Visual Abstract
Abstract
Heavy menstrual bleeding (HMB) is a common symptom in adolescence, often leading to significant disruptions in daily life, such as school absences, shame caused by the stigma surrounding menstruation, and symptoms from iron deficiency. Further, HMB may be the first and/or only sign of an underlying bleeding disorder. Navigating the symptoms, effects, and treatments of HMB during adolescence requires a collaborative approach between the patient, caregivers, and healthcare providers. This work can be effectively and efficiently conducted in interdisciplinary clinics, where patients see hematology, gynecology, and adolescent providers. In these settings, healthcare providers exchange knowledge and expertise, after which they can reach a consensus for diagnostic evaluation and therapeutic intervention. Development and implementation of an interdisciplinary hematology and gynecology clinic can be challenging; however, the crucial rationale is that established clinics improve patient outcomes. Using an example interdisciplinary adolescent clinic, we outline the critical components needed to execute a successful clinic for adolescents with HMB and share key takeaways.
Learning Objectives
Identify at least three key components for interdisciplinary hematology/gynecology care for adolescents with heavy menstrual bleeding
Explain how interdisciplinary care is important for adolescent patients with heavy menstrual bleeding
Compare types of interdisciplinary hematology/gynecology adolescent clinics and illustrate how each can be effective in delivering expert-level care
Introduction
Menstruation challenges the hemostatic system and, in some cases, requires expertise from both hematology and gynecology. This is particularly true for individuals with inherited bleeding disorders (IBDs) or those who take medications with a high risk of bleeding. Unfortunately, HMB may go unrecognized and untreated because of the stigma of menstruation and a lack of education for patients and healthcare providers.1,2 Significant consequences of HMB include iron deficiency with or without anemia, hospitalizations, unnecessary procedures, decreased work/school participation, and decreased quality of life.3 Preteens and teens experience these consequences in an already challenging time, and HMB is self-reported in 34% to 58% of adolescents.4-6 Recognizing the specific needs of adolescents with HMB, interdisciplinary clinics have become increasingly common, with now over 40 combined hematology and gynecology or adolescent medicine clinics across the United States.7 In addition, the number of individuals with the potential to menstruate being seen at Hemophilia Treatment Centers (HTCs) is steadily increasing: the number of females treated at HTCs grew by 345% from 1990 to 20108 and increased further from 2010 to 2020.9 Navigating the needs of adolescents with reproductive tract bleeding requires specialized knowledge and care. Therefore, advocates from national organizations and education groups promote the development of combined clinics and encourage the pursuit of HMB-specific research to improve care.10,11 Here, we focus on the interdisciplinary adolescent heavy menses clinic, with highlights and examples from one clinic, including critical components and important lessons learned during development and implementation.
CLINICAL CASE
A 14-year-old with type 1 von Willebrand Disease (VWD) presents to a hematology clinic with their parent. The patient presented at 2 years of age with bruising, epistaxis, and a family history of VWD and was subsequently diagnosed with type 1 VWD. Menarche started at age 13, and monthly bleeding episodes last 8 to 9 days, with 5 to 6 heavy days that require changing an overnight pad every hour during the day. They frequently miss school out of the fear of leaking blood onto their clothes and currently report fatigue, lightheadedness, headaches, and pica. Their parent is concerned about the heavy periods but also worried about potential side effects of hormonal therapies.
Spots, Dots, and Clots origin story and location
The Oregon Health and Science University (OHSU) Spots, Dots, and Clots Interdisciplinary Hematology/Gynecology clinic (SDC) was established in July 2015 as a partnership between the OHSU Center for Women's Health (CWH) and the OHSU HTC, which is now known as the Hemostasis and Thrombosis Center. Before 2015, an HTC hematologist saw patients with HMB and a bleeding disorder and as needed would consult with obstetricians and gynecologists who shared the same physical space. Over time, referrals for adolescents increased, which made apparent the need for pediatric/adolescent expertise; however, younger patients rarely had established care with a gynecologist or adolescent healthcare provider.
