Abstract
Purpose
We describe emergency medical services (EMS) protocols for pain management in the United States to elucidate systemic variability in protocols. We describe types of pain medications included in protocols, routes of administration, indications for use, standing orders for dosing, and use in pediatric patients.
Methods
We performed a review of all publicly accessible EMS protocols from the website http://www.emsprotocols.org, supplemented with internet searches. Data were abstracted into a data collection form from June 2021 to January 2022. We developed categories of responses to summarize the data, using frequencies and proportions to describe outcome measures.
Results
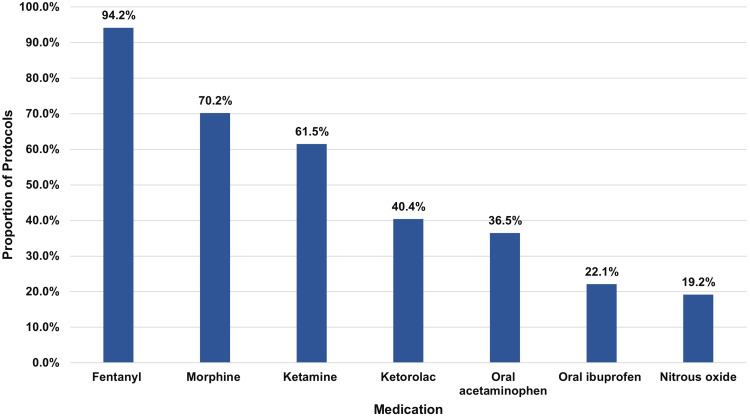
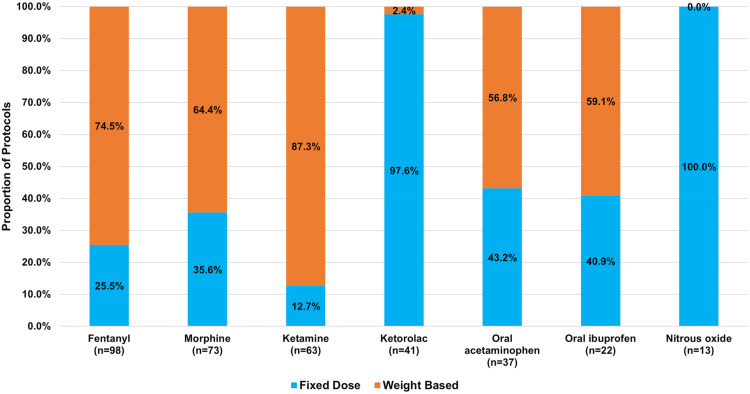
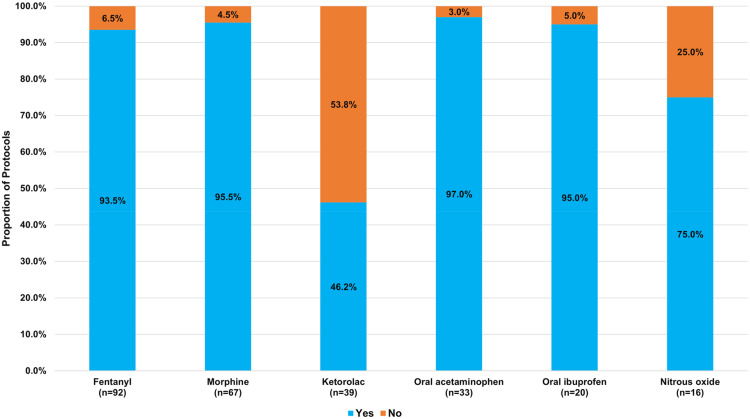
We reviewed 104 EMS protocols, spanning 43 states. The most common pain management medications include fentanyl (94.2%), morphine (70.2%), ketamine (61.5%), ketorolac (40.4%), oral acetaminophen (36.5%), oral ibuprofen (22.1%), and nitrous oxide (19.2%). The most common route of administration across all protocols and medications is intravenous. Severe pain, without a specified level, is the most common indication for fentanyl (65.3%), morphine (61.6%), ketorolac (50.0%), and nitrous oxide (40.0%). Musculoskeletal injuries and burns are the most common indications for morphine, 15.1% and 19.2% of protocols, respectively. The majority of protocols dictate the weight-based dosing of fentanyl (74.5%), morphine (64.4%), ketamine (87.3%), oral acetaminophen (56.8%), and oral ibuprofen (59.1%). However, 97.6% and 100.0% of protocols dictate a fixed dose of ketorolac and nitrous oxide, respectively. Fentanyl, morphine, oral acetaminophen, and oral ibuprofen can be administered to pediatric patients based on standing orders among >90.0% of protocols. However, only 46.2% and 75.0% of protocols allow the use of ketorolac and nitrous oxide in pediatric patients, respectively.
