Abstract
Osseous sarcoidosis is a rare manifestation of sarcoidosis, often mimicking other conditions like metastatic disease. Skeletal involvement occurs in only 3%-13% of cases (1), making diagnosis challenging. We present the case of a 63-year-old female with a 1-month history of inflammatory bone pain and multiple lytic and blastic lesions.
A 63-year-old female presented with a 1-month history of inflammatory pain in the left hip and lumbar spine. Radiological studies, including magnetic resonance imaging (MRI) and computed tomography (CT), revealed multiple bone lesions throughout the lumbar spine, sacrum and iliac bones, raising suspicion of metastatic disease a bone biopsy confirmed a diagnosis of sarcoidosis.
MRI and CT showed lytic and blastic lesions in the axial skeleton, with FDG-PET indicating diffuse uptake in the iliac bone and mediastinal adenopathy. Imaging was crucial in ruling out metastases and guiding the biopsy, which confirmed the diagnosis.
Osseous sarcoidosis is a rare entity that poses a significant diagnostic challenge, often resembling metastatic disease. Imaging techniques such as MRI and CT, combined with biopsy, are effective, noninvasive methods for evaluation and diagnosis. The patient was treated with corticosteroids in high doses and systemic methotrexate, showing improvement in inflammatory pain and stabilization of the bone lesions.
Keywords: Sarcoidosis, Osseous bone lesions, Granuloma
Introduction
Sarcoidosis is a poorly understood multisystem inflammatory disease with an unclear etiology, characterized histologically by noncaseating epithelioid and giant cell granulomas [1]. In the United States, sarcoidosis is more prevalent in African Americans, with an estimated prevalence of 35.5 per 100, 000 compared to 10.9 per 100,000 in Caucasians [[2], [3]]. In Scandinavian countries, prevalence rates for sarcoidosis have been reported at 64-77 per 100,000. Although sarcoidosis can affect any organ, osseous involvement is particularly rare, occurring in only 3%-13% of cases [1], specific demographic data for osseous sarcoidosis are limited due to its rarity and the challenge in identifying such cases.
Osseous sarcoidosis appears rare; the short tubular bones of the hands and feet are most frequently involved, often with an asymmetrical presentation [3]. A French study, however, has shown that the most common imaging presentation was the spine (52%), and pelvis (42%), followed by the hands (22%) and femur (19%).
Nonspecific pain is the most common feature of axial skeletal sarcoidosis; however, half of patients are asymptomatic [1].
Osseous sarcoidosis can present as multiple lytic and/or blastic lesions, and is often a challenge diagnostic because it mimics other conditions such as Multiple myeloma or metastatic bone disease [[2], [3]].
In recent years there has been an increase in cases of bone sarcoidosis requiring differentiation from malignant disease. In cases lesions are detected by CT or MRI, where lytic or blastic bone lesions, PET is a mandatory test to rule out occult neoplasia. However, in cases of bone sarcoidosis, it fails to reliably differentiate sarcoid lesions from metastases or other benign bone processes (Paget's disease, fibrous dysplasia, giant cell tumors, and osteomyelitis secondary to infections such as tuberculosis or fungal infections [10].
Normalized uptake values are equally high in lymphadenopathy, lung lesions and bone lesions; therefore, it is difficult to distinguish between the 2 by PET/CT. Also, patients with sarcoidosis are at increased risk for many malignancies, including lung cancer and lymphoma, presumably influenced by chronic inflammation, immune dysfunction, shared etiologic agents, genetic susceptibility, and induction by some drugs. Therefore, in most cases histologic confirmation of sarcoidosis is necessary to definitively rule out malignancy
Overlapping imaging findings cause delays in diagnosis and can lead to unnecessary investigations or misdiagnosis [11].
The objective of this case report is to highlight the importance of imaging techniques such as, FDG-PET in the diagnosis of osseous sarcoidosis. These modality play a pivotal role in ruling out malignancies and in some cases even useful in evaluating treatment efficacy. The guiding the bone biopsy remains essential for confirming sarcoidosis. It has been suggested that the best way to assess the extent of bone lesions is by a combination of radiographic techniques such as whole body bone scan and PET-CT, as they often manifest as polyostotic.
