Abstract
Purpose
The failure rate following posterolateral corner reconstruction (PLC) remains high. Previous research indicates that in posterior cruciate ligament (PCL) reconstruction the laxity is affected by the tibial slope (TS). However, there is currently no literature evaluating the impact of TS on surgical outcome in combined reconstruction of PLC/PCL.
Methods
This study analyzed 47 patients in a retrospective cohort study who underwent PCL and anatomical PLC reconstruction according to techniques described by Arciero or LaPrade. TS was measured, and patients were divided into two groups: Group A (n = 16) with TS < 8° and Group B (n = 31) with TS ≥ 8°. After a minimum follow-up of 12 months, the side-to-side difference (SSD) of posterior tibial translation (PTT) was assessed using instrumented stability testing (Rolimeter), and various patient-reported outcome measures (IKDC, Lysholm) were collected and compared.
Results
At a mean follow-up of 17.7 ± 4.7 months, group A exhibited a higher SSD of PTT (A 3.9 mm ± 2.1 vs. B: 2.8 mm ± 1.5; p < 0.05). A negative correlation was observed between SSD of PTT and both TS (r = − 0.43; R2 = 0.18; p < 0.01) and the Lysholm Score (r = − 0.41; R2 = 0.17; p < 0.01) in the overall cohort. Subgroup analysis revealed a higher Lysholm Score in patients with a postoperative SSD of PTT less than 4 mm (85.7 ± 10.1 vs. 79.2 ± 6.6; p = 0.0006).
Conclusion
In combined PCL and anatomic PLC reconstruction a TS < 8° results in elevated SSD of PTT. A flattened TS is linked to higher remaining SSD of PTT, while lower SSD of PTT is associated with improved clinical outcomes.
Level of evidence
Retrospective Cohort Study, IV.
Keywords: Reconstruction, Posterior slope, Posterior tibial translation, Posterior cruciate ligament, PCL, Posterolateral corner, PLC
Introduction
Soft tissue structures like the posterior cruciate ligament (PCL), posterolateral corner (PLC), and meniscus have long been recognized for their roles in posterior knee laxity. The PLC comprises the lateral collateral ligament (LCL) and the popliteus complex, which includes the popliteus muscle tendon unit and the arcuate complex. The arcuate complex consists of the popliteofibular ligament, the fabellofibular ligament, and the popliteomeniscal fibers. The popliteus complex is the crucial stabilizer against external tibial rotation and posterior translation [12, 24]. Arciero’s [3] fibula based and LaPrade’s [23] tibiofibular based anatomical PLC reconstructions are common techniques and proven to restore sufficient stability [38] as well as yielding equally satisfying clinical results [6, 7, 41].
However, the impact of tibial plateau bony geometry, particularly the tibial slope (TS), has remained less explored. Emerging research suggests that the inclination of the tibial plateau directly influences knee kinematics, including anteroposterior laxity, cruciate ligament loading, and the center of rotation [2, 17, 31]. Notably, the importance of the PLC in knee stability has gained prominence. Studies underscore the pivotal role of the PLC in maintaining knee stability, emphasizing its interaction with the TS, indicating that changes in TS can significantly affect load transmission within the knee joint and the anterior–posterior translation of the tibia [1, 16, 29]. An elevated TS, for instance, has been linked to potentially reducing mechanical graft overload following PCL reconstruction [19]. Conversely, a flattened TS is associated with markedly increased posterior tibial translation (PTT), providing insights into why existing surgical approaches struggle to restore knee stability effectively [17]. Despite these insights, there remains a gap in our understanding of how the TS influences posterior laxity, particularly in the context of anatomic posterolateral reconstruction (Arciero or LaPrade).
To the best of our knowledge, this study is the first to investigate the relationship between TS and PTT in the anatomical reconstruction of PLC/PCL deficient knees. Our primary objective was to explore whether a correlation exists between TS and posterior laxity following PLC and PCL reconstruction, with a specific focus on the importance of anatomic PLC reconstruction in knee stability. We hypothesised that elevated TS will correspond to a greater reduction in PTT following PLC and PCL reconstruction.
