Abstract
Background
This study is aimed to compare the differences in clinical outcomes between the crossed rod configuration and the parallel rod configuration applied in posterior occipitocervical and atlantoaxial fixations, and to assess the clinical applicability of crossed rods.
Methods
From January 2015 to December 2021, 21 patients with craniocervical junction disorders were treated surgically with the crossed rod technique (CR group). Meanwhile, 27 corresponding patients treated with the conventional parallel rod technique were included as control (PR group). Clinical data, internal fixation type, neurological status, clinical symptoms relief, image parameter, complications and bone fusion conditions were retrospectively analyzed and evaluated.
Results
No statistically significant differences were found in baseline characteristics, fixation type and postoperative complications between the two groups. Although the postoperative ADI was significantly reduced in both groups, the ADI was significantly greater in the CR group than that in the PR group after surgery and at the final follow-up (P < 0.05). All patients achieved bone fusion at 1-year postoperative follow-up except for one case in the PR group. However, patients in the CR group had a significantly higher fusion rate than those in the PR group at 3 months postoperatively (P < 0.05).
Conclusions
The application of a crossed rod configuration in posterior occipitocervical and atlantoaxial fixations provides good clinical applicability. Although this technique has a relatively weaker reduction force, it has greater fixation stability and a higher rate of early bone fusion. This technique could be an easy and viable alternative to the current parallel rod configuration for upper cervical surgery.
Keywords: Crossed rod, Parallel rod, Craniocervical junction, Arthrodesis, Internal fixation, Spinal fusion
Introduction
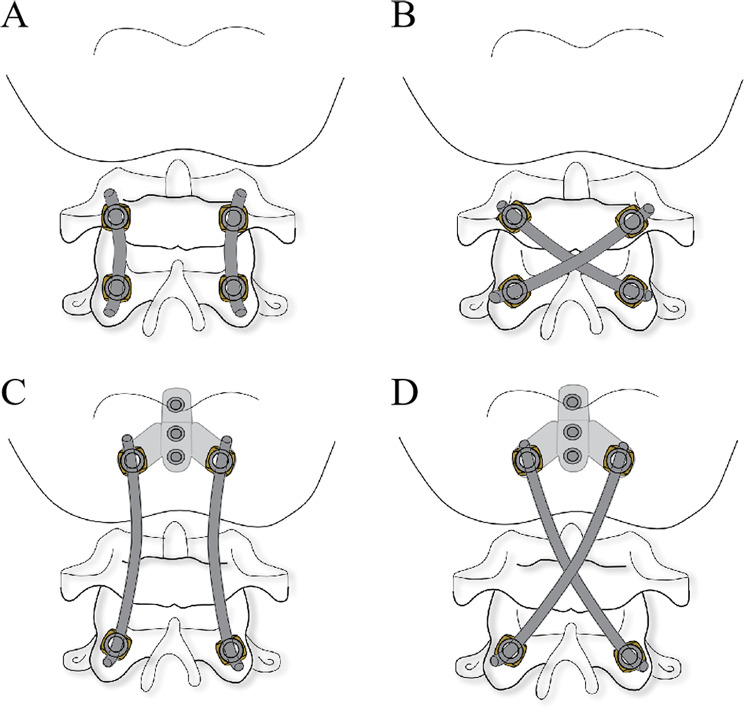
Posterior occipitocervical plate-screw-rod fixations and atlantoaxial screw-rod fixations with the parallel rod configuration are commonly used for craniocervical junction reconstruction [1, 2]. Because the craniocervical junction is particularly active, adding the transverse link is currently the most commonly used method to improve the stability of internal fixation system [3–5]. However, the large bending arc and limited space of the rods increase the difficulty of using transverse links. The novel crossed rod (CR) configuration, with an “X” shape differing from the “II” shape of the traditional parallel rod (PR) configuration (Fig. 1), has been used in some biomechanical studies, with results showing that this configuration provided better stability in comparison to the traditional construct [6–8]. This suggests that the CR configuration may be a viable, simpler method to increase the global stability of posterior occipitocervical and atlantoaxial fixations. Until now, however, the clinical application of this technique has not been studied. In the present study, a retrospective analysis of 48 patients with craniocervical junction disorders treated by posterior occipitocervical or atlantoaxial fixations was performed to assess the clinical outcomes of the CR configuration as well as to compare the differences between this technique and the prevalent PR method.
Fig. 1.