Conclusion
We found variability in EMS pain management protocols including the types of allowed medications, routes of administration, dosing, and indications for use. Further studies may assess whether standardized protocols across EMS systems could improve patient safety and quality of care.
Keywords: pain management, pediatrics, emergency medical services, protocols, variability
Introduction
Prehospital emergency medical services (EMS) play a critical role in the care of patients experiencing pain. EMS clinicians are often the first point of contact for patients in need of acute pain management. Clinical protocols for pain management help ensure the provision of consistent, high-quality, evidence-based care in the health care setting.1 However, the variability of these protocols across different EMS systems and regions can create challenges for both EMS clinicians and patients. In many industries, standardization of processes and protocols reduce errors.2 This is particularly important in EMS, where more than one-third of EMS clinicians work for more than one EMS agency,3 sometimes in different counties or even states. Lack of standardization in protocols may increase the risk of medication dosing errors,4,5 as EMS clinicians must remember which set of protocols to follow in high-stress situations.
Variability in EMS protocols for pain management can manifest in several ways, including the selection of medications,6 dosing regimens, routes of administration, indications for use, and the level of autonomy afforded to EMS clinicians for administration.7 Such inconsistencies in protocols may lead to differences in the pain relief provided to patients based on the EMS clinicians and their practice location. As a patient’s geographic location should not alter the care they receive, the current lack of consensus creates confusion and treatment discrepancies often experienced by patients and clinicians. An observational study conducted by Ferri et al revealed that nearly 80% of patients in the prehospital setting experiencing pain received no pharmacological pain management.8 Furthermore, in the small percentage of cases where pain medication was administered, established pain management algorithms were rarely followed.8 The study also noted variability in medication choice for severe pain, with fentanyl being the most frequently administered analgesic, followed by morphine, ketorolac, and acetaminophen.8
The objective of this study was to describe variability of prehospital EMS pain management protocols in terms of types of pain medications, routes of administration for each, indications for use, standing orders for dosing, and use in pediatric patients in the United States.
Methods
Study Design and Data Sources
We reviewed EMS protocols in the United States for pain management protocols. Drawing on methodology from prior literature,2,9,10 we accessed the website http://www.emsprotocols.org, which compiles EMS protocols from around the United States and Canada; however, we reviewed only protocols from the United States for this study. The website is public and periodically updated based on the public availability of protocols. The protocol review took place between June 2021 and January 2022. All protocols from the United States that were available on the website were reviewed. For protocols not available on the website, we attempted to obtain protocols via internet searches. The goal was to obtain and review at least one EMS protocol per state. We did not contact agencies directly to obtain protocols. Institutional Review Board approval was not required, as this study did not involve human subjects and all protocols were publicly available.
Data Collection and Analysis
The research team created a standardized electronic data collection form (Supplement 1) using the Research Electronic Capture (REDCap) platform,11 as there are no validated and/or published tools for reviewing prehospital pain management protocols. After reviewing the first five protocols, the data collection form was revised and finalized. After receiving initial training by the lead author (TL), the research team abstracted accessible EMS protocols. The research team consisted of EMS clinicians and/or medical school students; anyone with a concern about a particular protocol flagged the protocol. It was then reviewed by the entire team, including two physicians with dual board certification in emergency medicine and EMS (PB and JB).
The review of protocols focused on what medications are listed in pain management protocols, the dosing of these medications, the routes of administration, indications for use, and whether EMS clinicians may administer them based on standing orders or required direct medical oversight to administer these medications in both adult and pediatric patients. We created response categories to represent the data, due to the wide range of responses across various protocols. Descriptive statistics, including frequencies and proportions, are reported to summarize results.
