Abstract
BACKGROUND:
Heart failure (HF), or congestive Heart failure (CHF), is a heart disorder with a number of symptoms caused by the heart’s inability to pump blood. Our aim in conducting this study is to investigate the adherence to dietary approaches to stop hypertension (DASH) diet components and the risk of HF in Iranian adult women and men.
METHODS:
In this hospital-based, case-control study, we included 340 participants (194 men and 146 women) aged 30–70 years who were recently (less than 6 months) diagnosed with HF. In this study, there were 169 participants in the control group and 171 participants in the case group. A semi-quantitative food frequency questionnaire (FFQ) with 148 items was used to assess food intake. Multiple logistic regression statistical tests were used to evaluate the relationship between DASH score and HF.
RESULTS:
After adjusting for confounding variables, the data showed that adherence to the DASH diet was associated with a reduced risk of HF. Our data show that a significant relationship was found between the consumption of fruits (OR: 0.62; 95% CI: 0.53-0.68), vegetables (OR: 0.53; 95% CI: 0.28-0.81), legumes and nuts (OR: 0.75; 95% CI: 0.65-0.68), and heart failure, but no significant relationship was found with the other components of the DASH diet and heart failure.
CONCLUSION:
Findings suggest that there is an inverse relationship between adherence to the DASH-style diet and the likelihood of HF, and adherence to some components of the DASH diet was also effective in reducing the risk of HF. To obtain more complete results, it is necessary to conduct cohort studies and randomized clinical trials.
Key Words: Heart Failure, Congestive Heart Failure, Diet, DASH Diet, Cardiovascular Diseases
Introduction
Cardiovascular diseases are currently one of the most common chronic diseases and the main cause of death worldwide. Due to the increase in life expectancy in the general population, especially in developing countries such as Iran, heart failure (HF) has become a major public health problem1. It is estimated that more than 26 million people in the world have heart failure2.
In heart failure, the heart is not able to pump blood in proportion to the body weight. In other words, the heart is very weak, and there are many reasons for HF, the most important of which include coronary artery disease, heart attack, and high blood pressure3. In general, HF is seen in the left, right, or both parts. In biventricular HF, both sides of the heart are affected; however, HF is more common on the left side4,5. Systemic inflammation is often present in patients with acute and chronic HF6,7. A number of inflammatory mediators and cytokines are involved in the pathophysiology of HF, including high-sensitivity C-reactive protein (hsCRP), tumor necrosis factor-alpha (TNF-α), and a number of interleukins8,9.
Dietary Approaches to Stop Hypertension (DASH) is a type of eating style that recommends increased consumption of fruits, vegetables, whole grains, fish, nuts, dairy products, and vegetable oils. Also, in this diet, the consumption of processed meats, simple sugars, desserts, alcohol, and fats has decreased10. In the DASH food pattern, there is a higher consumption of nutrients such as potassium, calcium, magnesium, fiber, and vegetable proteins, as well as a lower consumption of refined carbohydrates and saturated fats, which play a key role in controlling blood pressure11.
A wide variety of studies have shown that following the DASH diet can be associated with a reduced risk of heart problems12,13. The DASH diet has been proven to reduce inflammation14, weight15, blood pressure16, metabolic syndrome17, diabetes18, and cancer19,20. Although many studies have shown the effect of the DASH diet in reducing the incidence of heart diseases, no case-control study has yet been conducted regarding the role of the DASH diet and its components in reducing the incidence of HF. Several studies have shown that the components of the DASH diet (whole grains, dairy products, and lower amounts of red meat, sodium, and added sugar) are associated with a reduced risk of heart disease21,22. Additionally, to our knowledge, the data on the relationship between adherence to the DASH diet and HF are mainly limited to Western countries, with little evidence from less developed countries. Therefore, our purpose in conducting this case-control study is to investigate and analyze adherence to the DASH dietary pattern in relation to HF in Iranian adults.
Methods
Study design and population
The design of this study is case-control, conducted on 194 men and 146 women aged 30-70. The cases were chosen from patients with HF, diagnosed by a cardiologist in the last six months, who were referred to the HF department of Chamran Hospital, Isfahan, Iran, from July 2023 to December 2023. HF was defined based on signs and symptoms diagnosed and recorded by a cardiologist and confirmed histologically at the Cardiovascular Research Center and HF Clinic in Chamran Hospital.
The control group was selected using the companion control method after screening for eligibility. Cases and controls who met any of the following criteria were excluded: 1) incomplete questionnaires, 2) lack of consent to participate, 3) taking special supplements, 4) following special diets, or 5) diagnosed with malignancy and cancer. Finally, 171 cases and 169 controls were included in the study. Written consent was obtained from all participants. The Medical Ethics Committee at Isfahan University of Medical Sciences approved the study protocol (IR.MUI.RESEARCH.REC.1402.168).
