Abstract
Posterior shoulder instability (PSI) is a shoulder pathology that is challenging to diagnose, leading to treatment delay and exacerbation of symptoms. Etiology can be both traumatic and atraumatic, and a comprehensive clinical history plays a significant role in achieving diagnosis. Imaging in the setting of PSI can reveal a reverse-Bankart lesion, a reverse Hill-Sachs lesion, posterior labral cysts, and potentially glenoid or lesser tuberosity fractures. Both conservative and surgical options exist for patients with PSI, and management often depends on case severity, extent of bone loss, and patient goals and expectations. Holistic patient education regarding the etiologies, mechanisms and possible treatment options available is pivotal for achieving high levels of patient satisfaction and optimal outcomes.
Key Words: Dislocation, Posterior instability, Reverse bankart, Reverse hill-sachs, Shoulder
Introduction
Posterior shoulder instability (PSI) is a complex and increasingly relevant condition with a variety of proposed mechanisms and treatment options. PSI is relatively rare, accounting for less than 4% of all unstable shoulders,1 and can be a challenging clinical diagnosis to make as patients typically present with vague complaints of pain and functional limitation. As such, PSI often goes unrecognized. A systematic review by Xu et al. reported that 73.2% of patients had the initial diagnosis missed.1
Numerous risk factors predispose to PSI, including bony abnormalities, ligamentous laxity, and disruptions in the stability of the glenohumeral joint.2 The incidence of PSI is also higher in individuals engaging in vigorous physical activities, such as military personnel, weightlifters, overhead athletes, and athletes who play contact sports like American football and rugby.2 In one study of 311 shoulder instability patients with a military background, 30% had anterior instability, 24% had PSI, and 44% had both.3 Moreover, the incidence of PSI is higher in males and the younger population. In specific, PSI was 8 times more common in males than females, and the incidence for both sexes showed to be the highest between the ages of 14 and 19, persisting to the 4th decade of life.4
The management of PSI encompasses a wide range of interventions, ranging from conservative measures like physical therapy to more invasive approaches, including arthroscopic or open shoulder surgery.5-9 Thus, the purpose of this study is to investigate the prevalence of PSI, elucidate the mechanisms of injury and diagnosis, and discuss pertinent treatment modalities and interventions based on the reported clinical outcomes.
Main body
Mechanisms and Associated Lesions
As the shallow and flat glenoid cavity allows for the increased range of motion and mobility of the glenohumeral joint, there is an increased risk of instability and dislocation.10 PSI can result from multiple mechanisms, such as acute traumatic events, repetitive microtrauma, and atraumatic events.2 The most common cause of recurrent PSI is repetitive microtrauma in the posteroinferior region of the shoulder that accumulates over time.11 Overhead activities, such as baseball, tennis swimming, and overhead weightlifting, can result in repetitive minor injuries in the position of flexion, internal rotation, and adduction. Blocking techniques in American football, repetitive bench-pressing, acute trauma to the anterior shoulder, and axial loads with the shoulder in internal rotation and flexion, which can be seen in contact athletes, are also associated causes.2,11,12 Additionally, PSI can be caused by hyperabduction, traction, and rotation. In a case report of a patient who experienced a humeral avulsion of the inferior glenohumeral ligament (HAGL), the patient had PSI.13 HAGL lesions are more commonly associated with anterior instability; however, cases of posterior lesions have been described as well.13,14 Moreover, PSI can occur after seizures secondary to traumatic falls or unbalanced muscle contraction.15 During seizure activity, the internal rotators overpower the external rotators, forcing the humerus into a position of flexion, internal rotation, and adduction.16 A similar imbalance of contraction forces around the shoulder joint can be seen after an electric shock, which can cause PSI.17
There are numerous lesions associated with PSI, such as reverse Bankart lesions, reverse Hill-Sachs, posterior labral cysts, posterior glenoid rim fracture, lesser tuberosity fracture, and a large capsular pouch. A reverse Bankart lesion is characterized by the detachment of the capsulolabral complex in the posteroinferior region.11 A reverse Hill-Sachs lesion is a fracture of the anteromedial portion of the humeral head, which can occur after a posterior shoulder dislocation.18 Posterior labral cysts and posterior glenoid rim fractures are often associated with chronic reverse Bankart lesions.11 Paralabral cysts resulting from tears in the posterosuperior labrum can result in pain and external rotation weakness for the patient.19 Further, a large capsular pouch is often associated with chronic posterior instability.11 A lesser tuberosity (LT) fracture may be caused by an acute trauma or after repetitive stress from excessive overhead use of the arm.20 LT fractures are associated with an acute posterior dislocation.11 As the LT is important for stability, a fracture LT may also result in shoulder dislocation.