Clinical case
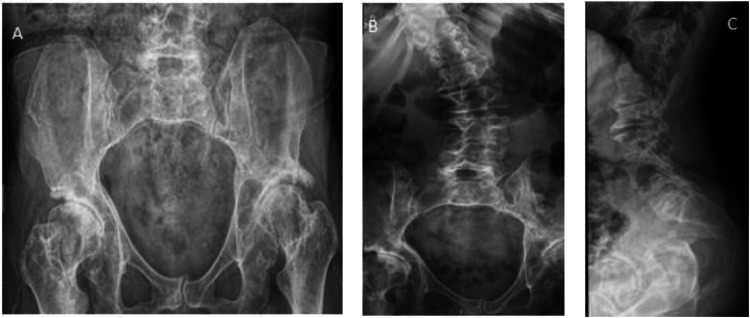
A 63-year-old woman with a 1-month history of inflammatory pain in the left hip and lumbar spine. The patient denied any history of trauma. Previously, the patient referred a 1-year history of fatigue and progressive dyspnea. No weight loss, fever, or night sweats were reported. She had a prior medical history of kyphoscoliosis, osteoarthritis, vertebral fractures and bilateral hip dysplasia. A lumbar spine and pelvis x-Ray revealed the previously known deformities (Fig. 1). Blood tests revealed normal kidney function, normal calcium levels, and angiotensin-converting enzyme (ACE) at the high upper limit. No other relevant findings were reported in blood tests.
Fig. 1.
(A) Pelvis X-ray showing hip dysplasia and osteoarthritis, (B-C) lumbar spine deformities showing kyphoscoliosis, osteophytes, and vertebral fractures, lytic and blastic lesions.
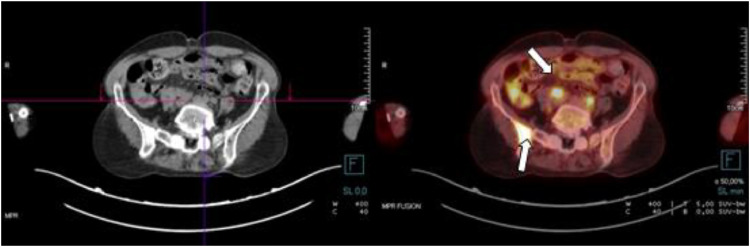
Since the patient complained of pain with a neuropathic component, the study was extended with magnetic resonance imaging (MRI) of the spine and hip, that revealed multiple lytic and blastic bone lesions T2 hyperintense lesions were observed in the L2 and L3 vertebral bodies, with infiltration in the trabecular skeleton of both iliac bones and the left sacral wing. Further infiltration was seen in the left acetabular region and the bilateral ischiopubic branches (Fig. 2). Considering a probable diagnosis of bone metastases, a whole- body computed tomography (CT) scan and a FDG-PET was performed (Fig. 2, Fig. 3), which showed Hypermetabolic deposits located in the jugular regions, axillary, pretracheal and perivascular region, left pulmonary hilum, As well as at the infradiaphragmatic level highly suspicious of lymph proliferative disease. However hyper metabolic lesions were observed as well in the right humeral head, right acetabular region, left femoral, acetabular region, and right ischium.
Fig. 2.
(A) multiple mixed (sclerotic and lytic) bone lesion (arrow). (B) Bone CT guided biopsy performed in the bigger lesion located in the iliac right bone. (C-D) multiple bone lesions hypo intense in T1 and hyper intense in STIR (arrows).
Fig. 3.
18F-fludeoxyglucose positron-emission tomography: uptake in the retroperitoneal multiple lymphadenopathies. Diffuse and nonspecific uptake on the right iliac bone (arrow).
