Abstract
Background:
Treatment of diabetes and its complications is a primary health care expense. Up to 25% of people with diabetes will develop diabetic foot ulcers (DFUs). Removable cast walker (RCW) boots commonly prescribed for DFU treatment, promote healing, and provide offloading and wound protection. Patient RCW removal for hygiene and wound care can lead to decreased adherence and treatment effectiveness. This study evaluated a new system for wear-time adherence measurement using multiple sensor types.
Methods:
An electronic wear-time monitor was developed, which included internal and external temperature sensors, an accelerometer, and capacitive proximity foot and ankle sensors. Time-stamped and date-stamped data were saved once per minute for up to 22 days. Ten healthy volunteer subjects were recruited to wear an RCW for two weeks while keeping a diary of don/doff times. Sensor data were then compared with volunteers’ wear diaries using confusion matrix predictive analytics.
Results:
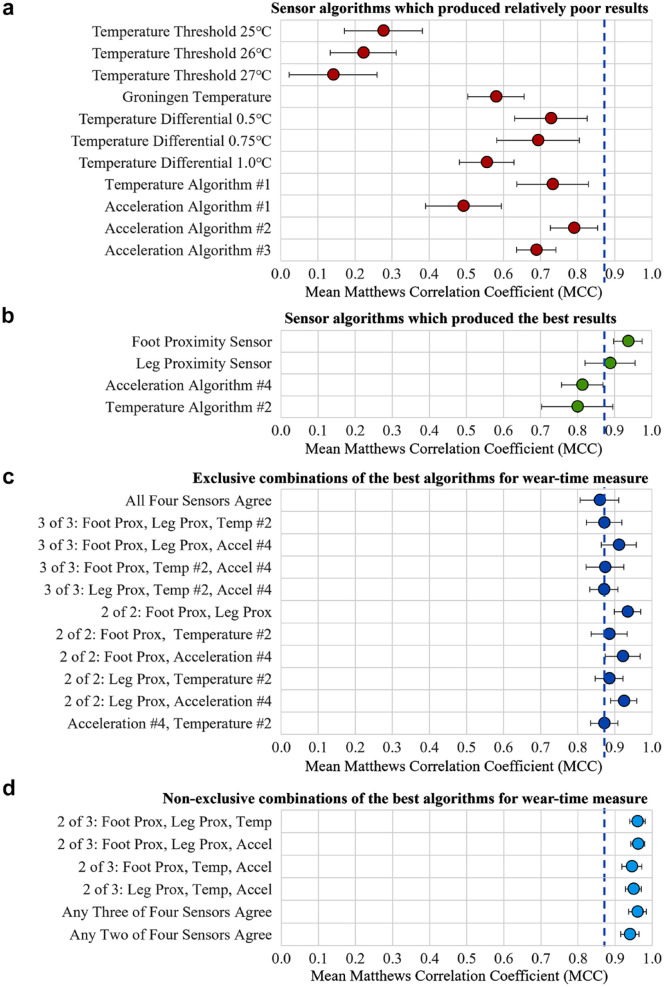
Algorithms were developed for data processing. Correlation coefficients between algorithms and diaries were calculated for individual and multiple sensor combinations. Differential temperature and accelerometer algorithms were significantly better at predicting subject wear-time than individual temperature sensor algorithms (P = .009, P = .001, respectively). Foot proximity had significantly better correlation with subject diaries than temperature (P = .024), and acceleration algorithms (P = .005). Multi-sensor analysis showed high correlation (.96) with wear-time from subject diaries.
Conclusions:
Removable cast walker wear-time can be accurately determined using an electronic data recorder and multiple sensors. Wear-time measurement accuracy can be improved using algorithms that operate on data from multiple sensors that use a variety of sensor technologies.
Keywords: diabetic foot ulcer, removable cast walker, adherence, adherence monitor, wear-time, orthosis wear-time
Introduction
Treatment of diabetes and its complications is a primary health care expense. An estimated 537 million adults worldwide had diabetes in 2021 with the numbers expected to increase by 46% by 2045. 1 Nearly half of patients with diabetes develop peripheral neuropathy, which reduces sensation and pain intensity in the feet and, up to a quarter of patients with diabetes will develop diabetic foot ulcers (DFUs) and disability.2-4 Diabetic foot ulcers are expensive to treat, reduce quality of life, and are associated with increased risk of life-threatening complications. Orthoses (custom shoe insoles, offloading removable cast walkers [RCWs], and offloading shoes, etc) are commonly prescribed to patients with DFU to promote wound healing, and to provide offloading and protection during activities of daily living.5,6 Orthotic footwear is cost-effective and generally considered effective for prevention and treatment of DFU.7-9 Failure to protect the foot can lead to ulcer worsening, infection, or surgical intervention, such as grafting or amputation.10-13
Diabetic foot ulcer offloading and adherence with prescribed treatment are important topics in diabetic foot care. 14 Offloading footwear including total contact casts (TCCs) that cannot be removed by the patient are considered the gold standard treatment for DFU. 15 The use of TCC can be clinically time intensive requiring weekly or biweekly recasting.16-18 One alternative, RCW boots, allows removal of the orthosis for hygiene purposes, daily wound care, and range of motion exercises. However, easy RCW removal can decrease patient adherence with prescribed wear, potentially leading to decreased treatment effectiveness and further injury of the foot.13,17
Non-adherence to prescribed wear-times (reduced wear) and lack of patient education are cited as reasons for failure of orthotic treatment.19-21 Clinician opinion and patient self-reports have been used as a subjective basis for determining the minimum wear-time necessary to achieve treatment goals.22-24 A review by Swinnen and Kerckhofs 20 on orthotic adherence reported that 6% to 80% of patients never wore their orthosis. Furthermore, patient self-reports tend to overestimate wear-time.22,25-28 Understanding patient non-adherence and finding ways to improve adherence are necessary for evidence-based DFU treatment. 3
The consensus from literature is that an electronic system can objectively determine orthosis wear-time and help in formulating evidence-based criteria for DFU treatment. 14 Electronic wear-time data can be examined against measures of wound healing to determine treatment efficacy and dosage effects. Accurately determined orthotic wear-time may allow clinicians to understand patient orthosis use and intervene in the treatment or change the offloading strategy if poor wear-time adherence is found. In turn, patients can be prompted to communicate concerns regarding comfort, appearance, perceived stability, disruptions to daily routines, or other adherence obstacles to clinicians. 29
Studies in the literature have attempted to measure orthosis wear-time using a variety of sensor technologies. Many of these systems are not well suited for wear-time measurement of RCW due to lack of accuracy, low data capacity, or because they are intended to be embedded into the orthotic insole while treatment of DFU often requires insole modification or replacement.