Presentation and Imaging
Injuries associated with PSI can involve multiple structures, such as the bones, ligaments, or the rotator cuff.21 PSI can present with variable symptoms that are often nonspecific and subtle, which can make PSI difficult to recognize.22 Symptoms intensify with the arm in a vulnerable position of 90° flexion, adduction, and internal rotation.23 Patients often describe a deep, aching pain in the posterior shoulder as well as a clicking or popping sensation.22,23 Range of motion, strength testing, and neurovascular examination may be unaffected and normal, and both shoulders should be compared in order to detect differences between sides.22 Palpation is important as tenderness over the posterior joint line might be due to synovitis resulting from multiple episodes of instability.22
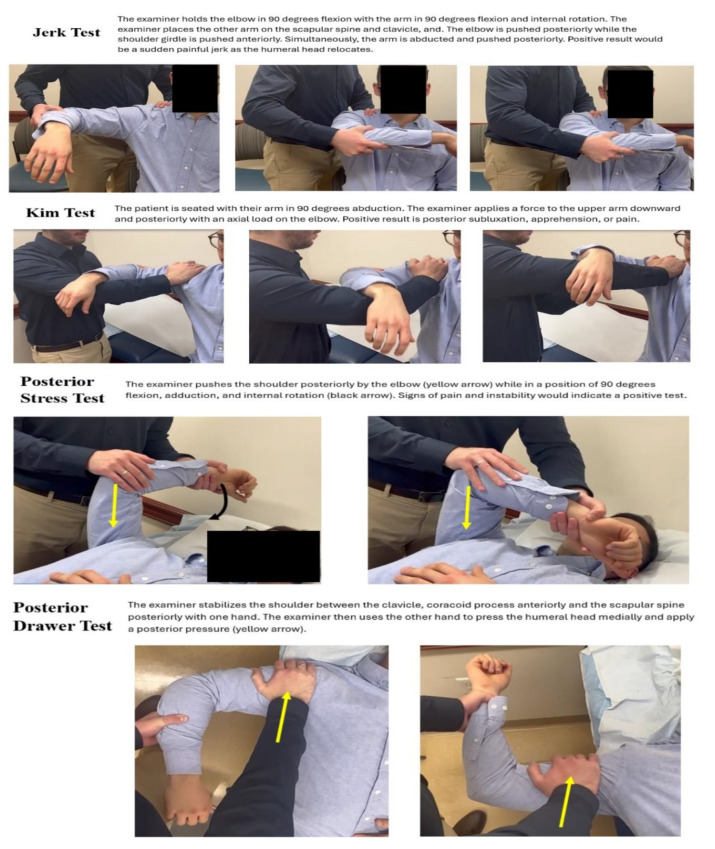
Physical exam maneuvers that can be utilized to test for PSI include the jerk test, Kim test, posterior stress test, and the posterior drawer test [Figure 1]. In the jerk test, the examiner will hold the elbow in 90° flexion with the arm in 90° flexion and internal rotation. The examiner will place another hand on the scapular spine and clavicle. While pushing anteriorly on the shoulder girdle, the elbow will be pushed posteriorly simultaneously while abducting the arm as it is pushed posteriorly. As the humeral head relocates, a positive test result would be a sudden painful jerk [Figure 1].23 In the Kim Test, the patient will be in the seated position with the arm in 90° abduction. Then, the examiner will apply a force to the upper arm downward and posteriorly with an axial load to the elbow. If there is posterior subluxation with pain during the Kim test, the result is positive for PSI [Figure 1].23 In the posterior stress test, the examiner will look for signs of pain and symptoms of instability when the shoulder is pushed posteriorly by the elbow while in a position of 90° flexion, adduction, and internal rotation [Figure 1].23 During the posterior drawer test, the examiner will stabilize the shoulder between the clavicle, coracoid process anteriorly, and the scapular spine posteriorly with one hand. With the other hand, the examiner will press the humeral head medially towards the glenoid, and then a posterior pressure will be applied. Using this maneuver, the neutral position of the joint and the degree of passive translation can be evaluated and determined [Figure 1].23
Figure 1.