Materials and methods
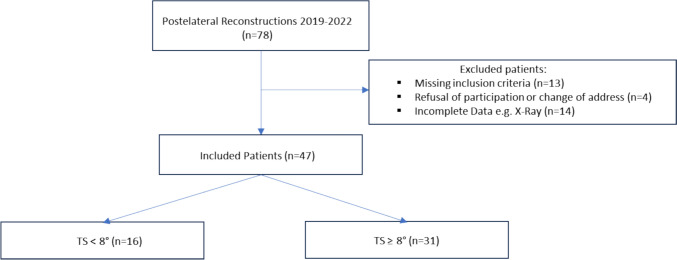
Patient population: this study used a retrospective cohort study design. The in-house trauma register was screened at two level I trauma centres for all patients undergoing combined PLC and PCL reconstruction surgery between 2018 and 2022 (see Fig. 1). Only patients presenting with chronic injuries (> 6 weeks), a combination of varus and posterolateral instability (Fanelli B [14], see Table 1) and additional posterior instability (> 5 mm of side-to-side difference on bilateral posterior stress radiographs, Telos) due to PCL injury were included. Diagnosis was based on MRI-imaging, stress radiography and physical examination to assess ligamentous instability. Exclusion criteria were patient age under 18 years, higher grade cartilage defects (ICRS > 2), peroneal nerve injuries, higher- or lower-grade PLC injuries (Fanelli A/C), revision PCL/PLC reconstruction, missing radiographic data, varus or valgus malalignment as determined by long leg radiographs, prior slope correcting osteotomy, and additional affected structures (e.g. ACL, MCL). All included Patients were divided into two groups according to their TS based on the findings of Gwinner et al. [17]: group A with TS < 8° and group B with TS ≥ 8°. An institutional ethics commission approved this study and informed consent was obtained by each patient prior to clinical follow-up investigation.
Fig. 1.
Flow Chart of patient selection
Table 1.
The Fanelli and Larson classification [14] classifies the damage in posterolateral structures
| Fanelli and Larson classification | Scale of damage |
|---|---|
| Type A | > 10° Increase in External Rotation (ER) of Tibia |
| Type B | > 10° increase in ER of Tibia + mild-moderate instability in varus stress |
| Type C | > 10° increase in ER of Tibia + severe instability in varus stress |
Surgical management: All PCL reconstructions were arthroscopically performed by a single bundle technique. Hamstring tendon autografts were used in all cases. Additional posterolateral reconstruction according to Arciero [3] or LaPrade [23] or their derivative arthroscopic reconstructions [15, 22] were performed. The choice of surgical technique was initially randomised, but later changed in favour of Arciero’s technique, as the clinical outcomes are equivalent [13, 41], but Arciero’s technique was simpler and less invasive. Arciero’s technique utilizes a fibula-based reconstruction with an anatomic transfibular tunnel placement along the native functional anatomy of the LCL and popliteus tendon. In contrast, LaPrade’s approach includes an additional tibiofibular graft to address tibiofibular instability.
Rehabilitation: peripheral nerve block anaesthesia was uniformly administered. Standardized physical therapy commenced 48 h post-operation, incorporating 6–8 weeks of wearing stabilizing braces (Jack PCL Brace; Albrecht, Bernau am Chiemsee, Germany). The initial 6 weeks involved a restricted range of motion, with a maximum knee flexion of 45° for the first 2 weeks. Passive knee flexion was initiated after drain removal, followed by progressive mobilization to 60° up to week 4, and 90° in weeks 5 and 6. Weight-bearing was limited to 20 kg for six weeks, transitioning to full weight-bearing after this period.
Clinical testing and radiological assessment: two independent observers (A.K. and H.F.) assessed the TS and PTT, with both parameters measured in a blinded fashion on preoperatively performed bilateral Telos Stress Radiographs. Mean values for the TS and PTT were subsequently computed. TS, defined as the angle between a line parallel to the posterior inclination of the tibial plateau and a line perpendicular to the diaphyseal shaft axis, was measured following the method by Dejour et al. [11]. The medial TS was selected due to the superimposition of the medial contour on lateral radiographs and recent literature suggests that it might be more significant than the lateral TS in PCL injuries [25]. The diaphyseal shaft axis was established using midpoints between the anterior and posterior tibial cortex at specified locations (9 and 15 cm distally to the joint line). The tangent line to the medial tibial plateau and the perpendicular to the diaphyseal axis determined the TS. In cases of multiple radiographs, TS was measured on the one containing the longest diaphyseal axis and the best true lateral view. (see Fig. 2).
Fig. 2.
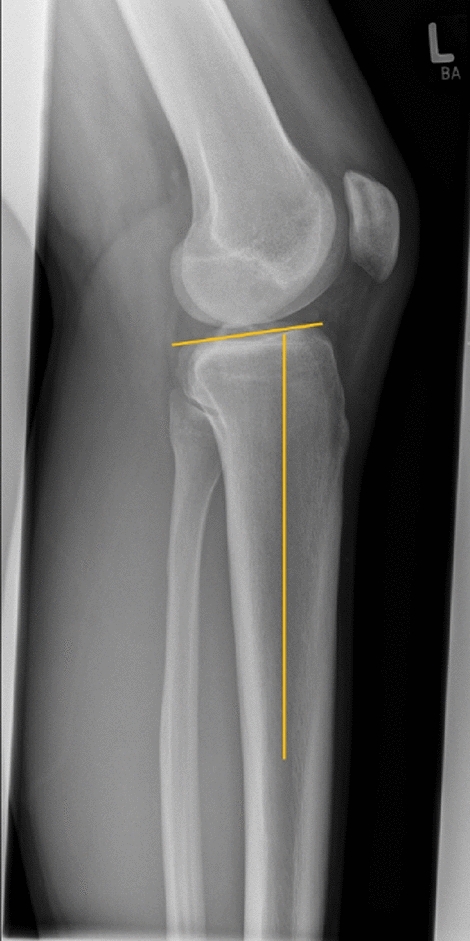
Preoperative measurement of the Tibial Slope (TS): The TS is defined as the angle between a line parallel to the posterior inclination of the tibial plateau and a line perpendicular to the diaphyseal shaft axis
A follow-up examination, conducted at a minimum of 12 months post-surgery, utilized Lysholm and IKDC scoring systems for functional outcomes. The posterior drawer test was performed on both knees using the Rolimeter test to assess PTT according to Höher et al. [22], and from this data, the postoperative side-to-side difference of the PTT (SSD of PTT) was calculated.