Keeping the clinical importance of accurately measuring wear-time in mind, a system was designed using multiple sensor technologies to determine when an orthosis was being worn (donned) and not worn (doffed). The system was based on our contention that a combination of sensors can provide more information to better determine whether an orthosis was being worn, especially during sedentary activities or when the RCW was exposed to extreme temperature environments.
The long-term goal of this research is to improve outcomes (reduce time to healing and complications) and reduce treatment costs of patients who are prescribed orthoses for DFU treatment. The short-term goals were to develop a cost-effective, accurate, and validated electronic system to measure wear-time of RCW boots and to provide measures of accuracy for different sensor types. Objective wear-time data from different sensor types attached to RCW orthoses were used in testing the following hypotheses.
Hypotheses
Hypothesis 1 (H1): It is possible to accurately determine RCW boot wear-time using electronic sensors and data recorder.
Hypothesis 1a (H1a): Accuracy of wear-time measurement will vary depending on sensor technology.
Hypothesis 1b (H1b): Multiple sensors and various combinations of sensor technologies can improve accuracy of wear-time measurement.
Materials and Methods
Design of Adherence Monitor
Requirements for the adherence monitor system included no alteration to the fit or function of the RCW. For this reason, the monitor system was attached to the outside of the boot shell so that the boot liner could be removed for hygiene purposes and to allow the foot bed to be replaced or modified as needed to provide offloading of the ulcer. The system was designed to collect data for a minimum of three weeks to cover the interval between most clinic follow-up visits, to store time-stamped data, to utilize multiple sensor technologies, and to be expandable to accommodate additional or alternate sensors for future use in other orthoses, prostheses, or assistive technologies.
Using these guidelines, the monitor circuitry included a low power microcontroller, real-time clock, and two megabits of memory. The monitor circuit board measures 32 mm (W) × 32 mm (L) × 7.5 mm (H) and was housed in an enclosure attached to the outside of the RCW’s plastic shell, positioned laterally over the ankle of the affected foot. This location had a relatively flat surface and was the location least likely to affect a subject/patient during wear. The system was powered by a replaceable 3-V coin cell battery (CR1632). The enclosure was designed to protect the recorder circuit board from impact and measures approximately 42 mm (W) × 65 mm (L) × 10mm (H) (Figure 1a).
Figure 1.
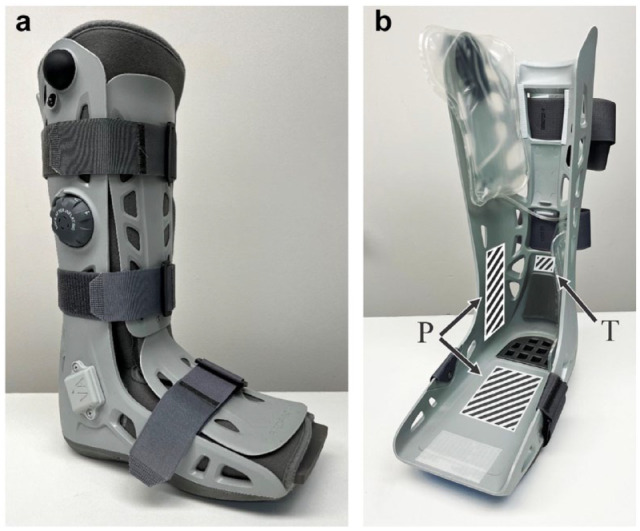
(a) Removable cast walker (Aircast AirSelect, DJO Global, Vista, California) with the adherence monitor mounted externally over the ankle. (b) Inside of the RCW with liner removed and right-side air bladder lifted out of the way to show sensor placement. (P) shows placement of proximity sensors. (T) shows placement of internal temperature sensor.
Sensors
To determine RCW wear-time, the data recorder collected data from five electronic sensors. Preliminary studies and published literature were used to delineate sensor technologies that were best capable of minimal power consumption and accurate wear-time measures. These sensors included two temperature sensors, a three-axis accelerometer, and two capacitive proximity sensors. Time-stamped and date-stamped sensor data were saved once per minute allowing the recorder to save up to 22 days of wear-time data. The sample period could be altered to accommodate longer data collection periods.
The two capacitive proximity sensors were secured to the inside of the boot shell, one under the mid-foot and the other laterally over the ankle (Figure 1b). Each proximity sensor was 0.012 mm thick with an area of 60 cm2 and was tuned to respond when a conductive body was within 30 mm of the sensor. One temperature sensor was secured to the inside of the boot shell behind the boot liner and above the heel padding (Figure 1b). The second temperature sensor measured ambient temperature and was on the monitor circuit board attached to the outside of the RCW.24,25,30-32 Two temperature sensors allowed calculation of differential temperature. Boot acceleration was measured using the three-axis accelerometer also on the monitor circuit board attached to the RCW shell exterior. Since the goal of this technology was to measure RCW wear-time, and since limiting standing and walking is part of the prescribed treatment of DFUs, the accelerometer monitored boot orientation or instantaneous acceleration and not step count or physical activity (PA) that would require greater memory for data storage and a larger battery or periodic battery charging.