Dietary assessment
A valid and reliable FFQ semi-questionnaire with 148 items23 was used to assess dietary food intake for both groups. The frequency and amount of food consumed were converted into grams per day and recorded daily, weekly, or monthly over the past year. A customized version of Nutritionist IV software was used for diet analysis.
Calculation of DASH score
Fung’s standard method was used to score the DASH diet24. In this study, to eliminate the effect of the individual’s energy intake on the components of the DASH score, the intake of each food group was estimated per 1000 kcal. We calculated the DASH score for eight components of this diet, and the calculation of this score determines the degree of compliance of the individual to this diet. Consuming low amounts of sodium, sweets, sugar-sweetened beverages, and processed red meat, as well as consuming high amounts of low-fat dairy products, whole grains, nuts and legumes, fruits, and vegetables, were considered. In scoring the DASH diet, the highest score was given to the people who followed the DASH diet the most. Conversely, the lowest score was given to people who had the least adherence to the DASH diet. This scoring method was also used for sodium, sweets, and red or processed meats. Finally, a total DASH score (ranging from 8 to 40) was given to each participant.
Anthropometric assessment
Trained experts collected anthropometric data from all subjects using standardized methods and calibrated devices. Height without shoes was measured using a standard tape, and body weight was measured with bare feet and light clothes using an Olympia scale. Body mass index (BMI) was calculated using the formula: weight (kg) divided by the square of height (m²). Waist circumference (WC) and hip circumference were measured with an accuracy of 0.1 cm at the maximum circumference of the hip. All measurements were performed by an expert to limit observer error and were carried out based on National Institutes of Health guidelines25. Physical activity was assessed by a validated questionnaire26.
Evaluation of other variables
Using a pre-tested questionnaire, we collected information about age, marital status, place of residence, alcohol consumption, and smoking status, which was categorized as never, current, or former. In the case of alcohol consumption, any amount of alcohol consumed during a month was defined as an alcohol user, and in the case of smoking, one cigarette per day was defined as a cigarette user. We also collected information on cardiovascular disease history, based on self-reporting and medical documentation. Diabetes was defined as the use of anti-hyperglycemic drugs, while hypertension was defined by the use of antihypertensive drugs. Systolic and diastolic blood pressures were measured twice, at least 15 minutes apart, by a trained person using a mercury sphygmomanometer on the right arm while the participant was seated. The average of these measurements was recorded27. The questionnaire was completed for all participants through face-to-face interviews.
Statistical analysis
SPSS software version 21.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The Kolmogorov-Smirnov test was used to determine the normality of the data. For data with a normal distribution, the mean ± standard deviation was used, and for data with a non-normal distribution, the median and interquartile range were used. Qualitative variables were reported as frequency and percentage. The participants were divided into the following four groups based on the cut point for adherence to the DASH diet: T1: <20, T2: 21-24, T3: 25-28, and T4: ≥29. Statistical analyses, including simple t-tests, chi-square tests, ANOVA, and multivariate logistic regression, were conducted. Statistically significant results were determined by p-values of <0.05 (two-tailed). Odds ratios (OR) and 95% confidence intervals (CI) were used to report the results of the multivariate logistic regression. Confounding factors such as BMI (kg/m²), sex, age (years), alcohol consumption, physical activity (MET (hour/day)), smoking, diabetes history, family history of coronary heart disease, marital status, and place of residence were included in the final models of statistical analysis. A p-value < 0.05 was considered statistically significant, and all p-values reported were two-tailed.
Results
The anthropometric and demographic parameters of the participants in the case and control groups are presented in Table 1. Regarding age, physical activity, residency, alcohol consumption, smoking status, family history of coronary heart disease (CHD), marital status, and blood pressure, no statistically significant differences were observed between the participants in the case HF and control groups. However, the case group reported a lower daily caloric intake compared to the control group, with a mean ± SD of total energy (kcal/d): 2075 ± 324.5 versus 2254.2 ± 112.14 (p < 0.001), and BMI: 30.23 ± 1.37 versus 27.41 ± 2.48 (p < 0.001).
Table.1.
General characteristics of people participating in the study based on HF and control group.
