Abstract
Purpose
To determine the level of uptake of telemedicine among postgraduate obstetrics and gynaecology (O&G) trainees in London, and how they perceive its impact on their training.
Methods
A mixed-methods survey aimed at exploring trainee perspectives of telemedicine use in clinical practice and its implications for training. Study participants were O&G specialist doctors on the London (UK) training programme. The survey was distributed to the 2022 cohort via Email communication facilitated by Health Education England.
Results
The response rate was 46.3% (118/255). Of respondents, 96% (113/118) had experience of telemedicine, in a range of clinical environments; 91% (106/117) felt telemedicine should become embedded in O&G practice (the most frequent reported advantage was time-saving and a barrier was language translation); 43% of trainees (50/116) stated that they were unable to attain effective clinical training during telemedicine appointments; and 70% (81/116) indicated a preference for remote online teaching. The majority of trainees (75%) had some level of experience in the use of technology in clinical training, encompassing various modalities including surgical and ultrasound simulation, remote real-time training and virtual reality patient consultations. Trainee responses, on the whole, reflected a lack of confidence in their ultrasound skills; 79.5% (74/93) of trainees responsible for acute gynaecology admissions reported that at least 25% of admissions were for deferred ultrasound scanning investigation. Most trainees anticipated that real-time remote supervision for both USS and laparoscopy would enhance training opportunities and expedite time to patient diagnosis and management. Anticipated barriers included concerns regarding the uptake of technology and connectivity issues.
Conclusion
Telemedicine for clinical care has been demonstrated to be well-received by most O&G trainees. However, it is necessary to consider effective O&G training when delivering telemedicine. Technology gives rise to a number of training opportunities, with the development of online teaching, telementoring and simulation. Trainees report both advantages and disadvantages which should be carefully considered to optimise postgraduate O&G training.
Keywords: telemedicine, postgraduate training, obstetrics and gynaecology
Introduction
The use of technology has revolutionised the provision of healthcare services, with a significant increase in uptake in recent years. Traditionally, doctor–patient relationships have been shaped by in-person interactions, which include history-taking, physical examination, investigations and treatment. However, telemedicine involves the use of communication and information technology to provide clinical care for patients from a remote location.1–3 The COVID-19 pandemic played a crucial role in accelerating the uptake of integrating technology in healthcare. This prompted IT systems, healthcare systems, clinicians and patients to establish the necessary infrastructure for effective telemedicine consultations. These changes were implemented to ensure that essential healthcare services could still be delivered while maintaining social distancing measures and facilitating the ongoing provision of care to patients who were in isolation.
The desire to prevent the spread of Covid-19 was greater than the challenges posed by the integration of technology in healthcare. As a result, telemedicine has now become a regular aspect of daily medical practice and it is evident that its benefits, to both patients and clinicians, continue even after the pandemic (as per the NHS England 2019 NHS Long Term Plan). However, disadvantages have been suggested with regards to negative experiences and the risk of diagnostic inaccuracies using telemedicine.4,5 The swift adoption of technology and adaptation of clinical consultations and patient pathways were aimed at reducing human-to-human exposure during the Covid-19 pandemic. The adoption of telemedicine in mainstream practice was not established with training as a consideration. Now, three years on, we evaluate the impact on postgraduate training.
This study aims to help better understand trainees’ perceptions of telemedicine, and their views on its use in postgraduate training. The rationale of the study is to determine whether trainees perceive telemedicine to have impacted training and whether the uptake of telemedicine can be optimized to benefit O&G trainees. The survey has a particular focus on evaluating O&G ultrasound scanning (USS) and laparoscopy training and whether telementoring would be well received by trainees.
Methods
Study Design
An in-depth survey investigating trainee perspectives on telemedicine, its use in clinical practice and impact on training, was designed based on previously published questionnaires6,7 and a systematic review of telemedicine in gynaecology.8 The methodology for survey development and validation was developed following a literature review.9–11 Feedback on the questionnaire and content validation were gathered from a combination of five O&G trainees and consultants involved in postgraduate O&G training. Input was derived to ensure the survey addressed the topic and there were no issues with question comprehension. Anonymity was a priority to ensure participation with genuine responses, thus minimal demographic data were collected.
