For the last 15 years, Canadians have faced uncertainty regarding the availability of public funds to provide universal, high-quality health care. In this paper, we point out the essential stability of Canada's health care spending during the last decade and the need for resources to ensure that an aging population will have access to the increasing range of beneficial health technologies and services it legitimately expects. We lay out principles and options for structural changes necessary to ensure the stability of public health care funding.
The media and governments often present health care costs as rapidly escalating. Expressing expenditures in absolute numbers of dollars ignores both inflation and changes in the size of the population. Per capita spending ignores the aging of the population and economic growth. Expressing expenditures in terms of the gross domestic product (GDP) captures the relation between health spending and societal resources.
In 1992, Canada's total spending on health care as a percentage of its economy reached 10% of the GDP.1 Of these expenditures, 74%, or 7.3% of GDP, represented government expenditures.2,3 Responding to concerns about deficits, both federal and provincial governments reined in health spending. Consequently, per capita spending on health care fell between 1992 and 1996,1,2 and did not return to its 1992 level until 1999. Given the economic growth over this period, Canada now spends only 9.4% of its GDP on health care, substantially less than in 1992 (Fig. 1).
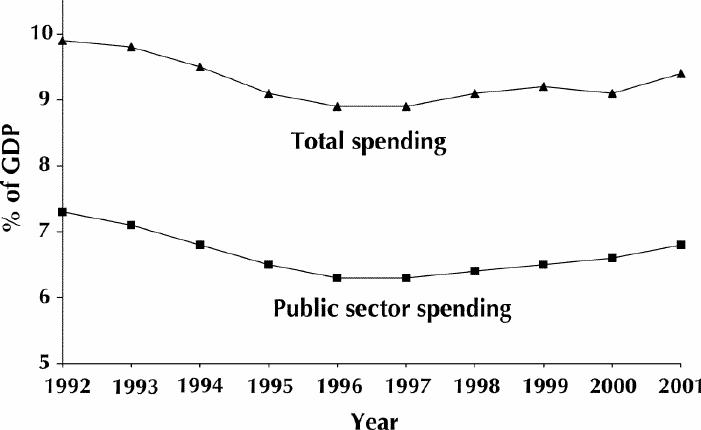
Fig. 1: Public sector spending (by federal and provincial governments) and total spending (including private insurance, employee benefit packages and nonreimbursed private expenditure by individuals) on health care in Canada, 1992–2001. GDP = gross domestic product.
International comparisons reinforce this picture.4 In 1992, only the United States spent more on health, as a proportion of GDP, than Canada did. In 1998, the latest year for which figures are available for international comparisons, both Canada and France spent 9.3%, Germany spent 10.3% and Switzerland spent 10.4% of their national incomes on public and private health care.5,6
The primary reason for Canada's success in constraining expenditures is that a single payer, the government, is responsible for the provision of physician and hospital services. Single-payer funding allows administrative efficiencies and the necessary redirection of spending.7,8 For instance, in the last 2 decades, governments have facilitated a transition to more community-based care and a reduction in the share that hospitals receive of total health spending from 38% to 31.5%.9
Canada's restrained spending has produced long waits in emergency departments for unavailable hospital beds; delays in cataract, joint replacement and cardiac surgery; and the unavailability of needed home care services.10,11 Solving these problems will require increased commitment of resources to health care. Moreover, continuing technological innovation within health care will ensure a high level of ongoing demand for resources. This demand threatens Canada's success both in maintaining equity of delivery of physician and hospital services12 and improving equity in areas such as prescription drugs and home care. By equity, we mean equal access to services irrespective of ability to pay. Public funding of prescription drug plans has provided some degree of equity for the elderly and those on social assistance, as has public funding of some basic home care services. However, limited and variable coverage across provinces has meant that many Canadians suffer financial hardship, or do without the drugs and home care services that they need.
