Abstract
BACKGROUND
Low-velocity penetrating brain injury (PBI) is an uncommon variant of traumatic brain injury (TBI). Patients affected by PBI can present with highly variable injury patterns, which, along with guideline-directed TBI care, may require the employment of unique operative management strategies. There are no strict guidelines for the management of low-velocity penetrating injuries. Characterizing approaches and outcomes for various injury patterns may be of use in guiding surgical decision-making. The authors report their experience with two cases of PBI by mechanism of a nail gun with a retained intracranial foreign body requiring surgical removal.
OBSERVATIONS
The two patients were managed using different operative approaches with directly visualized nail removal, and both cases were managed with different empiric antibiotic regimens. Both patients were neurologically intact at follow-up and had no perioperative complications.
LESSONS
These cases illustrate two methods of foreign body removal and the perioperative management protocol utilized at the authors’ institution.
Keywords: penetrating brain injury, intracranial foreign body, traumatic brain injury, nail gun injury
ABBREVIATIONS: CT = computed tomography, CTA = CT angiography, ICU = intensive care unit, IV = intravenous, MRA = magnetic resonance angiography, OR = operating room, PBI = penetrating brain injury, TBI = traumatic brain injury.
Traumatic brain injury (TBI) is a frequent diagnosis in the neurosurgical field, but penetrating brain injuries (PBIs) are far less common. PBIs can be classified based on the velocity of the offending projectile or object. A velocity threshold of 100 m/sec has been proposed to differentiate between high- and low-velocity PBIs.1 Low-velocity PBIs (e.g., nails, hammers, knives, and pencils) are a rarer presenting diagnosis, comprising only 0.4% of all head trauma.2 The most common reported causes of these injuries are accidents, violence, and suicide attempts. Low-velocity PBIs typically require surgical intervention and can have favorable patient outcomes.3
Illustrative Cases
Case 1
A 45-year-old male presented to the emergency department from an outside facility for further evaluation of a TBI with a retained intracranial foreign body. The patient was climbing down a ladder at a roofing construction site, and a nail gun impacted his cranium, driving a nail into the intracranial space. He reported light-headedness and dizziness without loss of consciousness. On neurological examination, he was awake, alert, and oriented to self and location. He exhibited a left lower facial droop with no additional focal deficits.
A computed tomography (CT) scan of the head (Fig. 1) demonstrated a 7.5 cm nail with entry into the right parietal bone, approximately 1 cm posterior to the coronal suture and 5 cm to the right of the midline. The nail traversed the superior frontal convexity anteriorly and medially, terminating in the right temporal stem. It did not appear to violate the sylvian fissure. There were small-volume acute blood products surrounding the nail track without any large intraparenchymal hematoma. CT angiography (CTA) of the head and neck demonstrated no acute vascular injury. The patient was given a dose of intravenous (IV) vancomycin, ceftriaxone, and metronidazole, as well as 1 g of IV levetiracetam.
FIG. 1.
Case 1. Coronal CT scan of the head without contrast demonstrates the 7.5 cm nail with entry into the right parietal bone, approximately 1 cm posterior to the coronal suture and 5 cm to the right of the midline, with scant hemorrhage along the nail track.