The final study questionnaire is attached within the Supplementary Material. The survey was sent out to a small group of trainees 3 months apart to ensure there was no difference in responses. The final survey was circulated using Microsoft Forms via Health Education England to postgraduate O&G trainees in London in September 2022, a total of 255 potential participants. Approximately 10–20 minutes was given to complete the questionnaire. Participants were free to withdraw at any point during the questionnaire up until the point of submission, and all responses were anonymous. No personal health information or identifiable information was collected as part of the survey.
Closed, multiple-choice questions, Likert scale or rating scale questions, presented as descriptive statistics analysed via Excel and SPSS version 26, were used to analyse and compare data between postgraduate training level groups (senior house officer [SHO], junior registrar and senior registrar). The chi-squared test was applied for categorical data and the Kruskal–Wallis test for ordinal data, with Likert score results. Fewer open-ended questions were included, which allowed for simple thematic qualitative analysis.12 There were three sections to the questionnaire: 1. Demographics, 2. Telemedicine in O&G Trainees’ Patient Consultations, and 3. Telemedicine in O&G Trainee Education.
Study Participants
The study participants were doctors on the obstetrics and gynaecology specialist training programme in London, UK (North West/North Central and East/South). All individuals on the programme in 2022 were contacted via Email and asked to participate.
Ethical Approval
The study was reviewed by the Education Ethics Review Process team at Imperial College London and ethical approval was granted (EERP2223-001).
Results
Demographics
The survey was sent to 255 individuals. The response rate was 46.3% (118/255). The breakdown by year of speciality training for the 118 respondents is outlined in Table 1. Of these individuals, 33.9% (40/118) were SHOs (ST1-2), 44.1% (52/118) were junior registrars (ST3-5) and 22% (26/118) were senior registrars (ST6-7).
Table 1.
Survey Respondent O&G Speciality Training Level
| Speciality Training Year | Number of Respondents | % Total Respondents |
|---|---|---|
| ST1 | 22 | 19% |
| ST2 | 18 | 15% |
| ST3 | 18 | 15% |
| ST4 | 18 | 15% |
| ST5 | 16 | 14% |
| ST6 | 13 | 11% |
| ST7 | 13 | 11% |
Telemedicine in O&G Trainees’ Patient Consultations
Use of Telemedicine
Among respondents, 96% (113/118) had participated in patient encounters using telemedicine. Of those, 80% (90/113) had participated in telemedicine using telephone consultations only, 19% (21/113) had used both telephone and video consultations, and <2% (2/113) had used video consultations only. Of the 5 respondents (4%) who had not participated in patient encounters using telemedicine, 3 felt that clinical appointments were not required at their stage of training, and 2 that the clinic/hospital was not set up to deliver telemedicine.
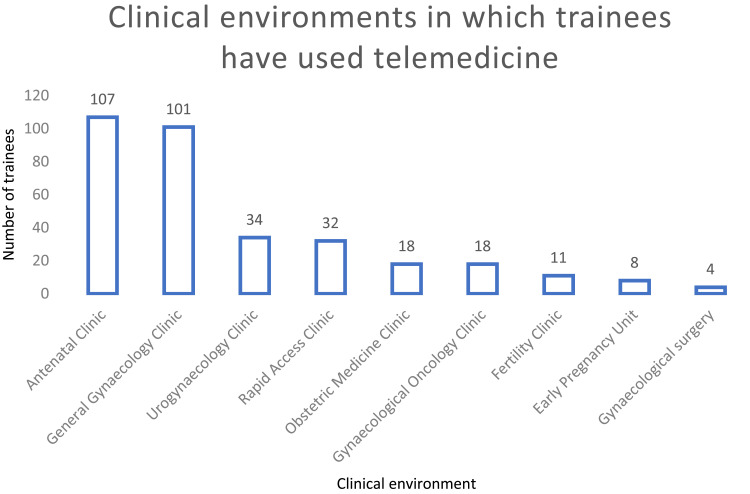
Trainees had used telemedicine in a range of clinical environments (Figure 1), with the majority using it in the antenatal clinic (95%) and general gynaecology clinic (89%, n=116). The use of telemedicine by trainees was lower in environments where specific equipment is likely to be needed, such as ultrasound/colposcopy.
Figure 1.
Range of clinical environments in which O&G trainees have used telemedicine in clinical practice.