Many refer to the problem of maintaining equitable quality health care as “sustainability.” By sustainability, we mean having mechanisms in place to ensure that Canadians, irrespective of their ability to pay, will have continued access to prompt, technologically current, competent and compassionate health care that addresses the full range of their health needs. The resistance of both federal and provincial governments to committing adequate funds to health care in a planned and consistent fashion represents a serious threat to sustainability.
The political environment is dominated by acrimonious debates between provincial and federal governments that misrepresent historical patterns of health care spending and feature demands by each government that the other should allocate resources to remedy the perceived funding crisis. Existing funding arrangements fail to make either federal or provincial governments accountable for ensuring adequate resources for health care. For instance, the federal government's contribution to spending as part of the agreement that established national medicare was originally tied to the GDP, but the federal government moved away from linking transfers to national wealth during the 1980s.13 In 1995, the federal government unilaterally instituted large cuts in the health care funding available to the provinces. Even in the face of large budget surpluses, the federal government delayed returning funding to 1995 levels for 6 years.
At the same time, the provinces are able to avoid committing increased resources of their own to health care and effectively use the federal money to fund tax cuts. The cumulative impact of the provinces' tax cuts has reduced provincial revenue in 2001/02 by $20 billion relative to the tax regime in place in 1995.14
The current situation allows both levels of government to accuse the other of being responsible for health care delivery problems and for inadequacies in funding, while failing to address the problem.
Only a change in the current funding formula will reverse this situation and ensure accountability by both levels of government. Any solution must ensure that both levels of government acknowledge their responsibility to provide adequate funding for universal access to needed physician, hospital and other health services, without imposing on patients financial barriers to care. Further, provincial governments must acknowledge that the federal contribution to spending entitles the federal government to have a say in how the money is spent. Finally, any workable solution will make transparent the relative contributions of the 2 levels of government to health care spending.
A variety of funding formulas would meet these criteria. Any solution would begin with the provincial and federal governments agreeing to establish the current funding levels as a base situation and instituting mechanisms to ensure that base funding committed to health care is actually spent on health care. We will now focus on how subsequent new funding might be managed.
One mechanism would see the federal and provincial governments agreeing to a minimum per capita public spending level on health indexed to inflation. The federal and provincial governments could then negotiate the proportion of additional expenditures that each would contribute as the population grew. Governments might see an advantage to this strategy in that required increases in health spending would be limited to those dictated by population growth and inflation.
This approach, however, makes no allowance for changes in health care that create needs for increases in per capita funding. In addition, it would not take into account changes in the economy, which has been stable or growing since the Great Depression. A larger GDP provides us with the opportunity to extend the range of public services, including, for instance, home care, drugs, vision care and dental care. This extension would both improve equity and, as with hospital care, enhance efficiency. These considerations suggest that, as a second option, substituting health care expenditure as a proportion of the GDP for per capita spending would be more appealing.
A third proposal would see the federal government matching, in some fixed proportion, new health expenditures by the provinces — as they did when medicare was introduced. In return, the federal government would place conditions on the transfer of funds — also one of the stipulations of the original medicare plan. Advantages of this approach include its incentive for provinces to increase health care spending and its earlier success in achieving equitable national health care delivery.
In negotiating such an arrangement, bargaining issues would include the amount of federal money that would accompany each new dollar of provincial expenditures and the extent of federal control of the conditions under which the money was spent. The larger their contribution, the greater the control the federal government could demand. A large federal contribution would help to minimize rationing and, given the federal government's historical support for universal access, could help maintain access to high-quality care irrespective of ability to pay.
Health care financing in Canada has been characterized by stability of per capita health care funding, by a drop in the proportion of GDP spent on public health care and by tax cuts representing forgone income that governments could have allocated to health care. Strengthening Canadian health care requires a funding formula that remedies the current ability of both provincial and federal governments to cut health care funding indiscriminately and easily obfuscate the situation to mask their cuts. We have presented a number of models of alternative funding arrangements that would make provincial and federal government roles and responsibilities clear and transparent, and would therefore foster accountability and co-operation. Any of these models would provide a foundation for maintaining the health care system that Canadians cherish so proudly.