Results
A total of 104 protocols were available, retrieved, and reviewed as part of this analysis (Table 1); 19 (18.3%) of protocols were from the state of California and 5 (4.8%) each were from Virginia, Oregon, Illinois, and Colorado. Overall, as shown in Figure 1, protocols allow the use of fentanyl (94.2%), morphine (70.2%), ketamine (61.5%), ketorolac (40.4%), oral acetaminophen (36.5%), oral ibuprofen (22.1%), and nitrous oxide (19.2%). Less commonly allowed medications for pain management included aspirin (4 protocols, 3.8%), midazolam (4 protocols, 3.8%), hydromorphone (2 protocols, 1.9%), and nalbuphine, meperidine, sufentanil, and lidocaine (one protocol each, 1.0%).
Table 1.
State/County/Region/Agency Protocols Included in Review (n = 104 Protocols/43 States)
| State | State/County/Region/Agency | n (%) |
|---|---|---|
| Alabama | Alabama Statewide | 1 (1.0%) |
| Alaska | Anchorage Fire Department; Fairbanks North Star Borough; Matanuska-Susitna Borough | 3 (2.9%) |
| Arizona | Central Arizona Regional; Southeast Arizona; Phoenix Fire Department | 3 (2.9%) |
| California | Alameda County; Coastal Valley EMS; Yolo County; Ventura County; Solano County; Sierra - Sacramento Valley; Santa Cruz; Santa Barbara; San Mateo County; San Luis Obispo; San Joaquin; San Francisco; San Benito; Sacramento; North Coast; Nor-Cal EMS; Napa County; Contra Costa County; Mountain Valley EMS | 19 (18.3%) |
| Colorado | Boulder County; Denver Metro; Mesa County; Thompson Valley EMS; Chaffee County | 5 (4.8%) |
| Connecticut | Connecticut Statewide; North Central Connecticut EMS Council | 2 (1.9%) |
| Delaware | Delaware Statewide | 1 (1.0%) |
| Florida | Delray Beach Fire Rescue; Franklin County EMS; Okaloosa County | 3 (2.9%) |
| Idaho | Treasure Valley EMS | 1 (1.0%) |
| Illinois | East Central Illinois EMS; Good Samaritan; Regional EMS; Illinois Region 6; Illinois Region 8; Illinois Region X | 5 (4.8%) |
| Indiana | IU Health LifeLine; Indianapolis Metro | 2 (1.9%) |
| Iowa | MercyOne Ambulance; Scott County; West Des Moines | 3 (2.9%) |
| Kansas | Douglas County EMS; Great Bend Fire/EMS | 2 (1.9%) |
| Kentucky | Kentucky Statewide | 1 (1.0%) |
| Maine | Maine Statewide | 1 (1.0%) |
| Maryland | Maryland Statewide | 1 (1.0%) |
| Massachusetts | Massachusetts Statewide | 1 (1.0%) |
| Minnesota | Hennepin County | 1 (1.0%) |
| Missouri | SSM EMS; Kansas City Missouri Fire Department; Cole County | 3 (2.9%) |
| Montana | Montana Statewide | 1 (1.0%) |
| Nebraska | Nebraska Model Statewide | 1 (1.0%) |
| Nevada | Clark County | 1 (1.0%) |
| New Hampshire | New Hampshire Statewide | 1 (1.0%) |
| New Jersey | New Jersey Statewide | 1 (1.0%) |
| New Mexico | New Mexico Statewide; Sandoval County | 2 (1.0%) |
| New York | New York City REMAC; New York Statewide; Suffolk County EMS System | 3 (2.9%) |
| North Carolina | Buncombe/Madison/Yancey EMS; North Carolina Statewide; Wake County; Orange County | 4 (3.9%) |
| North Dakota | North Dakota Ambulance Services | 1 (1.0%) |
| Ohio | Lucas County; Southwest Ohio; Summa Region 8 | 3 (2.9%) |
| Oklahoma | Oklahoma Statewide | 1 (1.0%) |
| Oregon | East Cascade EMS; Jackson County; Josephine County; Lane County; Multnomah County | 5 (4.8%) |
| Pennsylvania | Pennsylvania Statewide | 1 (1.0%) |
| Rhode Island | Rhode Island Statewide | 1 (1.0%) |
| South Carolina | South Carolina Statewide | 1 (1.0%) |
| South Dakota | Rapid City Fire Department | 1 (1.0%) |
| Texas | Austin-Travis County; BioTel; Houston Fire Department; Montgomery County Hospital District | 4 (3.9%) |
| Utah | Davis County | 1 (1.0%) |
| Vermont | Vermont Statewide | 1 (1.0%) |
| Virginia | Blue Ridge; Central Shenandoah EMS; Old Dominion EMSA; Peninsulas EMS; Prince William County | 5 (4.8%) |
| Washington | Chelan/Douglas County; Grays Harbor; San Juan County; Spokane County | 4 (3.9%) |
| Washington DC | District of Columbia | 1 (1.0%) |
| West Virginia | West Virginia Statewide | 1 (1.0%) |
| Wisconsin | Dane County | 1 (1.0%) |
Notes: Reproduced from Li T, Koloden D, Berkowitz J et al. Prehospital transport and termination of resuscitation of cardiac arrest patients: A review of prehospital care protocols in the United States. Resusc Plus. 2023;14:100397.10 Creative commons (https://creativecommons.org/licenses/by-nc-nd/4.0/).