Value of Telemedicine in Consulting Patients
Of respondents, 91% (106/117) felt that telemedicine should become a permanent part of O&G practice. There was no statistical difference between postgraduate training level groups (SHO, junior registrar and senior registrar): X2 = 0.351 (p-value 0.84). In general, respondents did not find telemedicine patient encounters more difficult to conduct than in-patient visits (median = 5, where 1 = much easier and 10 = much more difficult than in-patient visits; interquartile range [IQR] = 3, n = 116). Trainees found that telemedicine consultations saved time in comparison to those conducted in person (median = 4, where 1 = saves significant time and 10 = takes significantly more time; IQR = 2, n = 115). No specific reasons were given to explain the time-saving achieved by telemedicine consultations compared to face-to-face consultations.
Indeed, 77% (90/117) of respondents felt that they were fully successful in conducting at least three-quarters of their telemedicine patient consultations, with the majority of them booking a face-to-face follow up for their telemedicine consultations less than 50% of the time.
Barriers to Telemedicine in Patient Consultations
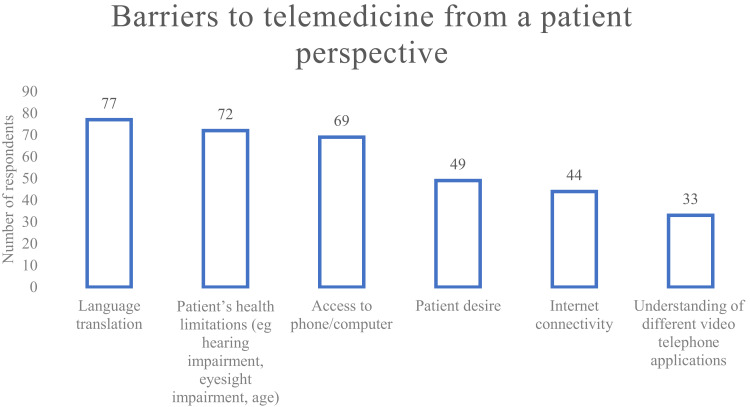
Trainees felt that the commonest barrier experienced by patients in telemedicine consultations was language translation, an issue reported by 66% (77/116) of respondents. 41% (46/113) of respondents felt that they did not have easy access to an interpreter in telemedicine consultations. Other issues reported by more than half of respondents were patient health limitations, such as hearing or eyesight impairment, and lack of access to the required technology, such as a phone or computer. Less than 50% of respondents stated that patient desire for a face-to-face appointment, internet connectivity and understanding the different video/telephone applications acted as barriers (Figure 2).
Figure 2.
Barriers to telemedicine from a patient perspective, as reported by O&G trainees.
Appropriateness of Telemedicine
The majority (73%, 84/115) of trainees felt that telemedicine was inappropriate for consultations involving the management of post-operative complications; 57% (66/115) did not think the discussion of detailed surgical plans with patients was suitable for tele-consultation and 50% (58/115) felt that the first post-operative appointment was not suitable for telemedicine.
Telemedicine in O&G Trainee Education
Effectiveness of Telemedicine in Clinical Training
Of respondents, 43% (50/117) felt that they had not managed to achieve effective clinical training with telemedicine appointments. There was no statistical difference between postgraduate training level groups (SHO, junior registrar and senior registrar): X2 = 0.070 (p-value 0.97). Of the 57% (67/117) of trainees who had achieved effective clinical training with telemedicine appointments, 61% (41/67) felt that telemedicine consultations were useful when they had obtained the patient’s medical history, presented to the senior, received feedback and then finished the consultation alone. 22% (15/67) felt that telemedicine consultations were useful when they obtained the patient’s history, presented to the senior, received feedback but the senior colleague finished the consultation alone. Only 10% (7/67) felt that it was useful when they finished the consultation with a senior colleague, and 6% (4/67) of respondents felt that it was useful when they saw the patient together with the senior observing the interaction with the patient.
Remote Teaching
Of respondents, 97% (113/116) had attended teaching sessions remotely online. Of those, 48% (54/113) were able to attend more than three-quarters of virtual training sessions, which is a requirement of the training programme. 70% (81/116) of trainees preferred remote teaching to in-person sessions.
Trainees who had attended <75% of remote teaching sessions were asked to outline the reasons why they had done so. In total, there were 37 responses to this question, with the majority (92%, 34/37) reporting that this was due to rota or on-call commitments. The other reasons are described in Table 2.
Table 2.