Physical exam maneuvers utilized to test for posterior shoulder instability
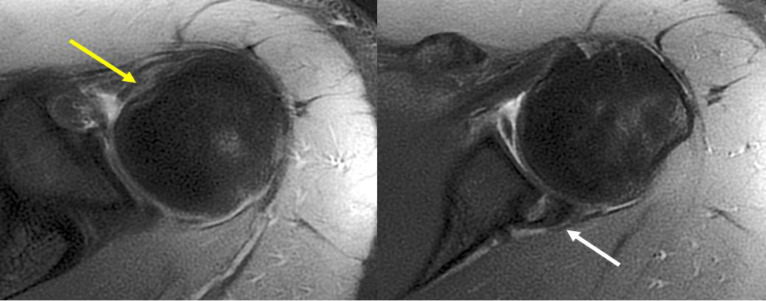
Imaging is an important tool used to diagnose PSI, with different advantages and disadvantages for each modality. Radiographs are able to show osseous lesions of the humerus or glenoid, which allows for posterior bony Bankart lesions and reverse Hill-Sachs lesions to be identified.18 Disadvantages to radiographs are that bone fragments may be rarely seen and soft tissue and ligamentous structures cannot be visualized.18 Computed Tomography (CT) imaging allows for fractures not visible in radiographs to be seen, while also assessing the severity and extent of fractures as well as glenoid and humeral version.22 Severe bone deformities and bone loss can be analyzed on CT.24 Studies have shown that measurements of Hill-Sachs lesions using CT display low inter-examiner reliability; however, there is no universally accepted method to quantify bone loss.25 That being said, Magnetic Resonance Imaging (MRI) remains the ultimate tool and standard of care for assessment of shoulder instability pathologies like posterior capsulolabral complex lesions (reverse Bankart), cartilage damage, tendon tears, reverse Hill-Sachs lesions, and degenerative changes can be identified [Figure 2].22,24
Figure 2.
MRI images (axial view) showing a reverse Hill-Sachs lesion (yellow arrow) and a posterior capsulolabral lesion (white arrow) in a patient with posterior instability due to a prior dislocation event
Interventions and Treatment
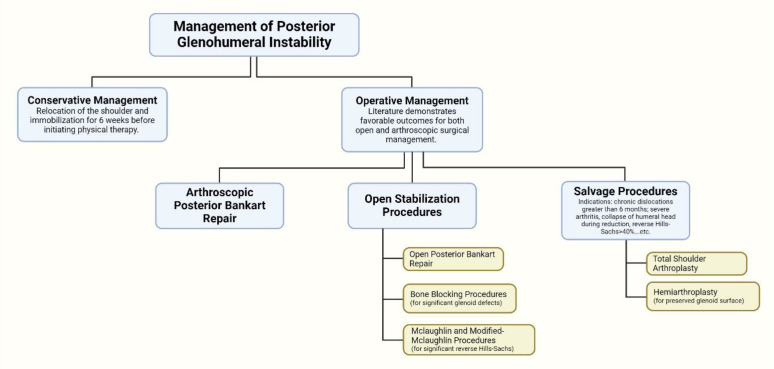
The management of PSI largely depends on a variety of factors including but not limited to the patient’s history and presentation, the degree of severity of the instability, the presence of concomitant lesions, the patient’s quality of life and expectations, and the potential for the failure of conservative treatment [Figure 3]. Conservative management typically consists of relocation of the shoulder, immobilization in a position of 1 to 20 degrees of external rotation, and physical therapy after 6 weeks. The goals of physical therapy include rotator cuff strengthening, periscapular stabilization, and activity modification. Crucially, it was discovered by Burkhead et al. that nonsurgical management in patients with traumatic PSI can result in as low as a 19% success rate.26-29 However, in microtraumatic and atraumatic PSI, the rate of recovery can range anywhere from 70-90%.26-29
Figure 3.
