Abstract
Background
Radial artery cannulation can be challenging, particularly for inexperienced providers. This study aimed to compare the success rates of resident physicians performing radial artery cannulation with mild sedation and analgesia versus without.
Materials and methods
This study was a prospective, single-center, double-blind randomized controlled trial. Twelve anesthesiology residents performed radial artery insertions on 96 patients. The procedures were conducted with either mild sedation and analgesia (treatment group) or an equivalent volume of 0.9%Nacl (control group), in a random order. The primary outcome was the success rate of radial artery cannulation within 10 min for each group. Secondary outcomes included the first-attempt success rate, visual analogue scale (VAS) scores, and self-reported patient discomfort scores (0 corresponding to “no anxious”, 1 corresponding to “mildly anxious”, 2 corresponding to “moderately anxious” and 3 corresponding to “very anxious”).
Results
The success rate of radial artery cannulation within 10 min was 75.0% (36/48) in the treatment group and 54.2% (26/48) in the control group, respectively (difference 20.8%; P = 0.033, OR: 1.38, 95%CI: 1.02–1.88). The first-attempt success rate was 68.8% (33/48) in the treatment group, compared to 52.1% (25/48) in the control group (difference 16.7%; P = 0.095, OR: 1.32, 95%CI: 0.95–1.84). The VAS scores and self-reported patient discomfort scores were significantly lower in the treatment group than in the control group (2.0 [2.0, 2.0] vs. 3.0 [2.0, 4.0], P = 0.005; 1.0 [0.0, 2.0] vs. 2.0 [2.0, 2.0], P<0.001, respectively).
Conclusions
The success rate of radial artery cannulation within 10 min significantly increased for anesthesiology residents with the use of mild sedation and analgesia. Additionally, these medications resulted in a notable reduction in procedure-related pain and patient discomfort.
Trial registration
The study was registered at ClinicalTrials.gov (NCT05863455), with Qing-he Zhou as the principal investigator, on May 16, 2023.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-024-06568-8.
Keywords: Radial artery cannulation, Mild sedation and analgesia, Novice residents
Introduction
Arterial catheterization is crucial for continuous monitoring of arterial pressure and blood sampling during major surgeries [1, 2]. The radial artery is the preferred site due to its lower risk of complications compared to other access points [3].
Since many cannulations are carried out by non-experts, especially in training programs, radial artery cannulation is a key component of standardized training for residents [4]. However, radial artery catheterization is particularly challenging for novice operators, due to the small vessel diameter. It often leads to multiple attempts and complications such as hematoma, arterial occlusion, and prolonged procedures [5]. The increased pain from two punctures (one for the local anesthetic, one for arterial blood sampling) has been identified as a significant concern [6]. Many patients fear this procedure, as it is associated with significant pain and anxiety [7]. Repeated attempts not only heighten patient discomfort and the risk of complication [8, 9], but also undermine the operators’ confidence. Therefore, studies on educational strategies for essential clinical skills can provide valuable guidance for the standardized training of clinical postgraduates.
Studies have investigated the effects of mild sedatives and analgesics on the radial artery. Lower rates of radial artery spasm have been reported with the use of opioid analgesia combined with sedation during transradial percutaneous coronary intervention (PCI) procedures [10]. Sufentanil, a selective µ-receptor agonist, provides potent analgesia [11]. Midazolam binds to specific sites on the GABA receptor complex, exerting anti-anxiety effects at lower doses [12]. The combination of midazolam and fentanyl has a synergistic effect, reducing sympathetic nervous system excitation [13]. Both opioids [14, 15] and benzodiazepines [16] have shown concentration-dependent vasodilatory effects.
Although the incidence of spasm with this approach is remarkably low [10], the use of mild sedation and analgesia for radial artery cannulation by novice operators has not been thoroughly studied. Considering the small internal diameter of the radial artery and the inexperience of beginners, mild sedation and analgesia may improve the success rate of cannulation for novice operators. Therefore, this study aims to compare the effects of intravenous injection of sufentanil 0.1 µg/kg and midazolam 0.03 mg/kg (based on the reference [17] and preliminary experimental data) versus equivalent volume of 0.9%NaCl during radial artery cannulation for novice residents.