A cut-off value of 4 mm SSD of PTT was chosen to divide patients into clinically significant instability [32, 43]. Postoperative PCL graft failure was defined as non-traumatic PCL re-rupture confirmed by MRI or arthroscopy.
Statistical analysis
Statistical analysis was performed using GraphPad Prism 8 (San Diego, CA, USA). Data are presented as means and standard deviations (SD). The calculation was based on two groups: (1) patients with a TS < 8° (Group A) compared to (2) patients with a TS ≥ 8° (Group B). The intra-rater and inter-rater reliability for the measurement of the tibial slope (TS) were evaluated using the intraclass correlation coefficient (ICC). The primary outcome was defined by instrumental stability testing (SSD of PTT) and the secondary outcome by PROMS (Lysholm and IKDC-Score). Additional subgrouping was performed for BMI (Body mass index), surgical technique and SSD of PTT. The differences between the groups were calculated using the student’s t-test and Mann Whitney U-Test or Wilcoxon matched-pairs rank test for non-parametric parameters. Categorical parameters were compared using Fisher’s exact test. Pearson correlation analysis examined the association between TS and PTT or PROMS. For group comparisons of categorical variables, the chi-square test was applied. The statistical significance level was set at p < 0.05. Sample size calculation using G-Power (version 3.1.9.7., Heinrich Heine University, Düsseldorf) indicated that a sample size of n = 12 in each group would be required to detect a difference of 10 points with an SD of 10 in the clinical Lysholm score, with a α error of 5% and a power of 0.8. A significance level of p < 0.05 was applied.
Results
Patient demographics
Ultimately, 47 patients were included, with a mean follow-up of 17.7 ± 4.7 months (range 12–22): 16 in group A (TS < 8°) and 31 in group B (TS ≥ 8°). The average age was 37 ± 12.0 years (range: 19–61) and time to surgery was 109.1 ± 12.5 weeks (range: 8–526). There were no differences regarding demographic data between groups. One patient (group B) had a tear of the posterior horn of the lateral meniscus, which was successfully resolved by all inside sutures.
Tibial slope
The mean TS measured 8.6° ± 3.0° (range 2–15°) for the surgically treated knee and 9.5° ± 3.0° (range 4–16°) for the contralateral knee. Pearson correlation analysis showed a significant correlation between the postoperative SSD of PTT and TS in the overall patient cohort (p = 0.0037) with r = -0.43 and R2 = 0.18 (see Fig. 3). However, there was no direct correlation between TS and the clinical outcome (Lysholm and IKDC-Score). The ICC demonstrated strong agreement for both intra-observer reliability (0.93, 95% CI: 0.887–0.938) and inter-observer reliability (0.86, 95% CI: 0.810–0.890) in the measurement of the TS.
Fig. 3.
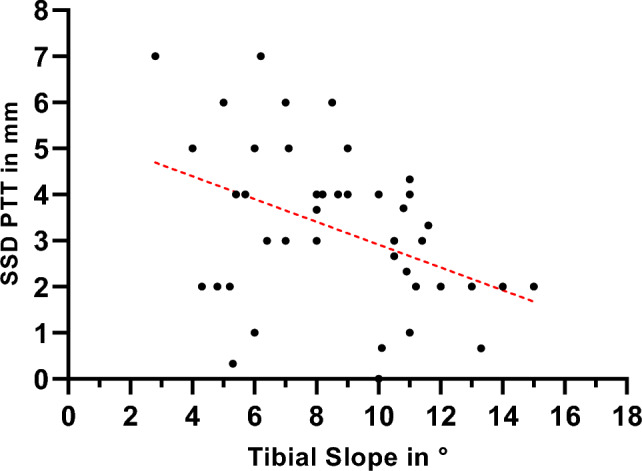
Regression Plot showing a negative association between postoperative SSD of PTT and TS. The central dotted line is the calculated regression line, indicating a significant correlation between TS and SSD of PTT (r = -0.43 and R2 = 0.18; p = 0.0037). SSD of PTT Side- to-side difference of posterior tibial translation
Patient reported functional outcome
The Lysholm Score averaged at 83.0 ± 9.3 and IKDC Score at 73.5 ± 14.5 points at follow-up and showed no difference between groups (see Table 2).
Table 2.