Contrast diagram of crossed rod and parallel rod structure. (A) Atlantoaxial parallel rod fixation (B) Atlantoaxial crossed rod fixation (C) Occipitocervical parallel rod fixation (D) Occipitocervical crossed rod fixation
Materials and methods
Patient characteristics
This study received ethical approval from our hospital’s ethics committee (2024012), and all patients provided informed consent. From January 2015 to December 2021, 21 patients with craniocervical junction disorders were recruited and the CR configuration was applied in all cases (CR group). The detailed screening criteria were (1) diagnosis of craniocervical junction disorders including atlantoaxial dislocation, atlantoaxial fracture, basilar invagination and atlantoaxial intraspinal tumor by clinical and imaging examinations; (2) no previous cervical disease or history of cervical surgery. The exclusion criteria were (1) inability to tolerate surgery, and (2) incomplete follow-up data. Twenty-seven patients with craniocervical junction disorders were treated with the conventional PR configuration during the same period and were included as control (PR group). The CR group contained 11 males and 10 females, while the PR group had 15 men and 12 women. Among 21 patients in the CR group prior to surgery, there were 19 cases with clinical symptoms of occipitocervical pain (90.5%), 13 with numbness of limbs (61.9%), 10 with weakness of limbs (47.6%), and 5 with unsteady gait (23.8%). Of the 27 patients in the PR group, 23 had symptoms of occipitocervical pain (85.2%), 14 had numbness of limbs (51.9%), 12 had weakness of limbs (44.4%) and 6 had unsteady gait (22.2%). Five cases in the CR group and eight cases in the PR group underwent posterior occipitocervical fixation were diagnosed with Basilar invagination combined with Chiari malformation or atlantoaxial dislocation. In the CR group, posterior atlantoaxial fixation was performed in 9 cases with atlantoaxial dislocation, 8 cases with atlantoaxial fracture and 2 case with atlantoaxial intraspinal tumor. In the PR group, posterior atlantoaxial fixation was performed in 11 cases with atlantoaxial dislocation, 9 cases with atlantoaxial fracture and 2 case with atlantoaxial intraspinal tumor. Routine preoperative cervical anteroposterior and lateral X-rays, computed tomography (CT) with three-dimensional reconstruction, and magnetic resonance imaging (MRI) were performed and collected for each case.
Surgical technique and postoperative management
CR fixation method
Under general anesthesia, the patient was placed in a prone position. Skull traction (weighing 3–4 kg) was applied to maintain moderate cervical flexion. A longitudinal posterior midline incision was performed from the occipital to the C2 spinous process. Subperiosteal dissection in both directions was performed to expose the occipital bone, the posterior arch of C1, and the lateral mass of C2. If atlantoaxial fixation was performed, C1 and C2 screws were placed. For C1, a pedicle screw was preferred, but a lateral mass screw was used instead when the C1 posterior arch was too thin and less than 2.0 mm in height. A C2 pedicle screw or a translaminar screw was inserted, with a preference for a pedicle screw. A translaminar screw was used when the placement of a C2 pedicle screw was unsafe due to anatomical variations. If occipitocervical fixation was performed, an occipital plate and C2 screws were implanted. The choice of C2 screw type was consistent with atlantoaxial fixation. Then, two rods of appropriate length were installed with a crossed structure and locked. After cervical alignment and good placement of the internal fixation were confirmed by the intraoperative fluoroscopy, autogenous bone grafting was performed below the rod structure for fusion. A drainage tube was then placed, and the incision was closed in layers.
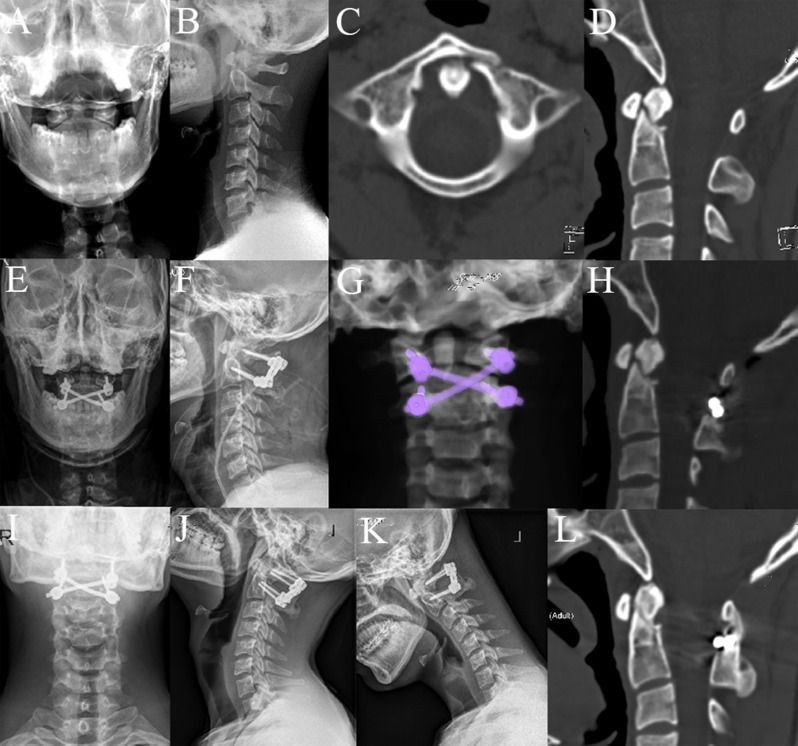
The drainage tube was removed 48 h after surgery. Cervical X-rays and CT scans were obtained 3 days postoperatively to assess the position of the internal fixation for all cases. MRI scans were performed to evaluate spinal cord decompression. Postoperative external immobilization with a rigid cervical collar was performed for 3 months. we generally recommend our patients have follow-up imaging examinations at 3, 6, and 12 months after surgery, and then every 12 months or at times of discomfort. Cervical X-rays and CT scans were performed at each follow-up. Bone fusion was confirmed by continuous bone bridge formation on CT scan (Figs. 2 and 3).
