Abstract
Intracranial cystic lesions such as hemangioblastoma (HB) are commonly found incidentally; however, they can be difficult to diagnose because they require various differential diagnoses. A contrast-enhanced mural nodule on magnetic resonance imaging (MRI) is typical and can be diagnosed preoperatively; however, some small nodules cannot be visualised and only cysts may be seen, complicating preoperative diagnosis. In such cases, thorough observation of the cysts is necessary for a definitive diagnosis. To achieve this, minimally invasive surgery, such as endoscopic keyhole surgery, is required. Herein, we report the case of a man in his 50s who presented with an unstable gait, and experienced dizziness for several months. Preoperative MRI revealed a cystic lesion in the left cerebellar hemisphere, without a mural nodule. Although there was no diagnostic evidence of HB, we suspected that the symptoms were caused by this cystic lesion because of its recent occurrence. Upon detecting a mural nodule, we diagnosed it as a cerebellar HB and completely resected it using an endoscopic keyhole approach. The patient's symptoms alleviated postoperatively. The endoscopic keyhole approach may be useful as a less invasive procedure for diagnosing and removing cystic cerebellar HBs, especially for lesions that are difficult to diagnose using preoperative imaging.
Keywords: cerebellar hemangioblastoma, endoscope, keyhole approach
Introduction
Intracranial cystic lesions can be asymptomatic and only require follow-up, such as typical arachnoid cysts; symptomatic, requiring treatment; and secondary to a tumour, requiring treatment.1) Intracranial symptomatic cystic lesions require consideration in the differential diagnosis and indications for surgical treatment. Hemangioblastoma (HB) is a common cystic lesion that requires surgical treatment and can be diagnosed based on specific imaging findings, such as enhanced mural nodules with adjacent non-enhanced surrounding cysts or enhanced solid lesions on magnetic resonance imaging (MRI). However, nodules may not be detected in rare cases, making preoperative diagnosis difficult.2,3) In such cases, sufficient observation of the cyst is necessary to make a definitive diagnosis, and a less invasive procedure, such as endoscopic keyhole surgery, is required. Herein, we report a case of HB in which endoscopic keyhole surgery was effective for diagnosing and removing a symptomatic cystic lesion.
Case Report
Observations
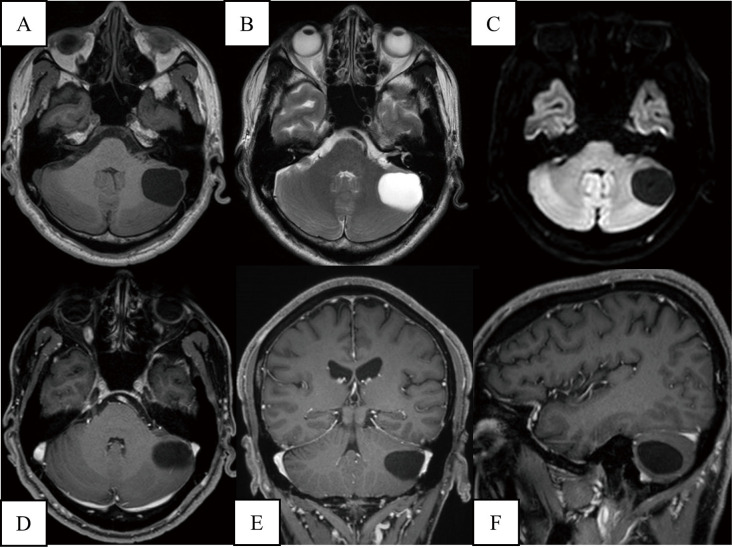
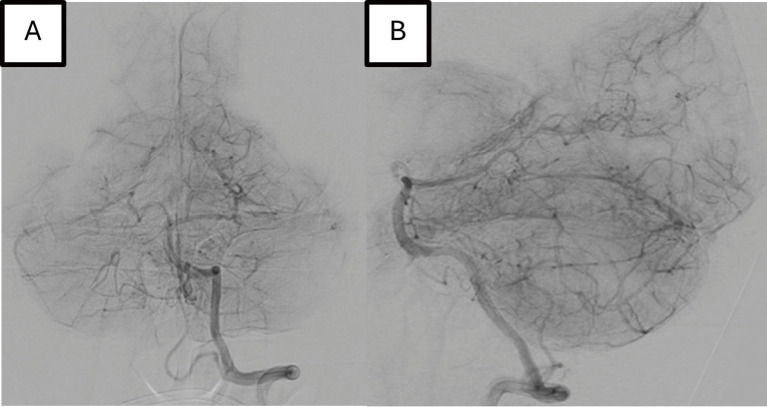
The patient was a man in his 50s with an unstable gait and experienced dizziness for several months. After several months of waiting and observation, the symptoms did not improve, and he was unable to work. He did not have any past medical, medication, or family histories. The patient was conscious, and he had no other neurological deficiencies on admission. Head MRI showed a cystic lesion in the left cerebellar hemisphere. The MRI also showed a low intensity on T1-weighted imaging (T1WI), a high intensity on T2-weighted imaging, and a low intensity on diffusion-weighted imaging (DWI). Contrast-enhanced T1WI showed no nodular lesions. Oedematous changes in the brain around the mass lesion and brainstem compression were not observed (Fig. 1). Digital subtraction angiography revealed no mural nodules or abnormal vessels (Fig. 2). Although there was no diagnostic evidence of HB, we suspected that the patient's symptoms were due to cerebellar syndrome caused by this lesion because it occurred relatively recently. Differential diagnosis to exclude other cystic lesions, such as arachnoid cysts, was required; hence, we considered it necessary to puncture and observe inside the cyst. Consequently, we planned a keyhole approach with a small craniotomy and endoscopic surgery for diagnosis and resection.