The Table presents demographics, clinical outcomes and complications categorized by TS
| Characteristics | Total (n = 47) | TS < 8° (n = 16) | TS ≥ 8° (n = 31) | p-value |
|---|---|---|---|---|
| Female sexb | 11 (23.4) | 2 (12.5) | 9 (29.0) | n.s |
| Age in yearsa | 37.0 ± 12.0 | 39.2 ± 10.9 | 36.2 ± 13.2 | n.s |
| BMI in kg/m2a | 26.06 ± 3.9 | 26.3 ± 3.9 | 26.2 ± 4.0 | n.s |
| Time to surgery in weeksa | 109.1 ± 12.5 | 106.8 ± 11.2 | 110.4 ± 12.9 | n.s |
| Meniscal tearb | 1 (2.1) | 0 | 1 (3.2) | n.s |
| Arcierob | 36 (78.7) | 13 (81.3) | 23 (74.2) | n.s |
| Follow-up, in monthsa | 17.7 ± 4.7 | 17.6 ± 4.9 | 16.9 ± 4.5 | n.s |
| PROMSa | ||||
| ▪ Lysholm Score | 83.0 ± 9.3 | 82.7 ± 8.7 | 83.2 ± 8.9 | n.s |
| ▪ IKDC Score | 73.5 ± 14.5 | 75.3 ± 13.4 | 70.1 ± 16.1 | n.s |
| SSD of PTT in mma | 3.2 ± 1.7 | 3.9 ± 2.1 | 2.8 ± 1.5 | 0.0457 |
| Graft failureb | 1 (2.1) | 1 (6.3) | 0 | n.s |
| Joint stiffnessb | 1 (2.1) | 0 | 1 (3.2) | n.s |
Group A (TS < 8°) had a significantly higher SSD of PTT (3.9 mm ± 2.1 vs. 2.8 mm ± 1.5, p = 0.0457
aMean ± SD
bn (in %); SSD of PTT Side- to-side difference of posterior tibial translation; TS Tibial Slope; Bold text indicating p < 0.05
Posterior tibial translation
The mean postoperative SSD of PTT was calculated as 3.2 mm ± 1.7 (range 0–7). Group A (TS < 8°), exhibited a significantly higher SSD of PTT in comparison to Group B (TS ≥ 8°): Group A: 3.9 mm ± 2.1 vs. Group B: 2.8 mm ± 1.5; p = 0.0457 (see Table 2). A negative correlation between SSD of PPT and Lysholm Score (r = -0.41 and R2 = 0.17; p = 0.0048), but not IKDC Score was shown (see Fig. 4).
Fig. 4.
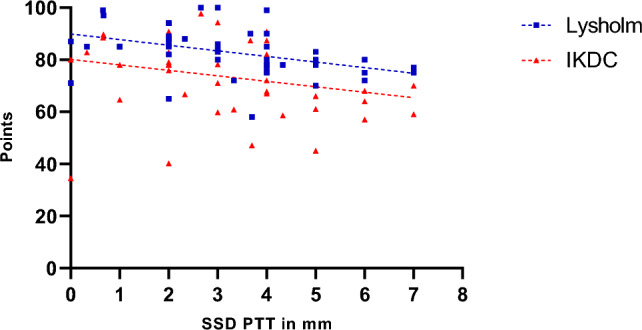
Regression Plot showing a negative association between SSD PTT and Lysholm Score (r = -0.41 and R2 = 0.17; p = 0.0048) but not IKDC-Score (r = -0.26 and R2 = 0.65; p = 0.0858). SSD of PTT Side-to-side difference of posterior tibial translation
Subgroups
The Lysholm Score and IKDC Score were significantly higher in patients with postoperative SSD of PTT < 4 mm and BMI < 30 kg/m2 compared to those with postoperative SSD of PTT ≥ 4 mm and BMI ≥ 30 kg/m2, respectively (Lysholm: SSD of PTT < 4 mm vs. SSD of PTT ≥ 4 mm, p = 0.0006; IKDC: BMI < 30 kg/m2 vs. BMI ≥ 30 kg/m2, p = 0.0484). If postoperative SSD of PTT was ≥ 4 mm, no patient achieved a Lysholm or IKDC Score ≥ 90 points. There were no differences in PROMs between different surgical techniques (Arciero vs. LaPrade). (See Table 3).
Table 3.