Methods
Aim
This study aimed to compare teaching without sedation and analgesia with teaching that incorporates mild sedation and analgesia, in order to determine which method is more effective in helping residents learn the radial artery puncture technique.
Study design and study population
This single-center, prospective, double-blind randomized study was conducted at the Affiliated Hospital of Jiaxing University. The study was approved by the ethics committee of the Affiliated Hospital of Jiaxing University, China, on April 26, 2023 (reference number 2023-KY-297) and was registered at ClinicalTrials.gov (NCT05863455), with Qing-he Zhou as the principal investigator, on May 16, 2023. Written informed consent was obtained from all patients. Participants were selected from those undergoing scheduled major surgeries requiring continuous arterial pressure monitoring. Patients over 20 years old, with a body mass index (BMI) of 18–28 kg/m2, and American Society of Anesthesiologists (ASA) grades I-III were included. All patients agreed to participate in this study and signed informed consent forms.
Exclusion criteria included a positive Allen’s test; infection at the puncture site; coagulation disorders; arterial diseases (such as Raynaud’s disease or thromboangiitis obliterans); use of vasoactive drugs within 30 min before measurement during the study; patients with arterial abnormalities and bends; hemorrhagic shock; arterial atherosclerosis; radial artery puncture within the past 30 days; chronic use of opioid or benzodiazepine drugs; and known allergies or adverse reactions to benzodiazepines or opioids.
Twelve resident physicians from the standardized residency training program (SRTP) at the Affiliated Hospital of Jiaxing University were eligible for the study. None had prior experience or training in radial artery puncture.
Randomization
Standardized training was provided to twelve resident physicians. Patients were assigned to either the treatment group (mild sedation and analgesia) or the control group (an equivalent volume of 0.9%NaCl) using a randomized block design. Assignments were placed in opaque envelopes, which were opened just before cannulation. To ensure balanced distribution among operators, each operator was randomly assigned procedures in blocks of four. Each block included two procedures with mild sedation and analgesia and two with 0.9%NaCl. Once an operator participated, they were required to complete two blocks (i.e., each operator performed the mild sedation and analgesia procedure four times and the 0.9%NaCl procedure four times).
Intervention
The theoretical instruction on radial artery puncture techniques covered the anatomical location, puncture preparation, procedure, and potential complications. Following this, each beginner performed 30 arterial catheterization procedures under the guidance of a supervising anesthesiologist.
Patients were instructed to fast for 8 h and avoid any preoperative medication before entering the operating room. Upon arrival, an intravenous line was established, and 8–10 mL/kg of lactated Ringer’s solution was administered. Oxygen was provided, and vital signs-including non-invasive blood pressure, respiratory rate, electrocardiography, heart rate, and SpO2-were monitored. The choice of wrist for the procedure was determined at the operator’s discretion or based on surgical indications. The patient was positioned supine with the operative upper limb abducted, palm facing upwards, and the wrist elevated by 3 cm. The transverse crease on the upper wrist, where the radial artery pulse was strongest, was marked, and the circumference of the wrist was measured by the operator.
After a negative result from the modified Allen’s test, the ultrasound probe (L4-12t; GE LOGIQ e; GE Medical Systems China Co., Ltd) was fitted with sterile disposable plastic caps. The probe was adjusted to obtain the highest quality ultrasound image, with the transducer depth set to 2.0 cm. An experienced anesthesiologist used ultrasound to locate the short axis of the radial artery and measure its diameter. The probe was then shifted to the long axis to evaluate the peak systolic velocity (PSV) of the radial artery using a longitudinal Doppler spectrum waveform. The Doppler sample gate was positioned in the center of the blood flow, avoiding the vessel wall, with some leeway for movement. The incident angle was adjusted and maintained at 50–60°. All values were measured three times, and the average was calculated.
In the treatment group, sufentanil (0.1 µg/kg) and midazolam (0.03 mg/kg) were administered slowly (over 2 min) via intravenous push at the start of the procedure. The control group received the equivalent volume of 0.9%NaCl. Three minutes after the intervention, ultrasound was used again at the same puncture site to measure the diameter and PSV. The average of three measurements was recorded. Afterwards, the anesthesiologist removed the marks that had been made previously.