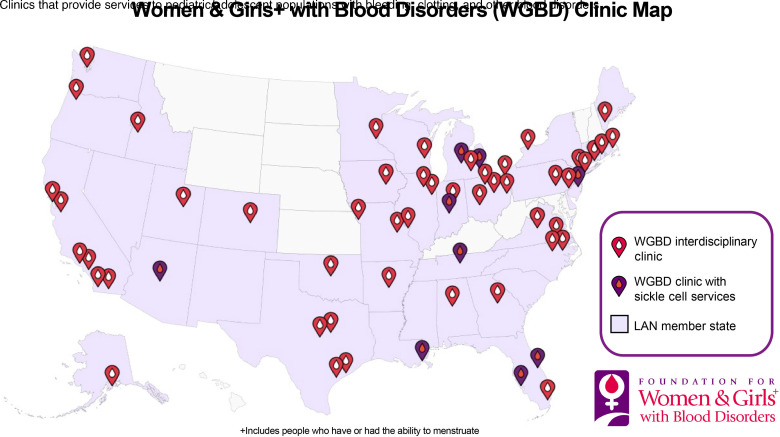
Approximately 2 years before establishing SDC, OHSU reached out to the Foundation for Women & Girls+ with Blood Disorders (FWGBD). The foundation ultimately created a Learning Action Network (LAN)7 and became instrumental in facilitating cross-institutional education and collaboration. To this day, the FWGBD LAN remains committed to establishing and implementing interdisciplinary clinics and maintaining a website on clinic locations (Figure 1). The Spots, Dots, and Clots name came from a contest held among pediatric hematology/oncology fellows to determine an appropriate name for the clinic. In 2015, there were only a few similar clinics across the country. The SDC team relied on their guidance and used their experience to build clinic templates and create referral procedures and billing processes.
Figure 1.
Map of clinics serving adolescents with heavy menses. Interdisciplinary clinics for adolescents with heavy menstrual bleeding (red with white drop) associated with the Foundation for Women & Girls+ with Blood Disorders are located throughout the United States. LAN, Learning Action Network.
SDC operates within CWH, which is on the main OHSU campus but across campus from the HTC. SDC patients connect to other HTC services as needed asynchronously. The CWH clinic space and support team are equipped for routine gynecologic health maintenance and procedures. While the primary patient population served at CWH is in the adult age group, the space is welcoming and adolescent friendly.
Key takeaways
Identify the physical space for the clinic. Points to consider include access to procedure space, lab testing, additional HTC needs, and adolescent or gynecology services. No one space will be perfect, but the SDC team prioritized access to gynecology procedure equipment over proximity to the HTC. Teams at other centers have prioritized HTC services. It is helpful to connect with other centers and interdisciplinary teams and learn approaches to establish/implement a clinic. Table 1 provides examples of clinic models.
Table 1.
Other clinic examples
| Example Clinic A | Example Clinic B | Example Clinic C | Example Clinic D | |
|---|---|---|---|---|
| Provider team | Pediatric hematologist + adolescent medicine NP | HTC NP + adolescent medicine physician | HTC pediatric hematologist + adolescent gynecologist | HTC pediatric hematologist + adolescent medicine physician |
| Location | HTC clinic | Adolescent medicine clinic | HTC clinic and gynecology clinic | HTC clinic |
| Clinic frequency | Two half-days/month | Four half-days/month | Asynchronous visits | One half-day/quarter in combination with HTC comprehensive clinic |
| Patient populations | Anyone diagnosed with IBD and HMB | Anyone with HMB needing evaluation for underlying bleeding disorder | Each provider sees patient with HMB, either with or without diagnosed IBD | Anyone with HMB needing evaluation for an underlying IBD; anyone diagnosed with IBD and HMB |
| Bonus features | Access to nutritionist on-site | On-site/day-of visit; intrauterine device insertion | HTC social worker evaluates each patient for underlying anxiety/depression | Access to all HTC services; space for IV infusions |
| Challenges | Growing patient population; no clinic rooms to expand to | Getting coagulation lab work, since coagulation lab is off-site | Visits are asynchronous; specialists consult with one another via multiple platforms | No access to gynecologic procedures |
| Opportunity | Add telehealth option; consider outreach clinic | Arrange labs to be done at HTC; coordinate referrals to other HTC services as needed | Organize pre- and post-clinic time to discuss patients, create treatment plans, and assign follow-up tasks | Arrange for procedures with a gynecologist who primarily sees adolescents |
HMB, heavy menstrual bleeding; HTC, Hemophilia Treatment Center; IBD, inherited bleeding disorder; NP, nurse practitioner.