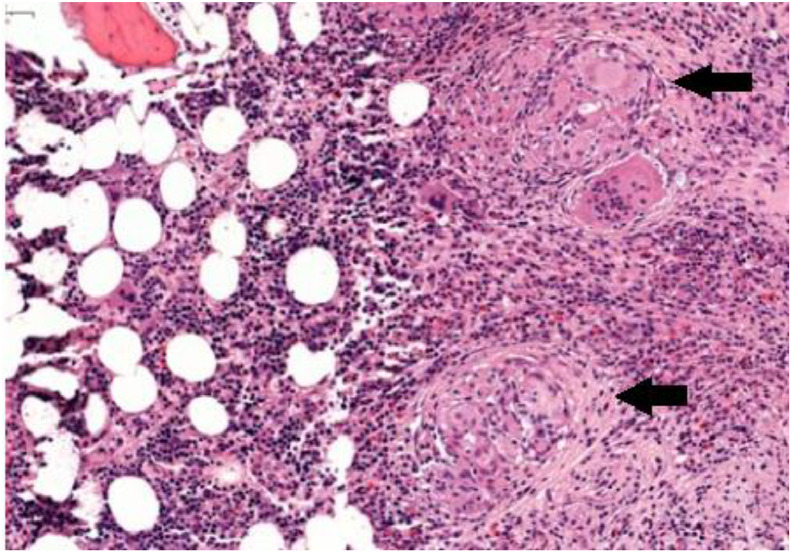
A CT-guided iliac bone biopsy was performed which confirmed the presence of noncaseating granulomas (Fig. 4). Hematoxylin an eosin staining demonstrated noncaseating epitheloid cell granulomas with multinucleated giant cells.
Fig. 4.
Bone marrow cylinder HE 15×: presence of abundant well-formed epithelioid granuloma, noncoalescent without necrosis (black arrow).
An infectious process was ruled out with negative cultures and negative quantiferon, proliferative disease was also ruled out due to the biopsy findings. A diagnosis of sarcoidosis with lytic and blastic lesion was made base on the radiological and histological findings. Treatment with prednisone 1mg/kg was started with clinical improvement, we associated methotrexate 20 mg/week as corticosteroid sparing agent. After 6 months of treatment and given that we did not achieve a decrease in corticosteroids we decided to start biological therapy with infliximab at 5 mg/kg/8 weeks. This treatment led to a resolution of lymphadenopathy and stabilization of the bone lesions but only a partial response in bone pain was achieved to date
Discussion
We reported a case of multiple bone sarcoidosis mimic an osseous metastasis, with a histological osseous confirmation, FDG-PET/CT was fundamental for the differential diagnosis excluding lymphoproliferative processes. When sarcoidosis affects the skeleton, pain is typically the most frequent and initial symptom, and when it involves the spine, neurological symptoms may also occur. However, some authors have noted that bone involvement can be asymptomatic [4]. The coexistence of sarcoidosis with bone deformities such as kyphoscoliosis, osteoarthritis, hip dysplasia, and vertebral fractures is even more unusual and it has probably delayed the diagnosis in our patient.
There are reported cases of multiple simultaneous bone lesions, but only 1 case similar to ours in which the vertebrae, pelvis, humerus and vertebral as in this case are involved (polyostotic), In a study by Zhou et al. [9], the spine and pelvis were identified as the sites of sarcoid bone lesions in 68.8% and 35.9% of cases. Due to the similarities in imaging test, sarcoidosis FDG-PET findings shows areas of increased uptake and osteolytic skeletal lesions in CT in the other hand metastases shows increased uptake and occasionally photopaenic areas may be seen due to a lack of an osteoblastic response in FDG-PET and lytic lesions which usually initially destroy the medulla in CT, differentiating bone sarcoidosis lesions from metastases requires a bone biopsy in most of the cases, which provided the definitive diagnosis of osseous sarcoidosis [[7], [8], [9]].
There is no consensus about therapeutic management of bone sarcoidosis. Asymptomatic patients typically do not require treatment [6]. In fact, the current treatment strategy for osseous sarcoidosis consists of corticosteroid therapy for symptomatic patients [1,3,4,5]. Prednisone, at doses of 20-40 mg per day, is commonly used as first-line therapy and has proven to be effective in many cases associated with Methotrexate (MTX) to tappers corticosteroids, a second line treatment, is tumor necrosis factor-alpha inhibitors (TNFi) with varying results [12].
Other therapies, such as hydroxychloroquine, bisphosphonates, colchicine, gabapentin and surgery, have been used to treat osseous sarcoidosis, with varying results [12].