Table showing Lysholm and IKDC Scores divided into subgroups
| Subgroups | n | Lysholma | p-value | IKDCa | p-value |
|---|---|---|---|---|---|
| SSD of PTT < 4 mm | 27 | 85.7 ± 10.1 | 0.0006 | 76.0 ± 16.0 | n.s |
| SSD of PTT ≥ 4 mm | 20 | 79.2 ± 6.6 | 69.9 ± 11.4 | ||
| BMI < 30 kg/m2 | 38 | 81.1 ± 7.3 | n.s | 75.1 ± 13.5 | 0.0484 |
| BMI ≥ 30 kg/m2 | 9 | 83.5 ± 9.7 | 75.1 ± 13.5 | ||
| Arciero | 36 | 82.5 ± 9.1 | n.s | 72.7 ± 14.6 | n.s |
| LaPrade | 11 | 84.9 ± 10.2 | 75.8 ± 14.3 |
The Lysholm Score was significantly higher in patients with postoperative SSD of PTT < 4 mm (85.7 ± 10.1 vs. 79.2 ± 6.6, p = 0.0006), while the IKDC Score was higher in patients with a BMI < 30 kg/m2 (75.1 ± 13.5 vs. 75.1 ± 13.5, p = 0.0484)
aMean ± SD; Bold text indicating p < 0.05; SSD of PTT Side-to-side difference of posterior tibial translation
Complications
No patients experienced complications such as vascular or nerve injury, compartment syndrome, deep vein thrombosis, or infection. Only one patient reported joint stiffness (range of motion 0–5–110°), which was resolved by arthroscopic arthrolysis after 46 weeks (range of motion at last follow-up 0–0–125°). In another case, a dislocated femoral PCL flipbutton was noticed during postoperative X-Ray and required revision surgery.
PCL-graft failure occurred in one patient with a TS < 8° (see Table 2), who experienced a non-traumatic re-rupture and required revision PCL reconstruction. The patient's SSD of PTT was 5 mm during the final follow-up.
Discussion
The main finding of this retrospective study on chronic Fanelli type B combined with PCL injuries is that a TS of less than 8° is associated with higher rates of persisting posterior instability after combined anatomic PCL and PLC reconstruction. Additionally, a flattened TS is linked to increased postoperative tibial translation (SSD of PTT) which ultimately leads to worse clinical outcome (Lysholm-Score).
This study is the first to suggest a potential correlation between TS and PTT in patients undergoing PCL reconstruction concurrently with anatomic posterolateral reconstruction based on a defined preoperative classification according to Fanelli. The findings indicate that an elevated TS results in diminished in situ forces acting on the PCL, aligning with previously documented outcomes [17, 31]. The direct association between TS and tibial translation during weightbearing has been established in both cadaveric models [34, 37] and clinical investigations [5, 11, 17]. The knee’s geometric attributes have a significant impact on clinical outcomes. This is demonstrated by the connection between a flattened TS and increased residual PTT [31, 42]. This association remains consistent even after PCL and PLC reconstruction, leading to a reduced reduction in PTT. Importantly, neither surgical technique nor BMI demonstrated a significant impact on the extent of SSD of PTT, which emphasizes the influence of TS on postoperative knee stability. Furthermore, we found a negative correlation between SSD of PTT and the Lysholm Score, suggesting improved clinical outcomes in stable knees. Specifically, patients with a noteworthy SSD of PTT of < 4 mm and a BMI below 30 kg/m2 exhibited significantly higher Lysholm and IKDC Scores, respectively. These findings are consistent with previous research examining patient-reported outcome measures and the restoration of stability, confirming positive outcomes [26, 33, 39, 41]. However, to the best of our knowledge, a cut of value of 4 mm SSD of PTT has never been described in PCL/PLC-deficient knees and needs to be re-evaluated in future research.
Complete restoration of knee kinematics in PLC reconstruction remains elusive, contributing to the failure of a significant number of patients to achieve full recovery [27, 29]. Previous research has primarily focused on PCL/ PLC reconstruction techniques and improper tunnel placement [21, 28, 29]. Building upon previous evidence linking ACL graft failure to TS, as reported by Salmon et al., who documented an 11-fold higher rate of ACL graft failure in patients with a TS of ≥ 12° [8, 30]. This finding aligns with the observations of Gwinner et al. [17], who conducted a subgroup analysis of the patient cohort based on their TS. Notably, they demonstrated a significantly lower reduction in PTT in patients with TS ranging from 5 to 8° compared to those with TS exceeding 8°, with extensive load leading to graft failure. The study by Gwinner et al. [17] has some limitations. These include the use of a non-anatomic PLC reconstruction technique (according to Larson et al. [35]), a lack of preoperative classification of instability, absence of clinical scores, and a mean postoperative SSD of PTT of 4.8 ± 3.3 mm at 12 months and 5.4 ± 3.4 mm at final follow-up, indicating a high failure rate according to our criteria (> 6 mm SSD of PTT). Non-anatomic PLC reconstruction techniques may have a greater influence on the clinical result and remaining postoperative instability compared to more anatomic techniques. However, it is worth noting that Gwinner et al. [17] conducted a long-term observation, which is a strength of their study and a limitations of our presented data. A recent study on patients with PCL reconstruction found that a higher tibial slope (TS) was protective against a positive posterior drawer test, which is also consistent with our findings [9]. The average TS in patients with a positive drawer test was 6.2°, while those with a negative drawer test had an average TS of 8.3°. However, they did not find a correlation between TS and Lysholm or IKDC scores, nor with graft failure.