The puncture site was sterilized with povidone-iodine solution, and local anesthesia was achieved through a subcutaneous injection of 0.5–1.5 mL of 2% lidocaine. A 22G BD puncture trocar was used, with the needle inserted at a 30° angle to the skin. Upon entering the radial artery, the angle was reduced to 15°, and the needle was advanced by 1–2 mm. The cannula was then inserted, secured, and connected to the arterial transducer. Attempts were recorded as the number of needle advancements requiring a new skin puncture or when the needle was completely withdrawn. Each new attempt used a fresh catheterization set, and no feedback was given by the supervising anesthesiologist (After each operator completed their respective blocks, the supervising anesthesiologist reviewed the footage and provided feedback on their performance).
Two researchers recorded all measurements, calculated the average, and documented the measurement times. A maximum of three cannulation attempts per radial site per resident was allowed. A successful puncture and catheterization was defined as puncturing the radial artery within 10 min, with visible blood return at the needle hub and successful placement of the catheter sheath (the arterial waveform was confirmed on the monitor). The failure rate was defined as the proportion of patients requiring more than three attempts or taking more than 10 min to achieve successful cannulation. Any failed cannulations were addressed by an expert anesthesiologist. The first successful puncture was defined as puncturing the radial artery on the first attempt, with visible blood return at the needle hub and successful placement of the sheath (the arterial waveform was confirmed on the monitor). The total time to cannulation was measured from the first skin puncture until a stable arterial waveform was achieved. If multiple attempts were made, the time for each puncture until catheter withdrawal or waveform stability was recorded and totaled.
Vasospasm was defined as a greater than 25% reduction in the radial artery diameter post-intubation [18, 19], in the absence of an intra-arterial hematoma. Hematoma was characterized as a visible by ultrasound or palpable swelling at the cannulation site. Adverse events were monitored for 24 h postoperatively, and the results were integrated into a continuously updated summary of complications for each group. A visual analogue scale (VAS) ranging from 0 to 10 was employed to assess pain intensity. The study also evaluated patient comfort levels by having patients grade their discomfort (0 corresponding to “no anxious”, 1 corresponding to “mildly anxious”, 2 corresponding to “moderately anxious” and 3 corresponding to “very anxious”).
Statistical methods
All analyses were performed according to intention-to-treat. The χ2 test was used to compare the treatment and control groups on categorical data. A two-sample independent t-test was used to compare the groups on continuous normally distributed data. When the Shapiro–Wilks test indicated non-normality, the Mann –Whiney U-test was used. Time to successful arterial cannulation was illustrated by the Kaplan–Meier curve and compared using the log-rank test. A P value of 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 19.0 (SPSS Inc., Chicago, Illinois, USA).
Sample size
On the basis of the results in previous study conducted at the Affiliated Hospital of Jiaxing University, we estimated that a clinically significant improvement in success rate within 10 min would be 88% in the treatment group (unpublished data, n = 20) by comparison with 61% in the control group (unpublished data, n = 20), in our sample of interest. A sample size of 47 patients per group would provide a power of 80% to compare these groups at a significance level of 0.05 with a two-sided χ2 test. Therefore, a total of 96 patients were planned for enrollment.