Fig. 2.
A 39-year-old woman diagnosed with basilar invagination and Chiari malformation. A-D. Preoperative X-rays, CT scan and MRI showed evidence of basilar invagination and Chiari malformation. E-I. Postoperative X-rays, CT scan, MRI and three-dimensional reconstruction showed posterior occipitocervical fixation using the crossed rod configuration after C1 laminectomy, enlargement of the foramen magnum, and cerebellar tonsillectomy. J-L. X-rays and CT scan from the 6-month follow-up showed stable fixation and bone fusion
Fig. 3.
A 22-year-old man diagnosed with atlantoaxial fracture. A-D. Preoperative X-rays and CT scans showed evidence of atlas and odontoid fractures. E-H. Postoperative X-rays, CT scan and three-dimensional reconstruction showed posterior atlantoaxial fixation using the crossed rod configuration. I-L. X-rays and CT scan from the 3-month follow-up showed stable fixation and bone fusion
PR fixation method
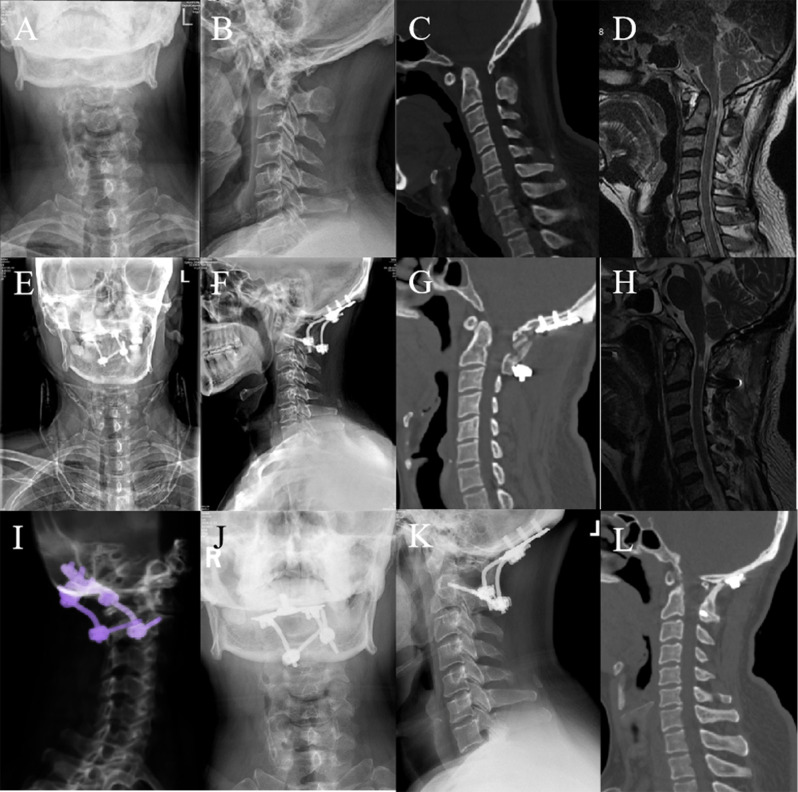
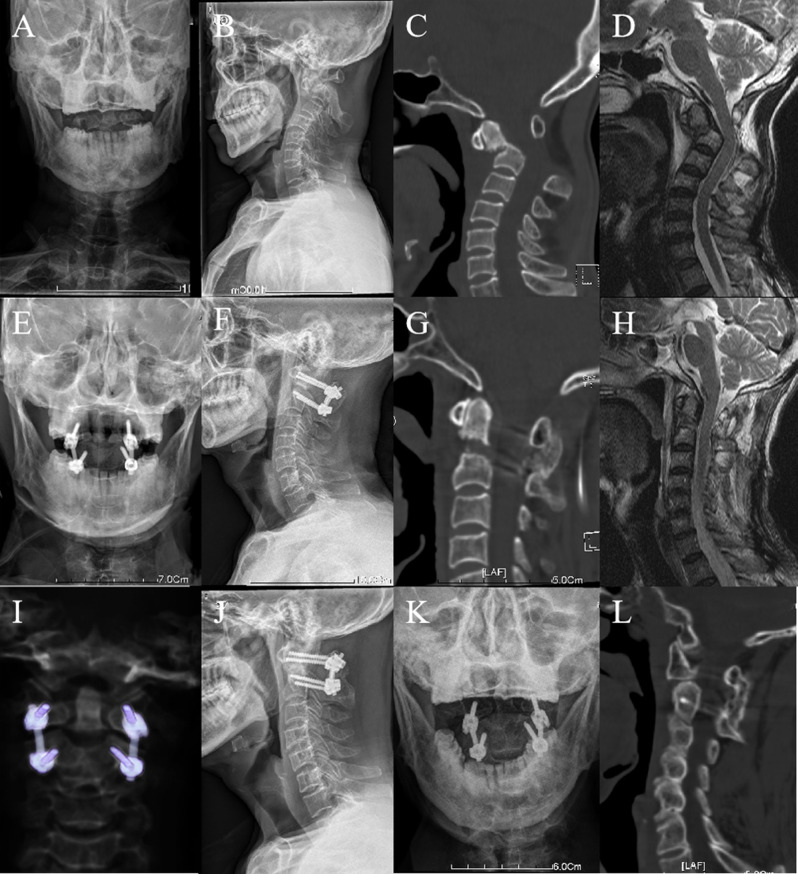
Whether atlantoaxial fixation or occipitocervical fixation, the overall surgical procedure and steps were consistent with those in the CR group, except that the cross-rod structure was changed to a parallel-rod structure for connecting screws (Figs. 4 and 5).
Fig. 4.
A 46-year-old man diagnosed with basilar invagination and atlantoaxial dislocation. A-D. Preoperative X-rays, CT scan and MRI showed evidence of basilar invagination and atlantoaxial dislocation. E-I. Postoperative X-rays, CT scan, MRI and three-dimensional reconstruction showed posterior occipitocervical fixation using the conventional parallel rod configuration after C1 laminectomy and atlantoaxial dislocation reduction. J-L. X-rays and CT scan from the 6-month follow-up showed good reduction and bone fusion
Fig. 5.
