| Sex | ||
| - Male | 76 | 66.1% |
| - Female | 39 | 33.9% |
| Comorbidity | ||
| - Obesity | 66 | 56.4% |
| - Overweight | 17 | 20% |
| - Others | 3 | 3.6% |
| - Degree* | ||
| 0 | 2 | |
| 1 | 68 | |
| 2 | 26 | |
| 3 | 15 | |
| - Type of fixation | ||
| Reduction | 14 | |
| In-situ fixation | 99 | |
| Second affected hip | ||
| - Side | ||
| Right | 23 | 76.7% |
| Left | 7 | 23.3% |
| - Degree | ||
| 0 | 11 | |
| 1 | 15 | |
| 2 | 1 | |
| 3 | 0 | |
| - Type of fixation | ||
| Reduction | 0 | |
| In-situ fixation | 28 |
Note: *According to Wilson et al. 22
Note: **Valid percentage only considers cases that contained information in the medical record.
Table 2. Evaluation of the peritubercle lucency sign.
| Lucency Sign | Unilateral (n) | Bilateral (n) | Total (N) |
|---|---|---|---|
| Absent | 71 | 9 | 80 |
| Present | 14 | 21 | 35 |
| Total | 85 | 30 | 115 |
Notes: Unilateral – there was no evolution to disease; bilateral – there was evolution to disease.
Table 3. Pairing sign with age.
| N | Minimum | Maximum | Average | Deviaton error | |