He was then taken to the operating room (OR) for removal of the nail. Endotracheal general anesthesia was induced in a standard fashion, and an arterial line was placed for continuous blood pressure monitoring. The patient was placed supine with the head turned to expose the right side. A small puncture wound was noted on the scalp. The nail was not visible externally. A lazy S incision was planned, centered over the nail entry point. After sterile preparation and draping, the skin was incised sharply, and scalp dissection was performed with Bovie cautery. Self-retaining retractors were placed, and the nail head was visualized embedded within the parietal bone. A 5-cm × 5-cm circular craniotomy was performed with the nail head at the center to allow enough exposure to access and control in the event of bleeding during nail removal. A smaller circular craniectomy, 1.5 cm in diameter, centered over the embedded nail head was performed to isolate the nail from the larger craniotomy (Fig. 2). This was done to allow controlled removal of the surrounding bone flap without disturbing the nail. Once the craniotomy bone flap was removed, the field was inspected. There was congealed epidural hematoma that was evacuated with irrigation and aspiration. A cruciate durotomy was made for exposure and inspection of the underlying cerebral cortex. There were focal subarachnoid blood products adjacent to the entry of the nail, without any active hemorrhage appreciated. The nail was found to be highly mobile. The penetrating site at the cerebral cortex was gently retracted with a Penfield dissector, and irrigation was applied down the track to decrease the frictional forces of the nail shank on adjacent parenchyma upon removal. Gentle traction with forceps was then applied to the nail head along the longitudinal axis to remove the nail. We then inspected and irrigated the penetrating track with no signs of active hemorrhage. We waited for 5 minutes with no interval cerebral swelling or herniation of the exposed brain matter through the craniectomy defect. We then inspected the penetrating track again using gentle retraction with Penfield dissectors, and still no active hemorrhage was noted. The field was irrigated thoroughly, and devitalized bone fragments were removed to decrease infection risk. At this point, closure was performed in a standard fashion. The OR was left sterile, and the patient remained intubated. The patient was transported for a CT scan immediately, which revealed small track site blood products without underlying hematoma. The patient was then transported to the intensive care unit (ICU) for postoperative care. The patient was extubated the following day. He was awake, alert, and fully oriented, with stable left lower facial droop and no new focal deficits. The patient received a 7-day course of IV vancomycin, ceftriaxone, and metronidazole, followed by a 2-week course of oral clindamycin. Levetiracetam was continued. He worked with physical therapy throughout his hospital stay and was discharged home on postoperative day 8. At follow-up on postoperative day 16, his facial droop had resolved.
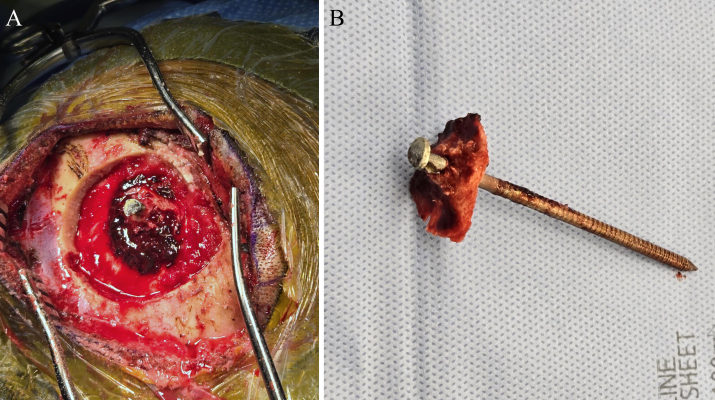
FIG. 2.
Case 1. A: Intraoperative photograph demonstrating the retained nail and surrounding bone left after turning a small and a larger surrounding craniotomy to allow for adequate exposure and visualization prior to nail removal in the event of significant hemorrhage. Upon nail removal, no significant hemorrhage was encountered, but this method showcases how excellent exposure can be obtained prior to nail removal in the event that parenchymal exposure and exploration are warranted. B: Postoperative photograph of the removed nail, with the bone island still attached.
Case 2
A 27-year-old male with a history of bipolar disorder and congenital hydrocephalus presented to the emergency department after sustaining a nail gun injury to the head. The patient reported that he was working on a house using a nail gun when he tripped over the cord and the nail gun went off multiple times, causing three nails to strike him in the head. He denied loss of consciousness. On neurological examination, the patient demonstrated no focal deficits. His only subjective complaint was of headache. Despite a history of prior suicide attempts, the patient denied any current suicidal ideation.
A CT scan of the head was obtained (Fig. 3), which revealed three nails: one penetrating through the right parietal bone into the brain parenchyma and another penetrating the left frontal bone into the brain parenchyma. There was associated right parietal and left frontal subarachnoid hemorrhage with no large hematoma. The third nail penetrated the midline of the frontal bone, approximately 3 cm anterior to the coronal suture, but did not breach the inner cortex. CTA of the head and neck did not demonstrate any acute vascular injury. The patient was started on IV antibiotic coverage with vancomycin, ceftriaxone, and metronidazole. The course was maintained for 7 days. He was also given Keppra 1 g IV twice daily for seizure prophylaxis.