Figure 1.
Medications Used for Pain Management (n = 104 protocols).
Allowable routes of administration based on standing orders vary by medication (Table 2). Across all protocols and medications, intravenous administration is the most common allowable route of administration. Among the 98 protocols allowing the use of fentanyl, all (100.0%) of them allow intravenous administration, 70.4% allow intramuscular, 76.5% intranasal, 70.4% intraosseous, and 1.0% nebulized. For the 73 protocols allowing the administration of morphine, 100.0%, 68.5%, 5.5%, and 67.1% allow intravenous, intramuscular, intranasal, and intraosseous administration, respectively. No protocols allow the nebulization of morphine. For ketamine, 92.2%, 57.8%, 34.4%, and 56.3% of protocols allow intravenous, intramuscular, intranasal, and intraosseous administration, respectively. Nebulization of ketamine was not allowed by any protocol. Lastly, among the 42 protocols allowing the use of ketorolac, intravenous, intramuscular, intranasal, and intraosseous administration was allowed by 92.9%, 83.3%, 7.1%, and 28.6% of protocols. Nebulization of ketorolac was not allowed by any of the 42 protocols.
Table 2.
Routes of Administration Based on Standing Orders (n = 104 Protocols)
| Intravenous | Intramuscular | Intranasal | Intraosseous | Nebulization | |
|---|---|---|---|---|---|
| Fentanyl (n = 98) | |||||
| Yes, n (%) | 98 (100.0%) | 69 (70.4%) | 75 (76.5%) | 69 (70.4%) | 1 (1.0%) |
| No, n (%) | 0 (0.0%) | 29 (29.6%) | 23 (23.5%) | 29 (29.6%) | 97 (99.0%) |
| Morphine (n = 73) | |||||
| Yes, n (%) | 73 (100.0%) | 50 (68.5%) | 4 (5.5%) | 49 (67.1%) | 0 (0.0%) |
| No, n (%) | 0 (0.0%) | 23 (31.5%) | 69 (94.5%) | 24 (32.9%) | 73 (100.0%) |
| Ketamine (n = 64) | |||||
| Yes, n (%) | 59 (92.2%) | 37 (57.8%) | 22 (34.4%) | 36 (56.3%) | 0 (0.0%) |
| No, n (%) | 5 (7.8%) | 27 (42.2%) | 42 (65.6%) | 28 (43.8%) | 64 (100.0%) |
| Ketorolac (n = 42) | |||||
| Yes, n (%) | 39 (92.9%) | 35 (83.3%) | 3 (7.1%) | 12 (28.6%) | 0 (0.0%) |
| No, n (%) | 3 (7.1%) | 7 (16.7%) | 39 (92.9%) | 30 (71.4%) | 42 (100.0%) |
Table 3 displays the indications for use of the various pain management medications based on standing orders. Severe pain, without a specified pain level, is the most common indication for fentanyl (65.3%), morphine (61.6%), ketorolac (50.0%), and nitrous oxide (40.0%). The most common indication for oral acetaminophen (47.4%) and oral ibuprofen (47.8%) is a specific pain level. Musculoskeletal injuries and burns are the most common indications for morphine, 15.1% and 19.2% of protocols, respectively.