Results
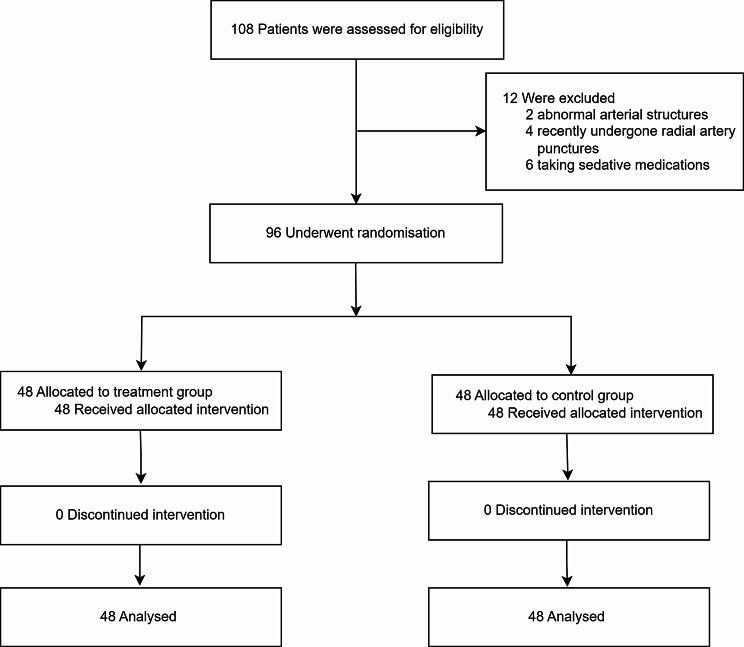
Between September 2024 and October 2024, a total of 108 patients were included in the study. Two patients were excluded due to abnormal arterial structures, four due to recent radial artery punctures, and six because they were taking sedative medications. The remaining 96 patients were randomized to the treatment group and control group in a 1:1 ratio (n = 48 each, Fig. 1). A total of 12 trainees performed the cannulations, with each trainee completing two procedures. Table 1 showed the characteristics of the patients in both groups. None of the patient characteristics were statistically different between the two groups.
Fig. 1.
Flow chart for the research
Table 1.
Population characteristics. Values are presented as mean (SD) and number of patients unless stated otherwise
| Demographic data | Treatment Group (n = 48) | Control Group (n = 48) | P values |
|---|---|---|---|
| Age (yrs) | 64.2 ± 10.1 | 62.9 ± 7.95 | 0.698 |
| Female sex, n (%) | 21 (43.8%) | 25 (52.1%) | 0.414 |
| BMI (kg/m2) | 22.5 ± 2.82 | 22.7 ± 2.83 | 0.803 |
| ASA physical status, n (%) | |||
| II | 38 (79.2%) | 40 (83.3%) | |
| III | 10 (20.8%) | 8 (16.7%) | |
| Wrist circumference (cm) | 15.8 ± 0.95 | 15.2 ± 1.23 | 0.364 |
| Diabetes, n (%) | 7 (14.6%) | 6 (12.5%) | 0.765 |
| Hypertension, n (%) | 24 (50.0%) | 31 (64.6%) | 0.149 |
| Smoking, n (%) | 7 (14.6%) | 11 (22.9%) | 0.296 |
| Dyslipidemia, n (%) | 2 (4.2%) | 1 (2.1%) | 0.557 |
Note Data are presented as the mean ± SD, or number of patients (%). P values as a result of t-test or χ2 test
Abbreviations: BMI, body mass index; ASA, American Society of Anesthesiologists
The results were presented in Table 2. The overall success rate within 10 min was higher in the treatment group compared with the control group [36/48 (75.0%) vs. 26/48 (54.2%), P = 0.033, OR: 1.38, 95%CI: 1.02–1.88]. However, the first-attempt success rate was not significantly greater in the treatment group than in the control group [33/48 (68.8%) vs. 25/48(52.1%), P = 0.095, OR: 1.32, 95%CI: 0.95–1.84]. Cumulative success rates within 10 min for both groups are illustrated by the Kaplan–Meier curve (Fig. 2). Significant differences were observed between the treatment group and the control group in the change from baseline for both diameter (0.26 cm [0.18, 0.60] vs. 0.01 cm [0.00, 0.05], P<0.001) and PSV (6.85 cm/s [0.00, 11.6] vs. 0.00 cm/s [-0.40, 1.01], P = 0.008). The visual analogue scale (VAS) scores and self-reported patient discomfort scores were significantly lower in the treatment group than in the control group (2.0 [2.0, 2.0] vs. 3.0 [2.0, 4.0], P = 0.005; 1.0 [0.0, 2.0] vs. 2.0 [2.0, 2.0], P<0.001, respectively) (Table 2).
Table 2.