Patient population, scheduling, and billing
Table 2 highlights new and return patient populations who may meet criteria to be scheduled in a combined clinic. SDC receives new patient referrals from internal providers (primary care or subspecialists) and external providers, with referrals routed through either pediatric hematology or gynecology. Scheduling for SDC is managed by the HTC team and includes staggered back-to-back 30-minute appointments with hematology and gynecology. At the time of scheduling, patients and caregivers are informed about the 2 visits and how the healthcare providers work together to provide optimal care. Billing for SDC occurs within each separate department, requiring separate insurance authorizations and copayments. An ongoing challenge is insurance denial of the 2 visits. Therefore, templated letters highlighting the importance of interdisciplinary care were created to appeal these decisions. Patients with HMB who already receive care at the HTC may require only a consultative visit or may choose to receive their ongoing bleeding disorder care at SDC.
Table 2.
Patient populations requiring evaluation and care at an interdisciplinary adolescent HMB clinic
| New patient chief complaints | Return patient chief complaints |
|---|---|
| IBD anticipating menses | HMB started on a new therapy in the last 3 months |
| IBD for management of HMB | HMB on a medication, now desiring contraception |
| Post-menstrual adolescent with HMB requiring evaluation for an underlying IBD | HMB with persistent iron deficiency |
| Adolescent with a personal or family history of thrombosis with or without HMB | HMB on a medication or starting a new medication for a comorbid condition (eg, depression) |
| Adolescent with a family history of IBD with HMB | |
| Adolescent with HMB and iron deficiency |
HMB, heavy menstrual bleeding; IBD, inherited bleeding disorder.
Key takeaways
Identify your patient population (Table 2). In doing so, referrals can be triaged appropriately, and clinic services will be used most effectively. Advertising services both within the institution and externally will improve access and may uncover patient populations with HMB who are undertreated at your institution (eg, patients with congenital heart disease on aspirin therapy experiencing HMB). Streamlining scheduling to one department can help mitigate duplicate work.
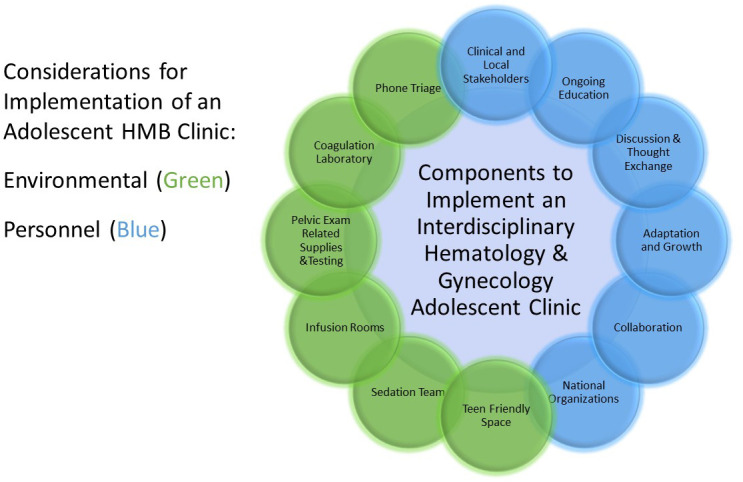
Clinic services including procedures and virtual clinics
SDC in-person clinic is staffed by rotating medical assistants (MAs) for patient rooming, including vital signs, medication updates, and room setup. Patients are given an SDC-specific intake form and a mood assessment questionnaire.12,13 As SDC prioritized gynecology services, each room has an exam bed that allows lithotomy positioning and is stocked with vaginal speculums and culture/cytology swabs. A procedure room is located nearby, and if needed, deep sedation (ie, for exam under anesthesia and intrauterine device placement) is provided by the pediatric anesthesia department. A nearby infusion room allows the SDC team to schedule medications requiring intravenous access such as IV iron. Period packs (small bags containing emergency period products) are provided to patients as needed. Importantly, laboratory testing is located on-site, including a coagulation laboratory. The healthcare team including MAs, nurses, anesthesia providers, and trainees are educated on adolescent HMB and the clinic as needed.