Management options for posterior glenohumeral instability
The array of surgical procedures that are available to shoulder surgeons for posterior instability include arthroscopic or open posterior Bankart repair, bone-blocking procedures, the Mclaughlin/modified Mclaughlin surgeries, and the hemi or total shoulder arthroplasty [Figure 3]. The literature demonstrates favorable outcomes for both open and arthroscopic surgical management. The approach better suited for the patient will depend on the presentation as well as the expectation and risk of recurrence. In one study looking at 31 shoulders that underwent posterior stabilization with either arthroscopic or open procedures, the arthroscopic surgery group did significantly better on patient-reported outcome measures, such as the Single Assessment Numeric Evaluation (SANE), Rowe, Simple Shoulder Test (SST), and Western Ontario and McMaster University Osteoarthritis index (WOMAC) scores.30 Although, Twenty-nine of 31 shoulders were rated as excellent or good by patients.30 Vopat et al. conducted a systematic review looking at 39 studies, including 2077 patients with both anterior and posterior shoulder instability who underwent arthroscopic Bankart repair.31 Patients with anterior instability were more likely to return to sport and had better post-op ASES scores when compared to those with posterior instability, but they were also more likely to have postoperative instability.31 There were no significant differences in the rates of complications.31
Bone-blocking procedures are typically reserved for more complex cases including glenoid retroversion of 10 to 25 degrees, critical glenoid defects, and persistent instability. Graft options include iliac crest, distal tibial allografts (DTA), and others.32 One study looked at seven J-shaped iliac crest autografts in patients with atraumatic posterior instability.33 Four out of seven patients reported posterior apprehension, with the Subjective Shoulder Value (SSV) score increasing from a median of 40% to 90%, the Constant score increasing from a median of 7 to 15, retroversion correcting from 16 to 0 degrees, and CT images displaying union in all J-grafts.33 Schwartz et al. conducted 19 arthroscopic bone blocks using iliac crest autografts in patients with PSI.34 In these patients, the mean Rowe score improved from 18.4 to 82.1, and the Walch-Duplay score improved from 37.4 to 82.9.34 All patients demonstrated radiologic bone healing, with nine able to return to their previous level of sport, three having persistent pain, and two having revisions.34 The Mclaughlin and Modified Mclaughlin procedures, similar to the Remplissage, are also options with indications that include a chronic locked posterior dislocation of less than 6 months or a significant reverse Hill-Sachs.35 The outcomes have been good in the literature with one retrospective clinical study looking at the Mclaughlin procedure demonstrating an average forward flexion increase of 120 degrees, a 27-point increase in the median UCLA score, and a 41-point increase in the Oxford instability score.35
Arthroplasty is largely reserved as a salvage procedure or last resort in patients with PSI, especially as these patients are typically young [Figure 3].36 Indications for a hemiarthroplasty include collapse of the humeral head during reduction, chronic dislocation of greater than 6 months, severe humeral head arthritis, and a reverse Hill-Sachs > 40%. Indications for an anatomic total shoulder arthroplasty are similar to that of the hemiarthroplasty, but include severe arthritis impacting the glenoid.