Univariate results of radial arterial cannulation
| Parameter | Treatment Group (n = 48) | Control Group (n = 48) | P values |
|---|---|---|---|
| First-attempt success (%) | 33 (68.8%) | 25 (52.1%) | 0.095 |
| Success within 10 min (%) | 36 (75.0%) | 26 (54.2%) | 0.033 |
| Number of attempts | |||
| 1 | 33 (68.8%) | 25 (52.1%) | |
| 2 | 11 (22.9%) | 8 (16.7%) | |
| 3 | 4 (8.3%) | 15 (31.3%) | |
| Adverse events | |||
| Spasm | 7 (14.6%) | 16 (33.3%) | 0.031 |
| Hematoma | 10 (20.8%) | 8 (16.7%) | 0.601 |
| Radial artery size | |||
| Differential diameter (cm) | 0.26 (0.18, 0.60) | 0.01 (0.00, 0.05) | <0.001 |
| Differential PSV (cm/s) | 6.85 (0.00, 11.60) | 0.00 (-0.40, 1.01) | 0.008 |
| Patient discomfort scores | 1.0 (0.0, 2.0) | 2.0 (2.0, 2.0) | <0.001 |
| VAS scores | 2.0 (2.0, 2.0) | 3.0 (2.0, 4.0) | 0.005 |
Note Data are presented as the median (interquartile range), or number of patients (%). P values as a result of U Mann-Whitney test or χ2 test
Abbreviation: PSV, peak systolic velocity; VAS, visual analogue scale
Fig. 2.
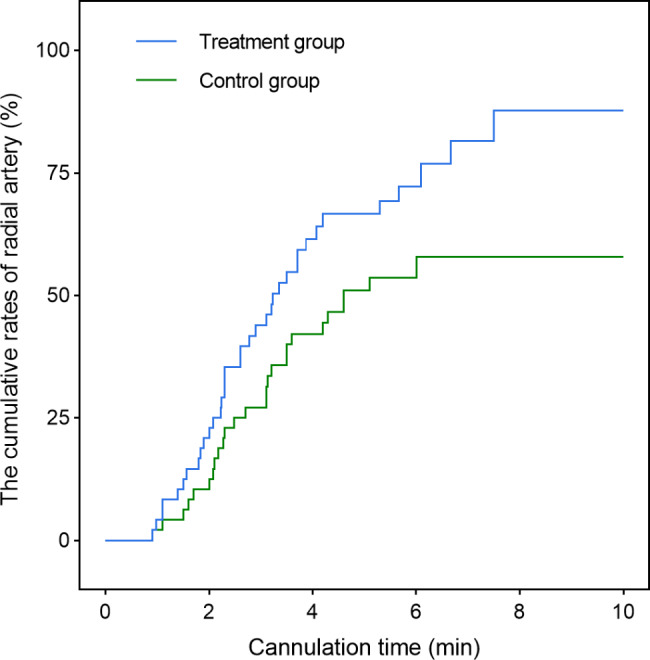
Cumulative successful cannulation within 10 min. Log-rank test P-value = 0.026. At the end of 10 min, radial arterial cannulation was completed in 75% of the treatment group and 54% of the control group
The incidence of hematoma did not differ significantly between the treatment and control groups, as shown in Table 2: 10/48 (20.8%) vs. 8/48 (16.7%); P = 0.601; OR: 1.25; 95%CI: 0.54–2.89. However, the incidence of spasm was lower in the treatment group compared to the control group: 7/48 (14.6%) vs. 16/48 (33.3%); P = 0.031; OR: 0.44; 95%CI: 0.20–0.97. Both hematoma and spasm showed spontaneous resolution postoperative. No other adverse events were observed within 24 h postoperatively.
Discussions
The current randomized study compared the success rates of radial arterial catheterization under mild sedation and analgesia versus non-sedation and analgesia in beginners. This approach, performed by trainee anesthesiologists, was completed in a shorter time with a higher success rate within 10 min, and a lower rate of procedure-related pain and patient discomfort. Our findings demonstrated that mild sedation and analgesia is a safe and effective technique for radial arterial catheterization, especially when performed by trainees.