A virtual clinic operates similarly to the in-person clinic, with a separate appointment for each provider. Patients can access the MyChart online health portal; visits require the patient to have their own MyChart account or have their parent listed as a proxy on their account. At OHSU, proxy status changes at age 15, requiring a patient signature of consent for their parent to access their account. Patients can be seen virtually while residing in either Washington or Oregon, since both providers are licensed in both states. The proxy age and rules regarding where the patient is located may vary depending on local laws. If needed, staff from hematology or gynecology order laboratory or imaging studies to be performed at local facilities, and then the ordering provider reviews the test. Unfortunately, due to known inconsistencies in coagulation testing,14 patients may need to travel to OHSU for hemostasis testing.
During either the in-person or virtual clinic, psychological and social support issues are discussed. Commonly, patients report missing school because of heavy bleeding or needing to use the bathroom more frequently during the school day than is allowed at their school. Given these unique needs of adolescents with heavy menses, assistance is given to develop school plans, such as a 504 plan or a simple physician note. Additionally, patients commonly have comorbidities, including anxiety and depression; therefore, access to in-clinic or asynchronous social work or psychological support is crucial to optimize patient care.
Key takeaways
Identify available services and team members. Clinic development requires taking advantage of services available at your site, which includes physical location, amenities, and team members. Creating the appropriate environment (ie, services, team, location) is important to establish trust for adolescents. Incorporating virtual visits gives families flexibility to spend less time away from school and/or work, but it also poses difficulties in obtaining laboratory or imaging studies for some patients who may not have internet access.
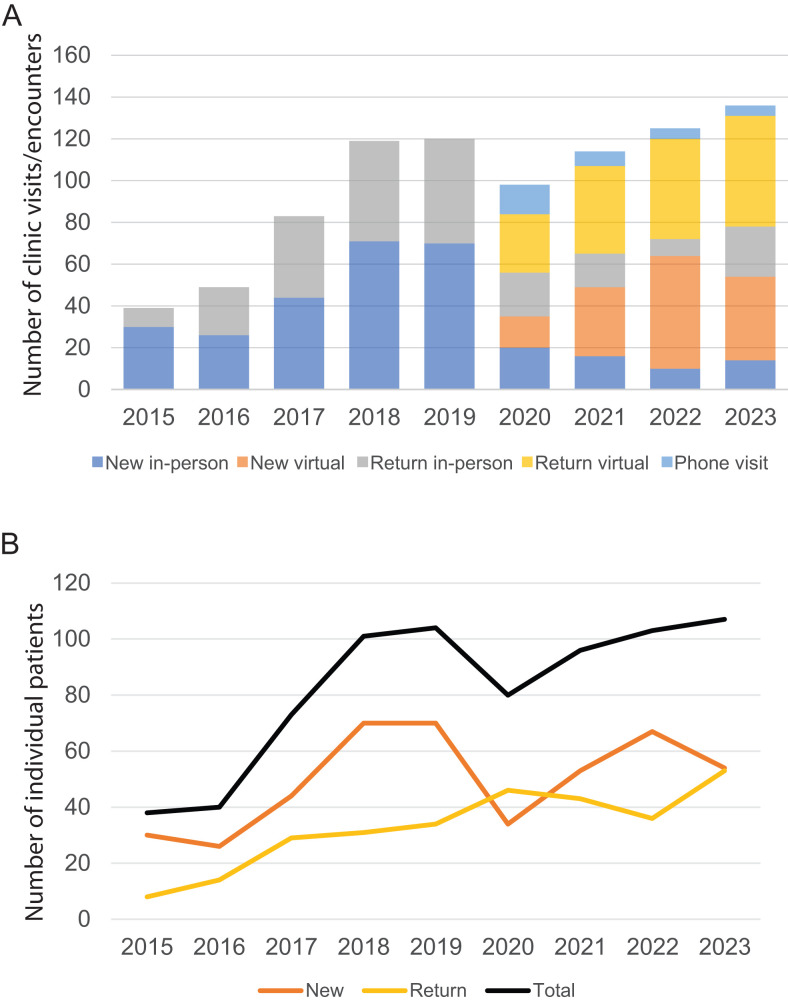
Clinic and patient volume
In 2015, the OHSU SDC clinic started with two half-day clinics per month. The SDC clinic switched to virtual clinics in the spring of 2020. In 2021, and again in 2023, two in-person clinic sessions per month were added to make two half-day virtual clinics and four half-day in-person clinics per month. Between 6 to 8 patients are seen per half-day clinic. Clinic volume grew over time with a slight downward trend in 2020, but now patient volume exceeds 2019 numbers (Figure 2). Given the number of providers participating in SDC, the team reached maximum clinic volume in 2024. Therefore, the current focus is on referral triage.
Figure 2.
OHSU Spots, Dots, and Clots clinic volume. Since emerging in 2015, the SDC clinic has seen overall steady growth in both clinic encounters and individual patient numbers. Figure 2A depicts the encounter types and numbers since the first clinic in 2015. Figure 2B provides individual patient numbers of total new patients (orange), total return patients (yellow), and total patients (black).