Validation of the Monitor
Ten healthy volunteer subjects (four males and six females) were recruited from medical center staff. After oversight committee approvals, subjects were provided an RCW with wear-time monitor and asked to periodically wear the orthosis for two weeks. There were no restrictions regarding where or when to wear the orthoses. However, they were requested to wear the orthoses for greater than ten minutes per don/doff event and instructed that daily wear should include at least two don/doff events. Subjects were instructed to keep a written diary of don/doff times. To ensure accurate time keeping, subjects were instructed to use computer time or cellular clock UTC (universal time coordinated) synced times. All subjects wore an RCW commonly prescribed for treatment of DFU (Aircast AirSelect, DJO Global, Vista, California) (Figure 1).
After the first three subjects completed their participation, data showed that the proximity sensor gain was too high resulting in signal saturation and compromised accuracy. The gain was subsequently adjusted, and the remaining subjects used data recorders programmed with the revised gain values. The first three subjects then repeated their wear trials for an additional two weeks.
Data Analysis
The recorded data sets included date and time stamps accurate to the minute. Sensor data included internal and external temperature with 0.25°C resolution, ±2 g X-Y-Z acceleration data, and foot and leg proximity data. Using analysis algorithms, sensor data were reduced to binary values with 1 representing when the orthosis was worn and 0 representing not worn. These algorithms included custom written and literature derived algorithms that used temperature differential or temperature thresholds.33,34 The Groningen algorithm, e.g., uses the slope and peaks of an individual temperature sensor to determine wear-time. 34
Several custom algorithms were developed to analyze temperature and acceleration sensor data, but only one algorithm was developed to process proximity data. A primary goal of data analysis was that the algorithms be automated to improve the processing speed and reduce human intervention. This strategy worked for temperature and acceleration, but not for proximity data that proved too variable for a completely automated routine and required that an analyst be part of the data analysis process.
Data from the algorithms were then compared with actual wear-time as recorded by the volunteers in their written diaries using binary classification and confusion matrix predictive analytics. 35 Algorithm output data were compared with true values from the subject diary producing measures of accuracy. The first step in this analysis was to reduce each algorithms output into counts of true positive (TP), true negative (TN), false positive (FP), and false negative (FN). Using equations from Table 1, these measures were then used to calculate precision, sensitivity and a measure of accuracy using the Matthews correlation coefficient (MCC).35,36
Table 1.
Equations Used for Confusion Matrix Analysis of Subject RCW Wear-Time Diary Data vs Adherence Monitor Electronic Data.
| Matrix measure | Equation | Result range |
|---|---|---|
| Precision | 0 ≤ precision ≤ 1 | |
| Sensitivity (recall, TPR) | 0 ≤ sensitivity ≤ 1 | |
| MCC accuracy | –1 ≤ MCC ≤ 1 |
Abbreviations: TPR, true-positive rate; MCC, Matthews correlation coefficient; Sqrt, square root; True positive (TP), when the diary and sensor algorithms agree the RCW was worn. True negative (TN), when both agree the RCW was not worn. False positive (FP), when the sensor algorithm indicates the RCW is being worn but diary indicates the RCW was not worn. False negative (FN), when the sensor algorithm indicates the RCW is not worn, but the diary indicates the RCW was worn.
The results from all subjects were averaged to determine average precision, sensitivity, and MCC with confidence intervals. Statistical analysis was performed using R 4.3.0 statistical software (R Core Team, 2023). Wilcoxon rank sum exact test with Bonferroni correction for multiple comparisons was used to test for significance. Significance was set at P < .05.
Results
Wear-time data from subjects’ written diaries are presented in Table 2. Trial dates are presented to show data were collected during the Northern Hemisphere Spring and Summer causing the greatest challenge for temperature sensor algorithms.
Table 2.
Data From Subjects’ Written Wear-Time Diaries.