Reasons for Trainees Not Attending ≥75% of Regional Remote Teaching, n = 37
| Reason | N | Reason | N |
|---|---|---|---|
| Rota/on-call/nights/zero days | 34 | Teaching not punctual | 2 |
| Annual leave | 5 | Other educational activity | 1 |
| Virtual teaching cancelled | 3 | Maternity leave | 1 |
| Poor communication on session details | 2 | Childcare | 1 |
| Lack of cover | 2 | Teaching not protected when remote | 1 |
Technology in Obstetrics Training
Of trainees, 68% (77/114) stated that they had no experiences involving the use of technology for training within obstetrics. Of the 37 trainees who had experience, 28 had experienced ultrasound simulation, 10 had experienced virtual reality practical skills, 3 had experienced virtual reality patient consultation and 1 had experienced ultrasound real-time remote training. One respondent reported that they had created virtual reality patient consultations for medical students but had not themselves been trained in using them.
Technology in Gynaecology Training
In contrast, the majority of trainees reported that they did have experience of using technology for training in gynaecology. Only 25% (29/114) stated that they had no experiences involving the use of technology for gynaecology training. Of the 75% (85/114) who had experience, 92% (78/85) had experienced laparoscopy simulation, 47% (40/85) had experienced hysteroscopy simulation and 27% (23/85) had experienced ultrasound simulation. Only 6% (5/85) of respondents had experienced some form of remote real-time training.
Trainee Perspectives on Remote Supervision in Gynaecology
Ultrasound Scanning in Acute Gynaecology
Trainees overall were low in confidence in their USS skills (median = 3, where 1 = not at all confident and 10 = very confident; IQR = 4, n = 102). Analysis across the three postgraduate levels (SHO, junior registrar and senior registrar) using the Kruskal–Wallis test applied to the Likert scores had a result of 20.22 (p-value = 4.06×10-5), demonstrating that there was a statistically significant difference in confidence in ultrasound skills among the three groups. The median confidence levels for the three groups were 2.0 (ST1–2, SHOs), 3.0 (ST3–5, junior registrars) and 7.0 (ST6–7, senior registrars).
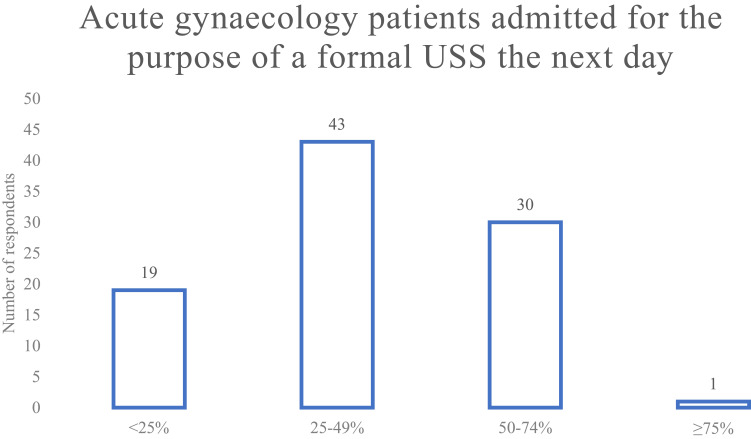
Of all postgraduate trainees, 89% (88/99) stated that they admit patients out of hours for a formal USS the next day. Figure 3 outlines what proportion of acute gynaecology admissions trainees estimate are being admitted for the purpose of a formal ultrasound scan the next day. Eighty-six per cent (85/99) of trainees stated that they are never involved in supervision of more junior trainees’ ultrasound scanning, whilst 6% did so monthly, 6% did so weekly and 2% did so daily (n = 99).
Figure 3.
Proportion of acute gynaecology patients admitted by O&G trainees for a formal USS the next day.
Remote Supervision for Acute Gynaecology Ultrasound Scanning
Overall, trainees tended to believe that remote ultrasonography supervision would improve patient time to diagnosis (median = 7, where 1 = no improvement at all and 10 = definite significant improvement; IQR = 2, n = 102).
Open-ended questions on the benefits and disadvantages of remote USS supervision as perceived by trainees each drew 57 responses. The most commonly stated benefit of remote USS supervision was increased training opportunities (74%, 42/57), followed by improving the patient pathway (54%, 31/57). The potential benefits put forward by trainees are outlined in Table 3.
Table 3.