Key takeaways
Identify the need for clinic frequency and future growth. Interdisciplinary clinics can become a “if you build it, they will come” situation. Therefore, upfront considerations include a growth forecast and the future accommodation of additional clinics. Deciding if you want to see any patient with HMB or only patients with diagnosed bleeding disorders and HMB will significantly affect clinic volume. It is important to be clear about follow-up and to consider discharging patients from the clinic once their treatment plan is stabilized and follow-up care is secured either with a gynecologist, HTC, or primary care provider.
Interdisciplinary coordination
Coordination during clinic requires upfront planning. At SDC, first the gynecologist sees the patient, although the order is often switched depending on patient needs. After obtaining the health history, including menstrual and baseline bleeding history, the clinician provides initial counseling about management options and preferences. The providers then discuss the patient in real time. The second provider will complete their visit, which typically includes a targeted physical exam and more detailed bleeding and family history. Pelvic exams are rarely needed. Each provider documents their own patient encounter. While there is overlap between clinic notes, the focus is different. The gynecologist concentrates on menstrual history, adolescent reproductive health screening, and menstrual management counseling and options. The hematologist highlights the family and bleeding history, physical exam findings, and laboratory testing. Prescription management is divided between the providers: hormonal medications (gynecologist), antifibrinolytics (either provider), or products specific to the IBD (hematologist). Decisions on follow-up are discussed jointly after any imaging, procedures, and laboratory studies are completed and results shared. Once a plan is determined, it is communicated to the patient.
Key takeaways
Identify champions for the clinic. SDC emerged because a hematologist and gynecologist were passionate to see it happen. Communication is key. The two specialists need to determine patient needs and management plans, which heavily rely on communication. In the SDC clinic, this has worked best in a synchronous fashion. Over time, preferred practice patterns and management styles can be learned, and that knowledge can be applied when seeing patients outside the interdisciplinary clinic. In other models, the two providers may discuss all patients in person after the interdisciplinary clinic is completed. Given the involvement of multiple care providers (physicians, nurses, MAs, schedulers, etc.), it is equally important to establish processes for communication and delegation of duties in order to avoid missed messages and duplicative work. For example, patients should know who to call and when, and for what issues, while staff should know to whom they should report concerns.
