Abstract
Introduction and importance
Diverticular disease of the appendix is a rare condition often mistaken for acute appendicitis, with most cases diagnosed incidentally during histopathology, underscoring the importance of comprehensive pathological evaluation for accurate diagnosis.
Case presentation
A 34-year-old male presented with one day of periumbilical pain migrating to the right iliac fossa, without vomiting or bowel changes. Clinical examination revealed tenderness in the RIF. Laboratory tests indicated a syndrome inflammatoire biologique. Ultrasound and CT scans suggested appendicular diverticulitis. Laparoscopic appendectomy confirmed an inflamed diverticulum. The patient had an uncomplicated recovery and was discharged on day 1, with no anomalies noted at one-year follow-up.
Clinical discussion
There are two types of appendiceal diverticula: congenital and acquired. Congenital diverticula result from outpouching of all appendiceal layers, while acquired diverticula arise from increased pressure due to factors like fecaliths or tumors. Risk factors for diverticular disease of the appendix (DDA) include male gender and age over 30. Diagnosing appendiceal diverticulitis preoperatively is challenging, often relying on ultrasound and CT findings. Appendicectomy is the preferred treatment, with pathological evaluation necessary for diagnosis. Prophylactic appendicectomy is advised for incidentally detected diverticular disease due to associated risks of perforation and malignancy.
Conclusion
The differential diagnosis of appendiceal diverticulitis is a rare but significant condition with increased risks of complications and malignancy. Early diagnosis and surgical intervention are crucial for effective management, highlighting the importance of thorough pathological evaluation in confirming the diagnosis.
Keywords: Appendiceal diverticulitis, Diagnosis, Complications, Surgical intervention, Pathological evaluation
Highlights
-
•
Appendiceal diverticulitis is a rare condition that can mimic acute appendicitis.
-
•
Effective management of appendiceal diverticulitis relies heavily on precise radiological interpretation, which can significantly impact the treatment approach and outcomes.
-
•
Appendiceal diverticulitis is associated with a heightened risk of complications, including perforation and appendiceal neoplasms.
1. Introduction
Diverticular disease of the vermiform appendix (DDA) is a rare condition that typically mimics acute appendicitis [1]. Its incidence ranges from 0.004 % to 2.1 % in appendectomy specimens [2]. Although imaging can aid in preoperative diagnosis, the majority of cases are identified incidentally during histopathological examination after surgery [3].
This incidental diagnosis underscores the difficulty in differentiating DDA from other acute abdominal conditions based solely on clinical presentation or imaging, emphasizing the importance of pathological examination for accurate diagnosis and management.
This work has been reported in line with the SCARE 2023 criteria [4].
2. Case presentation
The patient was a 34-year-old male with no significant medical or surgical history, who presented with a one-day history of periumbilical abdominal pain that later migrated to the right iliac fossa (RIF). The patient reported no episodes of vomiting or alterations in bowel transit. Upon clinical examination, tenderness was noted in the RIF, accompanied by guarding.
Initial laboratory investigations revealed an elevated C-reactive protein (CRP) level of 34 mg/L and a white blood cell count (WBC) of 14 × 10^9/L. Abdominal ultrasound showed a swollen appendix with associated fatty infiltration and a periappendicular fluid collection measuring 7 mm (Fig. 1).
Fig. 1.
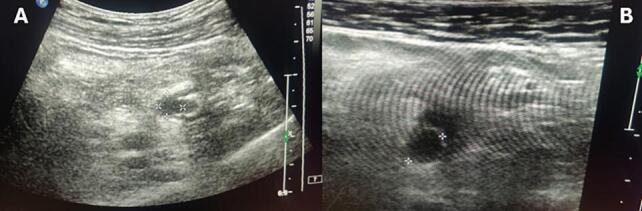
Longitudinal (A) and transverse (B) grayscale US images of the right lower quadrant demonstrate a small diverticular appendix outpouching and increased echogenicity of the adjacent fat.
A subsequent computed tomography (CT) scan indicated a swollen, non-aerated appendix with two appendicular wall formations measuring 4 mm and 7 mm, respectively, suggestive of appendicular diverticulitis (Fig. 2).
Fig. 2.
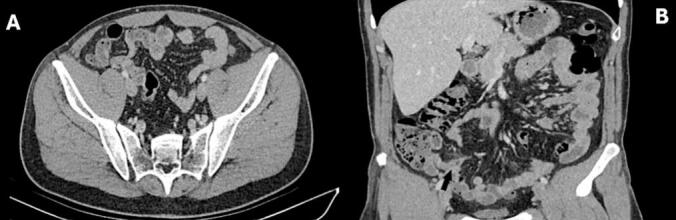
Axial (A), Coronal (B) contrast-enhanced CT images of the right lower quadrant demonstrate an appendiceal diverticula with inflammatory infiltration of the periappendiceal fat.