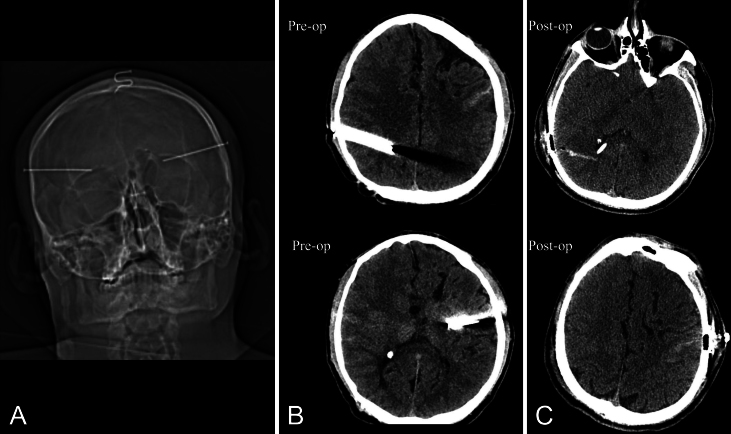
FIG. 3.
Case 2. Preoperative CT scout view (A) without contrast demonstrating biparietal nails violating the calvaria and the midline frontal nail suspended in the scalp but without violating bone. Preoperative CT images (B) compared to postoperative CT images (C) show scant residual hemorrhage within the nail tracks.
The patient was taken to the OR for removal of the nails. He was placed under general anesthesia, and an arterial line was placed for continuous blood pressure monitoring. He was placed supine, and the entire head was shaved with an electric razor. Three separate incisions were planned, and the patient was prepped and draped in a sterile fashion. A linear incision was created to incorporate the entry point of the midline frontal nail. The skin was opened sharply and dissected with electrocautery. A rongeur was used to remove the midline frontal nail from the skull. The nail appeared intact on removal. The wound was copiously irrigated with chlorhexidine-containing irrigation and vancomycin-containing saline solution. Next, curvilinear incisions were made over the entry points of the left frontal nail and right parietal nail. Temporalis fascia and muscle were divided, and the nail heads were identified protruding from the outer table. Self-retaining retractors were placed, and burr holes were created approximately 2 cm next to the protruding nails, and small 1.5- to 2-cm craniectomies were turned around each of the nails. The nails were then gently removed together with the bone in which they were anchored. Of note, during manipulation of the right nail, bradycardia with a heart rate down to around 30 bpm with no hypotension was noted. This resolved spontaneously within a few seconds after nail removal was completed. The nail tracks and field were copiously irrigated, and titanium plates and screws were used to cover the small craniectomy defects. The scalp was sharply debrided at the nail entry points until healthy bleeding tissue was encountered. The patient was extubated postprocedure, and a postoperative CT of the head demonstrated complete removal of the nails with minimal blood products along the nail tracks. The patient was monitored in the ICU overnight and maintained a nonfocal examination. He was discharged home after a 5-day course of triple-antibiotic coverage and completed 7 days of 1 g twice daily Keppra for seizure prophylaxis. He returned to the clinic 2 weeks later for follow-up and was doing well at that time, with no complaints, and his incisions were healing well.
Informed Consent
The necessary informed consent was obtained in this study.
Discussion
Given the low incidence and wide variability based on injury location of low-velocity PBIs, there are no strict guidelines for workup and management. There is a general consensus that the initial workup should include a CT scan of the head to assess for intraparenchymal hematoma and vascular imaging, such as CTA, to assess for vascular injury.4, 5 Antibiotics and anticonvulsants are generally used for initial management.4 Antibiotic prophylaxis typically includes a broad-spectrum regimen, but the exact regimen and duration of use vary.1, 4 Most neurosurgeons include the use of a cephalosporin and an average duration of up to 10 days,4 though some extend the antibiotic duration further. For our first case, we employed an aggressive IV broad-spectrum multidrug antibiotic regimen while the patient was an inpatient, followed by broad-spectrum single-agent therapy for 2 weeks thereafter. For our second case, the patient was managed with 5 days of an aggressive IV broad-spectrum regimen with no outpatient or prolonged course of antibiotics. The cases were performed by different surgeons, showcasing the regimen variability, even within a single institution.
The indications for surgical intervention in cases of PBI have been described as a retained foreign object, presence of dural defects, displaced bone fractures, intracranial hematoma, and evidence of direct vascular injury.5 Both of our patients met operative criteria by the first two indications.