O&G Trainee Responses on Potential Benefits of and Barriers to Remote USS Supervision
| Benefit of remote USS supervision, n = 57 | N |
|---|---|
| Increased opportunities for training | 42 |
| Improved patient pathway | 31 |
| Reduced time to diagnosis | 30 |
| Increased quality of training | 23 |
| Improved trainee confidence in USS judgement | 4 |
| Improved patient satisfaction | 2 |
| Allowed scanning out of hours | 2 |
| Improved patient safety | 1 |
| Barriers to remote USS supervision, n=57 | N |
| Uptake of technology by trainers | 35 |
| Remote connectivity issues | 22 |
| Remote image quality | 13 |
| Insufficient trainee experience for remote supervision to be sufficient | 8 |
| Uptake of technology by trainees | 7 |
| Patient acceptance | 3 |
| Availability of scanning machines/equipment | 3 |
| Missing diagnoses/pathology | 2 |
| Affordability | 2 |
Overall, trainees agreed that remote USS supervision would improve patient time from presentation to definitive management (theatre) (median = 7, where 1 = no improvement at all and 10 = definite significant improvement; IQR = 3, n = 98).
The commonest reported barrier was the uptake of this technology by trainers (61%, 35/57), followed by the possibility of remote connectivity issues (39%), or problems with remote image quality (23%, 13/57). All the potential barriers to remote gynaecology ultrasound supervision put forward by trainees are outlined in Table 3.
Trainees and Acute Gynaecological Surgery
Of respondents, 58% (59/102) performed acute gynaecology surgery out of hours (n = 102). Of those who do so, 93% (55/59) performed 5 or fewer procedures out of hours per month, and 7% (4/59) performed between 6–10 procedures per month; none performed more than this. In terms of all laparoscopic procedures, 89% (86/97) of trainees performed 5 or fewer procedures per month and 11% (11/97) performed between 6–10; none performed more than this. Overall, trainees were relatively underconfident in their laparoscopy skills (median = 3, where 1 = not at all confident and 10 = completely confident; IQR = 4, n = 102). The distribution of trainees participating in this survey must be taken into account; that is, more junior trainees were not projected to perform acute surgery.
Value of and Barriers to Remote Supervision for Laparoscopic Procedures
This open-ended question drew 46 responses. The majority of trainees felt that having remote supervision during laparoscopy procedures would increase training opportunities (59%, 27/46). The potential benefits of remote laparoscopy supervision put forward by O&G trainees are outlined in Table 4.
Table 4.
O&G Trainee Responses on Potential Benefits of and Barriers to Remote Gynaecology Laparoscopy Supervision
| Benefit of remote laparoscopy supervision, n = 46 | N |
|---|---|
| Increased opportunities for training | 27 |
| Reduced time to surgery | 19 |
| Increased quality of training | 18 |
| Increased patient access to laparoscopy | 15 |
| Improved patient pathway | 14 |
| Improved trainee confidence/skills in laparoscopy | 5 |
| Supported intra-operative diagnosis/decision making | 3 |
| Improved patient satisfaction | 1 |
| Improved workforce allocation | 1 |
| Barriers to remote USS supervision, n = 47 | N |
| Uptake of technology by trainers | 25 |
| Uptake of technology by theatre teams | 20 |
| Remote connectivity issues | 17 |
| Patient acceptance | 12 |
| Remote image quality | 11 |
| Uptake of technology by trainees | 9 |
| Risk of help being far away if there are complications | 5 |
| Lack of trainee experience in laparoscopy for virtual supervision to be sufficient | 4 |
| Accessing software | 1 |
The commonest reported barrier was the uptake of remote technology by trainers (53%, 24/46), followed by uptake of technology by theatre teams (43%, 20/46). The potential barriers to remote laparoscopy supervision put forward by O&G trainees are outlined in Table 4.
Discussion
Main Findings
This study is novel in its exploration of obstetrics and gynaecology trainees’ views and experience of the uptake of telemedicine in clinical practice and training within the speciality in the UK. Other studies have merely demonstrated the value of telemedicine in various specialities prior to Covid-19.13,14 The post-pandemic utilisation of telemedicine by postgraduate O&G trainees in clinical practice in the UK and its impact on training in postgraduate obstetrics and gynaecology have yet to be explored. In this study, we found that the majority of trainees have used telemedicine in clinical practice, and agree that telemedicine can form an effective part of the patient journey. However it is clear that the integration of telemedicine must be carefully considered, and caveats established regarding its optimum use in patient care and the impact on training.