Conclusion
PSI is a challenging condition to diagnose and treat as symptoms may not be specific, which can delay treatment and increase the severity. It is important for the surgeon to remain vigilant and be comprehensive when examining the presenting patient. Taking a full history, including details about demographics, injury mechanisms, pain patterns, and sports participation, and conducting a holistic physical exam, can be pivotal in directing the surgeon towards the diagnosis. Imaging can be very important in confirming the injury, assessing the degree of bone loss, and diagnosing other associated lesions, such as reverse-Bankart and reverse Hill-Sachs lesions. Treatment options for PSI can be conservative and surgical, and choosing the appropriate management option varies according to severity of injury, degree of bone loss, and patient expectations. It is of pivotal importance to educate patients on all the treatment options available and provide them with insights on the strengths and limitations of the different procedures, as this will help set appropriate therapeutic goals and expectations, and optimize patient outcomes.
Acknowledgment
N/A
Authors Contribution:
AK, MYF, PB, JK, and RDL were responsible for writing, validation, and literature review. JAA was responsible for supervising the project and revising the manuscript.
Declaration of Conflict of Interest:
JAA would like to disclose: Royalties from a company or supplier; Disclosures; OSTEOCENTRIC TECHNOLOGIES, ENOVIS, ZIMMER-BIOMET, STRYKER, GLOBUS MEDICAL, INC. Stocks in: SHOULDER JAM, AEVUMED, OBERD, OTS MEDICAL, ORTHOBULLETS, ATREON, RESTORE 3D. Research support from a company or supplier as a PI; Disclosures; ENOVIS, ARTHREX. Royalties, financial or material support from publishers; Disclosures; WOLTERS KLUWER, SLACK ORTHOPAEDICS, ELSEVIER. Board member/committee appointments for a society; Disclosures; AMERICAN SHOULDER AND ELBOW SOCIETY, MID ATLANTIC SHOULDER AND ELBOW SOCIETY, SHOULDER 360, PACIRA.
Declaration of Funding:
The author(s) received NO financial support for the preparation, research, authorship, and publication of this manuscript.
Declaration of Ethical Approval for Study:
N/A
Declaration of Informed Consent:
The authors declare there is no information (names, initials, hospital identification numbers, or photographs) in the submitted manuscript that can be used to identify patients.
References
- 1.Xu W, Huang L-X, Guo JJ, Jiang D-H, Zhang Y, Yang H-L. Neglected posterior dislocation of the shoulder: A systematic literature review. J Orthop Translat. 2015;3(2):89–94. doi: 10.1016/j.jot.2015.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Doehrmann R, Frush TJ. Posterior shoulder instability. 1st ed. Treasure Island (FL): StatPearls Publishing; 2024. [PubMed] [Google Scholar]
- 3.Swan ER, Lynch TB, Sheean AJ, Schmitz MR, Dickens JF, Patzkowski JC. High Incidence of Combined and Posterior Labral Tears in Military Patients with Operative Shoulder Instability. Am J Sports Med. 2022;50(6):1529–1533. doi: 10.1177/03635465221078609. [DOI] [PubMed] [Google Scholar]
- 4.Woodmass JM, Lee J, Wu IT, et al. Incidence of posterior shoulder instability and trends in surgical reconstruction: a 22-year population-based study. J Shoulder Elbow Surg. 2019;28(4):611–616. doi: 10.1016/j.jse.2018.08.046. [DOI] [PubMed] [Google Scholar]