Table 3.
Indications for Use Based on Standing Orders (n = 104 Protocols)
| Musculoskeletal Injuries | Burns | Specific Pain Level | Severe Pain, Not Otherwise Defined | Other Indications | Not Specified | |
|---|---|---|---|---|---|---|
| Fentanyl (n = 98) | ||||||
| Yes, n (%) | 9 (9.2%) | 12 (12.2%) | 29 (29.6%) | 64 (65.3%) | 28 (28.6%) | 4 (4.1%) |
| No, n (%) | 89 (90.8%) | 86 (87.8%) | 69 (70.4%) | 34 (34.7%) | 70 (71.4%) | 94 (95.9%) |
| Morphine (n = 73) | ||||||
| Yes, n (%) | 11 (15.1%) | 14 (19.2%) | 19 (26.0%) | 45 (61.6%) | 35 (48.0%) | 2 (2.7%) |
| No, n (%) | 62 (84.9%) | 59 (80.8%) | 54 (74.0%) | 28 (38.4%) | 38 (52.1%) | 71 (97.3%) |
| Ketamine (n = 64) | ||||||
| Yes, n (%) | 4 (6.3%) | 4 (6.3%) | 14 (21.9%) | 39 (60.9%) | 40 (62.5%) | 0 (0.0%) |
| No, n (%) | 60 (93.8%) | 60 (93.8) | 50 (78.1%) | 25 (39.1%) | 24 (37.5%) | 64 (100.0%) |
| Ketorolac (n = 42) | ||||||
| Yes, n (%) | 3 (7.1%) | 0 (0.0%) | 17 (40.5%) | 21 (50.0%) | 5 (11.9%) | 1 (2.4%) |
| No, n (%) | 39 (92.9%) | 42 (100.0%) | 25 (59.5%) | 21 (50.0%) | 37 (88.1%) | 41 (97.6%) |
| Oral acetaminophen (n = 38) | ||||||
| Yes, n (%) | 2 (5.3%) | 0 (0.0%) | 18 (47.4%) | 11 (29.0%) | 10 (26.3%) | 1 (2.6%) |
| No, n (%) | 36 (94.7%) | 38 (100.0%) | 20 (52.6%) | 27 (71.1%) | (73.7%) | 37 (97.4%) |
| Oral ibuprofen (n = 23) | ||||||
| Yes, n (%) | 1 (4.4%) | 0 (0.0%) | 11 (47.8%) | 7 (30.4%) | 6 (26.1%) | 1 (4.4%) |
| No, n (%) | 22 (95.7%) | 23 (100.0%) | 12 (52.2%) | 16 (69.6%) | 17 (73.9%) | 22 (95.7%) |
| Nitrous oxide (n = 20) | ||||||
| Yes, n (%) | 3 (15.0%) | 3 (15.0%) | 5 (25.0%) | 8 (40.0%) | 5 (25.0%) | 0 (0.0%) |
| No, n (%) | 17 (85.0%) | 17 (85.0%) | 15 (75.0%) | 12 (60.0%) | 15 (75.0%) | 20 (100.0%) |
Notes: Row percentages may sum to >100% due to medications having more than one indication.
Figure 2 shows each medication and whether they are administered at a fixed dose or whether the dosing is based on the patient’s weight, per standing orders. Most protocols dictate the weight-based dosing of fentanyl (74.5%), morphine (64.4%), ketamine (87.3%), oral acetaminophen (56.8%), and oral ibuprofen (59.1%). However, 97.6% and 100.0% of protocols dictate a fixed dose of ketorolac and nitrous oxide, respectively.
Figure 2.
Fixed Dose vs Weight-Based Dosing based on Standing Orders (n = 104 protocols).
As show in Figure 3, fentanyl, morphine, oral acetaminophen, and oral ibuprofen can be administered to pediatric patients based on standing orders among >90.0% of protocols. However, only 46.2% of protocols allow the use of ketorolac and 75.0% of protocols allow the use of nitrous oxide in pediatric patients.
Figure 3.
Used in Pediatric Patients based on Standing Orders (n = 104 protocols).