Fig. 1.
Preoperative MRI shows a cystic lesion in the left cerebellar hemisphere. It shows low intensity on T1WI (A), high intensity on T2WI (B), and low intensity on DWI (C). Contrast-enhanced T1WI shows no nodular lesion (D-F). There is no oedematous change in the brain around the mass lesion, and no brainstem compression is found. DWI: diffusion-weighted imaging; MRI: magnetic resonance imaging; T1WI: T1-weighted imaging; T2WI: T2-weighted imaging
Fig. 2.
Left vertebral angiograms. A: anterior view, B: lateral view. There is no nodular lesion that could be enhanced.
Surgical findings
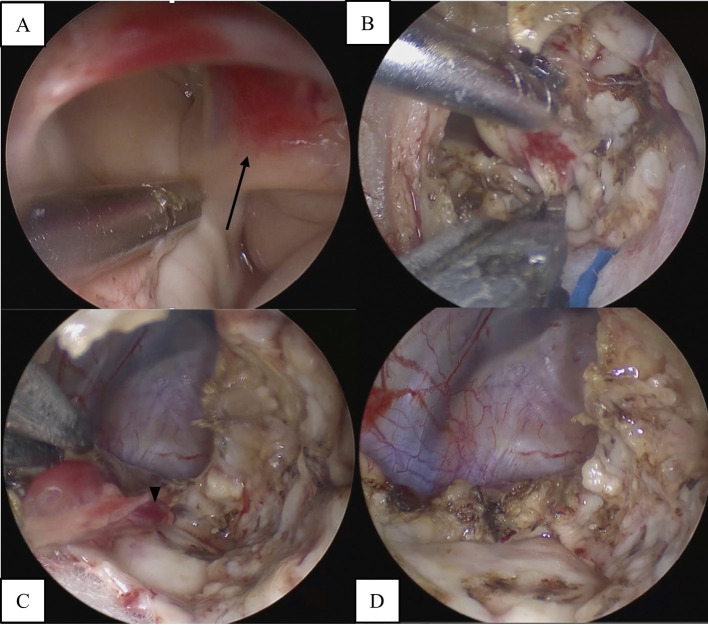
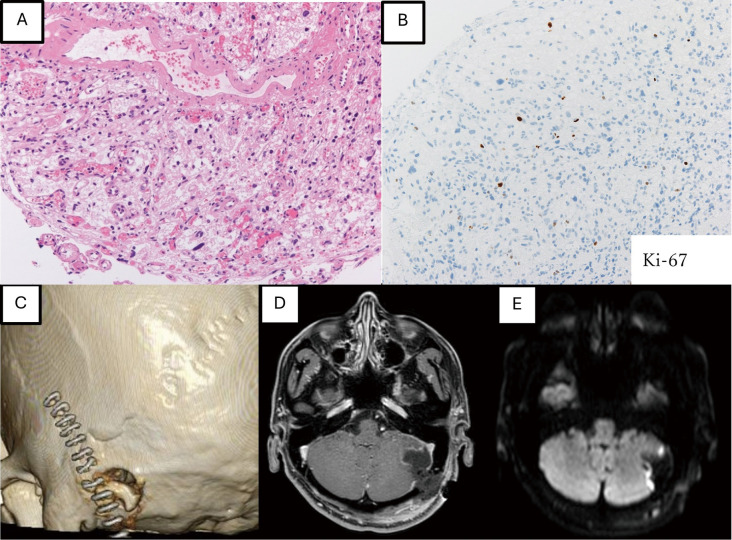
Under general anaesthesia, the patient was placed in the supine lateral position, and the head was fixed with a 3-point pin. We designed the skin incision and craniotomy using a surgical navigation system (StealthStation S8; Medtronic, Minneapolis, MA, USA) and created a 5-cm linear skin incision just above the planned burr hole. A single burr hole was made and enlarged using a diamond drill until the craniotomy reached 2 cm in diameter for endoscopic surgery. After the dural incision, we inserted a 4.0 mm diameter 0º rigid endoscope (Karl Storz Endoscopy Japan, Tokyo, Japan). Under the endoscopic view, we created a surgical corridor to access the cyst and opened it. Xanthochromy-like fluid was drained from the cyst, and we observed the inside of the cyst. A red mural nodule, approximately 3 mm in diameter, was detected on the lateral side of the cyst. Intraoperatively, this lesion was suspected to be a cerebellar HB. Subsequently, the mural nodules were endoscopically resected. We coagulated the small vessels around the tumour containing the cerebellar parenchyma and resected them en bloc (Fig. 3). Pathological findings revealed stromal cells with numerous vacuoles in the stroma and vascular structures in the surrounding area, which is consistent with HBs (Fig. 4).
