Abstract
ABSTRACT
Background
Studies comparing the frequency of different mental health conditions across different settings and evaluating their association with parental participation in newborn care are lacking. We aimed at evaluating the frequency of parental stress, anxiety and depression, along with the level of participation in newborn care, among parents of newborns in Italy, Brazil and Tanzania.
Methods
Parental stress, anxiety, depression and participation in care were assessed prospectively in parents of newborns in eight neonatal intensive care units (NICUs) utilising: the Parental Stressor Scale in NICU (PSS:NICU); the Edinburgh Postnatal Depression Scale (EPDS) and EPDS-Anxiety subscale (EPDS-A); the Index of Parental Participation in NICU (IPP-NICU). Univariate and multivariate analyses were conducted.
Results
Study outcomes were assessed on 742 parents (Brazil=327, Italy=191, Tanzania=224). Observed scores suggested a very high frequency of stress, anxiety and depression, with an overall estimated frequency of any of the mental health condition of 65.1%, 52.9% and 58.0% in Brazil, Italy, Tanzania, respectively (p<0.001). EPDS scores indicating depression (cut-off: ≥13 for Brazil and Tanzania, ≥12 for Italy) were significantly more frequent in Tanzania (52.3%) when compared with either Brazil (35.8%) and Italy (33.3%) (p<0.001). Parental participation in care was also significantly higher in Tanzania (median IPP-NICU=24) than in the other two countries (median=21 for Brazil, 18 for Italy, p<0.001). Severe stress (PSS:NICU ≥4) was significantly more frequently reported in Brazil (22.6%), compared with Italy (4.7%) and Tanzania (0%, p<0.001). Factors independently associated with either parental stress, anxiety or depression varied by country, and a significant association with parental participation in care was lacking.
Conclusions
Study findings suggest that parental stress, anxiety and depression are extremely frequent in NICUs in all countries despite diversity in the setting, and requiring immediate action. Further studies should explore the appropriate level of parental participation in care in different settings.
Keywords: Neonatology
WHAT IS ALREADY KNOWN ON THIS TOPIC
Existing literature highlighted a high frequency of mental distress among parents of infants in neonatal intensive care units (NICUs), but multicountry studies on multiple mental health outcomes and data from low-income settings are lacking.
Parents’ participation in care is a pillar of family-centred care, yet it has been poorly documented in most NICUs.
WHAT THIS STUDY ADDS
This study suggests that parental stress, anxiety and depression are extremely frequent in NICUs, both in high-income and low–middle-income countries, without a direct correlation with parental participation in newborn care.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Immediate action should be taken to screen parents in the NICU for depression, anxiety and stress.
Mechanisms should be put in place to provide rapid access to mental healthcare providers to the parents whose screening for psychological distress was found to be present.
Further studies should define the most appropriate level of parental participation in care in different settings, as well as support systems for parents, in alignment with the principle of family-centred care.
Introduction
Every newborn has the right to survive and thrive, yet each year globally 2.3 million die after birth, additionally 1.9 are stillbirths, and nearly all (98%) of these deaths occur in low and middle-income countries (LMIC).1,3 In addition, several million babies are born either preterm or small for gestational age4 5 or get sick in the first days of life, and among these, it is estimated that about 1 million survive with long-term disabilities.6 Implications of being small and sick often extend beyond the neonatal period.6 Small or sick newborns and their families are at high risk of long-term psychological and financial problems, which in turn can negatively affect their developmental, social and cognitive growth.4,8 Substantial human potential for lifelong health and well-being is lost through newborn mortality and morbidity.5 6
Babies who are preterm or small for gestational age or those with congenital anomalies or postnatal infections are usually hospitalised for a medium to long-term period in neonatal intensive care units (NICU) or semi-intensive care units. Globally, it is estimated that every year up to 30 million newborns require some level of inpatient care.9 Ensuring that all newborns receive the best care in NICU is critical and is recognised as a key aspect of human rights.9 10 Over the last decades, there has been increasing awareness on the importance of quality of care provided in NICU as well as on the stressful nature of the NICU environment, both for infants and for parents.11,14
Specific to the parents’ side, recent evidence suggests that the frequency of distressing symptoms among parents of infants in NICU is very high.11,13 A recent systematic review confirmed a high frequency of parental stress related to NICU admission documented by 53 included studies, independently from timing of hospitalisation or newborn characteristics, and with parental role alteration being the greatest source of stress.11 However, very few studies have been conducted in Asia and South America, and none in Africa.11
Other reviews12 13 looking at a wider range of mental health conditions in parents of newborns in NICU suggested a high frequency of depression and anxiety across diverse ethnocultural groups and countries.12 13 However, several gaps in existing evidence were noted: inconsistency in the use of measurement instruments and timing of measurement; lack of data on fathers; high risk subgroups.12,14 Although in the very recent years, a routine screening of mood and anxiety disorders for parents of newborn in NICU has been proposed by several authors,11,14 yet this is not a reality in most settings, limiting staff awareness on the problem as well as actions to mitigate mental distress in parents of newborn in NICU.
Similarly, although parents’ participation in care has been recognised as one of the core pillars of family-centred care and its benefit for parental and newborn health—including newborn weight gain, breastfeeding rate, decreasing length of stay and parental stress and anxiety—have been documented by several randomised controlled trial (RCTs),15,18 yet in most NICU settings, parental participation in care is not actively promoted nor implemented. Structured programmes, such as the Newborn Individualized Developmental Care and Assessment Program promoting an individualised, relationship-based, family-integrated model of care, by teaching to parents how to interact with their preterm infant19 20 are difficult to access for most professionals, particularly in LMICs. Little is known on the level of parents’ participation in newborn care in many NICU settings, especially in LMICs. Moreover, evidence is lacking on how, in different settings, different levels of participation in care correlates with different levels of mental distress.
This study aimed at documenting the frequency and severity of three mental health conditions—NICU-related stress, depression and anxiety—along with participation in newborn care, among parents of newborns in three different NICU settings: high-income (Italy), upper middle-income (Brazil) and low-income (Tanzania), to identify key differences and communalities. We also explored the association between NICU-related parental stress, depression, anxiety and parental participation to care, when corrected for other variables describing newborns and parental characteristics. This study was conducted within a multicentre project called ‘Empowering Parents in NICU’ (EPINICU), aiming at developing evidence-informed low-cost setting-specific models of interventions to improve mental health and well-being of parents of newborns admitted in NICU, and, where appropriate, improve parental participation in newborn care in NICU, across different settings.
Methods
Study design and setting
This was a multicentre cross-sectional study, and it is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement.21 The STROBE Checklist is provided as online supplemental table 1.
The study was conducted in three countries classified in three different income groups: Italy (high income), Brazil (upper middle income) and Tanzania (lower middle income). Data were collected in hospitals participating to the EPINICU project. The project included only referral and/or teaching hospitals. More details on hospital characteristics are provided in online supplemental table 2.
Study participants
Mother, fathers and other caregivers of newborns who were hospitalised in the NICU or semi-intensive care for at least 24 hours in Brazil and Tanzania (where hospitalisation is usually short) and 48 hours in Italy (where hospitalisation last at least 2 days), with an age of at least 18 years, able to understand the local language (Portuguese in Brazil, Italian in Italy and Swahili in Tanzania) were enrolled prospectively. A priori exclusion criteria were parents with previously diagnosed mental disorders or cognitive difficulties which hampered data collection; parents of newborns dead at birth or during hospitalisation or which were hospitalised for less than 24 hours; maternal deaths; parents aged less than 18 years; parents not fluent in the languages in which the questionnaire was provided (fluency was assessed by the clinicians in charge); parents not providing consent to the study.