A 61-year-old man diagnosed with odontoid fracture and atlantoaxial dislocation. A-D. Preoperative X-rays and CT scans showed evidence of the odontoid fracture combined with atlantoaxial dislocation. E-I. Postoperative X-rays, CT scan, MRI and three-dimensional reconstruction showed posterior atlantoaxial fixation using the parallel rod configuration. J-L. X-rays and CT scan from the 3-month follow-up showed stable fixation and bone fusion
Observed indexes
The surgical time, bleeding volume, postoperative complications and bone fusion conditions were recorded. Atlas-dens intervals (ADI) was used to assess the reducing condition of atlanto-axial dislocation. The Japanese Orthopaedic Association score (JOA) and Neck Disability Index (NDI) were used to evaluate the neurologic function and cervical dysfunction. The visual analogue scale (VAS) was used to assess the degree of occipital neck pain.
Statistical analysis
Statistical analysis was performed using the SPSS 27.0 software (IBM, Armonk, NY, USA). For continuous numeric variables, all data were subject to normal distribution based on K-S test and expressed as the mean and standard deviation. For non-continuous variables, all data would be expressed as the median plus the interquartile range. Student’s paired t test was used for intra-group comparisons and independent samples t test for inter-group comparisons. For nonparametric tests, the Mann-Whitney U test for independent samples and Wilcoxon signed-rank test for paired samples were used. The level of significance was set at p < 0.05.
This cohort study has been reported in line with the STROBE Guideline [9].
Results
Patient characteristics
The average follow-up time was 22.7 ± 7.5 months in CR group and 26.7 ± 8.6 months in PR group, with no difference between the two groups (P > 0.05). There were no statistically significant differences between the two groups in terms of gender [11 Male (52.4%) and 10 Female (47.6%) vs. 15 Male (55.6%) and 12 Female (44.4%), P > 0.05] and mean age (40.4 ± 9.8 years vs. 41.0 ± 11.9 years, P > 0.05). In addition, no differences were observed between the CR and PR groups in terms of preoperative symptoms and fixation type (P > 0.05, Table 1).
Table 1.