Fig. 3.
Intraoperative endoscopic view. A red nodule (arrow) is observed (A). Using an endoscope, small vessels are coagulated and drained around the nodule (B, C). Finally, en bloc resection of the nodule is achieved, with the surrounding brain parenchyma intact (D).
Fig. 4.
Pathological findings show that stromal cells with numerous vacuoles are observed in the stroma, and vascular structures are also observed in the surrounding area (A: Haematoxylin-Eosin, 40×). The Ki-67 positivity rate is 3.1% (B: Immunohistochemistry, 40×). Postoperative imaging, a small craniotomy with a diameter of approximately 2 cm is performed (C). MRI shows that the cyst is reduced in contrast-enhanced T1WI (D), and no high-intensity lesion is observed on DWI (E). DWI: diffusion-weighted imaging; MRI: magnetic resonance imaging; T1WI: T1-weighted imaging
Postoperative course
The patient's symptoms alleviate postoperatively, and the cyst shrank, as seen on MRI (Fig. 4). There were no postoperative complications, including cerebrospinal fluid leakage or infection, and the patient was discharged 9 days after surgery. Although additional differential diagnoses were performed to exclude Von Hippel-Lindau disease, there were no other abnormal findings; therefore, this was a single lesion. He returned to work 3 months postoperatively, and there was no recurrence or symptoms for 12 months postoperatively.
Discussion
Intracranial cystic lesions are common conditions found incidentally but can sometimes be difficult to diagnose due to the various differential diagnoses required. They are classified as non-neoplastic or neoplastic, with some requiring only follow-up and others requiring surgical treatment.1) Non-neoplastic cysts include arachnoid, colloid, epidermoid, and dermoid cysts. Neoplastic tumours include gliomas, brain metastases, neuroepithelial tumours, and HBs. HB is a relatively common disease in clinical practice.
HB is a typical cystic mass in the cerebellum. Head MRI, especially contrast-enhanced T1WI, has high sensitivity and specificity and is useful for diagnosis.2) A systematic review of 207 articles and 1,759 cases classified posterior cranial fossa HBs into 4 types. Solid HBs were the most common (47.7%), followed by cystic HBs (26.3%), cystic HBs with mural nodules (21.3%), and both solid and cystic nodules (4.7%).4) However, in some cases, the mural nodules were neither enhanced nor detected on MRI. Therefore, other cystic mass lesions, such as arachnoid cysts, must be considered in the differential diagnosis. Reports have shown that such negative findings can occur in lesions <5 mm in size and with late imaging due to early enhancement of the lesion after contrast administration.2,3) In the present case, the mural nodule was 3 mm in size, and no contrast effect was observed. HBs should be suspected even when only a cystic lesion is observed because they may be accompanied by a small mural nodule.