Study outcomes and data collection tools
We predefined as key outcomes for this study: (1) parental NICU-related stress (our primary outcome); (2) parental depression; (3) parental state and trait anxiety; (4) parental participation in newborns care. In order to collect these outcomes, we seek to select the most appropriate questionnaires, that is, those more widely validated and used, and feasible in our contexts (table 1). Newborns’ and parents’ characteristics were also collected.
Table 1. Key characteristics of questionnaire used for data collection.
| Outcome | Questionnaire | Number of domains and questions | Recall period | Score range | Cut-offs recommended in literature |
| Stress | Parental Stressor Scale for NICU (PSS:NICU) | 26 questions in three domains
|
Not specified | 1–5 for each question(total: 1–5) | No recommendation in literature |
| Depression | Edinburgh Postnatal Depression Scale (EPDS) | 10 questions | Last 7 days | 0–3 for each question(total: 0–30) | For diagnosis of depression:≥ 12 Italy≥ 13 Brazil and Tanzania22,33 |
| Anxiety | EPDS-Anxiety subscale (EPDS-A) | 3 questions | Last 7 days | 0 to 3 for each question(total: 0–9) | For diagnosis of anxiety:≥ 634 |
| State anxiety | State Anxiety Inventory (STAI Y1) | 20 questions | In the last 24/48 hour | 1–4 for each question(total 20–80) | For diagnosis of anxiety: >40Anxiety level41–50: mild anxiety51–60: moderate anxiety>60: severe anxiety35,46 |
| Traitanxiety | Trait Anxiety Inventory (STAI Y2) | 20 questions | Not specified (describe how you generally feel) | 1–4 for each question(total 20–80) | For diagnosis of anxiety: >40Anxiety level41–50: mild anxiety51–60: moderate anxiety>60: severe anxiety35,46 |
| Participation to care | Index of Parental Participation (IPP-NICU) | 30 questions in four domains
|
Previous 24 hours | 0–1 (yes or no) for each question(total 0–30, different maximum scores for each subdomain) | No recommendation in literature |
Stress was measured with the Parental Stressor Scale for NICU (PSS:NICU),22 which is a scale specific to parental stress related to NICU. The scale has been properly validated in Italy23 and Brazil.24 Studies on the PSS:NICU are lacking from Africa,11 therefore for use in our project in Tanzania the PSS:NICU questionnaire was translated and back translated in Swahili by expert mother tongue researchers, according to The Professional Society for Health Economics and Outcomes Research (ISPOR) guidelines.25 PSS:NICU includes 26 statements divided in three sections: stress due to ‘Sights and Sounds’ (6 items), to ‘Infant Behaviour and Appearance’ (13 items) and to ‘Parental Role Alteration’ (7 items). In PSS:NICU, questions do not refer to a specific time period. Answers for each question are on a Likert scale from 1 point for ‘not at all stressful’, 2 points for ‘mild stress’, 3 points for ‘fairly moderate stress’, 4 points for ‘very stressful’ and 5 points for ‘extreme/severe stress’. Total PSS:NICU scores are calculated according to author instructions,22 using two methods: (a) the stress occurrence level (SOL) is calculated including only experienced items; (b) the overall stress level (OSL) is calculated scoring ‘not applicable items’ with one point. According to the author’s instructions, SOL should be used when the focus is the parent as it captures better their experience, while OSL when the focus on the NICU environment.22
Parental depression was measured with the Edinburgh Postnatal Depression Scale (EPDS), which is the most widely used instrument for screening postnatal depression. It has been validated in many countries, including in Italy in mothers and fathers,24 26 and in Brazil24 27; it has been translated in Swahili28 and used in several African countries, including Tanzania.28,31 The scale includes 10 questions, which evaluate the emotional state of the last 7 days, with four possible answers each (points ranging from 0 to 3), and a total score ranging from 0 to 30. The cut-off values considered more accurate for the diagnosis of depression are: a value ≥12 both for women and men in Italy,24 26 and a cut-off ≥13 in Brazil24 27 and Tanzania,28,32 although other studies from Africa33 used a lower cut-off (≥12).
Anxiety was measured, as primary analysis, by considering the EPDS-Anxiety subscale (EPDS-A), which allows individuals with high anxiety symptoms to be identified through a subset of EPDS items.34 The EPDSA-A final score can range from 0 to 9 and a score ≥6 has proved to detected women with symptoms for at least one anxiety disorder, including generalised anxiety disorder, panic disorder or obsessive-compulsive disorder. As secondary additional analysis, in Italy and Brazil, anxiety was also measured by the State-Trait Anxiety Inventory (STAI), which include two complementary subscales: (1) the State Anxiety Scale (STAI State) evaluates the current state of anxiety, asking how respondents feel ‘right now’, using 20 items each with a scale from 1 (not symptoms) to 4 (very much so); (2) the Trait Anxiety Scale (STAI Trait) evaluates ‘anxiety proneness’, by assesses frequency of feelings ‘in general’, including general states of calmness, confidence and security.35 The Trait Anxiety Scale has been suggested to capture not exclusively trait anxiety but rather a higher order trait such as negative affectivity/neuroticism that characterises both anxiety and depression.36 37 The STAI has been validated in Italy,29,39 Brazil40 41 and widely used in Africa.42 43 Each scale includes 20 items with a score ranging from 1 (almost never) to 4 (almost always), thus for each scale, the total score can range from 20 to 80. Although slightly different cut-offs for STAI have been used in the literature, in general, scores over 40 are considered indicative of anxiety, scores in between 41 and 50 indicating mild anxiety, 51–60 moderate anxiety and>60 severe anxiety.44,46
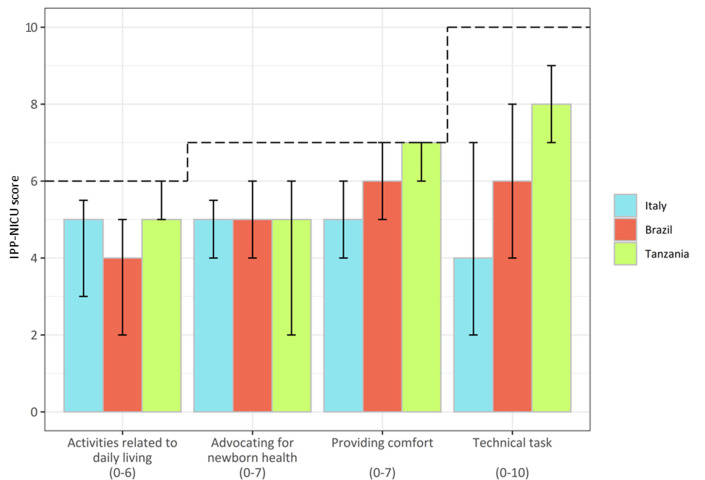
Parental participation was measured with the Index of Parental Participation (IPP) to paediatric care,47 which was previously used in context with low resources.48 For use in the NICU setting, the IPP was adapted by a team of senior neonatologists and epidemiologists. This adapted version of the IPP (IPP-NICU) was approved by Dr Melnik, the author of the original instrument.47 The IPP-NICU questionnaire was translated and back translated for use in the project in Brazil and Tanzania, following the ISPOR guidelines.25 The IPP-NICU includes four subdomains: activities related to Daily Living (6 items); Providing Comfort (7 items); Advocating for newborn health (7 items); Technical Tasks (10 items). Questions refer to the previous 24 hours. The total number of items is 30, with a dichotomous (yes/no) answering. The total score ranges from 0 to 30, with different maximum scores for each subdomain, and higher scores indicating higher parental participation in care.