|---|---|---|---|---|---|
| Age (months) | 36 | 9.08 | 14.00 | 11.9844 | 1.33053 |
Table 4. Statistical analysis: association between the presence of the peritubercle lucency sign and development of the SCFE.
| Statistical data | |
|---|---|
| Sample (N) | 115 |
| Sign emergence time | 1 month |
| Time before the slippage | 40 weeks |
| Anteroposterior/Frog-leg radiographs | 85%/95% |
| Accuracy | 80% |
| Sensitivity | 70% |
| Specificity | 83% |
| Positive predictive value | 60% |
| Negative predictive value | 89% |
3.1 Patients with the sign: pairing the ages of those affected (bilateral( and not affected (unilateral)
3.2 Patients without the sign: pairing the ages of those affected (bilateral) and not affected (unilateral)
| N | Minimum | Maximum | Average | Deviaton error | |
|---|---|---|---|---|---|
| Age (months) | 79 | 9.00 | 15.42 | 12.4181 | 1.20627 |
3.3 Group with all unaffected patients (unilateral): pairing the ages of those with and without the sign
| N | Minimum | Maximum | Average | Deviaton error | |
|---|---|---|---|---|---|
| Age (months)( | 82 | 9.00 | 15.42 | 12.3309 | 1.22065 |
3.4 Group with all affected patients (bilateral): pairing the ages of those with and without the sign
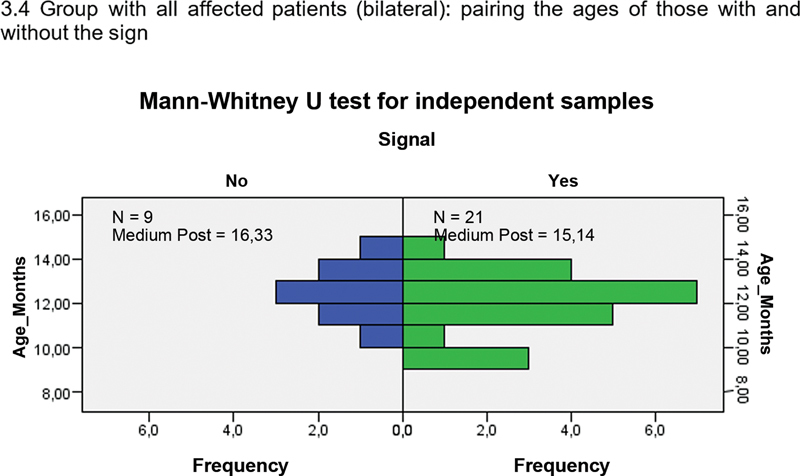
| N | Minimum | Maximum | Average | Deviaton error | |
|---|---|---|---|---|---|
| Age (months) | 30 | 9.08 | 14.67 | 12.1640 | 1.35121 |
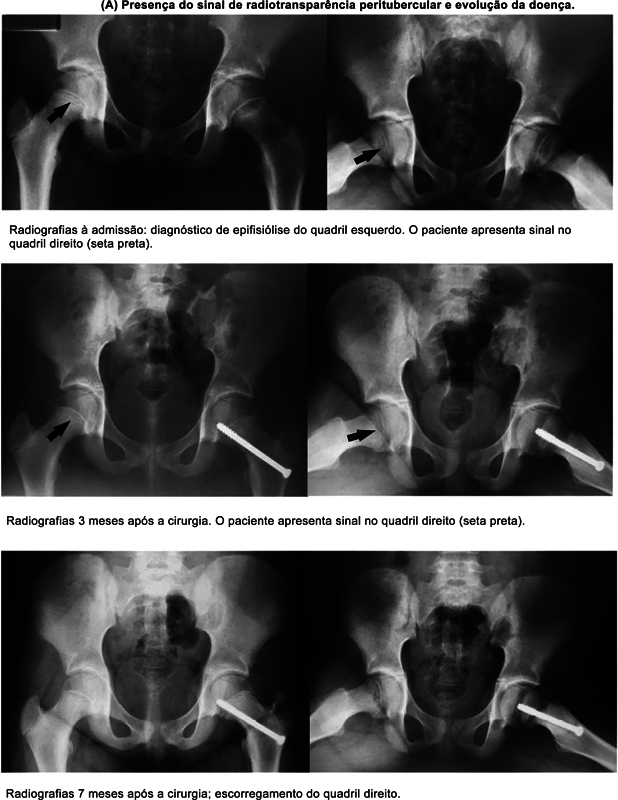
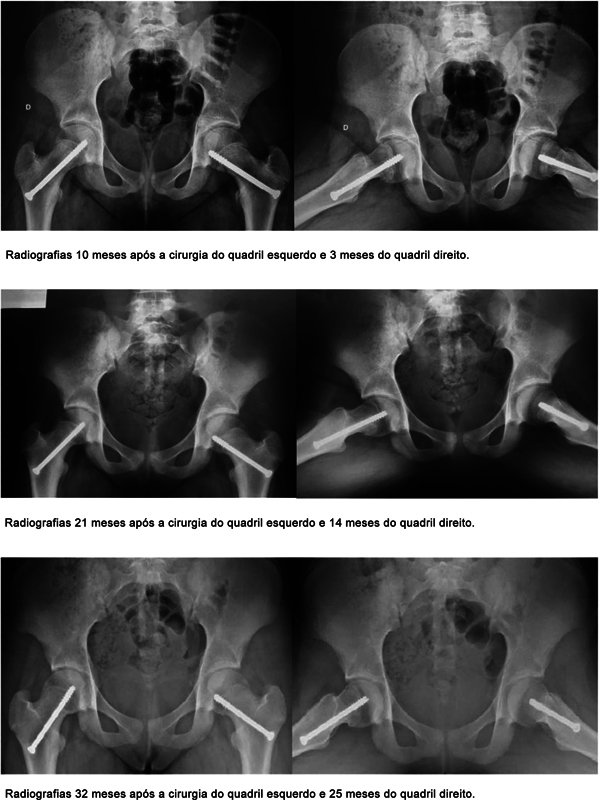
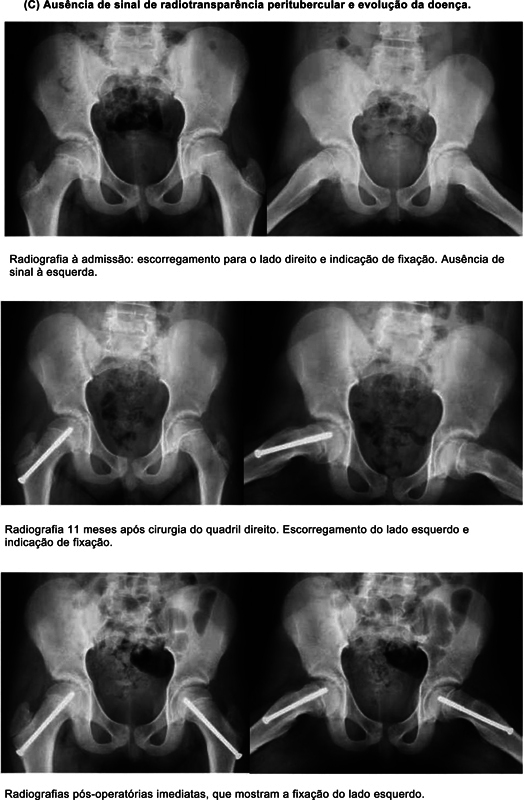
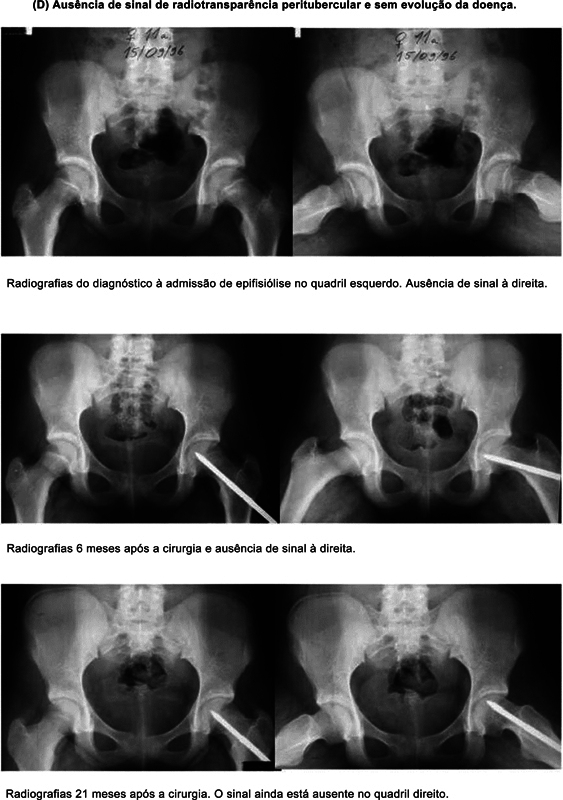
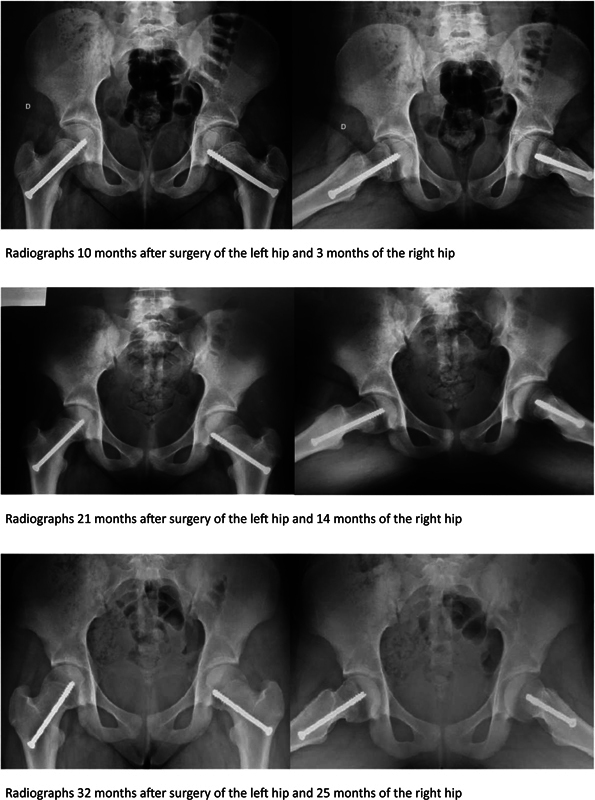
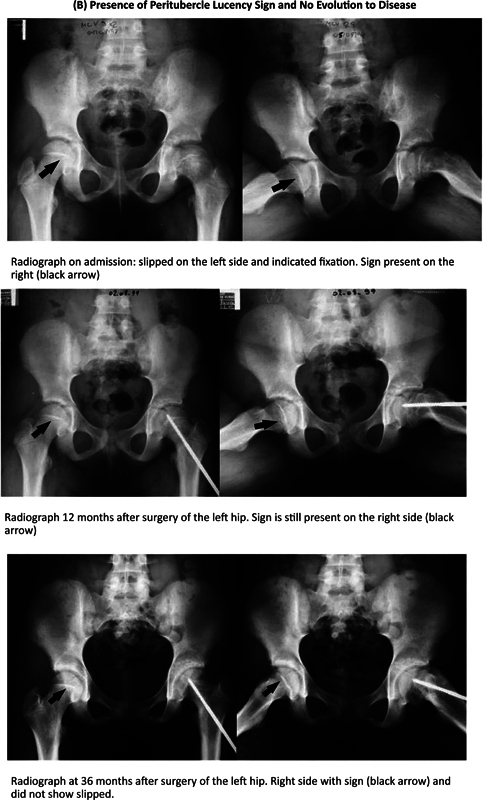
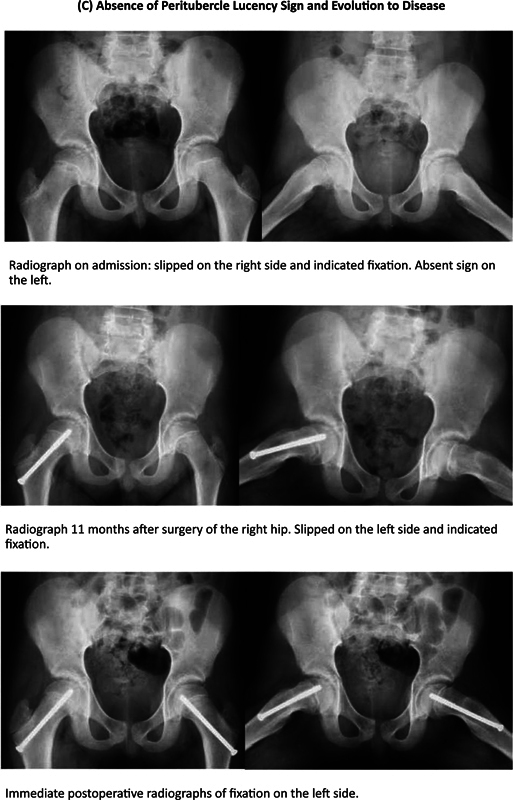
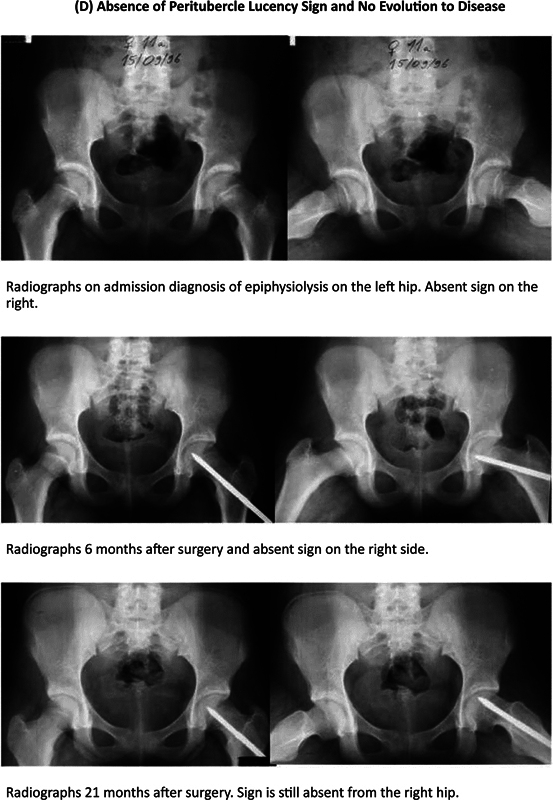
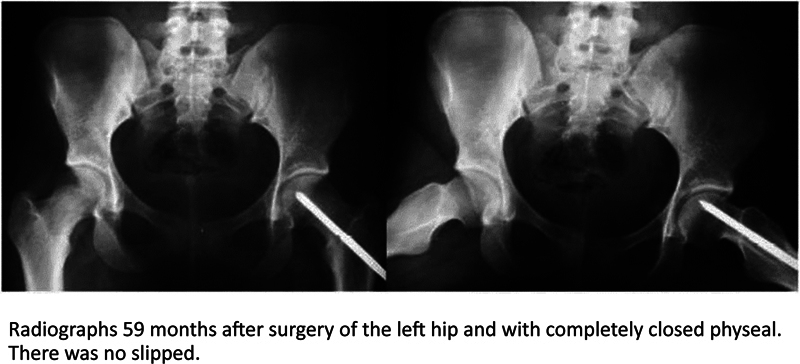
In cases in which the sign was present and the patients developed the disease in the contralateral hip, the sign was observed on average 21 days after the disease was first diagnosed on the initial side. The slippage typically occurred approximately 301 days later. In this group, the sign was more frequently observed in the