Discussion
The variability of clinical protocols, including prehospital EMS pain management protocols, is a substantial issue that may impact patient care and safety. Appropriate pain management has been shown to improve patient satisfaction and reduce morbidity and mortality.12–14 While standardization of clinical protocols remains an understudied area generally, there is even less published work about the standardization of EMS protocols. This descriptive analysis serves as a starting point to fuel further study on pain management protocols in the prehospital setting.
The results of our structured review indicate that EMS pain management protocols vary substantially across different systems, regions, and states. This is particularly concerning in the prehospital setting, where time is often of the essence and EMS clinicians do not have access to the same level of diagnostic and treatment resources as personnel in the hospital setting. Further, EMS clinicians often cannot access comprehensive patient information and medical history. In these situations, it is especially important that clinicians have access to clear, safe, evidence-based guidelines that can help them provide optimal care for patients experiencing pain and make informed decisions about the best course of action for their patients.
Many EMS protocols are based on guidelines from professional organizations, such as the National Association of EMS Physicians (NAEMSP) or the American College of Surgeons (ACS). There have been initiatives to develop evidence-based guidelines for the administration of analgesics in the prehospital setting;15,16 however, we find that there is no one guideline followed consistently in regional protocols, leading to variability in the medications and dosages used for pain management across regions and EMS agencies. This creates substantial inconsistencies in the type of pain management a patient would receive based on the EMS system they find themselves in geographically. Whether and how this variability impacts outcomes requires further study.
There are several factors that can contribute to variability in clinical protocols. These include a lack of standardization in guidelines and recommendations, conflicting evidence on the most effective interventions, local traditions and practices, and individual personnel preference. The availability of resources and infrastructure, as well as regulatory and legal considerations, can also influence the adoption and implementation of pain management protocols. Medication shortages may lead some agencies to have multiple medication options. Lastly, cost of medications may also be a factor, as some agencies may not stock certain medications due to high costs and needed storage conditions.
Future studies may examine the association between EMS pain management protocols and population density, rurality, and distance to hospitals. In areas where transport time may be extended due to the location of hospitals, longer-acting pain medications may be included in the formulary. More research is needed to better understand the consequences of protocol variability, and to identify effective strategies for reducing it. This could include studies that explore the factors that influence the adoption and implementation of clinical protocols, as well as those that assess the impact of regional standardization initiatives on patient outcomes. Additionally, research is needed to understand the role of EMS clinicians in driving protocol variability and to identify ways to promote adherence to evidence-based practices from all stakeholders. Further research will shed light on the degree of protocol flexibility or standardization that best serves patients. Lastly, future research may describe EMS protocols in other countries to provide a more comprehensive review of protocols for prehospital pain management.
Limitations
There are several limitations of this study to acknowledge. First, we only reviewed a convenience sample of EMS protocols that were publicly accessible on the internet. Protocols from seven states were unable to be publicly obtained. However, we attempted to review at least one protocol from each state, and we were able to cover 43 states. Nevertheless, our conclusions should not be substantially different if we were able to obtain EMS protocols from the remaining seven states; they would only add to the variability we found. Second, our study sample included 19 protocols from the state of California, which is 18.3% of the study sample and thus, our results may be skewed due to overrepresentation of protocols from California. However, this speaks to the variability of EMS protocols, where every county has their own protocol in some states, but in other states, all counties follow a statewide protocol. Further, we were not interested in which states did what; we were interested in the variation in protocols itself. Lastly, our study was descriptive in nature, and we sought to describe variability in protocols. We did not examine the effect of protocol variability on patient outcomes and safety.
Conclusion
In this review of EMS protocols from 43 states, we found substantial variability in the types of medications included in the pain management formulary, as well as the routes of administration, indications for use, weight-based vs fixed dosing, and use in pediatric patients. Further research is needed to identify the most effective protocols for managing pain in the prehospital setting, and to understand the factors that contribute to variability in practice. In the meantime, it is important for health care systems to review and update their protocols regularly to ensure that they are in line with current best practices and guidelines.
Acknowledgments
The authors would like to thank Tara Mendola, PhD for her editorial contributions to this manuscript.
Funding Statement
There is no funding to report.
Disclosure
The authors report there are no competing interests to declare.