The neurological outcome for PBI appears to be more related to the extent of the initial injury, with surgical intervention indicated to prevent secondary complications.1 Complete skull violation with intracranial penetration of a nail has been associated with lower survival rates than incomplete penetration.6 While one goal of surgery is to remove the foreign object, some nail trajectories involve vital structures and removal can pose a risk of further injury. Luo et al. describe a case with intracranial penetration by a nail traversing the left internal capsule into the temporal lobe adjacent to the brainstem in which surgical debridement, irrigation, and closure were performed with the nail left in place.6 This patient had no signs of infection or epilepsy at the 2-year follow-up. Thus, leaving a nail in place can be considered if it is thought that removal poses significant risk.
One potential surgical complication after removal of an intracranial nail is intraparenchymal hematoma. Adequate surgical exposure should be performed to provide quick access to explore and control bleeding; nail removal under direct visualization as opposed to blind removal yields an improved mortality rate, which is already favorable among nail gun PBIs versus ballistic injuries, which are much more prevalent.7 The use of intraoperative endoscopy or ultrasound can be considered as ancillary tools to inspect for underlying hematomas not directly visualized at the level of the cortex. We also favor immediate postoperative CT imaging for early screening of operative complications that may warrant a return to the OR.
These cases did not involve vascular injury; however, vascular injuries occur in 3%–20% of all cases of craniocervical trauma.8 Traumatic vascular injuries in the head include dissection, intramural hematoma formation, pseudoaneurysm formation, arteriovenous fistula formation, occlusion, and extravasation. The most worrisome vascular complication from penetrating head trauma is pseudoaneurysm formation, which is also the most common; the incidence of pseudoaneurysm formation after penetrating head trauma has been reported to be as high as 20%–50%.9–11
These lesions can present in a delayed fashion, and rupture risk is highest for untreated traumatic pseudoaneurysms in the first 1–3 weeks after injury, with mortality rates reaching up to 50% with rupture; hence, serial vascular imaging should be performed if there is an underlying suspicion for this despite negative initial imaging.10, 12 Pseudoaneurysm formation can occur within 2 hours after injury and most frequently occurs in the anterior circulation on distal middle cerebral artery branches.13 Posterior circulation pseudoaneurysm formation after penetrating trauma is rarely described in the literature, most likely because trauma to this location in the head is deadly.13
Patients who present with a PBI should be initially screened for vascular injury with CTA or magnetic resonance angiography (MRA) of the head to rule out vascular injury.8 If intracranial metal fragments are present, MRA is contraindicated. Cerebral angiography is recommended for patients with a concern for vascular injury or those at high risk for vascular injury, including those with a trajectory near the sylvian fissure, supraclinoid carotid artery, vertebrobasilar vessels, cavernous sinus region, or major dural venous sinuses.14
Both open surgical and endovascular methods can be used to treat traumatic vascular injuries in penetrating head trauma. Deconstructive or reconstructive techniques can be used to treat vascular injury. Ultimately, the surgeon must decide on the best form of treatment for the patient.
Observations
We present two cases of low-velocity PBI caused by nail gun injuries. Both patients underwent successful surgical removal of the foreign bodies and were also managed with empiric broad-spectrum antibiotics and antiepileptics. Notably, both patients demonstrated few deficits at presentation and were neurologically afocal at follow-up, underscoring the potential for favorable outcomes in similar cases when timely and appropriate operative intervention is performed. This is consistent with prior reports and a comprehensive review of available case reports and case series, which found that patients with nail gun PBIs who underwent surgical removal of nails under direct visualization had favorable outcomes.7, 15, 16 Despite this, further reporting is needed to guide specific management strategies and better define long-term neurological outcomes and prognosis in these patients.
Lessons
These cases highlight the importance of tailored management for nail gun PBI, including the consideration of the risks and benefits of foreign body removal with respect to the foreign body’s characteristics, location, and involved structures. As discussed, there are instances where it can be safer to leave a foreign object embedded, particularly when removal poses significant risks or could result in high morbidity for the patient. Preoperative planning is key, and anticipation of complications, including track hemorrhage and hematoma, should be accounted for with adequate exposure before removing foreign bodies violating the brain parenchyma. This is especially true for patients with the involvement of vascular structures and deep or eloquent structures. Our cases contribute to the growing body of literature supporting the nuanced approach to treating PBIs, emphasizing the need for careful assessment of each unique situation to optimize patient outcomes with respect to the mechanism of injury and the feasibility of safe foreign body removal. Further research and case documentation will be needed to better determine management strategies for nail gun injuries and other forms of penetrating trauma.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Giles, Smith, Strickland. Acquisition of data: Bowen. Drafting the article: Giles, Bowen, Duran, Smith. Critically revising the article: Giles, Duran, Smith, Strickland. Reviewed submitted version of manuscript: Bowen, Duran, Smith. Approved the final version of the manuscript on behalf of all authors: Giles. Study supervision: Strickland.