frog-leg view (20/21 cases, 95%) than in the AP view (18/21 cases, 85%). The inter-observer agreement between reviewers 1 and 2 was found to be strong, as measured by the Kappa test (k = 0.0801). In 10 cases, the evaluations needed to be reviewed by reviewer 3. No significant correlation was identified in the analysis regarding the presence or absence of the sign and the variables of interest ( Table 5 ). It is important to note that, despite the visual differences observed between the groups based in terms of the presence or absence of the sign, these differences did not show statistical significance. Eight cases were excluded for the following reasons: two had previously undergone fixation at a different facility; two had a degenerative disease in the contralateral hip (Legg-Calvé-Perthes disease); and four were excluded since follow-up control radiographs were not available. We were able to identify the presence and absence of the sign, with or without development of the disease, as shown in Fig. 3 .
Table 5. Statistical analysis regarding the presence or absence of the sign and the variables of interest.
| Variables of interest compared | Statistical test | Degree | Significance | Conclusion |
|---|---|---|---|---|
| Present sign versus age | 1.073 | 1 | 0.376 | Does not reject H 0 |
| Present sign versus sex | 3.196 | 1 | 0.091 | Does not reject H 0 |
| Present sign versus comorbidity | 4.487 | 2 | 0.106 | Does not reject H 0 |
| Present sign versus laterality | 1.073 | 1 | 0.376 | Does not reject H 0 |
| Present sign versus degree of the first side | 3.785 | 2 | 0.151 | Does not reject H 0 |
Fig. 3.
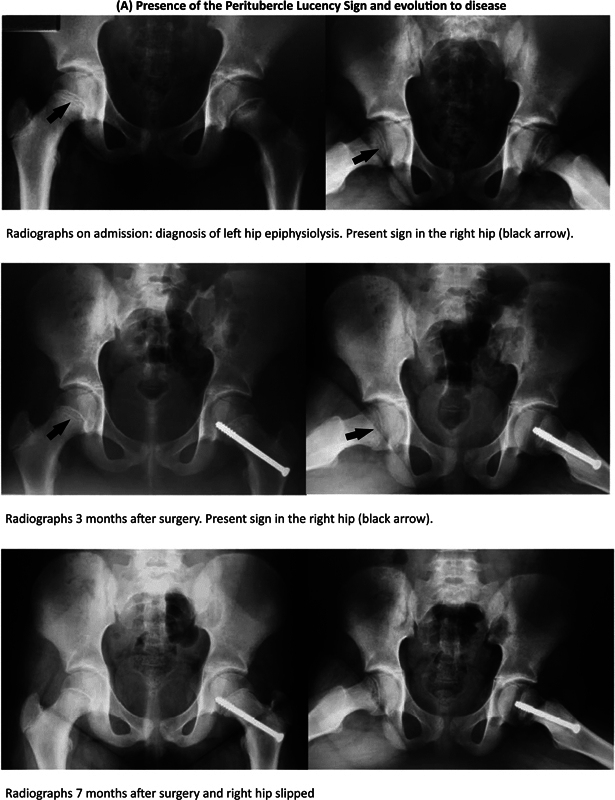
Radiological assessment of peritubercle lucency sign and development of slipped capital femoral epiphysis (SCFE). ( A ) Presence of the peritubercle lucency sign and development of the disease; ( B ) presence of the peritubercle lucency sign and absence of the disease; ( C ) absence of the peritubercle lucency sign and development of the disease; and ( D ) absence of the peritubercle lucency sign and absence of the disease.