| Trial start and end dates (month/day) | Number of don/doff events | Subject diary don time | Subject diary doff time | Total recorded time | |||||
|---|---|---|---|---|---|---|---|---|---|
| Subject | Start | End | Total minutes | Days h:min |
Total minutes | Days h:min |
Total minutes | Days h:min |
|
| 1. Trial 1 | 4/19 | 5/4 | 28 | 1768 | 01 05:28 |
19 835 | 13 18:35 | 21 603 | 15 00:03 |
| 2. Trial 1 | 4/21 | 5/8 | 23 | 1778 | 01 05:38 |
22 810 | 15 20:10 | 24 589 | 17 01:49 |
| 3. Trial 1 | 4/21 | 5/8 | 22 | 1147 | 00 19:07 |
23 177 | 16 02:17 | 24 324 | 16 21:24 |
| 1. Trial 2 | 8/4 | 8/23 | 22 | 1546 | 01 01:46 |
25 533 | 17 17:33 | 27 079 | 18 19:19 |
| 2. Trial 2 | 8/24 | 9/11 | 26 | 4863 | 03 09:03 |
20 936 | 14 12:56 | 25 799 | 17 21:59 |
| 3. Trial 2 | 9/21 | 10/13 | 25 | 1245 | 00 20:45 |
30 295 | 21 00:55 | 31 540 | 21 21:40 |
| 4 | 5/16 | 6/5 | 20 | 2467 | 01 17:07 |
26 061 | 18 02:21 | 28 528 | 19 19:28 |
| 5 | 5/16 | 6/5 | 20 | 1064 | 00 17:44 |
27 588 | 19 03:48 | 28 652 | 19 21:32 |
| 6 | 5/17 | 6/5 | 19 | 1425 | 00 23:45 |
18 918 | 13 03:18 | 20 343 | 14 03:03 |
| 7 | 6/7 | 6/27 | 4 | 177 | 00 02:57 |
28 779 | 19 23:39 | 28 956 | 20 02:36 |
| 8 | 6/7 | 6/23 | 21 | 1247 | 00 20:47 |
21 526 | 14 22:46 | 22 773 | 15 19:33 |
| 9 | 6/8 | 6/27 | 20 | 2078 | 01 10:38 |
25 367 | 17 14:47 | 27 445 | 19 01:25 |
| 10 | 6/8 | 6/27 | 13 | 789 | 00 13:09 |
26 580 | 18 11:00 | 27 369 | 19 00:09 |
| Total | 263 | 21 595 | 14 23:55 |
317 405 | 220 10:05 | 339 000 | 235 10:00 |
||
| Average | 20 | 1661 | 01 03:41 |
24 416 | 16 22:55 | 26 077 | 18 02:36 |
||
The number of don/doff events is the total number of times the subject wore the RCW. Don time is the total time the subject wore the RCW. Doff time is the total time the subject was not wearing the RCW. Total recorded time is the amount of time the wear-time recorder collected data.
The data recorders maintained accurate time throughout the trials remaining within ±3 seconds of UTC. Saturation of the proximity sensor signals in the first trials for subjects 1 to 3 caused difficulty with analysis of those data sets. However, these data were still included in the analyses. Accelerometer data from two trials (subject 3 trial 1 and subject 8) were not usable due to failure of the solder bond of the accelerometer chip to the circuit board.
Mean values of performance were calculated by applying each algorithm to the data obtained from the 13 volunteer RCW data sets. The first four algorithms (temp. threshold 25°C through Groningen temperature algorithm) use temperature measurements from inside the RCW only (Table 3A, Figure 2a). These four algorithms using an individual temperature sensor produced the poorest predictive wear-time results. The remaining four temperature algorithms (Table 3A, Figure 2a) use temperature differential between the internal and external sensors.
Table 3.
Heatmap of Predictive Analytic Results.
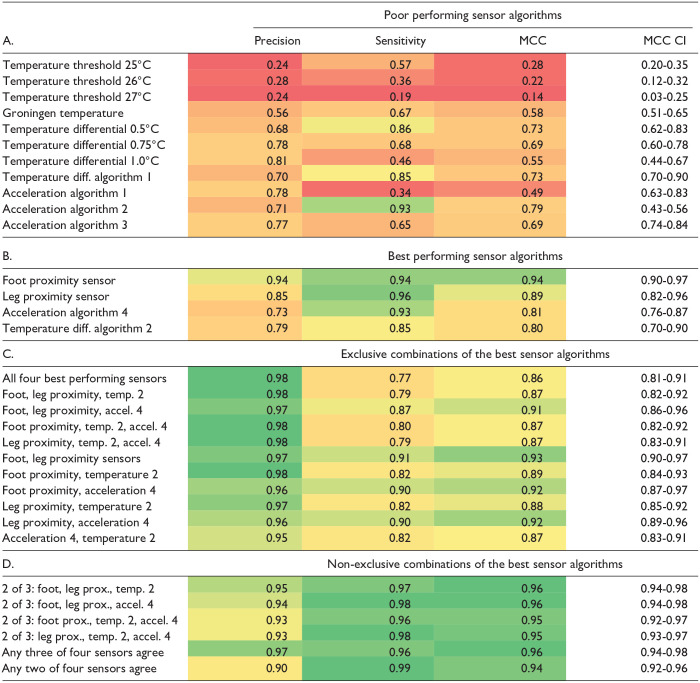
|
The table presents mean values of precision, sensitivity, and correlation data (MCC) of each algorithm’s ability to correctly classify wear and non-wear compared with volunteers’ wear-time diary data. Temperature differential (diff.) algorithms use temperature difference between internal and external sensors for analysis. (A.) Algorithms which produced the lowest precision, sensitivities, and MCC. (B.) Results of the best algorithms at correctly predicting wear-times. (C.) Results of exclusive combinations of the best sensor/algorithms (all sensors listed are included in analysis) at accurately predicting wear-times. (D.) Results of non-exclusive combinations of the best sensor algorithms (at each time interval, one or two of the sensors listed is not used to determine wear) at correctly predicting wear-times. Abbreviations: MCC, Matthews correlation coefficient; CI, 95% confidence interval; diff., differential; temp., temperature; prox., proximity.
Figure 2.
Mean Matthews correlation coefficient (MCC) results with 95% confidence intervals for 13 subject trials. The blue dashed line is drawn at 0.87 (87%), the level of predictive performance provided by the combination of the best acceleration and the best temperature algorithm (ie, acceleration 4 and temperature 2). (a) Algorithms which produced the lowest accuracy. (b) Best performing sensor algorithms. (c) Exclusive combinations of sensor/algorithms at predicting subject wear-time. (d) Non-exclusive combinations, or majority agreement of sensor/algorithms at predicting subject wear-time.