| variable |
Total
N=340 |
Controls
N=169 |
Cases
N=171 |
P value | |
|---|---|---|---|---|---|
| sex | women | 146(42.94) | 76(52.05) | 70(47.94) | 0.087 |
| men | 194(57.05) | 93(47.93) | 101(52.03) | ||
| BMI ( Kg/m 2 ) | 29.58±7.58 | 27.41±2.48 | 30.23±1.37 | ≤0.001 | |
| Age (years) | 62.7±7.7 | 59.3±3.5 | 64.5±6.3 | 0.179 | |
| Total energy (kcal/d) | 2088.1±248.32 | 2254.2± 112.14 | 2075 ± 324.5 | ≤0.001 | |
| Physical activity (MET (hour/day)) | low | 263(77.35) | 130(49.42) | 133(50.57) | 0.627 |
| moderate | 46(13.52) | 25(54.34) | 21(45.65) | ||
| high | 32(9.41) | 17(53.12) | 15(46.87) | ||
| Hypertension (positive) | yes | 103(30.29) | 47(45.63) | 56(54.36) | 0.115 |
| Alcohol (drinking) | never | 265(77.94) | 123(46.41) | 142(53.58) | 0.069 |
| current | 63(18.52) | 41(65.07) | 22(30.77) | ||
| former | 12(3.52) | 7(58.33) | 5(41.66) | ||
| Smoking (active or past) | never | 215(63.23) | 116(53.95) | 99(46.04) | 0.211 |
| current | 80(23.52) | 34(42.5) | 46(57.5) | ||
| former | 45(13.23) | 19(42.22) | 26(57.77) | ||
|
Family history
of Coronary heart disease |
yes | 81(23.82) | 39(48.14) | 42(51.85) | 0.766 |
| Diabetes history | yes | 72(21.17) | 23(31.94) | 49(68.05) | 0.094 |
| Marital status | yes | 278(81.76) | 141(50.71) | 137(49.28) | 0.675 |
| place | rural | 95(27.94) | 45(47.36) | 50(52.63) | 0.485 |
| urban | 245(72.05) | 124(50.61) | 121(49.38) | ||
Table 2 shows the main characteristics of the participants according to the DASH diet scoring quartile. We found that patients in the highest quartile of the DASH score had a lower BMI (p < 0.001). However, no other significant relationships were found between the DASH score and the other variables.
Table.2.
The main characteristics of the participants according to quartiles of DASH score.
| Variable |
Total
N=340 |
DASH score quartiles | P value | ||||
|---|---|---|---|---|---|---|---|
|
Q(1) (lowest)
N (%) |
Q(2)
N (%) |
Q(3)
N (%) |
Q(4) (highest) N (%) | ||||
| ≤20 | 21-24 | 25-28 | ≥29 | ||||
| sex | women | 146(42.95) | 61(41.78) | 38(20.02) | 25(17.12) | 22(150.6) | 0.58 |
| men | 194(57.05) | 48(24.74) | 42(21.64) | 54(27.83) | 50(53.19) | ||
| BMI (kg/m 2 ) | 30.78±3.34 | 31.73±3.87 | 30.87±3.74 | 29.50±3.92 | 26.32±3.36 | <0.001 | |
| Age (years) | 62.7±7.7 | 62.57±7.56 | 62.10±7.56 | 62.56±8.09 | 60.86±7.74 | 0.59 | |
| Energy intake (kcal) | 2134.1±248.32 | 2095.5±2380.8 | 2034.8±634.9 | 2142.9±684.2 | 2263.4±452.8 | 0.55 | |
| Physical activity (MET (day)) | low | 293(86.17) | 87(29.69) | 74(25.25) | 69(23.54) | 63(21.50) | 0.39 |
| moderate | 33(9.70) | 11(33.33) | 5(15.15) | 9(27.27) | 8(24.24) | ||
| high | 14(4.11) | 3(21.42) | 3(21.42) | 4(28.57) | 4(28.57) | ||
| Hypertension (positive) | yes | 257(75.58) | 87(33.85) | 68(26.45) | 61(23.73) | 52(20.23) | 0.20 |
| Alcohol (drinking) | never | 291(85.58) | 85(29.20) | 72(24.74) | 64(21.99) | 69(23.71) | 0.33 |
| current | 38(11.17) | 14(36.84) | 13(30.77) | 9(7.69) | 2(15.38) | ||
| former | 11(3.23) | 3(27.27) | 4(33.33) | 2(18.2) | 2(18.2) | ||
| Smoking (active or past) | never | 254(74.70) | 57(22.44) | 67(19.70) | 72(21.17) | 58.(17.05) | 0.45 |
| current | 58(17.05) | 21(36.20) | 13(22.41) | 13(22.41) | 11(18.96) | ||
| former | 29(8.52) | 10(34.48) | 7(24.13) | 6(20.68) | 6(20.68) | ||
|
Family history
Of coronary heart disease |
yes | 63(18.52) | 22(34.92 | 18(28.57) | 15(23.80) | 8(12.69) | 0.96 |
| Diabetes history | yes | 72(21.17) | 31(43.05) | 15(20.83) | 14(19.44) | 12(16.66) | ≤0.001 |
| Marital status | yes | 309(95.85) | 8427.18) | 72(21.17) | 99(32.03) | 54(15.88) | 0.79 |
| Place | rural | 75(22.05) | 17(22.66) | 15(20) | 23(30.6) | 20(26.6) | 0.19 |
| urban | 265(77.94) | 84.(31.69) | 69(26.03) | 58(21.88) | 54(20.37) | ||
Table 3 shows the components of the DASH diet as well as macronutrients consumed by participants. Participants with the lowest fat intake had the highest DASH scores (p < 0.001). Participants who consumed the highest amount of carbohydrates and protein had the highest DASH scores (p < 0.001). Individuals with the highest consumption of fruits, vegetables, legumes, and nuts had the highest DASH scores, which was statistically significant (p < 0.001). Also, participants who consumed the lowest amount of sodium, red, and processed meats had the highest DASH scores, although this difference was not statistically significant.