A structured form, developed in dialogue with partners and field tested before use, was used to collect key newborns and parental characteristics, according to predefined case definitions. Data from parents were collected with a structured questionnaire among parents, data on newborns were collected from medical records and from parents.
Data collection procedures
The study and above-described questionnaires were introduced to parents by trained health professionals, either a neonatologist or other NICU staff close to discharge from NICU. The questionnaires were self-administered in Italy and Brazil. In Tanzania, due to the high rate of maternal illiteracy, data were collected with an oral interview, carried forward by ad hoc trained researcher not involved in case management or in data analysis. To reduce the burden of data collection, STAI questionnaires were not performed in Tanzania and performed in a subsample of parents in the other two countries. In Brazil depression, parental state and trait anxiety and participation in care were assessed only in one facility (Instituto de Medicina Integral Professor Fernando Figueira - IMIP), while in the other five hospitals only data on stress were prioritised.
Data collection periods slightly varied due to administrative procedures (project contracts and ethical clearance), and the different impact of the COVID-19 on research activities, and specifically were in Italy from November 2019 to November 2020 (with a gap of 2 months in March and April 2020, due to COVID-19 restrictions); in Tanzania from December 2019 to August 2020; in Brazil from May 2020 to December 2021.
Data analysis
A sample of 166 parents was needed for each country based on an estimated prevalence of stress in parents of newborns in NICU of 50%±10%, based on the existing literature,11,13 with a confidence level of 99%.
First, we conducted a descriptive analysis, identifying key similarities and key differences across countries. Summary statistics were presented as absolute frequencies and percentages, and as medians and IQRs for continuous non-normally distributed data. Frequency of parental stress, anxiety and depression were assessed using the following cut-offs recommended by the literature (table 1): for EPDS, we assessed prevalence of parents with a score ≥13 in Brazil and Tanzania, and ≥12 in Italy2426,32; for EPDS-A, we used a cut-off ≥634; for the State-Trait STAI, we assessed prevalence of parents with a score cut-off >40.44,46 For the PSS:NICU, in absence of any indication in literature, we assessed prevalence of parents with a score ≥3, which identify ‘fairly moderate stress’. Anxiety was primarily assessed with EPDS-A, while STAI was used as additional score system in Brazil and Italy, and to assess severity of anxiety. Severe stress and severe anxiety were respectively calculated by considering the frequencies of parents with SOL score ≥4 and STAI state score >60.44,46 For calculating frequencies of all conditions, we used as a sample the subgroup of parents for whom all the scores of interests were available. To analyse intersections between groups of parents identified with different conditions, the SOL score was used for stress, as for existing recommendations.22
Additionally, we conducted univariate and multivariate logistic regression models for each country, considering the presence of mental health conditions under analysis (ie, depression, stress, anxiety, any of them) as binary outcome variables and parental participation to care as well as parental (ie, age, marital status, residence, financial situation, working status, role, education, participation to care) and newborn characteristics (gestational age, weight at birth, malformation, surgery, intubation, COVID-19, length of stay, unit of stay) as explanatory variables. For these analyses, we used the same cut-off descripted above for the mental health conditions, while we categorised the independent continuous variables according to their overall distribution in each country. The SOL score was used for stress, as for existing recommendations.22 Frequencies, ORs and adjusted ORs (adjOR) were calculated, with 95% CIs and p values of significance.
To assess differences between two values, we employed the two proportions, z test (for proportions) and the Mood’s median test (for medians). When comparing three proportions, we conducted multiple comparisons using the z test. For three or more medians, we used the Asymptotic K-sample Brown-Mood median test. All the tests were two tailed. Statistical analyses were performed using Stata V.14 and R V.4.1.2. For all tests performed, a p value of less than 0.05 was considered statistically significant.
Patient and public involvement in research
Patients were involved as responders of the questionnaire of data collection. In each of the countries, patients are being involved in designing actions on how to improve care in NICUs, based on the results of this study.
Results
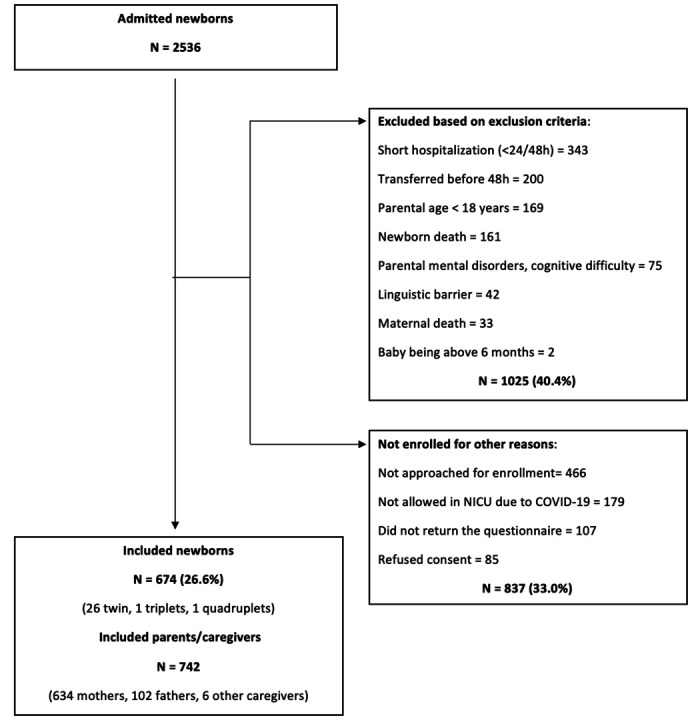
Population characteristics
Of the 2536 newborns admitted to the eight NICUs during the study period, 1511 (59.6%) meet the inclusion criteria. Among these, 837 (55.4%) were not enrolled due to several reasons related to their parents, including COVID-19, while only a minority (5.6%) refused consent (figure 1). Overall, we included 674 newborns and 742 parents/caregivers (Brazil=327, Italy=191, Tanzania=224). Fathers were mostly represented in the Italian sample (19, 79 and 4 fathers in Brazil, Italy and Tanzania, respectively).
Figure 1. Study flow diagram. NICU, neonatal intensive care unit.
Both parental (online supplemental table 3) and newborn (online supplemental table 4) characteristics significantly differed among the three countries.
Differences among parents included caregiver age, working status, marital status, educational level (all p values <0.001) and women parity (p=0.003).
Most of newborns’ characteristics, such as Apgar score at 5th minute and frequency of associated medical conditions and related treatments (ie, surgery, ventilation support at birth), were significantly different across countries (p values <0.05). Out of the total sample, 400 (59.3%) newborns were preterm (gestational age at birth <37 weeks), with a higher frequency in Brazil (78.6%) and Italy (61.7%) when compared with Tanzania (29.9%, p<0.001). The median length of stay in NICU for Brazil (29 days) was significantly higher than the one recorded in Italy (14 days, p<0.001) and Tanzania (7 days, p<0.001).