Consent Information
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review.
Patient consent
I confirm that I have obtained written informed consent from the patient for the publication of any information, data, or images pertaining to their case titled: Bone pain, a rare case of Osseous sarcoidosis in Radiology case reports. The patient has been fully informed about the purpose, scope, and potential impact of the publication and has given their explicit consent to share relevant information for educational and scientific purposes.
I confirm that the patient understands that their identity will remain confidential, and all personal details that could reveal their identity will be anonymized, unless explicitly agreed otherwise.
Should any further information be required, I am available to provide it.
Footnotes
Competing Interests: The author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgments: We extend our sincere thanks to the Rheumatology Department at University Hospital son Llátzer, and the Radiology and Imaging Department at Rotger Clinic. Without their support, this manuscript would not have been possible.
FERBT2024: The authors also express their gratitude to the Spanish Foundation of Rheumatology for providing medical writing/editorial assistance during the preparation of the manuscript. The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Charifi Y, Dkhissi Y, Haloua M, Alaoui Lamrani Y, Berrady G, Boubbou M, et al. Pelvic and lumbar pain revealing bone sarcoidosis: a case report. Clin Med Insights Case Rep. 2021;14 doi: 10.1177/11795476211014788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kucharz EJ. Osseous manifestations of sarcoidosis. Reumatologia. 2020;58(2):93–100. doi: 10.5114/reum.2020.95363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Robles LA, Matilla AF, Covarrubias MP. Sarcoidosis of the skull: a systematic review. World Neurosurg. 2020;139:387–394. doi: 10.1016/j.wneu.2020.04.114. [DOI] [PubMed] [Google Scholar]
- 4.Kucharz EJ. Osseous manifestations of sarcoidosis. Reumatologia. 2020;58:93–100. doi: 10.5114/reum.2020.95363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cadiou S, Robin F, Guillin R, et al. Spondyloarthritis and sarcoidosis: related or fake friends? A systematic literature review. Joint Bone Spine. 2020;87:579–587. doi: 10.1016/j.jbspin.2020.06.011. [DOI] [PubMed] [Google Scholar]
- 6.Bechman K, Christidis D, Walsh S, Birring SS, Galloway J. A review of the musculoskeletal manifestations of sarcoidosis. Rheumatology. 2018;57:777–783. doi: 10.1093/rheumatology/kex317. [DOI] [PubMed] [Google Scholar]
- 7.Akaike G, Itani M, Shah H, Ahuja J, Yilmaz Gunes B, Assaker R, et al. PET/CT in the diagnosis and workup of sarcoidosis: focus on atypical manifestations. Radiographics. 2018;38(5):1536–1549. doi: 10.1148/rg.2018180053. [DOI] [PubMed] [Google Scholar]
- 8.Makis W, Palayew M, Rush C, Probst S. Disseminated multi-system sarcoidosis mimicking metastases on 18F-FDG PET/CT. Molecular Imag Radion Ther. 2018;27(2):91. doi: 10.4274/mirt.29200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou Y, Lower EE, Li H, Farhey Y, Baughman RP. Clinical characteristics of patients with bone sarcoidosis. Semin Arthritis Rheum. 2017;47:143–148. doi: 10.1016/j.semarthrit.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 10.Yıldırım F, Kalkan K, Akkuzu G, Özgür DS, Karaalioğlu B, Deniz R, et al. Musculoskeletal involvement in sarcoidosis: A single center experience. J Turk Soc Rheumatol. 2024;16(2):57–63. [Google Scholar]
- 11.Riaz M, Jha S. Sarcoidosis presenting as multiple osseous lesions. Proc (Bayl Univ Med Cent). 2024;37(3):489–492. doi: 10.1080/08998280.2024.2325322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kadoma N, Atsumi K, Shinbu K, Nishima S, Hisakane K, Nagata K, et al. Evaluation of sarcoidosis with multiple bone lesions using both bone scintigraphy and FDG-PET/CT: a case report. Respir Med Case Rep. 2024;51 doi: 10.1016/j.rmcr.2024.102077. [DOI] [PMC free article] [PubMed] [Google Scholar]