Table 3.
Dietary Macronutrient intake and Components of DASH of the participants according energy-adjusted DASH score. The total received energy was adjusted.
| variable |
Q1
(lowest) ≤20 |
Q2
21-24 |
Q3
25-28 |
Q4
(highest) ≥29 |
P value |
|---|---|---|---|---|---|
| Dietary Macronutrient intake (energy-adjusted) | |||||
| Total fat (g/day) | 110.66±40.26 | 114.39±24.72 | 116.39±24.53 | 109.68±17.36 | <0.001 |
| Total energy (kJ/day) | 1912.5±2380.8 | 2034.8±634.9 | 2142.9±684.2 | 2263.4±452.8 | 0.55 |
| Protein (g/day) | 128.08±114.90 | 104.57±23.02 | 128.84±27.05 | 133.98±18.89 | <0.001 |
| Carbohydrate (g/day) | 527.98±512.56 | 484.21±122.31 | 528.36±123.8 | 576.2±85.14 | <0.001 |
| Components of DASH (serving/day) (energy-adjusted) | |||||
| Fruits | 2.41±1.55 | 4.08±1.41 | 4.43±0.94 | 5±0.00 | <0.001 |
| Vegetables | 2.61±1.48 | 4.71±0.67 | 4.66±0.60 | 4.96±0.19 | <0.001 |
| Nuts and legumes | 3.40±1.15 | 4.15±1.30 | 4.78±0.61 | 5±0.00 | <0.001 |
| Whole grains | 4.50±0.91 | 4.35±0.79 | 4.57±0.56 | 4.92±0.27 | 0.64 |
| Red and processed meat | 4.09±1.34 | 3.94±1.10 | 4.07±0.84 | 3.48±0.50 | 0.32 |
| Low fat dairy product | 1.89±1.10 | 2.29±0.98 | 2.63±1.04 | 2.54±0.90 | 0.473 |
| Sweetened beverage | 5.00±0.00 | 5.00±0.00 | 5.00±0.00 | 5.00±0.00 | 0.999 |
| Sodium | 3.32±1.06 | 3.12±1.37 | 3.02±0.47 | 2.78±0.65 | 0.48 |
The total received energy was adjusted. Values are mean (SD) or number (percentage)
The results of the multivariate logistic regression analysis, presented in Table 4, reveal significant findings. After adjusting for confounding variables—including BMI (kg/m²), age (years), alcohol consumption, smoking, physical activity (MET), family history of CHD, blood pressure, residence, marital status, daily caloric intake, and diabetes—the analysis shows a significant relationship between the consumption of vegetables (OR = 0.62, 95% CI: 0.50–0.68), fruits (OR = 0.53, 95% CI: 0.23–0.81), and whole grains (OR = 0.75, 95% CI: 0.65–0.88) with a lower risk of HF.
Table.4.
Relationship between components of DASH diet and HF
| variable |
crude model
OR (95% CI) |
Adjusted
a
model
OR (95% CI) |
Adjusted
b
model
OR (95% CI) |
Adjusted
c
model
OR (95% CI) |
|---|---|---|---|---|
| Fruits | 0.63(0.57-0.70)* | 0.63(0.56-0.69)* | 0.61(0.57-0.68)* | 0.62(0.53-0.68)* |
| Vegetables | 0.56(0.48-0.68)* | 0.56(0.46-0.68)* | 0.55(0.45-0.67)* | 0.53(0.28-0.81)* |
| Nuts and legumes | 0.76(0.67-0.87)* | 0.77(0.67-0.88)* | 0.75(0.65-0.86)* | 0.75(0.65-0.68)* |
| Whole grains | 0.97(0.74-1.27) | 1.09(0.82-1.45) | 1.12(0.82-1.52) | 1.13(0.83-1.55) |
| Red and processed meat | 1.00(0.52-1.93) | 1.05(0.54-2.03) | 1.01(0.50-2.03) | 1.05(0.52-2.14) |
| Low fat dairy product | 0.74(0.47-1.13) | 0.77(0.49-1.20) | 0.67(0.47-1.07) | 0.68(0.41-1.10) |
| Sodium | 4.13(2.51-6.79) | 4.04(2.49-6.89) | 4.01(2.35-6.83) | 3.93(2.30-6.71) |
Multiple logistic regressions adjusted for confounding factors in multiple models. Adjusted a by sex, age. Adjusted b by model a and BMI, smoking, residence, Family history of CHD, marital, physical activity, Blood pressure and alcohol. Adjusted c by model b and kcal and diabetes.