The incidence of vasospasm or hematoma is critical to the success rate of peripheral artery cannulation, as these complications can decrease the internal diameter of the artery. Our study found that administering intravenous sufentanil and midazolam prior to cannulation increased both the internal diameter and cross-sectional area of the radial artery, likely contributing to a higher overall success rate. The radial artery, primarily influenced by α1-adrenoceptors, is particularly susceptible to vasospasm during cannulation attempts [20]. Temporary vasospasm can occur in up to 57% of cases immediately after radial arterial cannulation [21], while sustained vasospasm affects 4–20% of patients during transradial cardiac catheterization in adults [22]. This vasospasm complicates both the cannulation process and the advancement of the catheter into the artery [23], ultimately reducing the success rate of radial artery cannulation [22]. Additionally, the control group exhibited a higher risk of delayed vasospasm, as the smaller diameter of the radial artery makes it more vulnerable to endothelial damage during the procedure. In the treatment group, vasospasm was observed in seven patients. The relatively larger internal diameter resulting from mild sedation and analgesia administration may have contributed to an increased success rate on the next attempt and reduced catheter malfunction.
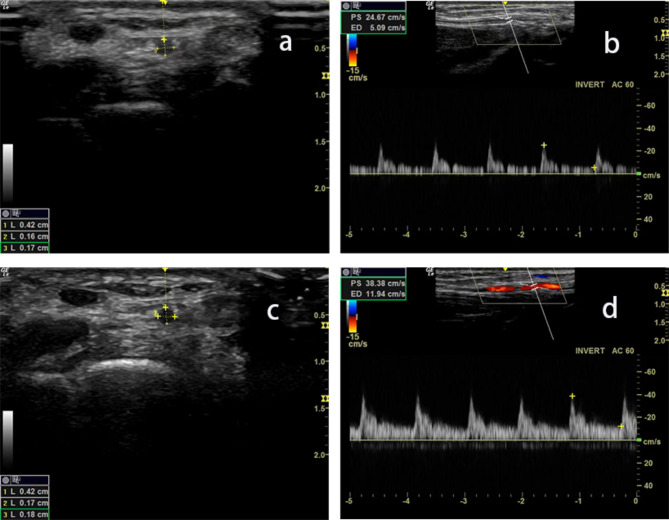
We utilized ultrasound to monitor changes in the radial artery before and after medication administration. Our findings revealed that following medication, the diameter of the radial artery slightly increased, accompanied by an elevation in blood flow velocity (Fig. 3). This effect might be attributed to mild sedation and analgesia inducing vasodilation [14–16], which reduced vascular resistance and enhances blood flow. When the needle punctured the vessel wall, blood flowed out rapidly. Therefore, using sedation and analgesics to increase the success rate of radial artery cannulation among beginners appeared to be a plausible hypothesis.
Fig. 3.
Ultrasound images of the radial artery in the mild sedation and analgesia group. (a) Diameter of radial artery before intravenous injection (b) Blood flow velocity before intravenous injection (c) Diameter of radial artery after intravenous injection (d) Blood flow velocity after intravenous injection
There was no significant difference in the success rate of the first catheterization between the two groups. Novice residents have lower puncture skills and weaker perception of pulse strength compared to experienced operators. Even with mild sedation and analgesia, the success rate for first-time radial artery cannulation is not significantly affected. Moreover, the use of mild sedation and analgesics not only reduced the occurrence of vascular spasms [10], but also enhanced the overall patient experience, thereby increasing the confidence of the operators [6]. In our study, since arterial cannulation was performed on awake patients with normal mean arterial pressures, the ability to identify the artery by palpation did not hinder successful cannulation.
In the current study, the administration of sufentanil at 0.1 µg/kg and midazolam at 0.03 mg/kg significantly increased the success rate of radial artery cannulation. Russell et al. previously identified that difficulties with percutaneous insertion at the radial artery site were associated with higher complication rates [24]. In our study, no clinically significant complications related to arterial line insertion were detected. It is important to note that we limited each radial artery cannulation attempt to a maximum of three and set a time limit of under 10 min for resident physicians to minimize the risk of complications.
The study demonstrated that the integration of mild sedation and analgesia in patients undergoing minimally invasive procedures resulted in favorable outcomes. Notably, prioritizing mild sedation and analgesia before procedures conducted by novices significantly enhanced the success rate and further facilitated the advancement of standardized residency training programs (SRTP).