Detected frequency of stress, depression and anxiety
Key similarities across countries:
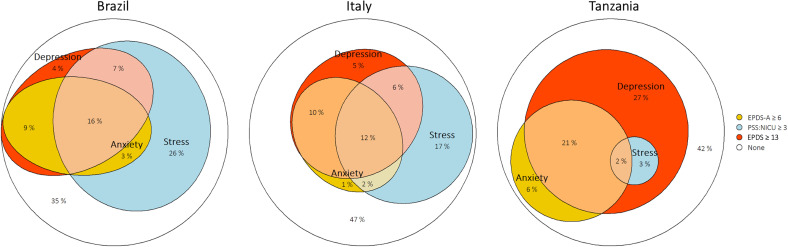
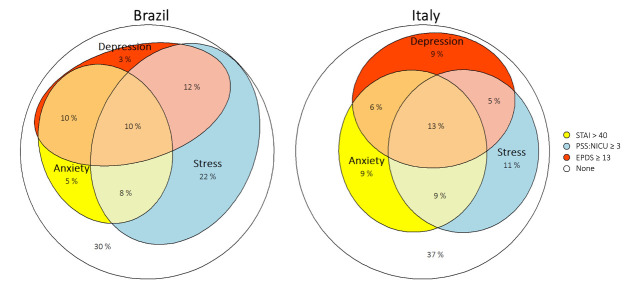
The detected frequencies of depression, anxiety and stress—calculated based on the pre-defined cut-off for each indicators—were high in all facilities (figure 2, online supplemental table 5A), with an overall frequency of any of the conditions of 65.1%, 52.9% and 58.0% in Brazil, Italy, Tanzania, respectively (all p values of multiple comparisons >0.05, in particular: Brazil vs Italy=0.06, Italy vs Tanzania=0.34, Brazil vs Tanzania=0.27). Results calculated using STAI were quite similar: 69.8% in Brazil and 63.1% in Italy (online supplemental table 5B, figure 3).
Figure 2. Frequency of detected parental depression, anxiety, stress and intersections among identified populations. For anxiety, the EPDS-A score was used. For PSS:NICU, the SOL score was used. Depression cut-offs: EPDS≥12 for Italy and≥13 for Brazil and Tanzania. EPDS, Edinburgh Postnatal Depression Scale; NICU, neonatal intensive care unit; PSS:NICU, Parental Stressor Scale in NICU; SOL, stress occurrence level.
Figure 3. Frequency of parental depression, anxiety (STAI score) and stress and intersections among identified populations. For PSS:NICU, the SOL score was used. For STAI, the STAI State score was used. Depression cut-offs: EPDS≥12 for Italy and≥13 for Brazil. In Tanzania, the STAI score was not collected. EPDS, Edinburgh Postnatal Depression Scale; NICU, neonatal intensive care unit; PSS:NICU, Parental Stressor Scale in NICU; SOL, stress occurrence level; STAI, State-Trait Anxiety Inventory.
Key differences across countries:
EPDS scores suggestive of depression were significantly more frequent in Tanzania (52.3%) when compared with both Brazil (35.8%) and Italy (33.3%)—(both p values <0.001).
The three countries had different patterns of intersections across populations identified with different conditions (figure 2, online supplemental table 6.
The frequency of all three conditions simultaneously was higher in Brazil (16.0%) and Italy (11.5%) compared with Tanzania (1.8%) (both p values for one-sided comparisons <0.001). Results calculated using STAI were quite similar: 10.4% in Brazile and 13.1% in Italy (online supplemental table 5A,B, figure 3).
Severity of stress, depression and anxiety
Key similarities across countries:
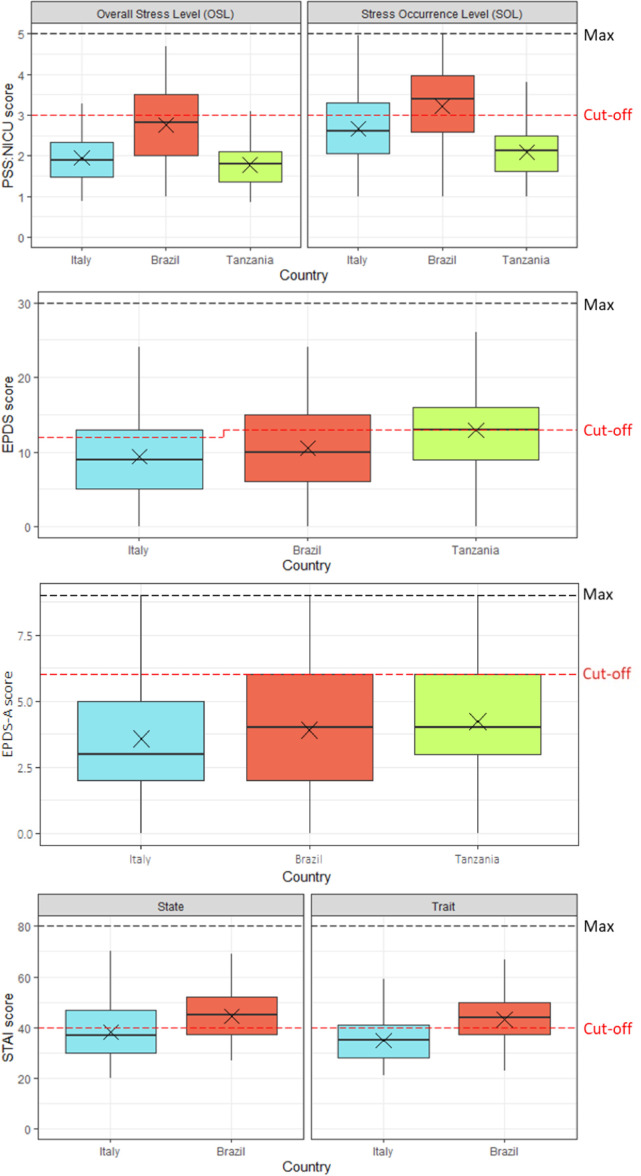
In all countries, the scores of stress, depression and anxiety had a wide variability (figure 4) and reached values near to the maximum: the EPDS maximum score was 24 in Italy and 26 in Brazil and Tanzania; the PSS:NICU SOL maximum score was 5 in Italy and 4 in Brazil and Tanzania; EPDS-A reached the maximum value (score of 9) in each country, while STAI state maximum score was 70 in Italy and 69 in Brazil.
Severe anxiety (defined as STAI State >60) had similar frequencies in Brazil (5%) and Italy (4%), p value=0.998 (online supplemental table 6B).
Figure 4. Severity of stress, depression and anxiety (median scores). The figure shows the median, the mean (represented by a ‘X’) and the IQR of each score. EPDS, Edinburgh Postnatal Depression Scale; NICU, neonatal intensive care unit; PSS:NICU, Parental Stressor Scale in NICU; STAI, State-Trait Anxiety Inventory.
Key differences across countries:
Parents in Tanzania had significantly higher median scores for depression (EPDS median equal to 13, IQR[9;16]) when compared with other countries (p value <0.001) (figure 4).
Parents in Brazil had higher median scores for anxiety and stress (STAI state median equal to 45 and SOL median equal to 3.4) than the other countries under analysis (p value=0.002 for STAI state, p value <0.001 for SOL); frequency of severe stress (PSS:NICU—SOL≥4) was also significantly higher in Brazil (22.6%) compared with Italy (4.69%, p value <0.001) and Tanzania (0%, p value <0.001) (figure 4, online supplemental tables 6B and 7).
Stress scores by domains
Key similarities across countries:
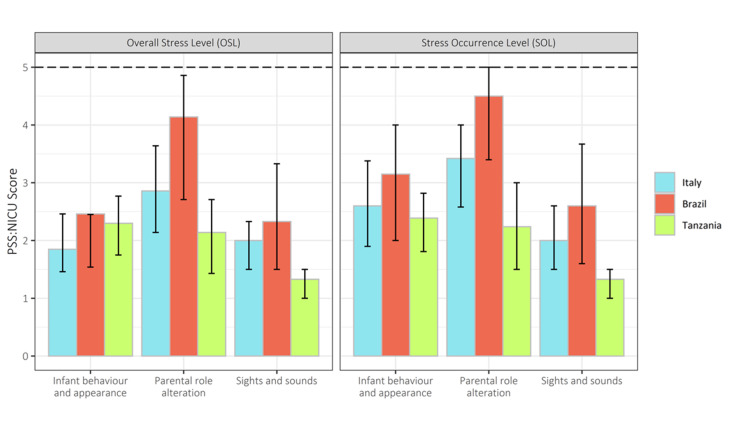
Among the different domains of the PSS Score, ‘Sights and sounds’ was the one perceived as least stressful, when compared with the other domains, in all three countries under analysis (figure 5).