The patient underwent a laparoscopic appendectomy. Intraoperative findings revealed an inflamed internal laterocaecal appendix with an intact base and a true diverticulum present on its body (Fig. 3, Fig. 4). Histological analysis of the appendix demonstrated transmural acute inflammation and serositis, along with multiple diverticula. Importantly, there was no evidence of parasites, dysplasia, or malignancy.
Fig. 3.
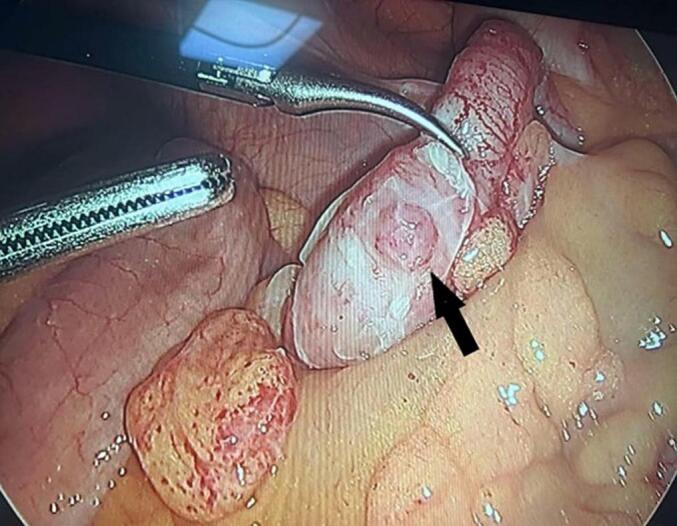
Intraoperative photos of the diverticular appendix (black arrow).
Fig. 4.
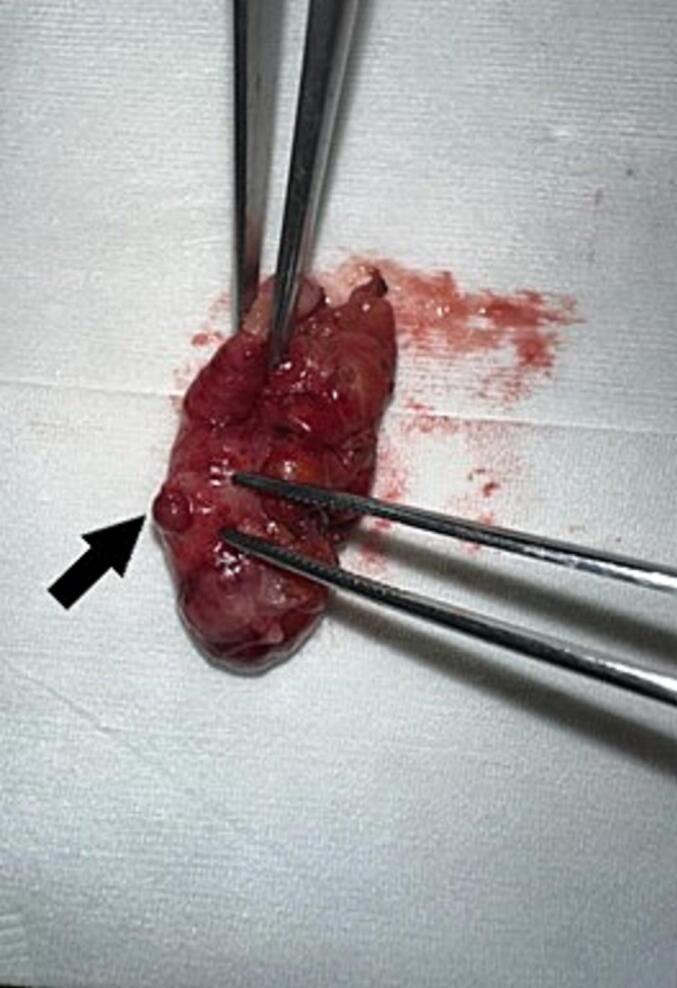
Photos of the surgical specimen (black arrow).
The postoperative course was straightforward, and the patient was discharged on postoperative day 1. Follow-up evaluations at one year post-surgery showed no anomalies, indicating a favorable recovery.
3. Discussion
There are two distinct types of appendiceal diverticula: congenital diverticula, which arise from the outpouching of all three appendiceal layers through a normal wall, and acquired diverticula, which occur secondary to increased pressure within the appendiceal lumen due to factors such as fecaliths, proximal tumors, or excessive mucus [3].
Known risk factors for diverticular disease of the appendix (DDA) include male gender, age over 30 years, Hirschsprung's disease, and cystic fibrosis [2]. The preoperative diagnosis of appendiceal diverticulitis can be challenging. Ultrasonographic findings typically reveal a hypoechoic lesion adjacent to the appendix, suggestive of an inflamed diverticulum [2].