- 5.Dimock R, Memon K, Consigliere P, Polyzois I, Imam MA, Narvani A. Posterior Shoulder Instability: The Augmented McLaughlin Procedure. Arch Bone Jt Surg. 2020;8(6):729–733. doi: 10.22038/abjs.2020.44481.2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alkaduhimi H, Hilgersom NFJ, Eygendaal D, van den Bekerom MPJ, Oh L. The Outcomes of Soft-Tissue Repair for Posterior Shoulder Instability Surgery. Arch Bone Jt Surg. 2022;10(1):45–51. doi: 10.22038/ABJS.2021.41491.2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Castropil W, Mauad JR, Amorim FHB. Arthroscopic Coracoid Bone Block for Posterior Glenohumeral Instability: Description of Surgical Technique and a Case Report. Arch Bone Jt Surg. 2023;11(9):591–594. doi: 10.22038/ABJS.2023.71320.3334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bitar AC, Medina G, Ribas L, Smid J, Adoni T. Arthroscopic Reverse Remplissage in a Bilateral Seizure-related Posterior Shoulder Dislocation: Technique Description and 3-Year Follow-up Case Report. Arch Bone Jt Surg. 2021;9(3):350–354. doi: 10.22038/abjs.2020.49649.2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Festbaum C, Minkus M, Akgün D, et al. Conservative treatment of acute traumatic posterior shoulder dislocations (Type A) is a viable option especially in patients with centred joint, low gamma angle, and middle or old age. Knee Surg Sports Traumatol Arthrosc. 2022;30(7):2500–2509. doi: 10.1007/s00167-022-06883-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kammel KR, El Bitar Y, Leber EH. Posterior shoulder dislocations. 1st ed. Treasure Island (FL): StatPearls Publishing; 2024. [PubMed] [Google Scholar]
- 11.Provencher MT, LeClere LE, King S, et al. Posterior instability of the shoulder: diagnosis and management. Am J Sports Med. 2011;39(4):874–86. doi: 10.1177/0363546510384232. [DOI] [PubMed] [Google Scholar]
- 12.Robinson CM, Aderinto J. Recurrent Posterior Shoulder Instability. J Bone Joint Surg Am. 2005;87(4):883–92. doi: 10.2106/JBJS.D.02906. [DOI] [PubMed] [Google Scholar]
- 13.Maalouly J, Aouad D, Ayoubi R, Dib N, El Rassi G. Posterior shoulder instability due to isolated reverse HAGL lesion in a young gymnast: A rare mechanism of injury and surgical technique. Trauma Case Rep. 2020;28:100312. doi: 10.1016/j.tcr.2020.100312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.George MS, Khazzam M, Kuhn JE. Humeral Avulsion of Glenohumeral Ligaments. J Am Acad Orthop Surg. 2011;19(3):127–33. doi: 10.5435/00124635-201103000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Betz ME, Traub SJ. Bilateral posterior shoulder dislocations following seizure. Intern Emerg Med. 2007;2(1):63–5. doi: 10.1007/s11739-007-0017-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Atwan Y, Wang A, Labrum JTt, et al. Management of Shoulder Instability in Patients with Seizure Disorders. Curr Rev Musculoskelet Med. 2023;16(5):201–210. doi: 10.1007/s12178-023-09833-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nie J, Jin M, Fang T, Li J. [Bilateral posterior shoulder dislocation with associated reverse Hill-Sachs lesions after electrical injury] Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi. 2022;40(7):527–529. doi: 10.3760/cma.j.cn121094-20210311-00137. [DOI] [PubMed] [Google Scholar]
- 18.Ippolito G, Zitiello M, De Marinis G, et al. Posterior Shoulder Dislocation with Engaging Reverse Hill-Sachs Lesion: A Retrospective Study of Ten Patients Treated with Arthroscopy or Open Reduction and Stabilization. J Clin Med. 2021;10(7):1410. doi: 10.3390/jcm10071410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tuite MJ, Pfirrmann CW. Shoulder: instability. In: Hodler J, editor. Musculoskeletal Diseases 2021-2024: Diagnostic Imaging. 1th ed. Cham (CH): Springer; 2021. [PubMed] [Google Scholar]