Figure 5. Stress by domain (median scores). The figure shows the median and the IQR of the PSS:NICU. NICU, neonatal intensive care unit; PSS:NICU, Parental Stressor Scale in NICU.
Key differences across countries:
For both Italian and Brazilian parents, the domains where the higher scores of parental stress were reported was the paternal role alteration (SOL median 3.4 for Italy and 4.5 for Brazil), while for Tanzanian parents, it was the infant behaviour and appearance (SOL median 2.38) (figure 5).
Parental participation in care
Key similarities across countries:
In no country parental participation in care score reached its possible maximum value, with the largest gap in all countries being on ‘technical tasks’ (figure 6).
Figure 6. Parental participation, by domain (median scores). The figure shows the median and the IQR of the IPP-NICU. NICU, neonatal intensive care unit; IPP-NICU, Index of Parental Participation in NICU.
Key differences across countries:
In general, Tanzanian parents had the highest participation scores (median IPP-NICU score equal to 24, IQR [21; 26]), even in the domain of technical task (median 8 out of 10, IQR [7; 9] vs Brazil (median 6, IQR [4;8]) and Italy (median 4, IQR [2;7])—p value <0.001). Italian parents reported the lowest scores (median IPP-NICU score equal to 18, IQR [12; 22]). In Brazil, there was a medium–high level of participation (median 21, IQR [15; 24.8]) (figure 6, online supplemental table 8).
Multivariate analyses
Results of multivariate analyses varied by country, with, in general, few factors significantly associated with mental health outcomes, when corrected for all other factors.
In Italy, (online supplemental tables 9–11), stress significantly negatively associated with being a parent of twin newborns (adjOR 0.24, 95% CI 0.06 to 0.71, p value=0.018), while both depression and anxiety significantly associated with being a mother (adjOR 2.93, 95% CI 1.35 to 6.65, p value=0.008; adjOR 3.03, 95% CI 1.27 to 7.83, p value=0.016).
In Brazil (online supplemental tables 12–14), mothers from the interior/rural area had significantly lower odds for stress than those from the city (adjOR 0.33, 95% CI 0.13 to 0.84, p value=0.023); all other variables had non-significant associations with any of the mental health outcomes of interest, when corrected for the other variables.
In Tanzania (online supplemental tables 15–17), parental age higher than 25 years old associated with higher odds of parental anxiety (adjOR 2.04, 95% CI 1.04 to 4.09, p value=0.040), while being the parent of a newborns with length of stay higher than 7 days associated with lower odds of parental anxiety (adjOR 0.43, 95% CI 0.21 to 0.84, p value=0.016); all other variables had non-significant associations with any of the mental health outcomes of interest, when corrected for the other variables.
Discussion
This study detected as a key communality across Italy, Brazil and Tanzania a very high frequency in of NICU-related stress, depression and anxiety, without a direct correlation with parental participation in newborn care. Key differences included a higher frequency of maternal depression in Tanzania, and stress in Brazil. Previously existing studies did not directly compare three major outcomes related to mental health—NICU-related stress, depression and anxiety (both state and trait)—along with participation in newborn care, and in this sense, this study is filling a research gap.
Study findings strongly support previous recommendations11,1449 50 on the need of routine screening for mood, anxiety disorders and stress in parents of newborn in NICU. The feasibility of screening for mood and anxiety disorder has been positively evaluated by a recent systematic review.51 Common facilitators included engaging multidisciplinary staff in programme development and implementation, partnering with experienced facilities (champions), and incorporating parents screening into routine newborn clinical practice, while constraint in accessing mental health support was the most significant barrier.51
Prevention and support/treatment to parents with mental distress can be provided not only through psychological and social services but also through many other innovative ways. Existing systematic reviews of interventions to reduce parental depressive and anxiety symptoms identified many effective interventions, including, beside cognitive behavioural therapy52: educational interventions on a wide range of topics such as newborn attachment, newborn growth and development, NICU environment, how to manipulate and nurture the baby, how to observe infant’s behaviours and provide positive stimulation and relaxation, newborn home care, training on problemsolving strategies, and on how to deal with own emotions, plus information on existing related resources52,54; parent’s-centred support communication54; parents’ groups53; fathers involvement in care53; parents dairy to process emotions and experiences53; music53; emotional support54; relaxation techniques (breathing, muscle relaxation, guided imagery)53 54; massage53; environmental interventions such as family rooms,54 noise reduction,52 bright light therapy.52
Such interventions clearly require involvement of NICU staff, including nurses, as highlighted by a recent systematic review.53 Therefore, as a first step, there is the need to increase staff awareness—which cannot be given for granted—on the very high frequency of mental distress among parents of newborns in NICU. Second, based on the observed prevalence of mental distress among parents of newborn in NICU, related competences should be incorporated in the core curriculum of all NICU key staff. Evidence suggests that gaps in communication are one of the key areas reported by mothers as substandard55 56; therefore, competences to effectively establish, on a routine basis, effective communication and a collaborative relationship between staff and parents, even those with severe mental distress, appear to be one of the key core competencies needed for staff working in NICU. All these changes require a culture of family-centred developmental care, where both family and staff needs are considered comprehensively (including psychological needs), in a proactive manner (taking action).
Study findings, with Tanzanian mothers compared with Italian and Brazilian parents reporting higher frequency of depression, despite higher participation to newborn care, are not in contradiction with existing RCTs, summarised by a recent systematic review,15 showing the many benefits of participation to care, including a reduction in maternal mental health distress and depression.15 Postpartum depression, as shown by a recent metanalysis,57 is frequent in African mothers and it is associated with a wide range of risk factors, which our study did not aim at exploring—such as poor obstetric condition, history of adverse birth and infant health outcomes, a previous history of mental health disorders, low economic status, poor social support and intimate partner violence. Higher participation in care in Tanzania may be explained by staff shortage. Plausibly, when participation in care is promoted in the right environment and through parents’ empowerment, it brings a benefit, while when mothers are left alone with their children without support, it may be not associated with good mental outcomes. The most appropriate level of parental participation in newborn care in different settings has not been established yet. We believe that such an evaluation should take into consideration, beside the context readiness (eg, existing resources, risk of infection, etc), both views of parents and staff, their level of empowerment, their cultural expectations and the existence of other existing support systems (eg, staff and parental training, policies.
Findings of the multivariate analyses suggest that risk factors for different mental health conditions may differ significantly across countries and settings, and calls for more in-depth studies. Other results of the multivariate analyses, such as the finding of stress negatively associated with twin birth or longer duration of stay, contradicts previous research and will need to be further confirmed.
We acknowledge limitations of this study. First, the observational nature of the study did not aim at testing any causal relationships among different study variables. In the lack of other previous multicountry assessments, this study was conceived as descriptive. However, it had the merit of documenting key mental health conditions together with participation in care, allowing comparison across countries, and providing data critical to develop context-specific interventions, as expected for the subsequent phases of the EPINICU project. Subgroup analyses looking at differences in study outcomes by sex of parents have been reported elsewhere.58
Second, data collection, occurring mostly during the COVID-19 pandemic, may have overestimated the frequency of mental distress, and slightly different time periods of data collection across the three countries may have affected results. However, detected frequency of stress, anxiety and depression aligns with those reported in studies in the prepandemic period,11,13 while the COVID-19 diseases per se mostly cause mild disease in children.59 An analysis of the Italian dataset across different time periods (prepandemic, low and high COVID-19 incidence) showed that prevalence of stress, anxiety and depression did not change significantly over time.60 Future studies shall document to which extent parental mental distress in NICU persists beyond COVID-19.