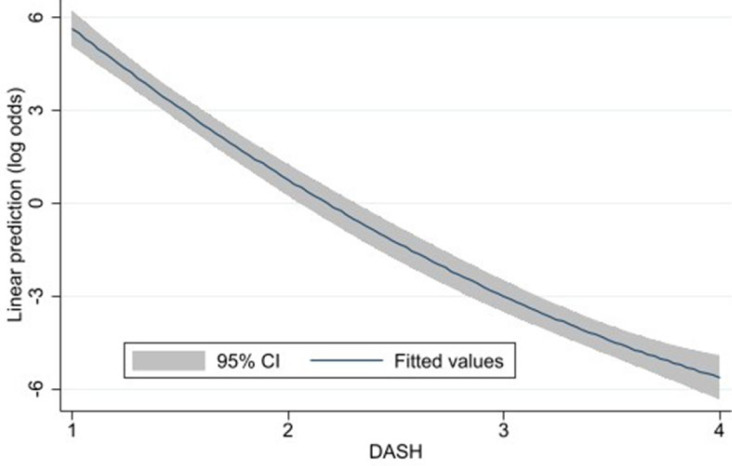
Fig. 1 illustrates that low adherence to the DASH diet is associated with an increased risk of HF, whereas higher adherence to the dietary pattern is linked to a reduced risk of HF.
Fig. 1.
Investigation of adherence to dash diet and occurrence of HF
Discussion
In this study, conducted on patients with HF at Chamran Hospital, Isfahan (Iran), we observed that adherence to the DASH diet, but not all components of the diet, was associated with a reduced risk of HF in adults. Our findings showed that higher consumption of fruits, vegetables, legumes, and nuts is associated with a reduced risk of HF. In other words, these data showed that increased consumption of vegetables, fruits, legumes, and nuts had a significant effect in reducing the risk of HF, although other components of the DASH diet did not show significant differences.
Other results showed that the daily caloric intake in patients could be affected by their heart problems and heart failure, which impacted their appetite. HF leads to dysfunction of the kidneys, liver, stomach, and intestines. This can lead to decreased appetite, nausea, malabsorption, and increased catabolism, resulting in malnutrition and cachexia26. Compared to conventional diets, the DASH diet has lower amounts of harmful compounds such as saturated fats, trans fatty acids, and cholesterol, while being rich in micronutrients that help lower blood pressure, such as potassium, calcium, and magnesium. A number of studies have reported that adherence to the DASH diet reduces insulin resistance and improves lipid profiles27,29, which is valuable for the prevention of cardiovascular disease (CVD). An observational study in Sweden showed that adherence to the DASH diet was associated with reduced heart disease30. Other studies have shown that following the DASH diet in the long term reduces the risk of heart disease31,32. The results of our study are consistent with other studies, but our data emphasized more on the type of DASH diet components, whereas other studies have shown the conclusion in general. This study revealed that there is a significant difference between the consumption of some components of the DASH diet (fruits, vegetables, nuts, and legumes) and reducing the risk of HF.
Major risk factors for HF include myocardial infarction, hypertension, cardiomyopathy, and valvular heart disease33,34. Oxidative stress is one of the main factors for heart diseases. One possible mechanism in the relationship between following the DASH diet and reducing HF is the antioxidant content of this diet. Clinical and experimental studies have shown that HF is aggravated under conditions of oxidative stress35,36. Oxidative stress aggravates HF by disrupting the function of myocardial proteins37. One study showed that HF occurring after myocardial infarction (MI) does not have a good prognosis if it is accompanied by a deficiency of antioxidant factors38. Several clinical studies have shown that improving antioxidant capacity, by enhancing endogenous glutathione (GSH) levels, is promising in HF patients. Several trials showed that increasing the GSH/oxidized GSH ratio (GSSG) is associated with improved heart function in patients with HF and acute MI33,40. A meta-analysis of clinical trial studies found that patients who followed the DASH diet had increased GSH levels41.
Another possible mechanism is the role of the DASH diet in reducing an individual’s body weight. A leftward shift in the Frank-Starling curve occurs in obese subjects due to increased blood volume and preload, leading to left ventricular (LV) dilation and hypertrophy. Also, left atrial enlargement causes changes in LV diastolic filling. All these changes cause diastolic and systolic disorders and finally HF42. Our study found that individuals adhering to the DASH diet had a lower BMI, which may offer protective benefits against cardiovascular disease. Research indicates that reducing obesity can decrease the risk of heart disease and heart attacks, leading to a lower incidence of heart failure43.
The results of a number of studies showed that the DASH diet is associated with a reduction in the risk of cardiovascular diseases. The most important role of this diet is to improve blood pressure in people with cardiovascular diseases and without diabetes21,44. One of the most important parts of the DASH diet is fruits, vegetables, nuts, and legumes. It seems that the role of these components of the DASH diet is more to control an individual’s blood pressure than their antioxidant role15,23. Another possible mechanism for the effect of the DASH diet is the role of fiber in improving the lipid profile and better blood sugar control12.