The individual sensor/algorithms which provided the best measure of orthosis wear-time are presented in Table 3B and Figure 2b. Table 3C and Figure 2c present results using exclusive combinations of sensor/algorithms using the best algorithm performers from Table 2B. These combinations were calculated using a logical AND on the output of the specified sensor/algorithms. In this way, if all algorithms in the data set provided a logic 1 (RCW was worn) then the result was a logic 1. If the output of any of the individual algorithms was logic 0 (not worn) the combined result was 0. Combined analysis resulted in improved wear-time results compared with results of these sensors alone, and overall tended to maximize precision while simultaneously improving wear-time MCC accuracy.
Results in Table 3D and Figure 2d are from non-exclusive combinations of the best performing sensor/algorithms. These combinations result in a logic 1 (RCW is worn) when at least two of three, three of four, or two of four of the algorithms agree the orthosis is donned. Not requiring unanimous agreement of the sensors, improves the correlation with subject diaries compared with exclusive combinations, and further highlights the importance of using multiple sensors and sensor technologies.
Table 4 presents MCC data for the best performing algorithms (Table 3B) applied to each individual subject trial showing intersubject variability in algorithm performance.
Table 4.
Results of Each Volunteer Subject Showing Matthews Correlation Coefficients (MCC) of the Best Sensor Algorithms at Correctly Predicting Wear-Times.
| Subject | Proximity foot | Proximity leg | Acceleration 4 | Temperature 2 |
|---|---|---|---|---|
| 1—Trial 1 | 0.93 | 0.97 | 0.79 | 0.86 |
| 2—Trial 1 | 0.75 | 0.91 | 0.65 | 0.69 |
| 3—Trial 1 | 0.88 | 0.97 | — | 0.39 |
| 1—Trial 2 | 0.99 | 0.98 | 0.86 | 0.94 |
| 2—Trial 2 | 1.00 | 0.90 | 0.87 | 0.97 |
| 3—Trial2 | 0.91 | 0.67 | 0.72 | 0.83 |
| 4 | 0.98 | 0.62 | 0.93 | 0.87 |
| 5 | 0.98 | 0.99 | 0.90 | 0.94 |
| 6 | 0.93 | 0.80 | 0.85 | 0.80 |
| 7 | 0.97 | 0.84 | 0.65 | 0.96 |
| 8 | 0.88 | 0.93 | - | 0.59 |
| 9 | 0.98 | 0.98 | 0.79 | 0.63 |
| 10 | 0.98 | 0.98 | 0.94 | 0.93 |
| Mean MCC | 0.94 | 0.89 | 0.81 | 0.80 |
| Stdev. | 0.07 | 0.12 | 0.10 | 0.18 |
| MCC CI | 0.90-0.97 | 0.82-0.96 | 0.76-0.87 | 0.70-0.90 |
Acceleration data were not available for subject 3, trial 1 and for subject 8.
Abbreviations: CI, confidence interval; stdev., standard deviation.
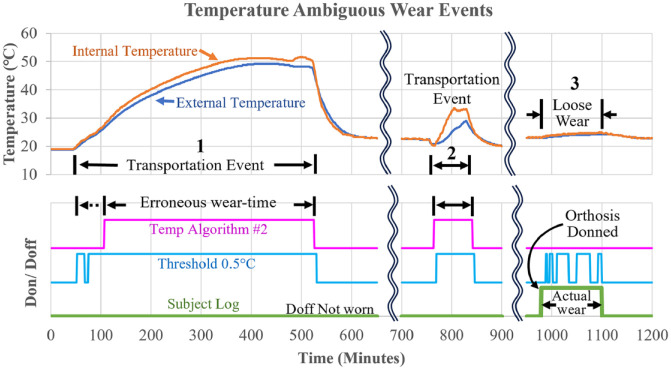
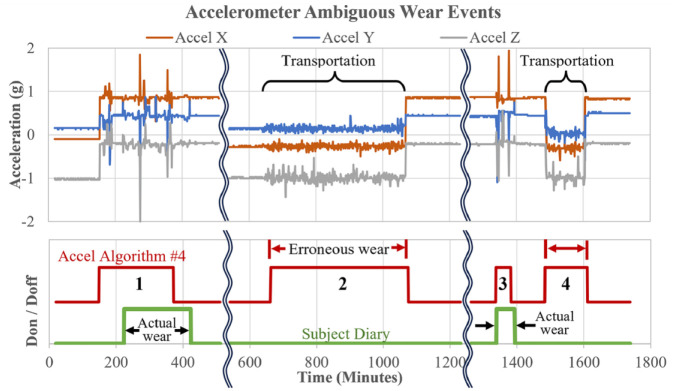
Algorithms based on acceleration and differential temperature had occasional difficulties discriminating wear from non-wear. Figure 3 shows two examples from one subject where the best temperature algorithm (temperature 2) was unable to accurately classify wear-time because of a positive temperature deviation while, per the subject log, the RCW was being transported. The third event was misclassified as non-wear due to a small temperature differential. Figure 4 shows data from a subject in which acceleration data (acceleration 4) during transportation of the RCW was misclassified. Interestingly, in each of these data sets, both the accelerometer and temperature algorithms had difficulty correctly classifying these transportation events, but the proximity sensors correctly identified these events. These figures highlight some challenges of using only one sensor technology for wear-time measurement.
Figure 3.
Examples of inaccurate wear/non-wear classification using differential temperature algorithms. The top graph shows internal and ambient temperature of three thermal events. The bottom graph shows data from the subject’s diary and the output of the two temperature algorithms (high = don, low = doff). The first two temperature events which were erroneously labeled as don time by the temperature algorithms, occurred during transportation of the RCW in a warm vehicle. The third event likely occurred because of loosely wearing the RCW in an office setting, such that, the leg was not in contact with the boot liner and hence was not near the internal temperature sensor.
Figure 4.