Third, this study was conducted in one single referral facility per country, except for Brazil. More studies (or even better, data from screening programmes) should aim at documenting the prevalence of parental mental distress in different settings.
Fourth, while previous studies suggested that the severity of parental mental distress may change during the course of hospitalisation,61 our study did not aim at documenting how such changes occurred. More evidence on this topic shall be derived from a desirable routine practice of screening mental distress in parents of newborn in NICU.
Fifth, the exclusion of parents with previously diagnosed mental health condition may have underestimated the frequency of our outcomes. Oral interview data collection procedure in Tanzania may reduce comparability of the results and biased results.
Finally, the questionnaire used may have their intrinsic limitations: they collect data that are based on a self-assessment and on different time periods (table 1); cultural appropriateness of EPDS in Africa is still debated32 and the same may apply to the concept of stress; IPP-NICU questionnaire does not capture parental satisfaction with participation to newborn care. With these limitations, the questionnaires used in this study are the most widely validated and used in literature.22,43
Conclusion
This study suggests that parental stress, anxiety and depression can be extremely frequent in NICUs, both in high-income and low–middle-income countries, without a direct correlation with parental participation in newborn care. Immediate action should be taken to screen parents in the NICU for depression, anxiety and stress, and to refer them to appropriate care. Further studies should define the most appropriate level of parental participation in care in different settings, as well as support systems for parents, in alignment with the principle of family-centred care.
supplementary material
Acknowledgements
We would like to thank all collaborators to the EPINICU Study Group; for Italy: Prof Egidio Barbi, Dr Stefano Bembich, Dr. Livia Bicego, Dr Emily Esposito, Dr. Silvia Nider; for Tanzania: Dr Giovanni Putoto, Dr Giovanni Torelli,; for Brazil: Dr Giselle Paiva, Dr Walkyria Campos, Dr Vivian Farias, Dr Lorena Freitas, Renata Araújo, Núbia Dantas, Maria Eduarda Fraga; for Sri Lanka: Dr Mohamed Rishard, Dr Hemantha Senanayake, Nalin Gamaathige. We thank all parents who took their time to respond to this survey despite the burden of COVID-19 pandemic. We thank Bernadette Mazurek Melnyk, PhD, APRN-CNP, FAANP, FNAP, FAAN for the authorised modified version of IPP/HC-AA in the NICU setting (Adapted from Dr. Melnyk’s instrument). We thank Dr. Margaret S. Miles for the authorised Italian version (PSS: NICU version 3.0 (19/01/06)) edited by R. Montirosso and B. Premoli (IRCCS 'E.Medea'—Associazione 'La Nostra Famiglia', Bosisio Parini (LC), Italia). We thank Dr. Martina Girardelli for the quality check of the Italian EPDS data.
Footnotes
Funding: The study was supported by 'Chiesi Foundation research grant 2019 in Neonatology' (prot. IRCCS n. 8142/2019—Registro Contratti n.1091) to our Institute of Research. As per the contract undersigned among parties, 'The Grant does not constitute, directly or indirectly, a fee for services provided or to be provided in favour of the Foundation'. This work was supported by the Italian Ministry of Health, through the contribution given to the Institute for Maternal and Child Health IRCCS Burlo Garofolo, Trieste—Italy.
Provenance and peer review: Not commissioned; externally peer-reviewed.
Patient consent for publication: Not applicable.
Ethics approval: The study was approved by the relevant ethical committees in all countries. Specifically, in Italy, it was approved by the Institutional Review Board of Friuli Venezia Giulia Region (Prot.31633, 22 October 2019. In Tanzania, by the National Institute for Medical Research (Reference Number NIMR/HQ/R.8a/Vol.IX/3295). In Brazil, by the 'Comissão Nacional de Ética em Pesquisa' (National Research Ethics Committee) (Number: 3.931.201, CAAE: 17362919.0.0000.5201, 24/03/2020), Fundação Universidade de Pernambuco (Number: 3.847.757, CAAE 27526919.6.0000.5192, 19/02/2020), Centro Integrado de Saúde Amaury de Medeiros (3.889.399 CAAE 27526919.6.3001.5191 28/02/2020), Empresa Brasileira de Servicos Hospitalares – (Hospital das Clínicas da Universidade Federal De Pernambuco - (Number: 3.905.586 CAAE: 27526919.6.3004.8807, 09/03/2020), Instituto de Medicina Integral Professor Fernando Figueira (Number: 3.910.660 CAAE: 27526919.6.3003.5201, 11/03/2020), and Hospital Agamenon Magalhães (Number: 3.949.213, CAAE 27526919.6.3002.5197, 01/04/2020). The research was conducted in accordance with the World Medical Association Declaration of Helsinki. Participants were informed on the objectives and methods of the study, including their rights in declining participation, and provided consent before responding to questionnaires. Anonymity in data collection was ensured by not collecting information that could disclose participants’ identity. Participants gave informed consent to participate in the study before taking part.
Collaborators: EPINICU Study Group; for Italy: Prof Egidio Barbi, Dr Stefano Bembich, Dr. Livia Bicego, Dr Emily Esposito, Dr. Silvia Nider; for Tanzania: Dr Giovanni Putoto, Dr Giovanni Torelli; for Brazil: Dr Giselle Paiva, Dr Walkyria Campos, Dr Vivian Farias, Dr Lorena Freitas, Renata Araújo, Núbia Dantas, Maria Eduarda Fraga; for Sri Lanka: Dr Mohamed Rishard, Dr Hemantha Senanayake, Nalin Gamaathige.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Marzia Lazzerini, Email: marzia.lazzerini@burlo.trieste.it.
Dafne Barcala Coutinho do Amaral Gomez, Email: dafnebarcala@hotmail.com.
Gaetano Azzimonti, Email: g.azzimonti@cuamm.org.
Jenny Bua, Email: jenny.bua@burlo.trieste.it.
Waldemar Brandão Neto, Email: waldemar.neto@upe.br.
Luca Brasili, Email: l.brasili@cuamm.org.
Laura Travan, Email: laura.travan@burlo.trieste.it.
Juliana Barradas de Souza, Email: julibarradas@hotmail.com.
Michele D'Alessandro, Email: mdalessandro@cuamm.org.
Sabrina Plet, Email: sabrina.plet@burlo.trieste.it.
Geisy Maria de Souza Lima, Email: canguru@imip.org.br.
Emmanuel Abraham Ndile, Email: emmanuelndile@gmail.com.
Maddalena Ermacora, Email: maddalena.ermacora@burlo.trieste.it.
Emanuelle Pessa Valente, Email: emanuelle.pessavalente@burlo.trieste.it.
Paolo Dalena, Email: paolo.dalena@burlo.trieste.it.
Ilaria Mariani, Email: ilaria.mariani@burlo.trieste.it.
on behalf of the EPINICU study group:
Egidio Barbi, Stefano Bembich, Livia Bicego, Emily Esposito, Silvia Nider, Giovanni Putoto, Giovanni Torelli, Giselle Paiva, Walkyria Campos, Vivian Farias, Lorena Freitas, Renata Araújo, Núbia Dantas, Maria Eduarda Fraga, Mohamed Rishard, Hemantha Senanayake, and Nalin Gamaathige
Data availability statement
Data are available upon reasonable request.