Comparison of baseline information between the two groups
| Items | CR group | PR group | p |
|---|---|---|---|
| Cases/n | 21 | 27 | / |
| Age/years | 40.4 ± 9.8 | 41.0 ± 11.9 | 0.869 |
| Gender/n(%) | 0.827 | ||
| Male | 11 (52.4%) | 15 (55.6%) | / |
| Female | 10 (47.6%) | 12 (44.4%) | / |
| Symptoms/n(%) | |||
| Occipitocervical pain | 19 (90.5%) | 23 (85.2%) | 0.582 |
| Numbness of limbs | 13 (61.9%) | 14 (51.9%) | 0.486 |
| Weakness of limbs | 10 (47.6%) | 12 (44.4%) | 0.827 |
| Unsteady gait | 5 (23.8%) | 6 (22.2%) | 0.897 |
| Diagnoses/n(%) | |||
| Atlantoaxial dislocation | 9 (42.9%) | 11 (40.7%) | 0.770 |
| Atlantoaxial fracture | 8 (38.1%) | 9 (33.3%) | 0.732 |
| Basilar invagination | 5 (23.8%) | 8 (29.6%) | 0.653 |
| Atlantoaxial intraspinal tumor | 2 (9.5%) | 2 (7.4%) | 0.594 |
| Fixation type/n(%) | 0.653 | ||
| C1-2 | 16 (76.2%) | 19 (70.4%) | / |
| C0-2 | 5 (23.8%) | 8 (29.6%) | / |
| Follow-up/months | 22.7 ± 7.5 | 26.7 ± 8.6 | 0.092 |
*Values are expressed as mean ± standard error, with the range or percentage in parentheses
CR = Crossed rod; PR = Parallel rod
Observed indexes
Surgeries were performed successfully in all 48 cases, with no intraoperative complications such as spinal nerves and blood vessels damage. There were no statistical differences between CR and PR groups in terms of the average operative time (146.2 ± 35.8 min vs. 134.4 ± 30.2 min, P > 0.05), and mean intraoperative blood loss (156.2 ± 89.0 mL vs. 120.4 ± 44.3 mL, P > 0.05). Regarding imaging parameters, no significant difference was found in the preoperative ADI between the two groups (6.5 ± 1.9 mm vs. 7.3 ± 2.2 mm, P > 0.05). However, although the ADI was reduced in both groups after surgery (CR: P1 < 0.05; PR:P1 < 0.05) and at the final follow-up (CR: P2 < 0.05; PR: P2 < 0.05), the ADI in the PR group was smaller compared to the CR group after surgery (1.5 ± 1.0 mm vs. 2.3 ± 0.9 mm, P < 0.05) and at the final follow-up (1.6 ± 0.7 mm vs. 2.3 ± 0.8 mm, P < 0.05). Meanwhile, no differences were found in preoperative JOA scores [13.0 (15.0–11.0) vs. 12.0 (14.0–11.0), P > 0.05], VAS scores [4.0(5.0-2.5) vs. 4.0(5.0–2.0), P > 0.05], and NDI [58.0(61.0–54.0) % vs. 58.0(60.0–56.0) %, P > 0.05] between the two groups. All patients experienced relief of clinical symptoms after surgery, as the postoperative JOA scores, VAS scores and NDI improved significantly in both groups after surgery and at the final follow-up (P < 0.05). There were no significant differences in JOA, VAS and NDI between the two groups after surgery and at the final follow-up (P < 0.05). Postoperative X-ray and CT scans showed proper placement of the internal fixation and well cervical sequence in all cases, and satisfactory spinal cord decompression was found via MRI. Except for one patient in the PR group, all cases achieved bone fusion at 12-month follow-up. However, we found that although there were no differences in fusion rates between the two groups at 6 and 12 months (90.5% vs. 85.2%; 100% vs. 96.3%, P > 0.05), the CR group had a significantly higher fusion rate than the PR group at 3 months postoperatively (80.9% vs. 51.6%, P < 0.05). No internal fixation failure, signs of instability or other complications occurred during the follow-up period (Table 2).
Table 2.