Although this study provides new information, there are some limitations that should be considered. First, the presence of selection bias in this study cannot be easily avoided, but to minimize this bias, we tried to include the controls within the hospital. Second, it is necessary to design prospective studies for more complete conclusions. There are several strengths of this study. First, based on available data, this study is the first to examine the association between adherence to the DASH diet and heart failure in a case-control study. In addition, we considered both sexes who had recently been diagnosed with HF as the case group. Second, we included a wide range of confounding factors in the study to moderate their effects on the final results. Third, we used a validated FFQ administered by a trained nutritionist, ensuring higher quality and low bias23.
Conclusion
This study revealed an inverse relationship between adhering to DASH diet and HF risk in adult. Overall, our study showed that high consumption of some components of the DASH diet, such as fruits, vegetables, legumes, and nuts, was associated with a reduced risk of HF. In other words, these data revealed that partial adherence to the DASH diet was also associated with a reduced risk of HF. In addition, it is recommended that the DASH diet plan can be valuable in reducing the risk of HF due to its balance and health. To confirm these results and obtain additional results, it is recommended to conduct cohort studies as well as randomized clinical trials in high sample size.
Acknowledgements
The authors are grateful to all the participants in the research, without their presence, this study would not have been possible.
Conflict of interests
The authors declare no conflict of interest.
Funding
The cost of this research was funded by Isfahan University of Medical Sciences.
Author’s Contributions
Formal analysis: MM, Investigation: AA, SMS, RA and MS, Resources:
AA and MS, Writing: AA, RA and MS, Review and editing: RA, MS, DS and SMS,
Visualization: SMS and MS, Supervision: SMS. All authors have read and approved the manuscript.
References
- 1.Bytyçi I, Bajraktari G. Mortality in heart failure patients. Anatol J Cardiol. 2015 Jan;15(1):63–8. doi: 10.5152/akd.2014.5731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Savarese G, Lund LH. Global Public Health Burden of Heart Failure. Card Fail Rev. 2017 Apr;3(1):7–11. doi: 10.15420/cfr.2016:25:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022 May;79(17):e263–e421. doi: 10.1016/j.jacc.2021.12.012. [DOI] [PubMed] [Google Scholar]
- 4.Hirata K, Hyodo E, Hozumi T, Kita R, Hirose M, Sakanoue Y, et al. Usefulness of a combination of systolic function by left ventricular ejection fraction and diastolic function by E/E’ to predict prognosis in patients with heart failure. Am J Cardiol. 2009 May;103(9):1275–9. doi: 10.1016/j.amjcard.2009.01.024. [DOI] [PubMed] [Google Scholar]
- 5.Eshraghi A, Mohammadzadeh Shabestri M, Jalalyazdi M, Alizadeh Sani Z. The Correlation between Left and Right Ventricular Ejection Fractions in Patients with Ischemic Heart Disease, Documented by Cardiac Magnetic Resonance Imaging. J Cardiothorac Med. 2016;4(1):407–10. [Google Scholar]
- 6.Eskandari V, Amirzargar AA, Mahmoudi MJ, Rahnemoon Z, Rahmani F, Sadati S, et al. Gene expression and levels of IL-6 and TNFα in PBMCs correlate with severity and functional class in patients with chronic heart failure. Ir J Med Sci. 2018 May;187(2):359–68. doi: 10.1007/s11845-017-1680-2. [DOI] [PubMed] [Google Scholar]
- 7.Perez AL, Grodin JL, Chaikijurajai T, O’Connor C, Starling RC, Wilson Tang WH, et al. Interleukin-6 and Outcomes in Acute Heart Failure: An ASCEND-HF Substudy. J Card Fail. 2021 Jun;27(6):670–6. doi: 10.1016/j.cardfail.2021.01.006. [DOI] [PubMed] [Google Scholar]