References
- 1.UNICEF. World Health Organization. World Bank Group . New York: United Nations Children’s Fund; 2022. [05-Dec-2022]. Levels & trends in child mortality 2022.https://data.unicef.org/resources/levels-and-trends-in-child-mortality/ Available. accessed. [Google Scholar]
- 2.United Nations Inter-agency Group for Child Mortality Estimation (UN IGME) New York: 2023. Never forgotten: the situation of Stillbirth around the globe, United Nations children’s Fund. [Google Scholar]
- 3.Hug L, Alexander M, You D, et al. National, regional, and global levels and trends in neonatal mortality between 1990 and 2017, with scenario-based projections to 2030: a systematic analysis. Lancet Glob Health. 2019;7:e710–20. doi: 10.1016/S2214-109X(19)30163-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blencowe H, Krasevec J, de Onis M, et al. National, regional, and worldwide estimates of low birthweight in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health. 2019;7:e849–60. doi: 10.1016/S2214-109X(18)30565-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee ACC, Katz J, Blencowe H, et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob Health. 2013;1:e26–36. doi: 10.1016/S2214-109X(13)70006-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lawn JE, Blencowe H, Oza S, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet. 2014;384:189–205. doi: 10.1016/S0140-6736(14)60496-7. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization . Geneva:: World Health Organization; 2012. Born too soon: the global action report on preterm birth. born too soon: the global action report on preterm birth. [Google Scholar]
- 8.Moxon SG, Lawn JE, Dickson KE, et al. Inpatient care of small and sick newborns: a multi-country analysis of health system bottlenecks and potential solutions. BMC Pregnancy Childbirth. 2015;15 Suppl 2:S7. doi: 10.1186/1471-2393-15-S2-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization Survive and thrive transforming care for every small and sick newborn. 2019. [25-Jan-2021]. https://apps.who.int/iris/bitstream/handle/10665/326495/9789241515887-eng.pdf Available. Accessed.
- 10.United Nations Convention on the Rights of the Child Adopted and opened for signature, ratification and accession by general assembly resolution 44/25 of 20 november 1989; entry into force 2 september 1990, in accordance with article 49. [17-Feb-2022]. https://www.ohchr.org/en/professionalinterest/pages/crc.aspx Available. Accessed.
- 11.Caporali C, Pisoni C, Gasparini L, et al. A global perspective on parental stress in the neonatal intensive care unit: a meta-analytic study. J Perinatol. 2020;40:1739–52. doi: 10.1038/s41372-020-00798-6. [DOI] [PubMed] [Google Scholar]
- 12.Staver MA, Moore TA, Hanna KM. An integrative review of maternal distress during neonatal intensive care hospitalization. Arch Womens Ment Health. 2021;24:217–29. doi: 10.1007/s00737-020-01063-7. [DOI] [PubMed] [Google Scholar]
- 13.Roque ATF, Lasiuk GC, Radünz V, et al. Scoping review of the mental health of parents of infants in the NICU. J Obstet Gynecol Neonatal Nurs. 2017;46:576–87. doi: 10.1016/j.jogn.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 14.Baldoni F, Ancora G, Latour JM. Being the father of a preterm-born child: contemporary research and recommendations for NICU staff. Front Pediatr. 2021;9:724992. doi: 10.3389/fped.2021.724992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.North K, Whelan R, Folger LV, et al. Family involvement in the routine care of hospitalized preterm or low birth weight infants: a systematic review and meta-analysis. Pediatrics. 2022;150:e2022057092O. doi: 10.1542/peds.2022-057092O. [DOI] [PubMed] [Google Scholar]
- 16.Gooding JS, Cooper LG, Blaine AI, et al. Family support and family-centered care in the neonatal intensive care unit: origins, advances, impact. Semin Perinatol. 2011;35:20–8. doi: 10.1053/j.semperi.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Committee on Hospital Care and Institute for Patient- and Family-Centered Care Patient- and family-centered care and the pediatrician’s role. Pediatrics. 2012;129:394–404. doi: 10.1542/peds.2011-3084. [DOI] [PubMed] [Google Scholar]
- 18.Harrison H. The principles for family-centered neonatal care. Pediatrics. 1993;92:643–50. [PubMed] [Google Scholar]
- 19.NIDCAP «Endorsements». [16-May-2024]. https://nidcap.org/the-nfi/endorsements Available. Accessed.
- 20.The COPE (Creating Opportunities for Parent Empowerment) NICU program. [16-May-2024]. http://www.copeforhope.com/nicu.php Available. Accessed.
- 21.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–8. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miles MS, Funk SG, Carlson J. Parental stressors scale: neonatal intensive care unit. Nurs Res. 1993;42:148–52. doi: 10.1097/00006199-199305000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Montirosso R, Provenzi L, Calciolari G, et al. Measuring maternal stress and perceived support in 25 Italian NICUs. Acta Paediatr. 2012;101:136–42. doi: 10.1111/j.1651-2227.2011.02440.x. [DOI] [PubMed] [Google Scholar]
- 24.Souza SR, Dupas G, Balieiro MMFG. Cultural adaptation and validation for the Portuguese language of the parental stress scale: neonatal intensive care unit (PSS:NICU) Acta Paul Enferm. 2012;25:171–6. doi: 10.1590/S0103-21002012000200003. [DOI] [Google Scholar]
- 25.Wild D, Grove A, Martin M, et al. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR task force for translation and cultural adaptation. Value Health. 2005;8:94–104. doi: 10.1111/j.1524-4733.2005.04054.x. [DOI] [PubMed] [Google Scholar]
- 26.Loscalzo Y, Giannini M, Contena B, et al. The Edinburgh postnatal depression scale for fathers: a contribution to the validation for an Italian sample. Gen Hosp Psychiatry. 2015;37:251–6. doi: 10.1016/j.genhosppsych.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 27.Santos IS, Matijasevich A, Tavares BF, et al. Validation of the Edinburgh postnatal depression scale (EPDS) in a sample of mothers from the 2004 Pelotas birth cohort study. Cad Saude Publica. 2007;23:2577–88. doi: 10.1590/s0102-311x2007001100005. [DOI] [PubMed] [Google Scholar]
- 28.Kumar M, Ongeri L, Mathai M, et al. Translation of EPDS questionnaire into Kiswahili: understanding the cross-cultural and translation issues in mental health research. J Pregnancy Child Health. 2015;2:1000134. doi: 10.4172/2376-127X.1000134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Holm-Larsen CE, Madsen FK, Rogathi JJ, et al. Postpartum depression and child growth in Tanzania: a cohort study. BJOG. 2019;126:590–8. doi: 10.1111/1471-0528.15495. [DOI] [PubMed] [Google Scholar]
- 30.Mbarak B, Kilewo C, Kuganda S, et al. Postpartum depression among women with pre-Eclampsia and Eclampsia in Tanzania; a call for integrative intervention. BMC Pregnancy Childbirth. 2019;19:270. doi: 10.1186/s12884-019-2395-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rwakarema M, Premji SS, Nyanza EC, et al. Antenatal depression is associated with pregnancy-related anxiety, partner relations, and wealth in women in northern Tanzania: a cross-sectional study. BMC Womens Health. 2015;15:68. doi: 10.1186/s12905-015-0225-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rogathi JJ, Manongi R, Mushi D, et al. Postpartum depression among women who have experienced intimate partner violence: a prospective cohort study at Moshi, Tanzania. J Affect Disord. 2017;218:238–45. doi: 10.1016/j.jad.2017.04.063. [DOI] [PubMed] [Google Scholar]