This study demonstrates the wide variety of clinical scenarios in which telemedicine has been incorporated within obstetrics and gynaecology clinical practice post-pandemic. A systematic review of telemedicine used in gynaecology prior to the pandemic8 demonstrates the relatively limited use of telehealth prior to its rapid uptake when Covid-19 acted as a catalyst in terms of removing barriers to technology. In this survey, focused questions on optimum scenarios for telemedicine demonstrated that trainees agree that there are certain clinical encounters in which telemedicine is not suitable; in particular, management of post-operative complications and consultations regarding surgical planning. Establishing thresholds to determine which clinical scenarios are suitable for use of telemedicine will be an important part of future practice; it is likely these will be patient-, clinician- and scenario-specific.
Barriers to telemedicine consultations prior to the Covid-19 pandemic focused on lack of access to technology; however, Covid-19 served as a disruptor that shifted uptake of telemedicine. In this survey of postgraduate trainees, the majority did not report patient or clinician use of technology as a barrier. However, it is important to note the lack of access to technology in certain patient groups, and the potential implications for health inequality, which was of particular significance when alternative, in-person appointments were not available for consultations that would otherwise be appropriate for telemedicine.15 Interestingly, the most frequently cited barrier was access to language translation (41%). This suggests that there is scope to improve technology to streamline access to translation services whilst using telemedicine. Of note, this survey took place in London, which comprises a significant migrant population; thus, viewing language translation as a particular barrier is likely to be a larger issue for this cohort. Language translation presents a potential challenge to in-person consultation too; however, telemedicine could exacerbate language barriers due to impaired non-verbal communication and reduced use of visual aids through telemedicine.15 It may be necessary to formally examine patient understanding following consultations involving language barriers to determine whether telemedicine is appropriate in this scenario.
A focus of this study is how telemedicine has impacted training opportunities. We found that the current practice of telemedicine consultations does not always lend itself to training, with 43% trainees feeling that they have not managed to achieve effective training. The organisation of appointments was explored further and trainees reported that the optimum timeline was when they obtained the history, presented to the senior, received feedback, and then finished the consultation alone. A focus on training at the outset of clinics and an agreement between trainee and trainer on how best to seek help and ensure ongoing training within the setting of telemedicine consultations is important to establish and ensure that training is kept a priority when harnessing telemedicine to optimise delivery of patient care.16
Most of the relevant literature available assesses the move to online teaching from traditional face-to-face didactic teaching for postgraduate trainees; few studies evaluate specifically the impact of delivering regional deanery speciality training online. The majority of these articles stem from the changes seen in medical education of trainees as a result of the Covid-19 pandemic.17–20 The move to online delivery was implemented as a necessity in a short space of time. In this study, we found that 70% of O&G trainees preferred remote teaching to in-person sessions. However, an important point raised by some studies20,21 is the importance of social interaction between peers, which face-to-face teaching provides. Winn 21 describes trainees reporting that “they missed the social interactions that were part of in-person didactic conferences”. Our survey did not explore trainees’ views on the advantages or disadvantages of remote teaching in general; however, the qualitative question exploring why trainees had not attended >75% teaching outlined that rota commitments had an impact. Therefore, having access to remote teaching that can also be viewed at a later date is likely to be the reason why the majority of trainees preferred remote regional postgraduate training. However, an important consideration is how comfortable trainees feel about asking questions in remote teaching, and the fact that there is likely to be less interaction between trainees and tutors if teaching sessions are viewed retrospectively.22 Furthermore, learners may be more likely to become distracted when teaching is virtual, and if teaching can be viewed at a later time, protected teaching time for trainees may be more likely to be compromised by clinical demands.
One section of our study focused on the use of technology specific to training. Interestingly, the majority of trainees did not have any experience of technology applications in obstetric training. However, most (75%) did have experience of gynaecology training. Within this cohort, the majority had had exposure to laparoscopy simulation training. Few trainees had experience of virtual reality training or real-time telementoring. This exposure to technology specific to training is likely to change in coming years.
