To the editor:
Lymphatic malformations (LMs) are benign anomalies often detected at birth, with an incidence of 1.2–2.8 per 1000 newborns. 1 While most early‐life LMs are asymptomatic and may only require observation, some cases necessitate emergency intervention due to complications such as bleeding, infection, respiratory difficulties, and significant cosmetic deformities. 2
A variety of treatment methods exist for LMs, including surgical resection, percutaneous sclerotherapy, and oral medication. Although surgical resection is a traditional approach, it can lead to severe tissue defects and functional complications. Oral sirolimus can improve clinical status but poses toxicity risks for neonates. 3 Percutaneous sclerotherapy has emerged as a promising alternative, with bleomycin being an effective sclerosing agent due to its favorable safety profile and efficacy in inducing vessel occlusion with minimal side effects. 4
We report a case of a 2‐day‐old boy with giant left auricular and cervical LMs, which caused difficulty in nursing, potential hearing loss, and severe cosmetic deformity. Physical examination showed a giant, transparent, ligament‐filled left ear, significantly larger than the contralateral ear (11 cm × 7 cm × 4 cm vs. 3 cm × 2 cm × 1 cm), and the left external auditory canal could not be found (Figure 1A). After a thorough assessment, including laboratory tests, computed tomography (Figure 1B), and ultrasound (Figure 1C), the diagnosis of extensive LMs was confirmed.
FIGURE 1.
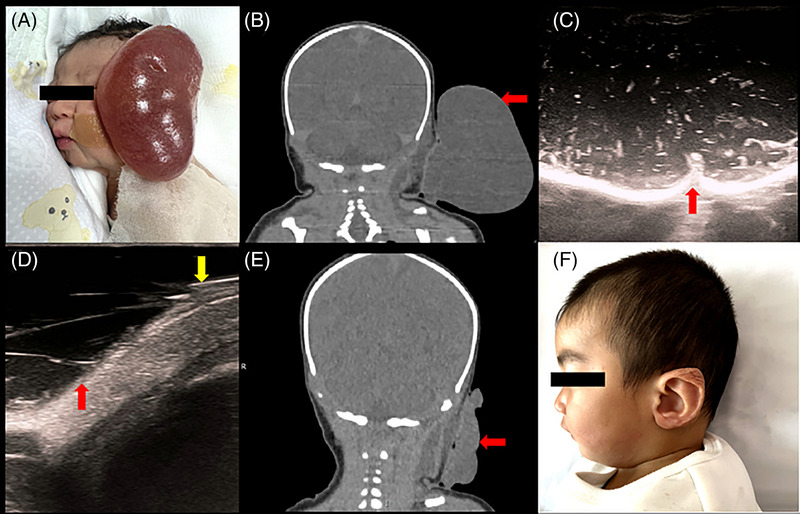
Bleomycin sclerotherapy with bedside ultrasound‐guided in emergency for an infant with lymphatic malformations. (A) The initial appearance of the lesion before treatment. (B) Coronal computed tomography (CT) of the lesion before treatment. (C) Ultrasound of the left auricula showed an anechoic area with some thin septa (red arrow). (D) Ultrasound image of the auricular lesion (red arrow) showing the aspiration of fluid by an 18‐G needle (yellow arrow) during the sclerotherapy procedure. (E) Coronal CT of the lesion at 9 days after therapy. (F) The appearance of the boy at the 1‐year follow‐up: the lesion is significantly diminished, and the aesthetic appearance has improved.
A multidisciplinary team recommended a two‐session treatment strategy of ultrasound‐guided bleomycin sclerotherapy. In the first session, rapid decompression was performed by aspiration of 132 mL of yellowish fluid with an 18‐G needle under local anesthesia, followed by 2 mL of bleomycin (Figure 1D). The patient experienced no complications, and a significant reduction in lesion size was observed nine days post‐therapy (Figure 1E). The second session, performed 4 months later, further reduced the residual lesion size, resulting in near‐total volume reduction and improved aesthetic appearance at the 1‐year follow‐up (Figure 1F).