Main principles and advantages of the interdisciplinary clinic
The primary mission of SDC is to diagnose and treat bleeding disorders presenting with heavy menstrual bleeding. The goals of the SDC clinic are to improve quality of life for young people and shorten the time from presentation to diagnosis and intervention.
Outlining the primary mission is critical to the success of any adolescent HMB program/clinic.
Objectives of an adolescent HMB clinic:
Expand screening for bleeding disorders by assessing those with heavy menstrual bleeding in order to provide a timely diagnosis
Enhance heavy menstrual bleeding and bleeding disorder education to trainees including medical students, pediatric and obstetrics/gynecology residents and fellows, and local and regional pediatric, adolescent, and gynecology providers
Use a shared decision-making model for management of heavy menstrual bleeding and iron homeostasis
Remove barriers to ensure appropriate access to evidence-based management strategies of heavy menstrual bleeding and iron deficiency
An adolescent HMB clinic requires a safe space for patients to discuss their care and make informed decisions. The clinic should strive to use language to reduce period stigma (ie, referring to medications as hormonal therapies). Importantly, providers should explain to patients the connections between their bleeding symptoms, the evaluation, and treatments. Several visits may be necessary to help a patient feel comfortable deciding on an intervention. The patient's goals should guide discussions and decisions. Clinic encounters must address barriers to school attendance, after-school activities participation, and social engagement.
Key takeaways
Identify goals and objectives to anchor the work performed and to guide growth. Keeping track of patient data in either a formal or informal way can help highlight the importance and effectiveness of establishing or expanding an HMB clinic. Because many adolescents experience HMB, any provider who encounters an adolescent with the potential for HMB should be provided with education to improve access to specialized interdisciplinary care. Encouraging learners to participate in an adolescent HMB clinic can help prepare the next generation of medical providers.
Other care delivery models for adolescents with HMB
Every healthcare system differs in the types of specialists, amenities, and physical spaces it offers to provide care. SDC is one example, but there are many ways to construct a team and clinic to manage adolescents with HMB (Table 1 gives examples of clinic descriptions). When an HMB clinic is primarily located within a hematology space, reproductive and gynecological care considerations should be integrated in the clinic, such as pregnancy testing, sexually transmitted infection screening, human papilloma vaccinations, Depo- Provera injections, and in-office ultrasound. If the adolescent heavy menses clinic is situated within a predominantly adult- focused gynecology space, then training should be provided in pediatric vital signs, phlebotomy, and infusion. When staffing a clinic with only one subspecialist, creating direct access plans for common needs from the other discipline becomes necessary.
Champions in hematology and gynecology or adolescent medicine (or both) can make the difference between a successful clinic and simply an idea. Once gathered, data should be presented to the appropriate administrative team regarding the importance and need for this care, thereby creating an additional advocate. As seen in the example clinic, it may take years to move from idea to implementation. Hopefully, with multiple champions and information from other centers, the time to establish a fully functioning clinic could significantly decrease and adolescents with HMB can obtain the care they desperately need.
Key takeaways
Identify current needs in your population, find stakeholders/ champions, and pave a way to deliver this important care. Explain the effects of HMB on adolescents to departments that have overlapping or similar missions, such as obstetrics/gynecology, adolescent medicine, family medicine, or pediatrics.
CLINICAL CASE (continued)
The 14-year-old was referred to SDC but continued to have HMB and anemia until seen 3 months later. During the SDC visit, the gynecologist provided education on a normal period, heavy period management, and the risks/benefits of medications. In a patient-centered fashion, preferred treatments were identified. The hematologist discussed how VWD impacts menstrual bleeding and the importance of decreasing menstrual bleeding to decrease iron losses. Laboratory studies showed significant iron deficiency anemia (hemoglobin 9.6 gm/dL, ferritin 3 mcg/L). The patient and parents opted to start treatment with tranexamic acid and an iron infusion. At their next follow-up, the patient's iron deficiency symptoms had improved, and tranexamic acid decreased menstrual bleeding by 40%. However, they still avoided activities because of leaking blood onto their clothes. After further discussion, the patient elected to have progestin therapy followed by intrauterine device placement to be performed under deep sedation.