Surgical treatment is the first choice for symptomatic or hypertrophic HB.1) Good results have been obtained in most cases after surgical treatment, and retrospective reports based on the National Cancer Database showed that gross total resection (GTR) is associated with longer overall survival. GTR has been reported to be the optimal treatment for HBs, even in modern times.5,6) Recently, some case reports showed that endoscopic tumour resection is safe and less invasive for cerebellar HB.7-10) Roach et al.10) described 9 cases of endoscopic resection of cerebellar HBs in 2022. Postoperative complications were absent, and the duration of hospitalisation was shorter than that of the standard transcranial approach. In 2019, Hasegawa et al.7) described 2 cases of endoscopic tumour resection for cystic cerebellar HBs. The major advantage of endoscopy is that it provides a wide view of the surgical field and manoeuvrability, even in small surgical corridors. However, the scope of its use depends on the case. A good indication for this technique in the current case is the tiny mural nodule that is undetected with preoperative imaging. In such cases, detecting the mural nodule and resecting it en bloc under the endoscopic procedures, including feeding arteries and draining veins, may not be difficult. Conversely, in cystic HBs where a feeding artery is detected on preoperative imaging evaluation, the indication for endoscopic procedure should be considered carefully. Although endoscopic resection may be possible using the space of the cyst, it is necessary to consider whether a lesion with high-flow blood supply can be safely resected by endoscopic procedure alone. It is necessary to evaluate the location and angle of the vessels or nodules and to consider the safe insertion and handling of the endoscopic instruments. Furthermore, in solid HB, securing an effective space for the endoscope is difficult, and the advantages of endoscopic procedures are low.
In this report, we demonstrated the usefulness of the endoscopic keyhole approach for diagnosing and resecting a symptomatic single cystic lesion of the cerebellar hemisphere, which was difficult to diagnose with preoperative imaging findings alone. When there is a cystic component, an endoscope may be used within the space of the cyst due to its ease of manipulation for observation or resection inside the cystic wall. When it was difficult to observe with only a 0° endoscope, we used a 30° angled endoscope, which enabled us to visualise the entire cystic wall. This allows even a tiny mural nodule to be observed in a small surgical corridor. Although it is possible to observe the inside of the cyst with a microscope, the surgical field is limited depending on the position of the patient, the size of the cyst, and the location of the mural nodule, and it may be difficult to observe the entire cystic wall from inside. Moreover, we used endoscopy-specific single-shaft instruments and malleable bipolar instruments, which are also used in endoscopic endonasal surgery, to allow easier manipulation, even in a limited surgical corridor. The endoscope can be utilised specifically for lesions requiring wide observation of the deep surgical field.
This case report demonstrates that the endoscopic keyhole approach may be useful as a less invasive procedure for the diagnosis and removal of cystic cerebellar HBs, especially for lesions that are difficult to diagnose using preoperative imaging.
Submission Statement
This manuscript is original and has not been submitted elsewhere in part or entirety.
Conflicts of Interest Disclosure
All authors have no conflict of interest.
Acknowledgments
We would like to thank Editage (www.editage.jp) for the English language editing.
References
- 1). Taillibert S, Le Rhun E, Chamberlain MC: Intracranial cystic lesions: a review. Curr Neurol Neurosci Rep 14: 481, 2014 [DOI] [PubMed] [Google Scholar]
- 2). Matsusue E, Inoue C, Tabuchi S, et al. : Advanced magnetic resonance imaging findings of cerebellar hemangioblastomas: a report of three cases and a literature review. Acta Radiol Open 11: 20584601221077074, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3). Lopes Dos Santos A, Trevas S, Rosado ML: A challenge in diagnosis of cerebellar hemangioblastoma. Cureus 14: e21713, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4). Kuharic M, Jankovic D, Splavski B, Boop FA, Arnautovic KI: Hemangioblastomas of the posterior cranial fossa in adults: demographics, clinical, morphologic, pathologic, surgical features, and outcomes. A systematic review. World Neurosurg 110: e1049-e1062, 2018 [DOI] [PubMed] [Google Scholar]
- 5). Huang Y, Chan L, Bai HX, et al. : Assessment of care pattern and outcome in hemangioblastoma. Sci Rep 8: 11144, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6). Giannetti AV, Rocha MD, Rosseto RS, Pedrosa HA: Pure neuroendoscopic resection of cystic cerebellar tumors. World Neurosurg 84: e7-e11, 2015 [DOI] [PubMed] [Google Scholar]
- 7). Hasegawa H, Shin M, Kin T, Saito N: Fully endoscopic minimally invasive tumor resection for cystic cerebellar hemangioblastoma. World Neurosurg 126: 483-490, 2019 [DOI] [PubMed] [Google Scholar]
- 8). Novak Z: Endoscopic cure of cerebellar hemangioblastoma. Bratisl Lek Listy 105: 8-10, 2004 [PubMed] [Google Scholar]
- 9). Di X: Multiple brain tumor nodule resections under direct visualization of a neuronavigated endoscope. Minim Invasive Neurosurg 50: 227-232, 2007 [DOI] [PubMed] [Google Scholar]
- 10). Roach J, Livermore L, Plaha P: Endoscope-assisted resection for cystic cerebellar hemangioblastomas. World Neurosurg 167: e217-e221, 2022 [DOI] [PubMed] [Google Scholar]