Although most early‐life LMs are asymptomatic, emergency interventions are critical for neonates presenting with complications such as airway obstruction, feeding difficulties, or severe cosmetic deformities. In this case, the giant lesion in the left ear auricula and neck caused difficulty in feeding and nursing, potential hearing loss, and severe cosmetic deformity. Comorbid infections can be fatal, as bacteria can enter the systemic vasculature and quickly spread through the tissues, leading to cellulitis or even sepsis given the immaturity of the neonates’ immune systems. In addition, unintentional injuries or spontaneous intralesional bleeding may occur due to the thin and friable walls of the lesion.
Bleomycin sclerotherapy is particularly advantageous due to its balanced efficacy and safety profile. Systematic reviews indicate that bleomycin is effective in reducing LMs size with fewer adverse events compared to other sclerosants like ethanol and doxycycline. 5 Procedural safety is paramount, especially in neonates. The most common complications reported are pain, infection, hematomas, and hyperpigmentation, with complication rates in the literature ranging from 0% to 20%. 6 A major concern with the use of bleomycin is the risk of pulmonary toxicity, which has been studied but never reported in the treatment of LMs over variable follow‐up periods (maximum, 16 years). 5 The risk of pulmonary fibrosis in pediatric patients is associated with a cumulative dose of more than 300 000 IU (30 mg). 7 In our case, no adverse effects, including pulmonary fibrosis, were observed during the follow‐up period.
In conclusion, ultrasound‐guided percutaneous bleomycin sclerotherapy may be a safe and effective minimally invasive treatment for neonates with giant LMs requiring emergency intervention. This approach offers a promising alternative to surgical resection, with the potential for significant lesion reduction and improved cosmetic outcomes.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the parents of the patient.
CONFLICT OF INTEREST
The authors declare no conflict of interest.
Ding J, Hei M, Cai W, Shi W, Ni X. A neonate in emergency for giant auricular and cervical lymphatic malformations: Ultrasound‐guided percutaneous bleomycin sclerotherapy may be a choice. Pediatr Investig. 2024;8:316–318. 10.1002/ped4.12443
REFERENCES
- 1. Filston HC. Hemangiomas, cystic hygromas, and teratomas of the head and neck. Semin Pediatr Surg. 1994;3:147‐159. [PubMed] [Google Scholar]
- 2. Dong S, Li L, Xu J, Han Z, Zheng X. Rapid response with good toleration of sirolimus for life‐threatening neonatal lymphatic malformations. Pediatr Investig. 2023;7:206‐211. DOI: 10.1002/ped4.12397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ji Y, Chen S, Yang K, Zhou J, Zhang X, Jiang X, et al. A prospective multicenter study of sirolimus for complicated vascular anomalies. J Vasc Surg. 2021;74:1673‐1681. DOI: 10.1016/j.jvs.2021.04.071 [DOI] [PubMed] [Google Scholar]
- 4. Fernandes S, Yeung P, Heran M, Courtemanche D, Chadha N, Baird R. Sclerosing agents in the management of lymphatic malformations in children: a systematic review. J Pediatr Surg. 2022;57:888‐896. DOI: 10.1016/j.jpedsurg.2021.12.056 [DOI] [PubMed] [Google Scholar]
- 5. Horbach S, Rigter IM, Smitt J, Reekers JA, Spuls PI, van der Horst C. Intralesional bleomycin injections for vascular malformations: a systematic review and meta‐analysis. Plast Reconstr Surg. 2016;137:244‐256. DOI: 10.1097/PRS.0000000000001924 [DOI] [PubMed] [Google Scholar]
- 6. Ardıçlı B, Karnak İ, Çiftçi AÖ, Tanyel FC, Şenocak ME. Sclerotherapy with bleomycin versus surgical excision for extracervical cystic lymphatic malformations in children. Surg Today. 2016;46:97‐101. DOI: 10.1007/s00595-015-1128-0 [DOI] [PubMed] [Google Scholar]
- 7. O'Sullivan JM, Huddart RA, Norman AR, Nicholls J, Dearnaley DP, Horwich A. Predicting the risk of bleomycin lung toxicity in patients with germ‐cell tumours. Ann Oncol. 2003;14:91‐96. DOI: 10.1093/annonc/mdg020 [DOI] [PubMed] [Google Scholar]