Computed tomography (CT) scan features compatible with appendiceal diverticulitis include rounded cystic outpouchings of the appendix with wall enhancement and solid enhancing masses emanating from the appendiceal wall [2]. This case is unique in that the diagnosis of appendiceal diverticulitis was made prospectively based on the sonographic findings and corroborated by contrast-enhanced CT.
Appendiceal diverticula are rare and often asymptomatic, making their clinical presentation challenging to distinguish from other appendiceal pathologies. When symptomatic, they may present with right lower quadrant pain, mimicking acute appendicitis, or with complications such as inflammation, perforation, or abscess formation. The diagnosis is frequently made intraoperatively or through histopathological examination.
Surgical management depends on the presentation and complications: appendectomy is typically sufficient in uncomplicated cases, whereas more extensive procedures may be required for perforated or inflamed diverticula.
Appendicectomy is the preferred treatment for acute appendiceal diverticulitis. A pathological evaluation of the resected specimen is essential for establishing a definitive diagnosis of appendiceal diverticulitis [5]. Yamana et al. demonstrated that the rate of perforation in cases of appendiceal diverticulitis is more than three times higher than that observed in acute appendicitis cases [5]. Furthermore, appendiceal diverticulitis is associated with an increased risk of concomitant appendiceal neoplasms, particularly mucinous adenomas and carcinoid tumors [5].
Given the high risk of diverticulitis, perforation, and the potential development of appendiceal malignancy, prophylactic elective appendicectomy is recommended for incidentally detected diverticular disease of the appendix. Importantly, appendiceal diverticulitis is typically diagnosed after pathological examination [1]. Additionally, there is no documented association between colonic diverticulosis and appendiceal diverticulosis.
4. Conclusion
The differential diagnosis of appendiceal diverticulitis in patients presenting with symptoms of acute appendicitis is crucial, as it is associated with a significantly higher rate of complications, including perforation, as well as an elevated risk of appendiceal neoplasms [5]. Given these potential risks, prophylactic appendicectomy is strongly recommended for cases involving non-inflamed diverticula [3]. Early identification and appropriate management of appendiceal diverticulitis can lead to better patient outcomes and reduce the likelihood of severe complications.
This version clarifies the importance of the differential diagnosis and highlights the need for timely intervention.
Author contribution
Med dheker Touati and Fahd Khefacha contributed to manuscript writing andediting, and data collection;
Mohamed Raouf BEN othmane and aymen Saidi contributed to data analysis;
Anis Belhadj and Faouzi chebbi contributed to conceptualization and supervision;
All authors have read and approved the final manuscript.
Patient consent
Written informed consent was obtained from the patient for the publication of this case report and its accompanying images. A copy of the written consent is available for the Editor-in-Chief of this journal to review upon request.
Ethical approval
Ethical approval is not applicable/waived at our institution “Mahmoud el Matri Hospital”. Due to the specific nature of case reports, which involve detailed descriptions of observations and interventions that have already been conducted on patients, as opposed to prospective studies involving planned interventions, our institution does not require formal ethical approval for such cases. We recognize the importance of ethics in medical research and are fully committed to upholding ethical standards in our medical and research practices.
Guarantor
Dr. Med Dheker TOUATI.
Research registration number
N/A.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of Generative AI and AI-assisted technologies in the writing process
AI tools were not used for the elaboration of the manuscript.
Funding
This research did not receive funding from any specific grant provided by public, commercial, or not-for-profit organizations.
Conflict of interest statement
No conflicts of interest.
Acknowledgements
Not applicable.
Data availability
The data supporting this case report are available upon request from the corresponding author.
References
- 1.Ergenç M, Uprak TK. Appendiceal diverticulitis presenting as acute appendicitis and diagnosed after appendectomy. Cureus. 14(3):e23050. [DOI] [PMC free article] [PubMed]
- 2.Chia M.L., Chan S.W.Y., Shelat V.G. Diverticular disease of the appendix is associated with complicated appendicitis. GE Port J. Gastroenterol. juill 2021;28(4):236–242. doi: 10.1159/000511822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ok L, S P, Mr I, Om A, M O, N R, B L, P I, Dw C, A SAAZ. Diverticulitis and diverticulosis of the appendix: a case series. Cureus [Internet] 28 oct 2022 [cité 15 oct 2024];14(10). Disponible sur: https://pubmed.ncbi.nlm.nih.gov/36447679/. [DOI] [PMC free article] [PubMed]
- 4.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A., Collaborators The SCARE 2023 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. Lond. Engl. 1 mai 2023;109(5):1136–1140. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Abdulmomen A.A., AlZahrani A.S., Mulla L.A.A., Alaqeel F.O. Acute perforated appendicitis associated with appendiceal diverticulitis in a young man: a case report with literature review. Am. J. Case Rep. 13 janv 2022;23 doi: 10.12659/AJCR.934838. (e934838-1-e934838-7) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting this case report are available upon request from the corresponding author.