Discussion
While anatomical and histological alterations in the disease have been extensively described in previous studies, 2 3 the peritubercle lucency sign on radiographs was only recently proposed as an indicator for early diagnosis. 19 This method has yielded results that are comparatively superior to those of magnetic resonance imaging. 23 The tubercle is commonly located in the posterosuperior quadrant, positioned more posteriorly in younger children and superiorly in older ones. 5 Its primary role is to provide structural support against the shear forces acting on the capital femoral physis. 5 The radiographic manifestation of the action of these forces would be the peritubercle lucency. 19
As described by Kleinman et al., 6 abnormalities in the capital femoral metaphysis (juxtaphyseal) can be challenging to detect, likely reflecting the localized reparative response to stress mechanisms that weaken the area. Song 24 suggested that orthopedists should explore new methodologies and algorithms to facilitate earlier diagnosis and treatment of this condition.
The present study aimed to assess the applicability of this sign. In our assessment, of 115 patients, all of whom met the inclusion criteria, 30 developed SCFE on the contralateral hip. The sign was present in 31% of the total sample (36/115). Of these 36 patients, 58% (21/36) developed the disease, while 42% (15/36) remained with the unilateral affection. In cases in which the sign was considered absent (79/115), the majority (70/79) did not develop SCFE, and 11% (9/79) developed the disease. Upon analyzing the 30 patients that developed SCFE, we found the sign present in 70% of these cases (21/30). In contrast, among the 85 cases that remained exclusively unilateral (that is, they did not develop SCFE) the absence of the sign was noted in 82% of these patients (70/85).
Our sensitivity and specificity indices were of 70% and 82% respectively. While these values are relatively lower than those reported by Maranho et al., 19 they are still considerably high. In 80% of the cases, we observed the sign on the initial radiographs of the first affected side either in the pre- or immediate postoperative period. The Kappa index between the two main observers reached a level of strong and superior agreement, according to Cohen. 25 However, to enhance the reliability of the findings, a third senior observer conducted additional analyses.
Our analysis had some limitations regarding the accessibility of previous radiographs and the lack of information in certain medical records. Despite these constraints, we maintained a minimum follow-up period of 18 months, as this time frame is widely accepted in the literature for the expected occurrence of SCFE in the contralateral hip. 1 9 10 Although there are documented cases in which SCFE occurred after this period, we did not encounter any cases in this study. Such cases were monitored until the complete closure of the triradiate cartilage was achieved.
Another limitation was the absence of a standardized position of patients during radiography. The position, which could vary in degrees of flexion, extension, rotation, and abduction, often depended on the patient's level of pain. However, the frog-leg view, which we considered the most effective for diagnosing SCFE, was less compromised and was the one that most often revealed the presence of the sign.
We believe that seeking and verifying the peritubercle lucency sign serves as a useful guide for early diagnosis, 26 helping to prevent more severe and pronounced cases. Further studies need to be conducted to determine whether the forces acting on the capital femoral physis can be considered responsible for the sign.
Conclusion
Our findings suggest a significant correlation between the presence of the sign on radiographs and the development of the disease in the patient's contralateral hip. While there are more accurate diagnostic tests, such as magnetic resonance imaging, the presence of the sign on radiographs appears to predict disease development. The interobserver agreement was similar to that of other studies, supporting its applicability in the clinical practice. Hence, the peritubercle lucency sign emerges as a promising supplementary tool in the early diagnosis of SCFE, being useful for therapeutic planning and feasible for wide-scale application when high-cost complementary exams are not available. While we found no connection involving the sign and patient-specific characteristics or disease traits, we advise using it judiciously, considering the clinical examination and, if required, other complementary imaging tests. This is because SCFE may still occur, even in the absence of the sign.
Funding Statement
Suporte Financeiro Os autores declaram que não receberam suporte financeiro de agências dos setores público, privado ou sem fins lucrativos para a realização deste estudo.