- 8.Szekely Y, Arbel Y. A Review of Interleukin-1 in Heart Disease: Where Do We Stand Today? Cardiol Ther. 2018 Jun;7(1):25–44. doi: 10.1007/s40119-018-0104-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Panahi M, Papanikolaou A, Torabi A, Zhang JG, Khan H, Vazir A, et al. Immunomodulatory interventions in myocardial infarction and heart failure: a systematic review of clinical trials and meta-analysis of IL-1 inhibition. Cardiovasc Res. 2018 Sep;114(11):1445–61. doi: 10.1093/cvr/cvy145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mozaffarian D, Appel LJ, Van Horn L. Components of a cardioprotective diet: new insights. Circulation. 2011 Jun;123(24):2870–91. doi: 10.1161/CIRCULATIONAHA.110.968735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones NRV, Forouhi NG, Khaw KT, Wareham NJ, Monsivais P. Accordance to the Dietary Approaches to Stop Hypertension diet pattern and cardiovascular disease in a British, population-based cohort. Eur J Epidemiol. 2018 Feb;33(2):235–44. doi: 10.1007/s10654-017-0354-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Farhadnejad H, Asghari G, Mirmiran P, Azizi F. Dietary approach to stop hypertension diet and cardiovascular risk factors among 10- to 18-year-old individuals. Pediatr Obes. 2018 Apr;13(4):185–94. doi: 10.1111/ijpo.12268. [DOI] [PubMed] [Google Scholar]
- 13.Shoaibinobarian N, Danehchin L, Mozafarinia M, Hekmatdoost A, Eghtesad S, Masoudi S, et al. The Association between DASH Diet Adherence and Cardiovascular Risk Factors. Int J Prev Med. 2023 Feb;:14–24. doi: 10.4103/ijpvm.ijpvm_336_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rodríguez-López CP, González-Torres MC, Aguilar-Salinas CA, Nájera-Medina O. DASH Diet as a Proposal for Improvement in Cellular Immunity and Its Association with Metabolic Parameters in Persons with Overweight and Obesity. Nutrients. 2021 Oct;13(10):3540. doi: 10.3390/nu13103540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin PH. et al. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study. Arch Intern Med. 2010 Jan;170(2):126–35. doi: 10.1001/archinternmed.2009.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Padma V. DASH Diet in Preventing Hypertension. ABR. 2014;8(2):94–6. [Google Scholar]
- 17.Farhadnejad H, Emamat H, Teymoori F, Tangestani H, Hekmatdoost A, Mirmiran P. Role of Dietary Approaches to Stop Hypertension Diet in Risk of Metabolic Syndrome: Evidence from Observational and Interventional Studies. Int J Prev Med. 2021 Mar;12: 24. doi: 10.4103/ijpvm.IJPVM_108_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peairs AD, Shah AS, Summer S, Hess M, Couch SC. Effects of the dietary approaches to stop hypertension (DASH) diet on glucose variability in youth with Type 1 diabetes. Diabetes Manag (Lond). 2017;7(5):383–91. [PMC free article] [PubMed] [Google Scholar]
- 19.Onvani S, Haghighatdoost F, Azadbakht L. Dietary approach to stop hypertension (DASH): diet components may be related to lower prevalence of different kinds of cancer: A review on the related documents. J Res Med Sci. 2015 Jul;20(7):707–13. doi: 10.4103/1735-1995.166233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mohseni R, Mohseni F, Alizadeh S, Abbasi S. The Association of Dietary Approaches to Stop Hypertension (DASH) Diet with the Risk of Colorectal Cancer: A Meta-Analysis of Observational Studies. Nutr Cancer. 2020;72(5):778–90. doi: 10.1080/01635581.2019.1651880. [DOI] [PubMed] [Google Scholar]
- 21.Chiavaroli L, Viguiliouk E, Nishi SK, Blanco Mejia S, Rahelić D, Kahleová H, et al. DASH Dietary Pattern and Cardiometabolic Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses. Nutrients. 2019 Feb;11(2) doi: 10.3390/nu11020338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ibsen DB, Levitan EB, Åkesson A, Gigante B, Wolk A. The DASH diet is associated with a lower risk of heart failure: a cohort study. Eur J Prev Cardiol. 2022 May;29(7):1114–23. doi: 10.1093/eurjpc/zwac003. [DOI] [PubMed] [Google Scholar]
- 23.Asghari G, Rezazadeh A, Hosseini-Esfahani F, Mehrabi Y, Mirmiran P, Azizi F. Reliability, comparative validity and stability of dietary patterns derived from an FFQ in the Tehran Lipid and Glucose Study. Br J Nutr. 2012 Sep;108(6):1109–17. doi: 10.1017/S0007114511006313. [DOI] [PubMed] [Google Scholar]
- 24.Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB. Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med. 2008 Apr;168(7):713–20. doi: 10.1001/archinte.168.7.713. [DOI] [PubMed] [Google Scholar]
- 25.National Center for Health Statistics (NCHS) National Health and Nutrition Examination Survey. Available from: https://www.cdc.gov/nchs/nhanes/index.htm.