Our study must be interpreted within the context of its limitations. We evaluated only anesthesia trainees, and different outcomes may be observed with more experienced anesthesiologists. Due to the limited sample size of operators, the overall learning curve and retention of procedural skills by residents post-surgery were not evaluated. Additionally, the relatively small sample size may limit the generalizability of our results, and the exclusion criteria (such as arterial abnormalities and use of vasoactive drugs) restrict the applicability of the findings to real-world clinical situations. Larger studies in the future are needed to confirm or challenge the advantages of mild sedation combined with analgesia methods. Moreover, it should be noted that the arterial cannulation size used in this study was a 22G catheter, and the impact of using a 20G catheter may result in different outcomes. Nonetheless, our results strongly support the superiority of mild sedation and analgesia, even among resident physicians with limited prior experience.
In conclusion, our results indicated that inexperienced operators could improve their success rates in radial artery catheterization by administering mild sedation and analgesia. This approach also reduced procedure-related pain and discomfort for patients.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors wish to acknowledge the support and contributions of their patient and students in conducting this study.
Abbreviations
- PCI
Percutaneous coronary intervention
- BMI
Body mass index
- ASA
American Society of Anesthesiologists
- SRTP
Standardized residency training programs
- PSV
Peak systolic velocity
- VAS,
Visual analogue scale
Author contributions
Y.X.: carried out the studies, participated in collecting data, and drafted the manuscript. Z.L.: participated in skills teaching and student management. Q.Z.: participated in the design of the study, read and approved all stages of the manuscript. All authors read and approved the final manuscript.
Funding
The study was provided by the Key Discipline Established with Zhejiang Provincial Traditional Chinese Medical Innovation Team (No. 2022-19), Zhejiang Provincial Key Clinical Specialty-Anesthesiology (2023-ZJZK-001) and Jiaxing Key Discipline of Medicine Anesthesiology (2023-ZC-001).
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author.
Declarations
Ethics approval and consent to participate
Ethical approval for this study was granted by the ethics committee of the Affiliated Hospital of Jiaxing University, China, on April 26, 2023 (reference number 2023-KY-297). The study was registered at ClinicalTrials.gov (NCT05863455), with Qing-he Zhou as the principal investigator, on May 16, 2023. All participants were provided with information on the study gave consent. The research protocol complied with the Consolidated Standards of Reporting Trials (CONSORT) statement and the Helsinki Declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kim SY, Lee JS, Kim WO, Sun JM, Kwon MK, Kil HK. Evaluation of radial and ulnar blood flow after radial artery cannulation with 20- and 22-gauge cannulae using duplex doppler ultrasound. Anaesthesia. 2012;67(10):1138–45. [DOI] [PubMed] [Google Scholar]
- 2.Rüsch D, Koch T, Seel F, Eberhart L. Vapocoolant Spray Versus Lidocaine Infiltration for Radial Artery Cannulation: a prospective, randomized, controlled clinical trial. J Cardiothorac Vasc Anesth. 2017;31(1):77–83. [DOI] [PubMed] [Google Scholar]
- 3.Bai B, Tian Y, Zhang Y, Yu C, Huang Y. Dynamic needle tip positioning versus the angle-distance technique for ultrasound-guided radial artery cannulation in adults: a randomized controlled trial. BMC Anesthesiol. 2020;20(1):231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Troianos CA, Hartman GS, Glas KE, et al. Special articles: guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular anesthesiologists. Anesth Analg. 2012;114(1):46–72. [DOI] [PubMed] [Google Scholar]
- 5.Brzezinski M, Luisetti T, London MJ. Radial artery cannulation: a comprehensive review of recent anatomic and physiologic investigations. Anesth Analg. 2009;109(6):1763–81. [DOI] [PubMed] [Google Scholar]