Footnotes
This article has been peer reviewed.
Contributors: Gordon Guyatt developed the idea for the commentary and wrote the final draft of the paper. Armine Yalnizyan contributed to the evolution of the idea, provided most of the data in the paper, wrote some of the passages and edited the entire manuscript. P.J. Devereaux contributed to the development and evolution of the ideas in the commentary and edited the manuscript.
Competing interests: None declared.
Correspondence to: Dr. Gordon Guyatt, Rm. 2C12, McMaster University Health Sciences Center, 1200 Main St. W, Hamilton ON L8S 4J9; fax 905 524-3841; guyatt@mcmaster.ca
References
- 1.Canadian Institute for Health Information. National health expenditure trends, 1975–2001. Ottawa: The Institute; 2001. Table 1. (Note: CIHI data for 2000 and 2001 are forecast figures.)
- 2.Canadian Institute for Health Information. National health expenditure trends, 1975–2001. Ottawa: The Institute; 2001. Tables 1 and 7.
- 3.Canadian Institute for Health Information. Preliminary provincial and territorial government health expenditure estimates, 1974/5 to 2001/2002. Ottawa: The Institute; 2001. Table A3.
- 4.Deber R, Swan B. Canadian health expenditures: Where do we really stand internationally? CMAJ 1999;160(12):1730-4. Available: www.cmaj.ca/cgi/reprint/160/12/1730 [PMC free article] [PubMed]
- 5.Organization for Economic Cooperation and Development. OECD health data 2001. Washington: The Organization; 2002. Table 10. Available: www .oecd .org /EN /statistics/0,,EN-statistics-12-nodirectorate-no-no--12,00 .html (accessed 2002 June 7).
- 6.World Health Organization. The world health report 2001. Geneva: The Organization; 2002. Statistical annex 5.
- 7.Fuchs VR, Hahn JS. How does Canada do it? A comparison of expenditures for physicians' services in the United States and Canada. N Engl J Med 1990; 323:884-90. [DOI] [PubMed]
- 8.Deber RB, Narine L, Baranek P, Sharpe N, Duvalko DM, Zlotnik-Shaul R, et al. The public-private mix in health care. In: Striking a balance: health care systems in Canada and elsewhere. Vol 4. Ottawa: National Forum on Health; 1998. p. 423-545.
- 9.Canadian Institute for Health Information. National health expenditure estimates, 1975 to 2001. Ottawa: The Institute; 2001. Table 2.
- 10.Sanmartin C, Shortt SE, Barer ML, Sheps S, Lewis S, McDonald PW. Waiting for medical services in Canada: lots of heat, but little light. CMAJ 2000;1629(9):1305-10. Available: www.cmaj.ca/cgi/content/full/162/9/1305. [PMC free article] [PubMed]
- 11.Shortt S, Ford D. Attitudes and activities related to waiting lists for medical services in Canada: a survey of provider, administrative, and consumer groups. In: McDonald P, Shortt S, Sanmartin C, Barer M, Lewis S, Sheps S, editors. Waiting lists and waiting times for health care in Canada: more management!!More money?? Ottawa: Health Canada; 1998. p. 165-92.
- 12.MM Finkelstein. Do factors other than need determine utilization of physicians' services in Ontario? CMAJ 2001;165(5):565-70. Available: www.cmaj.ca/cgi/content/full/165/5/565 [PMC free article] [PubMed]
- 13.Deber RB. Who wants to pay for health care? CMAJ 2000;163(1):43-4. Available: www.cmaj.ca/cgi/content/full/163/1/43 [PMC free article] [PubMed]
- 14.Department of Finance Canada. The fiscal balance in Canada — the facts. Ottawa: Department of Finance Canada; 2002. Available: www .fin .gc .ca /toce/2002/fbcfacts_e.html (last updated 2002 March 9) (accessed 2002 June 5).