Examples of inaccurate wear-time classification by an accelerometer algorithm. Vehicle transportation of the RCW or other non-wear activities was erroneously interpreted as wear-time by the best accelerometer wear-time algorithm. The top graph shows accelerometer X, Y, Z data. The subject diary trace shows actual don/doff times. The accelerometer algorithm trace shows premature and incorrect identification of the start and end of wear event 1, and good identification of event 3. From the subject’s diary, events 2 and 4 are known to be transportation of the orthosis but were erroneously labeled as don time by the algorithm.
Statistical analyses of MCC showed that the best differential temperature algorithm (temperature 2) and the best accelerometer algorithm (acceleration 4) were both significantly better at predicting subject wear-time than the best algorithm based on an individual temperature sensor (Groningen) (P = .009 and P = 0.001, respectively). The foot proximity sensor algorithm had significantly higher correlation with subject diaries than the best differential temperature algorithm, temperature 2 (P = .024), and the best acceleration algorithm (acceleration 4) (P = .005).
Discussion
Wear-time recorders in the literature are not well suited for RCW wear-time measurement of DFU patients because they are intended to be placed inside the orthosis or embedded into an orthotic insole or will alter the fit or function of the orthosis. Treatment of DFUs at our medical center using RCW boots often requires insole modification or replacement by clinic staff to allow for ulcer site offloading. Therefore, we chose to integrate the electronic monitor system into the RCW shell that would not alter the orthosis fit, function, prescription, or cause difficulties for the patient or clinical staff. The RCW used in this study has a removable padded liner and inflatable bladders to improve comfort and fit. These both present challenges for integration of an adherence monitor.
Many studies in the literature which measured wear-time of orthoses or custom-made footwear used a single temperature sensor placed adjacent to the skin.22,30,31,37-39 This arrangement is prone to false positives when ambient temperature approaches skin temperature. 40 Lutjeboer et al. used temperature sensors placed in the insole to measure foot temperature but not ambient temperature. Analysis of their data was done using their Groningen algorithm. 34 Our implementation of the Groningen algorithm resulted in only modest prediction of actual wear-time (Table 3). This may be due to the limited description of the algorithm, or the fact that placement of sensors in that study was more responsive to temperature change than sensor placement in this study.
Other recent publications used two temperature sensors, one facing toward and the other away from the patient.24,30,31 Using temperature differential produced more accurate results and better agreement with subject diaries in this work and published work by Menz and Bonanno. 33
Data collected in this study provided the ability to compare wear-time algorithms based on each individual sensor type and combinations of sensors. Our results of differential temperature measurement may have been degraded because the internal temperature sensor was not placed in contact with or even adjacent to the skin as in other published studies .24,31,33 Instead, the sensor was secured to the inside of the RCW shell and behind the liner. This placement insulated the sensor from the foot and reduced the distance between the external (ambient sensor) and the internal sensor, likely decreasing the temperature differential. Illustrating this, in our study, the temperature differential was generally < 3°C, compared with 6°C to 7°C in the work of Menz and Bonanno. 33
Physical activity monitors are good at detecting activities, such as walking, running, and stair climbing. 41 Inactivity/sedentary behavior and non-use of the PA monitor produce similar accelerometer data. Therefore, algorithms were developed to classify inactivity or non-use based on how long there is minimal or no acceleration.42-44 Diabetic foot ulcer patients are specifically requested to limit activities, such as standing and walking. For these reasons, PA monitors may not provide an accurate assessment of wear-time for DFU patients.
The proximity sensor algorithms had the highest MCC, but the sensors required considerable surface area inside the orthosis, were the most complex to integrate in the orthosis, and are known to be sensitive to moisture and proximity to electrically conductive objects external to the orthosis. In our volunteer trials, there were no issues with moisture, but this will likely occur in a patient population where cleaning of the RCW, extended wear-times causing perspiration, rain, snowfall, and so on are likely. While not statistically significant, the foot proximity sensor was notably better at predicting wear-time than the leg proximity sensor. Potential reasons for this are that inflatable bladders inside the RCW may increase the distance between the sensor and subject leg and it is possible for the leg to migrate anteriorly during walking or sitting if the leg straps on the RCW are not snug. The foot sensor does not have this limitation as the foot is always in contact with the RCW insole and a fixed distance from the sensor.
This volunteer data set showed a wear-time vs total recorded time ratio of 6.5% ± 4.4%, which means subject orthosis wear averaged just over 90 minutes a day. Diabetic foot ulcer patients are typically requested to wear the orthosis as much as can be tolerated, and during all weight-bearing activities. Therefore, it is expected that DFU patient wear-times will be greater than volunteer wear-times, which may affect sensor and data processing algorithm function.
Given the shortcomings of the different sensors investigated in this study, sensor type, sensor placement, and orthosis type will all affect the accuracy of a multi-sensor adherence system. Our data show multiple sensors and varying types of sensors can improve wear-time adherence system accuracy.
The main limitation of this study concerned the location of the internal temperature sensor. As previously discussed, its location was dictated by the RCW design incorporating a removable liner and inflatable bladders. Due to its attachment to the RCW shell, the sensitivity of the internal temperature sensor was likely diminished.
Difficulties with the proximity sensor gain, data analysis, and their sensitivity to ambient moisture, such as perspiration proved to be other limitations. We chose to use the accelerometer to measure boot orientation as a surrogate for motion and not measure step count. This was done to preserve battery life, memory space, and because the clinical prescription is to limit ambulation. Future revision may include step count for comparative analysis.
Our goal, in this work, was to automate data processing to not affect clinic workflow. While fully automated data processing was not realized for the proximity sensors, this limitation does not diminish the value of the technology and analysis presented.