Financial Support The authors declare that they did not receive financial support from agencies in the public, private, or non-profit sectors to conduct the present study.
Conflito de Interesses Os autores não têm conflito de interesses a declarar.
Contribuições dos Autores
Cada autor contribuiu individual e significativamente para o desenvolvimento desta pesquisa; AK: elaboração do projeto de pesquisa, avaliador 3, redação do artigo e revisão do texto; RVRM: elaboração do projeto de pesquisa, avaliador 1, redação do artigo, revisão do texto e revisão bibliográfica; MAG: elaboração do projeto de pesquisa, avaliador 2, redação do artigo e revisão de literatura; e MAO: elaboração do projeto de pesquisa, busca de prontuários e radiografias, e redação do artigo.
Trabalho desenvolvido no Departamento de Ortopedia Pediátrica, Hospital Infantil Joana de Gusmão, Florianópolis, SC, Brasil.
Author Contributions:
Each author contributed individually and significantly to the development of this research. AK: development of the research project, evaluator 3, writing of the article, and text review; RVRM: development of the research project, evaluator 1, writing of the article, text review, and bibliographical review; MAG: development of the research project, evaluator 2, writing of the article, and literature review; and MAO: development of the research project, search of records and radiographs and writing of the article.
Work carried out at the Department of Pediatric Orthopedics, Hospital Infantil Joana de Gusmão, Florianópolis, SC, Brazil.
Referências
- 1.Kotzias Neto A. Porto Alegre:: Artmed; 2016. Epiphysiolysis proximal femur; pp. 300–319. [Google Scholar]
- 2.Griffith M J. Slipping of the capital femoral epiphysis. Ann R Coll Surg Engl. 1976;58(01):34–42. [PMC free article] [PubMed] [Google Scholar]
- 3.Tayton K. Does the upper femoral epiphysis slip or rotate? J Bone Joint Surg Br. 2007;89(10):1402–1406. doi: 10.1302/0301-620X.89B10.19563. [DOI] [PubMed] [Google Scholar]
- 4.Novais E N, Maranho D A, Kim Y J, Kiapour A. Age- and Sex-Specific Morphologic Variations of Capital Femoral Epiphysis Growth in Children and Adolescents Without Hip Disorders. Orthop J Sports Med. 2018;6(06):2.325967118781579E15. doi: 10.1177/2325967118781579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu R W, Armstrong D G, Levine A D, Gilmore A, Thompson G H, Cooperman D R. An anatomic study of the epiphyseal tubercle and its importance in the pathogenesis of slipped capital femoral epiphysis. J Bone Joint Surg Am. 2013;95(06):e341–e348. doi: 10.2106/JBJS.L.00474. [DOI] [PubMed] [Google Scholar]
- 6.Kleinman P K, Marks S C, Jr, Spevak M R, Belanger P L, Richmond J M. Extension of growth-plate cartilage into the metaphysis: a sign of healing fracture in abused infants. AJR Am J Roentgenol. 1991;156(04):775–779. doi: 10.2214/ajr.156.4.2003445. [DOI] [PubMed] [Google Scholar]
- 7.Crawford A H. Slipped capital femoral epiphysis. J Bone Joint Surg Am. 1988;70(09):1422–1427. [PubMed] [Google Scholar]
- 8.Loder R T, Aronson D D, Greenfield M L. The epidemiology of bilateral slipped capital femoral epiphysis. A study of children in Michigan. J Bone Joint Surg Am. 1993;75(08):1141–1147. doi: 10.2106/00004623-199308000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Morrissy R T. Slipped capital femoral epiphysis - Natural history and etiology in treatment. Instr Course Lect. 1980;29:81–86. [Google Scholar]
- 10.Jensen H P, Steinke M S, Mikkelsen S S, Thomsen P B. Hip physiolysis. Bilaterality in 62 cases followed for 20 years. Acta Orthop Scand. 1990;61(05):419–420. doi: 10.3109/17453679008993553. [DOI] [PubMed] [Google Scholar]