References
- 1.Gordon DB, Dahl JL, Miaskowski C, et al. American pain society recommendations for improving the quality of acute and cancer pain management: American pain society quality of care task force. Arch Intern Med. 2005;165(14):1574–1580. doi: 10.1001/archinte.165.14.1574 [DOI] [PubMed] [Google Scholar]
- 2.Rostykus P, Kennel J, Adair K, et al. Variability in the treatment of prehospital hypoglycemia: a structured review of EMS protocols in the United States. Prehosp Emerg Care. 2016;20(4):524–530. doi: 10.3109/10903127.2015.1128031 [DOI] [PubMed] [Google Scholar]
- 3.Rivard MK, Cash RE, Chrzan K, Panchal AR. The impact of working overtime or multiple jobs in emergency medical services. Prehosp Emerg Care. 2020;24(5):657–664. doi: 10.1080/10903127.2019.1695301 [DOI] [PubMed] [Google Scholar]
- 4.Bates DW, Vanderveen T, Seger D, Yamaga C, Rothschild J. Variability in intravenous medication practices: implications for medication safety. Jt Comm J Qual Patient Saf. 2005;31(4):203–210. doi: 10.1016/s1553-7250(05)31026-9 [DOI] [PubMed] [Google Scholar]
- 5.Glanz JM, Binswanger IA, Shetterly SM, Narwaney KJ, Xu S. Association between opioid dose variability and opioid overdose among adults prescribed long-term opioid therapy. JAMA Network Open. 2019;2(4):e192613–e192613. doi: 10.1001/jamanetworkopen.2019.2613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Borland ML, Jacobs I, Rogers IR. Options in prehospital analgesia. Emerg Med. 2002;14(1):77–84. doi: 10.1046/j.1442-2026.2002.00288.x [DOI] [PubMed] [Google Scholar]
- 7.Samuel N, Steiner IP, Shavit I. Prehospital pain management of injured children: a systematic review of current evidence. Am J Emerg Med. 2015;33(3):451–454. doi: 10.1016/j.ajem.2014.12.012 [DOI] [PubMed] [Google Scholar]
- 8.Ferri P, Gambaretto C, Alberti S, et al. Pain management in a prehospital emergency setting: a retrospective observational study. J Pain Res. 2022;15:3433–3445. doi: 10.2147/JPR.S376586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Namboodri BL, Rosen T, Dayaa JA, et al. Elder abuse identification in the prehospital setting: an examination of state emergency medical services protocols. J Am Geriatr Soc. 2018;66(5):962–968. doi: 10.1111/jgs.15329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li T, Koloden D, Berkowitz J, et al. Prehospital transport and termination of resuscitation of cardiac arrest patients: a review of prehospital care protocols in the United States. Resusc Plus. 2023;14:100397. doi: 10.1016/j.resplu.2023.100397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sinatra R. Causes and consequences of inadequate management of acute pain. Pain Med. 2010;11(12):1859–1871. doi: 10.1111/j.1526-4637.2010.00983.x [DOI] [PubMed] [Google Scholar]
- 13.Häusler G, van der Vet PCR, Beeres FJP, Kaufman T, Kusen JQ, Poblete B. The impact of loco-regional anaesthesia on postoperative opioid use in elderly Hip fracture patients: an observational study. Eur J Trauma Emerg Surg. 2022;48(4):2943–2952. doi: 10.1007/s00068-021-01674-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson Q, Borsheski RR, Reeves-Viets JL. Pain management mini-series. Part I. A review of management of acute pain. Mo Med. 2013;110(1):74–79. [PMC free article] [PubMed] [Google Scholar]
- 15.Lindbeck G, Shah MI, Braithwaite S, et al. Evidence-based guidelines for prehospital pain management: recommendations. Prehosp Emerg Care. 2023;27(2):144–153. doi: 10.1080/10903127.2021.2018073 [DOI] [PubMed] [Google Scholar]
- 16.Yousefifard M, Askarian-Amiri S, Madani Neishaboori A, Sadeghi M, Saberian P, Baratloo A. Pre-hospital pain management; a systematic review of proposed guidelines. Arch Acad Emerg Med. 2019;7(1):e55. [PMC free article] [PubMed] [Google Scholar]