Comparisons of clinical data before and after surgery between the two groups
| Items | CR Group | PR Group | p |
|---|---|---|---|
| Surgical.time/min | 146.2 ± 35.8 | 134.4 ± 30.2 | 0.224 |
| Bleeding/mL | 156.2 ± 89.0 | 120.4 ± 44.3 | 0.075 |
| ADI /mm | |||
| Before surgery | 6.5 ± 1.9 | 7.3 ± 2.2 | 0.155 |
| At discharge | 2.3 ± 0.9 | 1.5 ± 1.0 | 0.012 |
| Final follow-up | 2.3 ± 0.8 | 1.6 ± 0.7 | 0.001 |
| P1 | < 0.001 | < 0.001 | / |
| P2 | < 0.001 | < 0.001 | / |
| JOA/score | |||
| Before surgery | 13.0 (15.0–11.0) | 12.0 (14.0–11.0) | 0.418 |
| At discharge | 15.0 (16.0–13.0) | 15.0 (16.0–13.0) | 0.416 |
| Final follow-up | 16.0 (17.0–14.0) | 16.0 (17.0–16.0) | 0.201 |
| P1 | < 0.001 | < 0.001 | / |
| P2 | < 0.001 | < 0.001 | / |
| VAS/score | |||
| Before surgery | 4.0(5.0-2.5) | 4.0(5.0–2.0) | 0.832 |
| At discharge | 1.0(2.0-0.5) | 1.0(2.0–0) | 0.583 |
| Final follow-up | 0(1.0–0) | 0(1.0–0) | 0.541 |
| P1 | < 0.001 | < 0.001 | / |
| P2 | < 0.001 | < 0.001 | / |
| NDI/% | |||
| Before operation | 58.0(61.0–54.0) | 58.0(60.0–56.0) | 0.975 |
| At discharge | 24.0(28.0–22.0) | 26.0(28.0–24.0) | 0.216 |
| Final follow-up | 2.0(4.0–0) | 0(4.0–0) | 0.365 |
| P1 | < 0.001 | < 0.001 | / |
| P2 | < 0.001 | < 0.001 | / |
| Complications/n(%) | |||
| Bone non-fusion | 0 | 1 (3.7%) | > 0.999 |
| Bony fusion/n(%) | |||
| 3-month follow-up | 17 (80.9%) | 14 (51.6%) | 0.037 |
| 6-month follow-up | 19 (90.5%) | 23 (85.2%) | 0.683 |
| 12-month follow-up | 21 (100%) | 26 (96.3%) | > 0.999 |
*Values are expressed as mean ± standard error or the median plus the interquartile range, with the range in parentheses
CR = Crossed rod; PR = Parallel rod; ADI = Atlas-dens intervals; JOA = Japanese Orthopaedic Association score; VAS = visual analogue scale; NDI = Neck Disability Index; P1 represents the statistical difference between preoperative and postoperative changes in observed values; P2 represents the statistical difference between preoperative and at the final follow-up changes in observed values
Discussion
Craniocervical junction disorders often require reconstruction of stability through strong internal fixation. At present, screw-rod fixation is the most commonly method applied in posterior atlantoaxial fixation [10, 11], whereas posterior occipitocervical fixation is usually performed with plate-screw-rod fixation [12, 13].
The range of motion in the craniocervical junction is large, thus methods to improve the stability of internal fixation structures are continually explored. Stability of the internal fixation is a crucial factor for bone fusion and consequently for a good clinical outcome. According to many biomechanical studies, C1 and C2 pedicle screws are applied preferentially in clinics to obtain better stability [6, 14, 15]. However, in the presence of anatomic variation, C1 lateral mass screws, C2 pars screws, and C2 translaminar screws were used as substitutes, thereby reducing the stability of the internal fixation [14, 16–18]. Currently, the use of transverse links in posterior screw-rod and plate-screw-rod fixation is a common method to increase the global stability [3–5]. Nevertheless, for upper cervical spine surgery, the large bending arc and limited space of rods make the placement of a transverse link difficult, which increases the surgical time and risks of infection and spinal cord injury. It is therefore worthwhile to seek a simpler, practicable process to improve the stability.
In current clinical practice, both the posterior atlantoaxial screw-rod and occipitocervical plate-screw-rod fixations utilize a PR configuration with a “II” shape. In 2011, Gabriel et al. [6] first studied the novel CR configuration by comparing its biomechanical stability to that of the traditional PR configuration by an in vitro occipitocervical fixation using C2 translaminar screws. The CR configuration showed 29%, 15% and 16% decreases in range of motion of flexion-extension, lateral bending and axial rotation respectively in comparison to the PR configuration. In 2017, Shen et al. [7] compared the CR and PR configurations in the atlantoaxial fixation using a unilateral C1 posterior arch screws and C2 laminar screws combined with an ipsilateral C1-C2 pedicle screw-rod system, obtaining similar results to Gabriel et al. Recently, Qiu et al. [8] investigated the biomechanics of the CR and PR constructs in the posterior atlantoaxial screw-rod fixation using C1 bilateral pedicle screws with C2 pedicle screws or C2 lamina screws, which revealed that the CR configuration could provide superior stability in axial rotation, lateral bending and extension. The CR technique’s “X” shape forms a multi-triangle construction that has better structural geometric stability and is a simpler way to increase the global stability of both posterior atlantoaxial screw-rod and occipitocervical plate-screw-rod fixations.