In recent decades, there has been a growing emphasis on correcting osseous malalignment, extending beyond the coronal plane to address sagittal plane issues, particularly in the context of chronic PCL/PLC instability. An elevated TS can offer protection to the grafts used for combined PCL/PLC reconstruction. While no standardized threshold exists for the degree of slope necessitating concurrent osteotomy, literature indicates potential benefits for patients with flat preoperative TS undergoing slope-increasing osteotomy. Bernhardson et al. [4] found a mean TS of 5.7 in PCL-injured patients compared to 8.6 in those without PCL injury. Weiler et al. [40], studying six patients with chronic PCL deficiency undergoing anterior opening wedge high tibial osteotomy, observed a mean preoperative TS of 3.7°, rising to 11.5° postoperatively. As a result, Kanakamedala et al. suggested considering slope-increasing osteotomy for primary PCL reconstruction with TS less than 5° and, in revision scenarios, for TS less than 7° [20]. Our study, constrained by sample size and ROC analysis limitations, did not pinpoint a specific threshold value.
Limitations
Conclusions drawn from this study are constrained by the small number of cases, a consequence of the rare occurrence of these complex injuries. While precise inclusion and exclusion criteria were employed, there was variability in the time between injury and surgery, albeit consistently exceeding 6 weeks, defining them as chronic injuries. Clinical follow-up utilized Rolimeter instead of stress radiographs. TS quantification relied on lateral views from standard radiographs, potentially overlooking asymmetries in the tibial plateau facets, as well as chondral or meniscal surfaces [10, 36]. The rarity of PLC injuries precluded matched-pair analysis. Long-term follow-up is essential to substantiate the feasibility of arthroscopic PLC reconstruction, given recent promising results.
Conclusion
In this scoping study, a tibial slope of less than 8° is associated with higher rates of posterior tibial translation in combined PLC and PCL reconstruction. The tibial slope was negatively correlated with posterior tibial translation, emphasizing the importance of bony alignment for stability. Patients with a SSD of PTT < 4 mm showed better Lysholm Scores, underlining the effect of stability on clinical outcome. The evidence provided suggests that the tibial slope should be considered in the decision-making process for surgeons, particularly in revision surgery. Further studies are needed to determine specific threshold values for slope correction osteotomy in PLC/PCL deficient knees.
Abbreviations
- ACL
Anterior cruciate ligament
- BMI
Body mass index
- IKDC
International Knee Documentation Committee
- ICRS
International Cartilage Repair Society
- ICC
Intraclass correlation coefficient
- LCL
Lateral collateral ligament
- MCL
Medial collateral ligament
- PCL
Posterior cruciate ligament
- PLC
Posterolateral corner
- PROMs
Patient-reported outcome measures
- PTT
Posterior tibial translation
- SD
Standard deviations
- SSD
Side-to-side difference
- TS
Tibial slope
- VAS
Visual analog scale
Author contributions
Conceptualization HF, SW, KHF, MK Methodology SW, HF, RA, MK Validation HF, SW, AK, KHF, RA, MK; Formal analysis HF, SW, MK.; Investigation HF, AK, SW; Writing—original draft preparation HF; Writing—review and editing all authors; Visualization HF; Supervision KHF, MK; Project administration RA, MK, KHF.; All authors have read and agreed to the final version of this manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Data availability
The data that support the findings of this study are available upon reasonable request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the institutional Ethics Committee of the University of Hamburg (2021–100677-BO-ff).
Informed consent
Informed consent was obtained of each study participant prior to inclusion.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Agneskirchner JD, Hurschler C, Stukenborg-Colsman C, Imhoff AB, Lobenhoffer P (2004) Effect of high tibial flexion osteotomy on cartilage pressure and joint kinematics: a biomechanical study in human cadaveric knees. Winner of the AGA-DonJoy Award 2004. Arch orthop Trauma Surg. 124(9):575–584 [DOI] [PubMed] [Google Scholar]
- 2.Ahmad R, Patel A, Mandalia V, Toms A (2016) Posterior tibial slope: effect on, and Interaction with, knee kinematics. JBJS Rev 4(4):e31-36 [DOI] [PubMed] [Google Scholar]
- 3.Arciero RA (2005) Anatomic posterolateral corner knee reconstruction. Arthroscopy 21(9):1147 [DOI] [PubMed] [Google Scholar]
- 4.Bernhardson AS, DePhillipo NN, Daney BT, Kennedy MI, Aman ZS, LaPrade RF (2019) Posterior tibial slope and risk of posterior cruciate ligament injury. Am J Sports Med 47(2):312–317 [DOI] [PubMed] [Google Scholar]