Conclusion
This study demonstrated that RCW wear-time up to three weeks can be accurately determined using an electronic system composed of a data recorder and multiple sensors. Results show that the wear-time monitoring system performed as intended, that accuracy of wear-time measurement is dependent on sensor technology and accuracy can be improved using multiple sensors and a variety of sensor technologies.
Acknowledgments
The contents of this work do not represent the views of the US Department of Veterans Affairs or the United States Government. The authors thank the study volunteer subjects for their participation.
Footnotes
Abbreviations: Accel., acceleration; CI, confidence interval; DFU, diabetic foot ulcer; Diff., differential; FN, false negative; FP, false positive; MCC, Matthews correlation coefficient; PA, physical activity; prox., proximity; RCW, removable cast walker; stdev., standard deviation; TCC, total contact cast; temp., temperature; TN, true negative; TP, true positive; UTC, universal time coordinated.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Grant from the Hines VA-Serwa Research Center on Aging, Chicago Association for Research and Education in Science, Hines, IL. Merit Review Award #1 I01 RX003781 from the U.S. Department of Veterans Affairs, Rehabilitation Research and Development Service, Washington, DC.
ORCID iD: Robert M. Havey  https://orcid.org/0000-0003-4040-8169
https://orcid.org/0000-0003-4040-8169
References
- 1. International Diabetes Federation. IDF Diabetes Atlas. 10th ed. Brussels, Belgium: International Diabetes Federation; 2021. [Google Scholar]
- 2. Aring A, Jones D, Falko J. Evaluation and prevention of diabetic neuropathy. Am Fam Physician. 2005;71(11):2123-2128. [PubMed] [Google Scholar]
- 3. Armstrong DG, Boulton AJ, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376(25):2367-2375. [DOI] [PubMed] [Google Scholar]
- 4. Stockl K, Vanderplas A, Tafesse E, Chang E. Costs of lower-extremity ulcers among patients with diabetes. Diabetes Care. 2004;27(9):2129-2134. [DOI] [PubMed] [Google Scholar]
- 5. Bellomo F, Lee S, McCarthy M, et al. Management of the diabetic foot. Semin Vasc Surg. 2022;35(3):219-227. [DOI] [PubMed] [Google Scholar]
- 6. de Oliveira A, Moore Z. Treatment of the diabetic foot by offloading: a systematic review. J Wound Care. 2015;24(12):560-570. [DOI] [PubMed] [Google Scholar]
- 7. Bus SA, Valk GD, van Deursen RW, et al. The effectiveness of footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in diabetes: a systematic review. Diabetes Metab Res Rev. 2008;24(suppl 1):S162-S180. [DOI] [PubMed] [Google Scholar]
- 8. Ulbrecht JS, Hurley T, Mauger DT, Cavanagh PR. Prevention of recurrent foot ulcers with plantar pressure–based in-shoe orthoses: the CareFUL prevention multicenter randomized controlled trial. Diabetes Care. 2014;37(7):1982-1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chantelau E, Haage P. An audit of cushioned diabetic footwear: relation to patient compliance. Diabet Med. 1994;11(1):114-116. [DOI] [PubMed] [Google Scholar]
- 10. Dang CN, Boulton AJ. Changing perspectives in diabetic foot ulcer management. Int J Low Extrem Wounds. 2003;2(1):4-12. [DOI] [PubMed] [Google Scholar]
- 11. Pinzur MS, Slovenkai MP, Trepman E, Shields NN, Diabetes Committee of American Orthopaedic Foot and Ankle Society. Guidelines for diabetic foot care: recommendations endorsed by the Diabetes Committee of the American Orthopaedic Foot and Ankle Society. Foot Ankle Int. 2005;26(1):113-119. [DOI] [PubMed] [Google Scholar]
- 12. Najafi B, Grewal GS, Bharara M, Menzies R, Talal TK, Armstrong DG. Can’t stand the pressure: the association between unprotected standing, walking, and wound healing in people with diabetes. J Diabetes Sci Technol. 2017;11(4):657-667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Armstrong DG, Lavery LA, Kimbriel HR, Nixon BP, Boulton AJ. Activity patterns of patients with diabetic foot ulceration. Diabetes Care. 2003;26(9):2595-2597. [DOI] [PubMed] [Google Scholar]
- 14. Bus SA, Reeves ND, Armstrong DG, Najafi B. Offloading and adherence through technological advancements: modern approaches for better foot care in diabetes. Diabetes Metab Res Rev. 2024;40(2):e3769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bus SA, Armstrong DG, Crews R, et al. Guidelines on offloading foot ulcers in persons with diabetes (IWGDF 2023 update). Diabetes Metab Res Rev. 2023;40(3):e3647. [DOI] [PubMed] [Google Scholar]
- 16. Crews R, Shen B, Campbell L, et al. Role and determinants of adherence to off-loading in diabetic foot ulcer healing: a prospective investigation. Diabetes Care. 2016;39(8):1371-1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mrdjenovich DE. Off-loading practices for the wounded foot: concepts and choices. J Am Col Certif Wound Spec. 2010;2(4):73-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Armstrong DG, Nguyen HC, Lavery LA, Van Schie CH, Boulton AJ, Harkless LB. Off-loading the diabetic foot wound. Diabetes Care. 2001;24(6):1019-1022. [DOI] [PubMed] [Google Scholar]
- 19. Knowles EA, Boulton AJ. Do people with diabetes wear their prescribed footwear. Diabet Med. 1996;13(12):1064-1068. [DOI] [PubMed] [Google Scholar]
- 20. Swinnen E, Kerckhofs E. Compliance of patients wearing an orthotic device or orthopedic shoes: a systematic review. J Bodyw Mov Ther. 2015;19(4):759-770. [DOI] [PubMed] [Google Scholar]