- 33.Tsai AC, Scott JA, Hung KJ, et al. Reliability and validity of instruments for assessing perinatal depression in African settings: systematic review and meta-analysis. PLoS One. 2013;8:e82521. doi: 10.1371/journal.pone.0082521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stasik-O’Brien SM, McCabe-Beane JE, Segre LS. Using the EPDS to identify anxiety in mothers of infants on the neonatal intensive care unit. Clin Nurs Res. 2019;28:473–87. doi: 10.1177/1054773817740532. [DOI] [PubMed] [Google Scholar]
- 35.Spielberger CD. Manual for the State-Trait Anxiety Inventory STAI. Palo Alto, CA: Mind Garden; 1983. [Google Scholar]
- 36.Pedrabissi L, Santinello M. Firenze:: Organizzazioni Speciali; 1989. Inventario per L'Ansia Di Stato E Di Tratto: Nuova Versione Italiana Dello STAI-forma Y [manual for the state-trait anxiety inventory: new Italian version of the STAY-Y form] [Google Scholar]
- 37.Santangelo G, Sacco R, Siciliano M, et al. Anxiety in multiple sclerosis: psychometric properties of the state-trait anxiety inventory. Acta Neurol Scand. 2016;134:458–66. doi: 10.1111/ane.12564. [DOI] [PubMed] [Google Scholar]
- 38.Knowles KA, Olatunji BO. Specificity of trait anxiety in anxiety and depression: meta-analysis of the state-trait anxiety inventory. Clin Psychol Rev. 2020;82:101928. doi: 10.1016/j.cpr.2020.101928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ilardi CR, Gamboz N, Iavarone A, et al. Psychometric properties of the STAI-Y scales and normative data in an Italian elderly population. Aging Clin Exp Res. 2021;33:2759–66. doi: 10.1007/s40520-021-01815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gorenstein C, Andrade L. Validation of a Portuguese version of the Beck depression inventory and the state-trait anxiety inventory in Brazilian subjects. Braz J Med Biol Res. 1996;29:453–7. [PubMed] [Google Scholar]
- 41.Delgado AM, Freire A da B, Wanderley ELS, et al. Analysis of the construct validity and internal consistency of the state-trait anxiety inventory (STAI) state-anxiety (S-anxiety) scale for pregnant women during labor. Rev Bras Ginecol Obstet. 2016;38:531–7. doi: 10.1055/s-0036-1593894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ukpong DI, Owolabi AT. Psychiatric morbidity associated with caesarean section: a study from Wesley Guild hospital, Ilesa, Nigeria. J Obstet Gynaecol. 2004;24:891–4. doi: 10.1080/01443610400018726. [DOI] [PubMed] [Google Scholar]
- 43.Redinger S, Pearson RM, Houle B, et al. Antenatal depression and anxiety across pregnancy in urban South Africa. J Affect Disord. 2020;277:296–305. doi: 10.1016/j.jad.2020.08.010. [DOI] [PubMed] [Google Scholar]
- 44.Barisone MG, Lerda S, Ansaldi S, et al. Psychopathology and epilepsy: clinical experience in a centre for the diagnosis and care of epilepsy. Ital J Psychopathol. 2004;10:336–42. [Google Scholar]
- 45.Polloni L, Cavallin F, Lolli E, et al. Psychological wellbeing of parents with infants admitted to the neonatal intensive care unit during SARS-CoV-2 pandemic. Children (Basel) 2021;8:755. doi: 10.3390/children8090755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Julian LJ. Measures of anxiety: state-trait anxiety inventory (STAI), Beck anxiety inventory (BAI), and hospital anxiety and depression scale-anxiety (HADS-A) Arthritis Care Res (Hoboken) 2011;63 Suppl 11:S467–72. doi: 10.1002/acr.20561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Melnyk BM. Coping with unplanned childhood hospitalization: effects of informational interventions on mothers and children. Nurs Res. 1994;43:50–5. doi: 10.1097/00006199-199401000-00011. [DOI] [PubMed] [Google Scholar]
- 48.Abdelkader R, Khalaf I, Kridli S, et al. Parents involvement in child’s care in an Arab pediatric setting. Health Sci J. 2016;10:12. [Google Scholar]
- 49.Johnson Rolfes J, Paulsen M. Protecting the infant-parent relationship: special emphasis on perinatal mood and anxiety disorder screening and treatment in neonatal intensive care unit parents. J Perinatol. 2022;42:815–8. doi: 10.1038/s41372-021-01256-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Murthy S, Haeusslein L, Bent S, et al. Feasibility of universal screening for postpartum mood and anxiety disorders among caregivers of infants hospitalized in NICUs: a systematic review. J Perinatol. 2021;41:1811–24. doi: 10.1038/s41372-021-01005-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mendelson T, Cluxton-Keller F, Vullo GC, et al. NICU-based interventions to reduce maternal depressive and anxiety symptoms: a meta-analysis. Pediatrics. 2017;139:e20161870. doi: 10.1542/peds.2016-1870. [DOI] [PubMed] [Google Scholar]
- 52.Sabnis A, Fojo S, Nayak SS, et al. Reducing parental trauma and stress in neonatal intensive care: systematic review and meta-analysis of hospital interventions. J Perinatol. 2019;39:375–86. doi: 10.1038/s41372-018-0310-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Maleki M, Mardani A, Harding C, et al. Nurses' strategies to provide emotional and practical support to the mothers of preterm infants in the neonatal intensive care unit: a systematic review and meta-analysis. Womens Health (Lond Engl) 2022;18:174550572211046. doi: 10.1177/17455057221104674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Almadhoob A, Ohlsson A. Sound reduction management in the neonatal intensive care unit for preterm or very low birth weight infants. Cochrane Database Syst Rev. 2020;1:CD010333. doi: 10.1002/14651858.CD010333.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lazzerini M, Covi B, Mariani I, et al. Quality of care at childbirth: findings of imagine EURO in Italy during the first year of the COVID-19 pandemic. Int J Gynaecol Obstet. 2022;157:405–17. doi: 10.1002/ijgo.14119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lazzerini M, Covi B, Mariani I, et al. Imagine EURO study group. quality of facility-based maternal and newborn care around the time of childbirth during the COVID-19 pandemic: online survey investigating maternal perspectives in 12 countries of the WHO European region. Lancet Reg Health Eur . 2022;13:100268. doi: 10.1016/j.lanepe.2021.100268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dadi AF, Akalu TY, Baraki AG, et al. Epidemiology of postnatal depression and its associated factors in Africa: a systematic review and meta-analysis. PLoS One. 2020;15:e0231940. doi: 10.1371/journal.pone.0231940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bua J, Dalena P, Mariani I, et al. Parental stress, depression, anxiety and participation in care in neonatal intensive care unit: a cross-sectional study in Italy comparing mothers versus fathers. BMJ Paediatr Open . 2024;8:e002429. doi: 10.1136/bmjpo-2023-002429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lazzerini M, Sforzi I, Trapani S, et al. Characteristics and risk factors for SARS-CoV-2 in children tested in the early phase of the pandemic: a cross-sectional study, Italy, 23 February to 24 May 2020. Euro Surveill. 2021;26:2001248. doi: 10.2807/1560-7917.ES.2021.26.14.2001248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bua J, Mariani I, Girardelli M, et al. Parental stress, depression, and participation in care before and during the COVID-19 pandemic: a prospective observational study in an Italian neonatal intensive care unit. Front Pediatr. 2021;9:737089. doi: 10.3389/fped.2021.737089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pace CC, Spittle AJ, Molesworth CM-L, et al. Evolution of depression and anxiety symptoms in parents of very preterm infants during the newborn period. JAMA Pediatr. 2016;170:863–70. doi: 10.1001/jamapediatrics.2016.0810. [DOI] [PubMed] [Google Scholar]