- 20.Spek RWA, Schoolmeesters BJA, den Haan C, Jaarsma RL, Doornberg JN, van den Bekerom MPJ. What are the patient-reported outcomes, functional limitations, and complications after lesser tuberosity fractures? A systematic review of 172 patients. JSES Int. 2021;5(4):754–764. doi: 10.1016/j.jseint.2021.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jana M, Gamanagatti S. Magnetic resonance imaging in glenohumeral instability. World J Radiol. 2011;3(9):224–32. doi: 10.4329/wjr.v3.i9.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ruiz Santiago F, Martínez Martínez A, Tomás Muñoz P, Pozo Sánchez J, Pérez AZ. Imaging of shoulder instability. Quant Imaging Med Surg. 2017;7(4):422–433. doi: 10.21037/qims.2017.08.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tannenbaum E, Sekiya JK. Evaluation and management of posterior shoulder instability. Sports Health. 2011;3(3):253–63. doi: 10.1177/1941738111400562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moroder P, Scheibel M. ABC classification of posterior shoulder instability. Obere Extrem. 2017;12(2):66–74. doi: 10.1007/s11678-017-0404-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kodali P, Jones MH, Polster J, Miniaci A, Fening SD. Accuracy of measurement of Hill-Sachs lesions with computed tomography. J Shoulder Elbow Surg. . 2011;20(8):1328–34. doi: 10.1016/j.jse.2011.01.030. [DOI] [PubMed] [Google Scholar]
- 26.Burkhead WZ, Rockwood CA. Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg Am. . 1992;74(6):890–6. [PubMed] [Google Scholar]
- 27.Fronek J, Warren RF, Bowen M. Posterior subluxation of the glenohumeral joint. J Bone Joint Surg Am. 1989;71(2):205–16. [PubMed] [Google Scholar]
- 28.Lanzi JT, Chandler PJ, Cameron KL, Bader JM, Owens BD. Epidemiology of Posterior Glenohumeral Instability in a Young Athletic Population. Am J Sports Med. 2017;45(14):3315–3321. doi: 10.1177/0363546517725067. [DOI] [PubMed] [Google Scholar]
- 29.Sadi J, Torchia E, Faber KJ, et al. Posterior Shoulder Instability Classification, Assessment, and Management: An International Delphi Study. J Orthop Sports Phys Ther. 2020;50(7):373–380. doi: 10.2519/jospt.2020.9225. [DOI] [PubMed] [Google Scholar]
- 30.Bottoni CR, Franks BR, Moore JH, DeBerardino TM, Taylor DC, Arciero RA. Operative Stabilization of Posterior Shoulder Instability. Am J Sports Med. . 2005;33(7):996–1002. doi: 10.1177/0363546504271509. [DOI] [PubMed] [Google Scholar]
- 31.Vopat ML, Coda RG, Giusti NE, et al. Differences in Outcomes Between Anterior and Posterior Shoulder Instability After Arthroscopic Bankart Repair: A Systematic Review and Meta-analysis. Orthop J Sports Med. . 2021;9(5):23259671211006437. doi: 10.1177/23259671211006437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fares MY, Boufadel P, Daher M, Koa J, Khanna A, Abboud JA. Anterior shoulder instability and open procedures: history, indications, and clinical outcomes. Clin Orthop Surg. 2023;15(4):521–533. doi: 10.4055/cios23018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ernstbrunner L, Häller T, Waltenspül M, Wieser K, Gerber C. Posterior open-wedge osteotomy and glenoid concavity reconstruction using an implant-free, J-shaped iliac crest bone graft in atraumatic posterior instability with pathologic glenoid retroversion and dysplasia: a preliminary report. Clin Orthop Relat Res. 2021;479(9):1995–2005. doi: 10.1097/CORR.0000000000001757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schwartz DG, Goebel S, Piper KJ, Kordasiewicz B, Boyle S, Lafosse L. Arthroscopic Posterior Bone Block Augmentation in Posterior Shoulder Instability. J Shoulder Elbow Surg. 2013;22(8):1092–101. doi: 10.1016/j.jse.2012.09.011. [DOI] [PubMed] [Google Scholar]
- 35.Brilakis E, Malahias M-A, Patramani M, et al. All-Arthroscopic McLaughlin's Procedure in Patients with Reverse Hill-Sachs Lesion Caused by Locked Posterior Shoulder Dislocation. Joints. 2019;7(3):71–77. doi: 10.1055/s-0039-3401820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sperling JW, Pring M, Antuna SA, Cofield RH. Shoulder arthroplasty for locked posterior dislocation of the shoulder. J Shoulder Elbow Surg. 2004;13(5):522–7. doi: 10.1016/j.jse.2004.02.012. [DOI] [PubMed] [Google Scholar]