- 5.Beynnon BD, Fleming BC, Labovitch R, Parsons B (2002) Chronic anterior cruciate ligament deficiency is associated with increased anterior translation of the tibia during the transition from non-weightbearing to weightbearing. J Orthop Res 20(2):332–337 [DOI] [PubMed] [Google Scholar]
- 6.Boksh K, Ghosh A, Narayan P, Divall P, Aujla R (2023) Fibular- versus tibiofibular-based reconstruction of the posterolateral corner of the knee: a systematic review and meta-analysis. Am J Sports med. 10.1177/03635465221138548 [DOI] [PubMed] [Google Scholar]
- 7.Boksh K, Ghosh A, Narayan P, Divall P, Aujla R (2023) Fibular- versus tibiofibular-based reconstruction of the posterolateral corner of the knee: a systematic review and meta-analysis. Am J Sports Med 51(14):3880–3892 [DOI] [PubMed] [Google Scholar]
- 8.Christensen JJ, Krych AJ, Engasser WM, Vanhees MK, Collins MS, Dahm DL (2015) Lateral tibial posterior slope is increased in patients with early graft failure after anterior cruciate ligament reconstruction. Am J Sports Med 43(10):2510–2514 [DOI] [PubMed] [Google Scholar]
- 9.Conyer RT, Allen TG, Reinholz AK et al (2024) Effect of posterior tibial slope on outcomes after posterior cruciate ligament reconstruction. Orthop J Sports Med 12(3):23259671241236804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dare DM, Fabricant PD, McCarthy MM et al (2015) Increased lateral tibial slope is a risk factor for pediatric anterior cruciate ligament injury: an MRI-based case-control study of 152 patients. Am J Sports Med 43(7):1632–1639 [DOI] [PubMed] [Google Scholar]
- 11.Dejour H, Bonnin M (1994) Tibial translation after anterior cruciate ligament rupture. Two radiological tests compared. J Bone Joint Surg. 76(5):745–749 [PubMed] [Google Scholar]
- 12.Domnick C, Frosch KH, Raschke MJ et al (2017) Kinematics of different components of the posterolateral corner of the knee in the lateral collateral ligament-intact state: a human cadaveric study. Arthroscopy 33(10):1821-1830.e1821 [DOI] [PubMed] [Google Scholar]
- 13.Fahlbusch H, Weiß S, Landenberger J et al (2024) Arthroscopic and open reconstruction of the posterolateral corner of the knee have equally good clinical results: first results of a prospective 12-month follow-up study. Arch Orthop Trauma Surg 144(6):2745–2752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fanelli GC, Larson RV (2002) Practical management of posterolateral instability of the knee. Arthroscopy 18(2 Suppl 1):1–8 [DOI] [PubMed] [Google Scholar]
- 15.Frings J, Kolb JP, Drenck TC et al (2019) Anatomic reconstruction of the posterolateral corner: an all-arthroscopic technique. Arthrosc Tech 8(2):e153–e161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Giffin JR, Stabile KJ, Zantop T, Vogrin TM, Woo SL, Harner CD (2007) Importance of tibial slope for stability of the posterior cruciate ligament deficient knee. Am J Sports Med 35(9):1443–1449 [DOI] [PubMed] [Google Scholar]
- 17.Gwinner C, Weiler A, Roider M, Schaefer FM, Jung TM (2017) Tibial slope strongly influences knee stability after posterior cruciate ligament reconstruction: a prospective 5- to 15-year follow-up. Am J Sports Med 45(2):355–361 [DOI] [PubMed] [Google Scholar]
- 18.Hewett TE, Noyes FR, Lee MD (1997) Diagnosis of complete and partial posterior cruciate ligament ruptures. Stress radiography compared with KT-1000 arthrometer and posterior drawer testing. Am J Sports Med 25(5):648–655 [DOI] [PubMed] [Google Scholar]
- 19.Jojima H, Whiteside LA, Ogata K (2004) Effect of tibial slope or posterior cruciate ligament release on knee kinematics. Clin Orthop Related Res. 426:194–198 [DOI] [PubMed] [Google Scholar]
- 20.Kanakamedala AC, Gipsman A, Lowe DT, Strauss EJ, Alaia MJ (2022) Combined anterior opening-wedge high tibial osteotomy and tibial tubercle osteotomy with posterior cruciate ligament reconstruction. Arthrosc Tech 11(4):e601–e608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim YM, Lee CA, Matava MJ (2011) Clinical results of arthroscopic single-bundle transtibial posterior cruciate ligament reconstruction: a systematic review. Am J Sports Med 39(2):425–434 [DOI] [PubMed] [Google Scholar]
- 22.Kolb JP, Frings J, Krause M, Hartel M, Frosch KH (2019) An all-arthroscopic technique for complex posterolateral corner reconstruction. Arthrosc Tech 8(9):e999–e1006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.LaPrade RF, Johansen S, Wentorf FA, Engebretsen L, Esterberg JL, Tso A (2004) An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med 32(6):1405–1414 [DOI] [PubMed] [Google Scholar]
- 24.LaPrade RF, Wozniczka JK, Stellmaker MP, Wijdicks CA (2010) Analysis of the static function of the popliteus tendon and evaluation of an anatomic reconstruction: the “fifth ligament” of the knee. Am J Sports Med 38(3):543–549 [DOI] [PubMed] [Google Scholar]