Qualitative data demonstrated that trainees anticipate real-time remote USS supervision would increase their training opportunities and exposure to the necessary skills. The value of having direct supervision during USS via telementoring has been demonstrated by previous studies,13,14 which revealed overall trainee satisfaction with telemedicine training for USS. Perceived barriers in our study were in line with those reported by users regarding telemedicine prior to the shift in attitudes following the Covid-19 pandemic. These barriers include uptake of technology and connectivity issues. It would be useful in future studies to explore the acceptability of remote USS from the perspective of senior colleagues who have overall responsibility for acting on the findings. Overall, however, real-time remote ultrasound supervision could provide an opportunity to increase access to training and reduce time to patient diagnosis, which may improve trainee confidence in USS.
Despite COVID-19 impacting elective gynaecology surgery training more than other areas,23 the prospect of remote supervision in surgery was less well-received by this cohort of trainees. Although the majority did think the technology would increase training opportunities, the increased risks associated with surgery compared to USS led to the majority of trainees disagreeing that the technology would reduce patient time to theatre. In many surgical cases, the physical presence of a named consultant is required and there were safety concerns raised in the open questions regarding barriers to this technology.
Strengths and Limitations
The limitations of our study include the response rate, which was 46.3%. We attempted to increase uptake by sharing the link to the survey via QR code during a face-to-face conference specifically for London O&G trainees. Despite increasing the response rate, it was difficult to achieve further responses because shift patterns and rota allocation meant not all trainees attended. In anticipation of a lower than complete response rate, we did not collect demographic data for the respondents aside from their year of training, as this could lead to identification of the individual participant and thus potentially affect how the survey was answered. Thus, as a cohort, we were unable to conduct analyses between sub-groups of trainees. Although we focused on trainee perspectives, we did not determine trainer perspectives in light of the impact of telemedicine on postgraduate O&G training. We also relied on trainees’ perceptions of the barriers of telemedicine in their practice, whereas ideally patient views would be sought in future studies. Lastly, a questionnaire response data source is subjective and does not provide us with objective outcome changes pre and post the increased uptake of telemedicine in clinical care. However, this survey does provide an overview of the impact of telemedicine on O&G training and offers insights into how this can be developed and optimised moving forwards past the COVID-19 pandemic.
Conclusion
Our survey shows that trainees think telemedicine offers both advantages and disadvantages to postgraduate O&G training. It is clear that the change in practice is now well-established, with 98% of participants having used telemedicine in clinical practice, and thus opportunities must be tailored to ensure ongoing good quality training to produce the O&G consultants of the future. Disadvantages include an impact on hands-on training, technical difficulties and development of communication skills. However, the benefits include increased access to training opportunities, enhanced patient care with change in options for monitoring, improved efficiency and greater productivity. Furthermore, technology development offers specific training opportunities that need to be standardised in terms of access and potentially utilised in assessment for progression. The healthcare landscape is changing and telemedicine plays a key role in this, thus ensuring focused attention is given to optimise O&G training in this context is important and will prepare clinicians for the future.
Data Sharing Statement
The datasets generated and analysed during the current study are not publicly available due to combinations of answers making individuals participating potentially identifiable. However, individual question response data are available from the corresponding author on reasonable request.
Ethical Approval and Consent to Participate
The study was reviewed by the Education Ethics Review Process team at Imperial College London and ethical approval was granted (EERP2223-001). Informed consent was obtained from all participants.
Disclosure
Professor Tom Bourne reports personal fees, non-financial support from Samsung Healthcare, non-financial support from GE Healthcare, non-financial support from Illumina, non-financial support from Roche Diagnostics and non-financial support from Abbott during the conduct of the study. The authors report no other conflicts of interest in this work.
References
- 1.DeNicola N, Grossman D, Marko K, et al. Telehealth interventions to improve obstetric and gynecologic health outcomes: a systematic review. Obstet Gynecol. 2020;135(2):371–382. doi: 10.1097/AOG.0000000000003646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stanberry B. Telemedicine: barriers and opportunities in the 21st century. J Intern Med. 2000;247(6):615–628. doi: 10.1046/j.1365-2796.2000.00699.x [DOI] [PubMed] [Google Scholar]
- 3.Council. EEGM. Regulatory approach to telemedicine; 2018.