- 21. Lincoln N, Radford K, Game F, Jeffcoate W. Education for secondary prevention of foot ulcers in people with diabetes: a randomized controlled trial. Diabetologia. 2008;51(11):1954-1961. [DOI] [PubMed] [Google Scholar]
- 22. Nicholson GP, Ferguson-Pell MW, Smith K, Edgar M, Morley T. The objective measurement of spinal orthosis use for the treatment of adolescent idiopathic scoliosis. Spine. 2003;28(20):2243-2250. [DOI] [PubMed] [Google Scholar]
- 23. Devanand D, Kedgley A. Objective methods of monitoring usage of orthotic devices for the extremities: a systematic review. Sensors. 2023;23(17):3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bus SA, Waaijman R, Nollet F. New monitoring technology to objectively assess adherence to prescribed footwear and assistive devices during ambulatory activity. Arch Phys Med Rehabil. 2012;93(11):2075-2079. [DOI] [PubMed] [Google Scholar]
- 25. Sangiorgio SN, Ho NC, Morgan RD, Ebramzadeh E, Zionts LE. The objective measurement of brace-use adherence in the treatment of idiopathic clubfoot. J Bone Joint Surg Am. 2016;98(19):1598-1605. [DOI] [PubMed] [Google Scholar]
- 26. Kuroki H, Inomata N, Hamanaka H, Higa K, Chosa E, Tajima N. Efficacy of the Osaka Medical College (OMC) brace in the treatment of adolescent idiopathic scoliosis following Scoliosis Research Society brace studies criteria. Scoliosis. 2015;10:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Waddell KJ, Lang CE. Comparison of self-report versus sensor-based methods for measuring the amount of upper limb activity outside the clinic. Arch Phys Med Rehabil. 2018;99(9):1913-1916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ababneh A, Finlayson K, Edwards H, et al. The validity and reliability of self-reported adherence to using offloading treatment in people with diabetes-related foot ulcers. Sensors. 2023;23(9):4423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Merbitz N. Treatment adherence. In: Budd MA, Hough S, Wegener ST, Stiers W, eds. Practical Psychology in Medical Rehabilitation. Cham: Springer; 2017:433-442. [Google Scholar]
- 30. Telfer S, Munguia J, Pallari J, Dalgarno K, Steultjens M, Woodburn J. Personalized foot orthoses with embedded temperature sensing: proof of concept and relationship with activity. Med Eng Phys. 2014;36(1):9-15. [DOI] [PubMed] [Google Scholar]
- 31. Waaijman R, Keukenkamp R, de Haart M, Polomski WP, Nollet F, Bus SA. Adherence to wearing prescription custom-made footwear in patients with diabetes at high risk for plantar foot ulceration. Diabetes Care. 2013;36(6):1613-1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Karol L, Virostek D, Felton K, Wheller L. Effect of compliance counseling on brace use and success in patients with adolescent idiopathic scoliosis. J Bone Joint Surg. 2016;98(1):9-14. [DOI] [PubMed] [Google Scholar]
- 33. Menz HB, Bonanno DR. Objective measurement of adherence to wearing foot orthoses using an embedded temperature sensor. Med Eng Phys. 2021;88:19-24. [DOI] [PubMed] [Google Scholar]
- 34. Lutjeboer J, Van Netten J, Postema K, Hijmans J. Validity and feasibility of a temperature sensor for measuring use and non-use of orthopedic footwear. J Rehabil Med. 2018;50(10):920-926. [DOI] [PubMed] [Google Scholar]
- 35. Foody GM. Challenges in the real world use of classification accuracy metrics: from recall and precision to the Matthews correlation coefficient. PLoS ONE. 2023;18(10):e0291908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Chicco D, Jurman G. The advantages of the Matthews correlation coefficient (MCC) over F1 score and accuracy in binary classification evaluation. BMC Genomics. 2020;21:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Miller DJ, Franzone JM, Matsumoto H, et al. Electronic monitoring improves brace-wearing compliance in patients with adolescent idiopathic scoliosis: a randomized clinical trial. Spine. 2012;37(9):717-721. [DOI] [PubMed] [Google Scholar]
- 38. Hunter LN, Sison-Williamson M, Mendoza MM, et al. The validity of compliance monitors to assess wearing time of thoracic-lumbar-sacral orthoses in children with spinal cord injury. Spine. 2008;33(14):1554-1561. [DOI] [PubMed] [Google Scholar]
- 39. Ehrmann D, Spengler M, Jahn M, et al. Adherence over time: the course of adherence to customized diabetic insoles as objectively assessed by a temperature sensor. J Diabetes Sci Technol. 2018;12(3):695-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Nardin RA, Fogerson PM, Nie R, Rutkove SB. Foot temperature in healthy individuals: effects of ambient temperature and age. J Am Podiatr Med Assoc. 2010;100(4):258-264. [DOI] [PubMed] [Google Scholar]
- 41. Yang CC, Hsu YL. A review of accelerometry-based wearable motion detectors for physical activity monitoring. Sensors. 2010;10(8):7772-7788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Heesch KC, Hill RL, Aguilar-Farias N, van Uffelen JGZ, Pavey T. Validity of objective methods for measuring sedentary behaviour in older adults: a systematic review. Int J Behav Nutr Phys Act. 2018;15(1):119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Winkler EA, Gardiner PA, Clark BK, Matthews CE, Owen N, Healy GN. Identifying sedentary time using automated estimates of accelerometer wear time. Br J Sports Med. 2012;46(6):436-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Choi L, Ward SC, Schnelle JF, Buchowski MS. Assessment of wear/nonwear time classification algorithms for triaxial accelerometer. Med Sci Sports Exerc. 2012;44(10):2009-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]