Conclusion
The interdisciplinary adolescent hematology/gynecology clinic is designed to improve patient outcomes, and it requires stakeholders, champions, patients, and national advocacy groups working together.
Conflict-of-interest disclosure
Maureen Baldwin: no competing financial interests to declare.
Kristina M. Haley: no competing financial interests to declare.
Janice M. Staber: no competing financial interests to declare.
Off-label drug use
Maureen Baldwin: Nothing to disclose.
Kristina M. Haley: Nothing to disclose.
Janice M. Staber: Nothing to disclose.
References
- 1.Weyand AC, James PD. Sexism in the management of bleeding disorders. Res Pract Thromb Haemost. 2021;5(1):51-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Henry C, Filoche S.. Reflections on access to care for heavy menstrual bleeding: past, present, and in times of the COVID-19 pandemic. Int J Gynaecol Obstet. 2023;162(suppl 2):23-28. [DOI] [PubMed] [Google Scholar]
- 3.Kulkarni R. Improving care and treatment options for women and girls with bleeding disorders. Eur J Haematol. 2015;95 (suppl 81):2-10. [DOI] [PubMed] [Google Scholar]
- 4.Van ’t Klooster SJ, de Vaan A, van Leeuwen J, et al.. Heavy menstrual bleeding in adolescents: incidence, diagnostics, and management practices in primary care. Res Pract Thromb Haemost. 2023;7(7):102229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hadjou O-K, Jouannin A, Lavoue V, Leveque J, Esvan M, Bidet M.. Prevalence of dysmenorrhea in adolescents in France: results of a large cross-sectional study. J Gynecol Obstet Hum Reprod. 2022;51(3):102302. [DOI] [PubMed] [Google Scholar]
- 6.Nur Azurah AG, Sanci L, Moore E, Grover S.. The quality of life of adolescents with menstrual problems. J Pediatr Adolesc Gynecol. 2013;26(2):102-108. [DOI] [PubMed] [Google Scholar]
- 7.Foundation for Women & Girls+ with Blood Disorders. Foundation's learning action networks. Accessed 24 April 2024. https://www.fwgbd.org/learning-action-networks.
- 8.Baker JR, Riske B, Drake JH, et al.. US Hemophilia Treatment Center population trends 1990-2010: patient diagnoses, demographics, health services utilization. Haemophilia. 2013;19(1):21-26. [DOI] [PubMed] [Google Scholar]
- 9.Wheeler AP, Lim MY, Huguelet PS, et al.. Trends in dedicated care for females with bleeding disorders within U.S. hemophilia treatment centers. Am J Hematol. 2023;98(12):E399-E402. [DOI] [PubMed] [Google Scholar]
- 10.Byams VR, Miller CH, Bethea FM, Abe K, Bean CJ, Schieve LA. Bleeding disorders in women and girls: state of the science and CDC collaborative programs. J Womens Health (Larchmt). 2022;31(3):301-309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baldwin MK, Ahmadzia HK, Bartlett DL, et al.. Building the foundation for a community-generated national research blueprint for inherited bleeding disorders: research to advance the health of people with inherited bleeding disorders with the potential to menstruate. Expert Rev Hematol. 2023;16(supp1):71-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Inman DD, Matthews J, Butcher L, Swartz C, Meadows AL. Identifying the risk of suicide among adolescents admitted to a children's hospital using the Ask Suicide-Screening Questions. J Child Adolesc Psychiatr Nurs. 2019; 32(2):68-72. [DOI] [PubMed] [Google Scholar]
- 13.Ginsburg AD, Stadem PS, Takala CR, et al.. An examination of screening tools for collaborative care of adolescent depression. J Clin Psychiatry. 2018;79(4). [DOI] [PubMed] [Google Scholar]
- 14.Jaffray J, Staber JM, Malvar J, et al.. Laboratory misdiagnosis of von Willebrand disease in post-menarchal females: a multi-center study. Am J Hematol. 2020;95(9):1022-1029. [DOI] [PubMed] [Google Scholar]