In this study, we investigate the primary clinical outcomes of the CR configuration used in upper cervical spine surgery. Furthermore, we are the first to compare the differences in clinical outcomes between the CR configuration and the PR configuration applied in posterior occipitocervical and atlantoaxial fixations. As expected, this technique can provide reliable internal fixation for craniocervical junction in clinical use. Compared with the preoperative period, patients in the CR group had a mean increase of 2–3 points in postoperative JOA scores, a mean decrease of 3 points in VAS scores and even more than 50% improvement in NDI at the final follow-up. The results also showed that no matter which fixation type was used, there was no significant difference in postoperative outcomes for patients treated with CR technique compared to the prevalent PR method. On the other hand, we found that although the postoperative ADI was significantly reduced in the CR group, it was still greater than that in the PR group. The screw-rod system or plate-screw-rod system can generate retraction force by bending the rod. Compared to the conventional PR placement, the CR configuration is not able to sufficiently transmit the reduction force generated by bending rods due to the crossed direction of the rods on both sides. Therefore, its reduction force is weaker than that of the PR structure for the same length. This is, of course, a downside to the CR technique. Therefore, this technique is not ideal for cases with severe atlantoaxial dislocation that require large reduction forces. However, in most cases without severe dislocations where only fixation or small reduction force is required, this technique is an option to improve the stability of fixation.
Furthermore, we also found that patients in the CR group had an 80.9% rate of bone fusion at 3 months after surgery, which was significantly higher than the 51.6% in the PR group. Usually, patients need to wear neck braces to accelerate this process, which, besides discomfort, prolongs the time for patients to return to normal life and work to a certain extent. Considering that the CR configuration creates a multiple triangular stabilizing structure, it increases the overall stability of the bone grafted area. Previous biomechanical studies have also demonstrated that the CR configuration has better three-dimensional stability [6–8]. As a result, patients can obtain rapid bone fusion in the early postoperative period and can restore the stability of the cervical spine earlier without the assistance of neck braces.
The CR configuration occupies the middle area, and whether this technique affects bone grafting needs to be explained. The CR configuration decreases the middle bone grafting area but increases the space for bone grafting on both sides, which is the opposite of the PR structure. On the other hand, we have found in practice that even if the rods cross, it does not adhere completely to the surface of the tissue, and there still exists a certain space underneath for bone grafting.
There are several limitations in the current study. First, the sample size is small, and more studies with a larger number of cases are needed in the future. Second, the present study is retrospective in nature and could not eliminate the selection bias that existed in the inclusion of cases. Thus the evidence level is relatively low. Future prospective studies may better control for follow-up timing intervals and may have the potential to better elucidate the applied value of the cross-rod technique. In addition, this study did not consider whether factors such as anatomical variations had an effect on the crossed rod technique. More detailed subgroup research will be needed in the future to further evaluate this technique comprehensively.
Conclusion
Based on the above, we believe that for posterior occipitocervical and atlantoaxial fixations, the application of a CR configuration can provide clinically reliable stabilization in reconstruction of the craniocervical junction. Although its reduction force is slightly weaker compared with the prevalent PR technique, patients have a higher rate of early bone fusion. This technique may be a viable alternative for the clinical application and warrants further research.
Acknowledgements
No.
Author contributions
XM, XZ, MC and HY contributed to the study conception and design. MC and HY contributed to the Material preparation. Data collection and analysis were performed by all authors. The first draft of the manuscript was written by XZ and MC. XM and XZ administrate the whole project and acquire funding. XM, XZ and MC were responsible for reviewing and revising. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by funds from the National Natural Science Foundation of China (82272582) and the Natural Science Foundation of Guangdong Province (2023A1515011857).
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethics approval and consent to participate
This retrospective study was approved by the Ethical Review Committee of General Hospital of Southern Theatre Command of Peoples Liberation Army (2024012), People’s Republic of China. The data are anonymous, and the requirement for informed consent was therefore waived.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mandi Cai and Haozhi Yang contributed equally and should be regarded as co-first authors.
Xiaobao Zou and Xiangyang Ma contributed equally and should be regarded as co-corresponding authors.
Contributor Information
Xiaobao Zou, Email: zouxb6478@126.com.
Xiangyang Ma, Email: maxy1001@126.com.