Correspondence
Tyler X. Giles: University of Mississippi Medical Center, Jackson, MS. tgiles2@umc.edu.
References
- 1.Awori J, Wilkinson DA, Gemmete JJ, Thompson BG, Chaudhary N, Pandey AS. Penetrating head injury by a nail gun: case report, review of the literature, and management considerations. J Stroke Cerebrovasc Dis. 2017;26(8):e143-e149. [DOI] [PubMed] [Google Scholar]
- 2.de Holanda LF, Pereira BJA, Holanda RR, et al. Neurosurgical management of nonmissile penetrating cranial lesions. World Neurosurg. 2016;90:420-429. [DOI] [PubMed] [Google Scholar]
- 3.Zyck S, Toshkezi G, Krishnamurthy S, et al. Treatment of penetrating nonmissile traumatic brain injury. Case series and review of the literature. World Neurosurg. 2016;91:297-307. [DOI] [PubMed] [Google Scholar]
- 4.Kaufman HH, Schwab K, Salazar AM. A national survey of neurosurgical care for penetrating head injury. Surg Neurol. 1991;36(5):370-377. [DOI] [PubMed] [Google Scholar]
- 5.Schreckinger M, Orringer D, Thompson BG, La Marca F, Sagher O. Transorbital penetrating injury: case series, review of the literature, and proposed management algorithm. J Neurosurg. 2011;114(1):53-61. [DOI] [PubMed] [Google Scholar]
- 6.Luo W, Liu H, Hao S, Zhang Y, Li J, Liu B. Penetrating brain injury caused by nail guns: two case reports and a review of the literature. Brain Inj. 2012;26(13-14):1756-1762. [DOI] [PubMed] [Google Scholar]
- 7.Murray L. Craniocerebral nail gun injuries: a definitive review of the literature. Brain Inj. 2021;35(2):164-172. [DOI] [PubMed] [Google Scholar]
- 8.Patel J, Huynh TJ, Rao D, Brzezicki G. Vascular trauma in the head and neck and endovascular neurointerventional management. J Clin Imaging Sci. 2020;10:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenfeld JV, Bell RS, Armonda R. Current concepts in penetrating and blast injury to the central nervous system. World J Surg. 2015;39(6):1352-1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Larson PS, Reisner A, Morassutti DJ, Abdulhadi B, Harpring JE. Traumatic intracranial aneurysms. Neurosurg Focus. 2000;8(1):e4. [DOI] [PubMed] [Google Scholar]
- 11.Gutiérrez-González R, Boto GR, Rivero-Garvía M, Pérez-Zamarrón A, Gómez G. Penetrating brain injury by drill bit. Clin Neurol Neurosurg. 2008;110(2):207-210. [DOI] [PubMed] [Google Scholar]
- 12.du Trevou MD, van Dellen JR. Penetrating stab wounds to the brain: the timing of angiography in patients presenting with the weapon already removed. Neurosurgery. 1992;31(5):905-912. [DOI] [PubMed] [Google Scholar]
- 13.Haddad FS, Haddad GF, Taha J. Traumatic intracranial aneurysms caused by missiles: their presentation and management. Neurosurgery. 1991;28(1):1-7. [DOI] [PubMed] [Google Scholar]
- 14.Kazim SF, Shamim MS, Tahir MZ, Enam SA, Waheed S. Management of penetrating brain injury. J Emerg Trauma Shock. 2011;4(3):395-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hendricks BK, DiDomenico JD, Lawton MT, Little AS. Unique presentation and novel surgical approach to a transcribriform penetrating head injury caused by a nail gun. Cureus. 2022;14(6):e25581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miki K, Natori Y, Kai Y, Mori M, Yamada T, Noguchi N. How to remove a penetrating intracranial large nail. World Neurosurg. 2019;127:442-445. [DOI] [PubMed] [Google Scholar]