- 4.Sloan M, Lever E, Harwood R, et al. Telemedicine in rheumatology: a mixed methods study exploring acceptability, preferences and experiences among patients and clinicians. Rheumatology. 2022;61(6):2262–2274. doi: 10.1093/rheumatology/keab796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rosen R, Wieringa S, Greenhalgh T, et al. Clinical risk in remote consultations in general practice: findings from in-COVID-19 pandemic qualitative research. BJGP Open. 2022;6(3):BJGPO.2021.0204. doi: 10.3399/BJGPO.2021.0204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shah A, Skertich NJ, Sullivan GA, et al. The utilization of telehealth during the COVID-19 pandemic: an American pediatric surgical association survey. J Pediatr Surg. 2022;57(7):1391–1397. doi: 10.1016/j.jpedsurg.2022.01.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yeoh SA, Young K, Putman M, et al. Rapid adoption of telemedicine in rheumatology care during the COVID-19 pandemic highlights training and supervision concerns among rheumatology trainees. ACR Open Rheumatol. 2022;4(2):128–133. doi: 10.1002/acr2.11355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murugesu S, Galazis N, Jones BP, et al. Evaluating the use of telemedicine in gynaecological practice: a systematic review. BMJ Open. 2020;10(12):e039457. doi: 10.1136/bmjopen-2020-039457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Artino AR Jr, La Rochelle JS, Dezee KJ, Gehlbach H. Developing questionnaires for educational research: AMEE Guide No. 87. Med Teach. 2014;36(6):463–474. doi: 10.3109/0142159X.2014.889814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burns KE, Duffett M, Kho ME, et al. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ. 2008;179(3):245–252. doi: 10.1503/cmaj.080372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Boynton PM, Greenhalgh T. Selecting, designing, and developing your questionnaire. BMJ. 2004;328(7451):1312–1315. doi: 10.1136/bmj.328.7451.1312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 13.Winn S, McKeown P, Lotfipour S, et al. Remote, synchronous, hands-on ultrasound education. Telemed J E Health. 2015;21(7):593–597. doi: 10.1089/tmj.2014.0050 [DOI] [PubMed] [Google Scholar]
- 14.Al-Kadi A, Dyer D, Ball CG, et al. User’s perceptions of remote trauma telesonography. J Telemed Telecare. 2009;15(5):251–254. doi: 10.1258/jtt.2009.081007 [DOI] [PubMed] [Google Scholar]
- 15.Galle A, Semaan A, Huysmans E, et al. A double-edged sword-telemedicine for maternal care during COVID-19: findings from a global mixed-methods study of healthcare providers. BMJ Glob Health. 2021;6(2):e004575. doi: 10.1136/bmjgh-2020-004575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gynaecologists) RRCoOa. RCOG Training in Gynaecological Surgery Recovery Plan; 2021. [Google Scholar]
- 17.Al-Ahmari AN, Ajlan AM, Bajunaid K, et al. Perception of neurosurgery residents and attendings on online webinars during COVID-19 pandemic and implications on future education. World Neurosurg. 2021;146:e811–e6. doi: 10.1016/j.wneu.2020.11.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aziz H, James T, Remulla D, et al. Effect of COVID-19 on surgical training across the United States: a national survey of general surgery residents. J Surg Educ. 2021;78(2):431–439. doi: 10.1016/j.jsurg.2020.07.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosen GH, Murray KS, Greene KL, Pruthi RS, Richstone L, Mirza M. Effect of COVID-19 on urology residency training: a nationwide survey of program directors by the society of academic urologists. J Urol. 2020;204(5):1039–1045. doi: 10.1097/JU.0000000000001155 [DOI] [PubMed] [Google Scholar]
- 20.Sleiwah A, Mughal M, Hachach-Haram N, Roblin P. COVID-19 lockdown learning: the uprising of virtual teaching. J Plast Reconstr Aesthet Surg. 2020;73(8):1575–1592. doi: 10.1016/j.bjps.2020.05.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Winn AS, Myers R, Grow HM, et al. Pediatric resident perspectives on the impact of COVID-19 on training. Hosp Pediatr. 2021;11:e373–e384. doi: 10.1542/hpeds.2021-005994 [DOI] [PubMed] [Google Scholar]
- 22.Dost S, Hossain A, Shehab M, Abdelwahed A, Al-Nusair L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ Open. 2020;10(11):e042378. doi: 10.1136/bmjopen-2020-042378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Currie JLD, Saso S, Guerrero K, Davies M. Impact of covid-19 on subspecialty training in obstetrics and gynaecology. J Obstet Gynaecol. 2022;42(8):3545–3551. doi: 10.1080/01443615.2022.2153654 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analysed during the current study are not publicly available due to combinations of answers making individuals participating potentially identifiable. However, individual question response data are available from the corresponding author on reasonable request.