- 26.Aadahl M, Jørgensen T. Validation of a new self-report instrument for measuring physical activity. Med Sci Sports Exerc. 2003 Jul;35(7):1196–202. doi: 10.1249/01.MSS.0000074446.02192.14. [DOI] [PubMed] [Google Scholar]
- 27.Al Zenki S, Al Omirah H, Al Hooti S, Al Hamad N, Jackson RT, Rao A, et al. High prevalence of metabolic syndrome among Kuwaiti adults--a wake-up call for public health intervention. Int J Environ Res Public Health. 2012 May;9(5):1984–96. doi: 10.3390/ijerph9051984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mahdavi A, Mohammadi H, Foshati S, Shokri Mashhadi N, Clark CCT, Moafi A, et al. Effects of the dietary approach to stop hypertension (DASH) diet on blood pressure, blood glucose, and lipid profile in adolescents with hemophilia: A randomized clinical trial. Food Sci Nutr. 2021;9(1):145–153. doi: 10.1002/fsn3.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Campbell AP. DASH Eating Plan: An Eating Pattern for Diabetes Management. Diabetes Spectr. 2017 May;30(2):76–81. doi: 10.2337/ds16-0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Levitan EB, Wolk A, Mittleman MA. Consistency with the DASH diet and incidence of heart failure. Arch Intern Med. 2009 May;169(9):851–7. doi: 10.1001/archinternmed.2009.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ibsen DB, Levitan EB, Åkesson A, Gigante B, Wolk A. The DASH diet is associated with a lower risk of heart failure: a cohort study. Eur J Prev Cardiol. 2022 May;29(7):1114–23. doi: 10.1093/eurjpc/zwac003. [DOI] [PubMed] [Google Scholar]
- 32.Chiavaroli L, Viguiliouk E, Nishi SK, Blanco Mejia S, Rahelić D, Kahleová H, et al. DASH Dietary Pattern and Cardiometabolic Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses. Nutrients. 2019 Feb;11(2) doi: 10.3390/nu11020338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pirouzeh R, Heidarzadeh-Esfahani N, Morvaridzadeh M, Izadi A, Yosaee S, Potter E, et al. Effect of DASH diet on oxidative stress parameters: A systematic review and meta-analysis of randomized clinical trials. Diabetes Metab Syndr. 2020 Nov-Dec;14(6):2131–38. doi: 10.1016/j.dsx.2020.10.031. [DOI] [PubMed] [Google Scholar]
- 34.Tsutsui H, Tsuchihashi-Makaya M, Kinugawa S, Goto D. Characteristics and outcomes of patients with heart failure in general practices and hospitals. Circ J. 2007 Apr;71(4):449–54. doi: 10.1253/circj.71.449. [DOI] [PubMed] [Google Scholar]
- 35.Belch JJ, Bridges AB, Scott N, Chopra M. Oxygen free radicals and congestive heart failure. Br Heart J. 1991 May;65(5):245–8. doi: 10.1136/hrt.65.5.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pang Y, Huang M, Lu J, Peng Z, Tang M, Huang P, et al. Global trends in research on oxidative stress related to heart failure from 2012 to 2021: a bibliometric analysis and suggestion to researchers. Ann Transl Med. 2023 Jan;11(2):54 . doi: 10.21037/atm-22-6573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vanreusel I, Taeymans J, Van Craenenbroeck E, Segers VFM, Van Berendoncks A, Briedé JJ, et al. Elevated oxidative stress in patients with congenital heart disease and the effect of cyanosis: a meta-analysis. Free Radic Res. 2023 May-Jun;57(6-12):470–86. doi: 10.1080/10715762.2023.2284639. [DOI] [PubMed] [Google Scholar]
- 38.Farías JG, Molina VM, Carrasco RA, Zepeda AB, Figueroa E, Letelier P, et al. Antioxidant Therapeutic Strategies for Cardiovascular Conditions Associated with Oxidative Stress. Nutrients. 2017 Sep;9(9) doi: 10.3390/nu9090966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Landmesser U, Drexler H. The clinical significance of endothelial dysfunction. Curr Opin Cardiol. 2005 Nov;20(6):547–51. doi: 10.1097/01.hco.0000179821.11071.79. [DOI] [PubMed] [Google Scholar]
- 40.Adamy C, Mulder P, Khouzami L, Andrieu-abadie N, Defer N, Candiani G, et al. Neutral sphingomyelinase inhibition participates to the benefts of N-acetylcysteine treatment in post-myocardial infarction failing heart rats. Circ Res. 2014;115(5):475– 77. doi: 10.1016/j.yjmcc.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 41.Bourraindeloup M, Adamy C, Candiani G, Cailleret M, Bourin MC, Badoual T, et al. N-acetylcysteine treatment normalizes serum tumor necrosis factor-alpha level and hinders the progression of cardiac injury in hypertensive rats. Circulation. 2004 Oct;110(14):2003–9. doi: 10.1161/01.CIR.0000143630.14515.7C. [DOI] [PubMed] [Google Scholar]
- 42.Alpert MA, Lavie CJ, Agrawal H, Kumar A, Kumar SA. Cardiac effects of obesity: pathophysiologic, clinical, and prognostic consequences - a review. J Cardiopulm Rehabil Prev. 2016 Jan-Feb;36(1):1–11. doi: 10.1097/HCR.0000000000000147. [DOI] [PubMed] [Google Scholar]
- 43.Lopez-Jimenez F, Almahmeed W, Bays H, Cuevas A, Di Angelantonio E, le Roux CW, et al. Obesity and cardiovascular disease: mechanistic insights and management strategies A joint position paper by the World Heart Federation and World Obesity Federation. Eur J Prev Cardiol. 2022 Dec;29(17):2218–37. doi: 10.1093/eurjpc/zwac187. [DOI] [PubMed] [Google Scholar]
- 44.Jannasch F, Kröger J, Schulze MB. Dietary Patterns and Type 2 Diabetes: A Systematic Literature Review and Meta-Analysis of Prospective Studies. J Nutr. 2017 Jun;147(6):1174–82. doi: 10.3945/jn.116.242552. [DOI] [PubMed] [Google Scholar]