- 6.Wade RG, Crawfurd J, Wade D, Holland R. Radial artery blood gas sampling: a randomized controlled trial of lidocaine local anesthesia. J Evid Based Med. 2015;8(4):185–91. [DOI] [PubMed] [Google Scholar]
- 7.Giner J, Casan P, Belda J, González M, Miralda RM, Sanchis J. Pain during arterial puncture. Chest. 1996;110(6):1443–5. [DOI] [PubMed] [Google Scholar]
- 8.Kanei Y, Kwan T, Nakra NC, et al. Transradial cardiac catheterization: a review of access site complications. Catheter Cardiovasc Interv. 2011;78(6):840–6. [DOI] [PubMed] [Google Scholar]
- 9.Gu WJ, Wu XD, Wang F, Ma ZL, Gu XP. Ultrasound Guidance facilitates radial artery catheterization: a Meta-analysis with Trial Sequential Analysis of Randomized controlled trials. Chest. 2016;149(1):166–79. [DOI] [PubMed] [Google Scholar]
- 10.Deftereos S, Giannopoulos G, Raisakis K, et al. Moderate procedural sedation and opioid analgesia during transradial coronary interventions to prevent spasm: a prospective randomized study. JACC Cardiovasc Interv. 2013;6(3):267–73. [DOI] [PubMed] [Google Scholar]
- 11.Zhu H, Chen Y, Huang S, Sun X. Interaction of Analgesic effects of Dezocine and Sufentanil for Relief of Postoperative Pain: a pilot study. Drug Des Devel Ther. 2020;14:4717–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Manoj M, Satya Prakash MVS, Swaminathan S, Kamaladevi RK. Comparison of ease of administration of intranasal midazolam spray and oral midazolam syrup by parents as premedication to children undergoing elective surgery. J Anesth. 2017;31(3):351–7. [DOI] [PubMed] [Google Scholar]
- 13.Wang L, Wu Q, Wang M, et al. The safety and efficacy of alfentanil combined with midazolam in fiberoptic bronchoscopy sedation: a randomized, double-blind, controlled trial. Front Pharmacol. 2022;13:1036840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sahin AS, Duman A, Atalik EK, et al. The mechanisms of the direct vascular effects of fentanyl on isolated human saphenous veins in vitro. J Cardiothorac Vasc Anesth. 2005;19(2):197–200. [DOI] [PubMed] [Google Scholar]
- 15.Gursoy S, Bagcivan I, Yildirim MK, Berkan O, Kaya T. Vasorelaxant effect of opioid analgesics on the isolated human radial artery. Eur J Anaesthesiol. 2006;23(6):496–500. [DOI] [PubMed] [Google Scholar]
- 16.Colussi GL, Di Fabio A, Catena C, Chiuch A, Sechi LA. Involvement of endothelium-dependent and -independent mechanisms in midazolam-induced vasodilation. Hypertens Res. 2011;34(8):929–34. [DOI] [PubMed] [Google Scholar]
- 17.Yao Y, Su Z, Chen Y, et al. Safety and efficacy of sufentanil combined with midazolam in bronchoscopy under conscious sedation: retrospective study of 11,158 cases. J Thorac Dis. 2019;11(10):4127–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jang YE, Ji SH, Kim EH, et al. Subcutaneous nitroglycerin for radial arterial catheterization in Pediatric patients: a Randomized Controlled Trial. Anesthesiology. 2020;133(1):53–63. [DOI] [PubMed] [Google Scholar]
- 19.Men X, Wang Q, Hu WS, et al. Correction: median nerve block increases the success rate of radial artery cannulation in women with gestational hypertension undergoing cesarean section. BMC Anesthesiol. 2022;22(1):272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.He GW, Yang CQ. Characteristics of adrenoceptors in the human radial artery: clinical implications. J Thorac Cardiovasc Surg. 1998;115(5):1136–41. [DOI] [PubMed] [Google Scholar]
- 21.Kim JM, Arakawa K, Bliss J. Arterial cannulation: factors in the development of occlusion. Anesth Analg. 1975;54(6):836–41. [DOI] [PubMed] [Google Scholar]
- 22.Ho HH, Jafary FH, Ong PJ. Radial artery spasm during transradial cardiac catheterization and percutaneous coronary intervention: incidence, predisposing factors, prevention, and management. Cardiovasc Revasc Med. 2012;13(3):193–5. [DOI] [PubMed] [Google Scholar]
- 23.Cuper NJ, de Graaff JC, Hartman BJ, Verdaasdonk RM, Kalkman CJ. Difficult arterial cannulation in children: is a near-infrared vascular imaging system the answer? Br J Anaesth. 2012;109(3):420–6. [DOI] [PubMed] [Google Scholar]
- 24.Russell JA, Joel M, Hudson RJ, Mangano DT, Schlobohm RM. Prospective evaluation of radial and femoral artery catheterization sites in critically ill adults. Crit Care Med. 1983;11(12):936–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author.