References
- 1.Joaquim AF, Osorio JA, Riew KD. Occipitocervical fixation: General considerations and surgical technique. Global Spine J. 2020;10(5):647–56. 10.1177/2192568219877878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang DG, Hao DJ, He BR, Wu QN, Liu TJ, Wang XD, Guo H, Fang XY. Posterior atlantoaxial fixation: a review of all techniques. Spine J. 2015;15(10):2271–81. 10.1016/j.spinee.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 3.Wang HW, Yin YH, Li T, Yu XG, Qiao GY. Effects of transverse connector on reduction and fixation of atlantoaxial dislocation and basilar invagination using posterior C1-C2 screw-rod technique. Spine J. 2019;19(12):1995–2002. 10.1016/j.spinee.2019.06.021. [DOI] [PubMed] [Google Scholar]
- 4.Lehman RA Jr., Dmitriev AE, Wilson KW. Biomechanical analysis of the C2 intralaminar fixation technique using a cross-link and offset connector for an unstable atlantoaxial joint. Spine J. 2012;12(2):151–6. 10.1016/j.spinee.2012.01.020. [DOI] [PubMed] [Google Scholar]
- 5.Cornaz F, Widmer J, Snedeker JG, Spirig JM, Farshad M. Cross-links in posterior pedicle screw-rod instrumentation of the spine: a systematic review on mechanical, biomechanical, numerical and clinical studies. Eur Spine J. 2021;30(1):34–49. 10.1007/s00586-020-06597-z. [DOI] [PubMed] [Google Scholar]
- 6.Gabriel JP, Muzumdar AM, Khalil S, Ingalhalikar A. A novel crossed rod configuration incorporating translaminar screws for occipitocervical internal fixation: an in vitro biomechanical study. Spine J. 2011;11(1):30–5. 10.1016/j.spinee.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 7.Shen K, Deng Z, Yang J, Liu C, Zhang R. Biomechanical study of novel unilateral C1 posterior arch screws and C2 laminar screws combined with an ipsilateral crossed C1-C2 pedicle screw-rod fixation for atlantoaxial instability. Arch Orthop Trauma Surg. 2017;137(10):1349–55. 10.1007/s00402-017-2781-0. [DOI] [PubMed] [Google Scholar]
- 8.Qiu F, Zou XB, Xu XL, Jiang WC, Liu GC, Ma XY. A biomechanical comparison of crossed and parallel rod configurations in atlantoaxial internal fixation. Eur Spine J. 2021;30(2):576–84. 10.1007/s00586-020-06655-6. [DOI] [PubMed] [Google Scholar]
- 9.Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12(12):1500–24. 10.1016/j.ijsu.2014.07.014. [DOI] [PubMed] [Google Scholar]
- 10.Huang DG, Zhang XL, Hao DJ, Yu CC, Mi BB, Yuan QL, He BR, Liu TJ, Guo H, Wang XD. Posterior atlantoaxial fusion with a screw-rod system: allograft versus iliac crest autograft. Clin Neurol Neurosurg. 2017;162:95–100. 10.1016/j.clineuro.2017.10.002. [DOI] [PubMed] [Google Scholar]
- 11.Bhowmick DA, Benzel EC. Posterior atlantoaxial fixation with screw-rod constructs: safety, advantages, and shortcomings. World Neurosurg. 2014;81(2):288–9. 10.1016/j.wneu.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 12.Ji W, Lin SY, Bao MG, Zou XB, Ge S, Ma XY, Chen JT, Yang JC. Anatomical analysis of the occipital bone in patients with basilar invagination: a computed tomography-based study. Spine J. 2020;20(6):866–73. 10.1016/j.spinee.2020.01.005. [DOI] [PubMed] [Google Scholar]
- 13.Kukreja S, Ambekar S, Sin AH, Nanda A. Occipitocervical fusion surgery: review of operative techniques and results. J Neurol Surg B Skull Base. 2015;76(5):331–9. 10.1055/s-0034-1543967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sim HB, Lee JW, Park JT, Mindea SA, Lim J, Park J. Biomechanical evaluations of various c1-c2 posterior fixation techniques. Spine (Phila Pa 1976). 2011;36(6):E401–7. 10.1097/BRS.0b013e31820611ba. [DOI] [PubMed] [Google Scholar]
- 15.Lapsiwala SB, Anderson PA, Oza A, Resnick DK. Biomechanical comparison of four C1 to C2 rigid fixative techniques: anterior transarticular, posterior transarticular, C1 to C2 pedicle, and C1 to C2 intralaminar screws. Neurosurgery. 2006;58(3):516–21. 10.1227/01.Neu.0000197222.05299.31. discussion – 21. [DOI] [PubMed] [Google Scholar]
- 16.Fensky F, Kueny RA, Sellenschloh K, Püschel K, Morlock MM, Rueger JM, Lehmann W, Huber G, Hansen-Algenstaedt N. Biomechanical advantage of C1 pedicle screws over C1 lateral mass screws: a cadaveric study. Eur Spine J. 2014;23(4):724–31. 10.1007/s00586-013-3143-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ma XY, Yin QS, Wu ZH, Xia H, Liu JF, Xiang M, Zhao WD, Zhong SZ. C1 pedicle screws versus C1 lateral mass screws: comparisons of pullout strengths and biomechanical stabilities. Spine (Phila Pa 1976). 2009;34(4):371–7. 10.1097/BRS.0b013e318193a21b. [DOI] [PubMed] [Google Scholar]
- 18.Su BW, Shimer AL, Chinthakunta S, Salloum K, Ames CP, Vaccaro AR, Bucklen B. Comparison of fatigue strength of C2 pedicle screws, C2 pars screws, and a hybrid construct in C1-C2 fixation. Spine (Phila Pa 1976). 2014;39(1):E12–9. 10.1097/brs.0000000000000063. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.