- 11.Southwick W O. Osteotomy through the lesser trochanter for slipped capital femoral epiphysis. J Bone Joint Surg Am. 1967;49(05):807–835. [PubMed] [Google Scholar]
- 12.Barrios C, Blasco M A, Blasco M C, Gascó J. Posterior sloping angle of the capital femoral physis: a predictor of bilaterality in slipped capital femoral epiphysis. J Pediatr Orthop. 2005;25(04):445–449. doi: 10.1097/01.bpo.0000158811.29602.a5. [DOI] [PubMed] [Google Scholar]
- 13.Nötzli H P, Wyss T F, Stoecklin C H, Schmid M R, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84(04):556–560. doi: 10.1302/0301-620x.84b4.12014. [DOI] [PubMed] [Google Scholar]
- 14.Steppacher S D, Tannast M, Werlen S, Siebenrock K A. Femoral morphology differs between deficient and excessive acetabular coverage. Clin Orthop Relat Res. 2008;466(04):782–790. doi: 10.1007/s11999-008-0141-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Laredo Filho J, Braga M B, Jr, Ishida A, Bortoletto A. Estudo crítico da indicação da pinagem preventiva do lado sadio na epifisiólise proximal do fêmur unilateral. Rev Bras Ortop. 1987;22(06):173–176. [Google Scholar]
- 16.Santili C. Epifisiólise. Rev Bras Ortop. 2001;36(03):49–56. [Google Scholar]
- 17.Mestriner M B, Verquietini C M, Waisberg G, Akkari M, Fukunaga E T, Santili C. Radiographic evaluation in epiphysiolysis: possible predictors of bilaterality? Acta Ortop Bras. 2012;20(04):203–206. doi: 10.1590/S1413-78522012000400001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maranho D A, Ferrer M G, Kim Y J, Miller P E, Novais E N. Predicting Risk of Contralateral Slip in Unilateral Slipped Capital Femoral Epiphysis: Posterior Epiphyseal Tilt Increases and Superior Epiphyseal Extension Reduces Risk. J Bone Joint Surg Am. 2019;101(03):209–217. doi: 10.2106/JBJS.18.00440. [DOI] [PubMed] [Google Scholar]
- 19.Maranho D A, Miller P E, Novais E N. The Peritubercle Lucency Sign is a Common and Early Radiographic Finding in Slipped Capital Femoral Epiphysis. J Pediatr Orthop. 2018;38(07):e371–e376. doi: 10.1097/BPO.0000000000001198. [DOI] [PubMed] [Google Scholar]
- 20.National Center for Health Statistics.CDC Growth Charts [Centers for Disease Control and Prevention website]December 15,2022. Available at:https://www.cdc.gov/growthcharts/cdc_charts.htm. [Accessed in 07/10/2023].
- 21.Fahey J J, O'Brien E T. Acute slipped capital femoral epiphysis: review of the literature and report of ten cases. J Bone Joint Surg Am. 1965;47:1105–1127. [PubMed] [Google Scholar]
- 22.Wilson P D, Jacobs B, Schecter L. Slipped capital femoral epiphysis: an end-result study. J Bone Joint Surg Am. 1965;47:1128–1145. [PubMed] [Google Scholar]
- 23.Maranho D A, Bixby S D, Miller P E et al. What Is the Accuracy and Reliability of the Peritubercle Lucency Sign on Radiographs for Early Diagnosis of Slipped Capital Femoral Epiphysis Compared With MRI as the Gold Standard? Clin Orthop Relat Res. 2020;478(05):1049–1059. doi: 10.1097/CORR.0000000000001136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Song K M. CORR Insights®: What is the Accuracy and Reliability of the Peritubercle Lucency Sign on Radiographs for Early Diagnosis of Slipped Capital Femoral Epiphysis Compared With MRI as the Gold Standard? Clin Orthop Relat Res. 2020;478(05):1060–1061. doi: 10.1097/CORR.0000000000001232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20(01):37–46. [Google Scholar]
- 26.Brown D W, Iorio T J, Mosher Z A et al. Intraobserver and interobserver reliability of the peritubercle lucency sign in slipped capital femoral epiphysis. J Pediatr Orthop. 2021;41(03):159–163. doi: 10.1097/BPO.0000000000001733. [DOI] [PubMed] [Google Scholar]