- 25.Li L, Li J, Zhou P et al (2023) Decreased medial posterior tibial slope is associated with an increased risk of posterior cruciate ligament rupture. Knee Surg Sports Traumatol Arthrosc 31(7):2966–2973 [DOI] [PubMed] [Google Scholar]
- 26.Liu P, Gong X, Zhang J, Ao Y (2020) Anatomic, all-arthroscopic reconstruction of posterolateral corner of the knee: a cadaveric biomechanical study. Arthroscopy 36(4):1121–1131 [DOI] [PubMed] [Google Scholar]
- 27.MacGillivray JD, Stein BE, Park M, Allen AA, Wickiewicz TL, Warren RF (2006) Comparison of tibial inlay versus transtibial techniques for isolated posterior cruciate ligament reconstruction: minimum 2-year follow-up. Arthroscopy 22(3):320–328 [DOI] [PubMed] [Google Scholar]
- 28.Noyes FR, Barber-Westin SD (2005) Posterior cruciate ligament revision reconstruction, part 1: causes of surgical failure in 52 consecutive operations. Am J Sports Med 33(5):646–654 [DOI] [PubMed] [Google Scholar]
- 29.Petrigliano FA, Suero EM, Voos JE, Pearle AD, Allen AA (2012) The effect of proximal tibial slope on dynamic stability testing of the posterior cruciate ligament- and posterolateral corner-deficient knee. Am J Sports Med 40(6):1322–1328 [DOI] [PubMed] [Google Scholar]
- 30.Salmon LJ, Heath E, Akrawi H, Roe JP, Linklater J, Pinczewski LA (2018) 20-year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: the catastrophic effect of age and posterior tibial slope. Am J Sports Med 46(3):531–543 [DOI] [PubMed] [Google Scholar]
- 31.Schatka I, Weiler A, Jung TM, Walter TC, Gwinner C (2018) High tibial slope correlates with increased posterior tibial translation in healthy knees. Knee Surg, Sports Traumatol, Arthrosc 26(9):2697–2703 [DOI] [PubMed] [Google Scholar]
- 32.Schulz MS, Russe K, Lampakis G, Strobel MJ (2005) Reliability of stress radiography for evaluation of posterior knee laxity. Am J Sports Med 33(4):502–506 [DOI] [PubMed] [Google Scholar]
- 33.Sharma A, Saha P, Bandyopadhyay U (2022) Reconstruction of the posterolateral corner of the knee using laprade and modified larson technique: a prospective study. Indian J Orthop 56(1):125–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shoemaker SC, Markolf KL (1986) The role of the meniscus in the anterior-posterior stability of the loaded anterior cruciate-deficient knee. Effects of partial versus total excision. J Bone Joint Surg Am. 68(1):71–79 [PubMed] [Google Scholar]
- 35.Sidles JA, Larson RV, Garbini JL, Downey DJ, Matsen FA 3rd (1988) Ligament length relationships in the moving knee. J Orthop Res 6(4):593–610 [DOI] [PubMed] [Google Scholar]
- 36.Simon RA, Everhart JS, Nagaraja HN, Chaudhari AM (2010) A case-control study of anterior cruciate ligament volume, tibial plateau slopes and intercondylar notch dimensions in ACL-injured knees. J Biomech 43(9):1702–1707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Torzilli PA, Deng X, Warren RF (1994) The effect of joint-compressive load and quadriceps muscle force on knee motion in the intact and anterior cruciate ligament-sectioned knee. Am J Sports Med 22(1):105–112 [DOI] [PubMed] [Google Scholar]
- 38.Treme GP, Salas C, Ortiz G et al (2019) A biomechanical comparison of the arciero and laprade reconstruction for posterolateral corner knee injuries. Orthop J Sports Med 7(4):2325967119838251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.van Gennip S, van der Wal WA, Heesterbeek PJC, Wymenga AB, Busch V (2020) Posterolateral corner reconstruction in combined injuries of the knee: Improved stability with Larson’s fibular sling reconstruction and comparison with LaPrade anatomical reconstruction. Knee 27(1):124–131 [DOI] [PubMed] [Google Scholar]
- 40.Weiler A, Dickschas J, Gwinner C (2021) Anterior open-wedge osteotomy in posterior cruciate ligament deficient knees: from a historical perspective to first clinical results. J Knee Surg 34(6):592–598 [DOI] [PubMed] [Google Scholar]
- 41.Weiss S, Krause M, Frosch KH (2023) Clinical results after arthroscopic reconstruction of the posterolateral corner of the knee: a prospective randomized trial comparing two different surgical techniques. Arch Orthop Trauma Surg 143(2):967–975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yoon KH, Lee JH, Kim SG et al (2023) Effect of posterior tibial slopes on graft survival rates at 10 years after primary single-bundle posterior cruciate ligament reconstruction. Am J Sports Med 51(5):1194–1201 [DOI] [PubMed] [Google Scholar]
- 43.Zawodny SR, Miller MD (2010) Complications of posterior cruciate ligament surgery. Sports Med Arthrosc Rev 18(4):269–274 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available upon reasonable request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.