Abstract
Objective
This study aimed to explore how dyadic coping (DC) influences the psychological resilience (PR) levels of patients with cervical cancer (CC) and their spouses.
Methods
From April to June 2024, this cross-sectional study involved 177 dyads of patients with CC and their spouses from the gynecology and oncology wards of two tertiary hospitals in Xinjiang. Data were collected through questionnaires on demographic information, clinical characteristics, the Resilience Scale, and the Dyadic Coping Inventory, all of which were self-report measures. The results were thoroughly analyzed utilizing the Actor-Partner Interdependence Mediation Model.
Results
The patients had a mean age of 49.94 ± 8.05 years (range: 26–64), with the majority being at stage II of CC. Their spouses had a mean age of 51.90 ± 8.02 years (range: 27–65). DC scores averaged 105.50 ± 23.98 for patients and 103.34 ± 22.26 for spouses, while PR scores were 63.51 ± 19.68 for patients and 67.44 ± 18.97 for spouses. Positive DC, which significantly correlated with higher levels of PR, was observed in patients with CC and their spouses (r = 0.285, P < 0.01; r = 0.697, P < 0.01). Conversely, a negative DC was associated with a lower PR (r = −0.187, −0.390; P < 0.01). Positive DC by patients with CC and their spouses equally improves both partners' PR. In contrast, negative DC by patients with CC and their spouses affects only their own PR.
Conclusions
Patients with CC and their spouses' PR is significantly influenced by both partners' DC behaviors. When both partners used positive coping strategies, their PR increased. Conversely, negative DC behaviors affected only patients' PR, possibly because of self-concealment and communication barriers, which may explain the lack of a reciprocal impact. Nurses should identify couples at risk for negative DC and implement resilience interventions to encourage both partners' engagement in positive coping.
Keywords: Cervical cancer, Psychological resilience, Dyadic coping, Actor-Partner interdependence model
Introduction
Cervical cancer (CC) is the leading gynecological malignancy in China.1 With the advent of early screening and the development of sophisticated treatments, the five-year survival percentage for CC patients in China has risen to 66.9%.2 However, prolonged treatment for CC often damages reproductive organs, impacting fertility and sexual function and leading to the emergence of adverse emotions.3,4 This leads to patients experiencing significant psychological distress. Influenced by traditional Chinese familial culture,5 primary caregivers are predominantly spouses who bear the majority of caregiving responsibilities; while fulfilling their caregiving roles, spouses must sustain the marital relationship, medical expenses, and they encounter psychological challenges such as anxiety and depression,6 which exacerbates their burden and negatively affects their mental health. Consequently, spouses often become “invisible patients,”7 meaning patients' and spouses' psychological well-being are significantly impacted.8
Psychological resilience (PR) refers to an individual's ability to effectively cope with and adapt to life's challenges and adversities. In this study, PR specifically refers to the ability of patients and their partners to cope with the stress and challenges related to cervical cancer and its treatment.9 PR was assessed using the 14-item Resilience Scale (RS-14), a validated tool that measures resilience across various dimensions, including personal capacity and positive cognition. Individuals who maintain their mental well-being under stress are typically those who can more effectively adapt to the difficulties engendered by illness, indicating a high level of PR.10 Additionally, PR is influenced not only by individuals coping mechanisms but also by the dyadic coping (DC) strategies of spouses.11 A study12 conducted on people with colorectal cancer found a significant association between the DC strategies of patients, their spouses and their PR. The patients' DC behaviors significantly impacted their quality of life, particularly their mental health, while spouses' coping strategies also significantly influenced their psychological well-being. Furthermore, research has exhibited that the more prevalent these DC behaviors are—such as stress communication, joint problem-solving, mutual emotional support, and proactive emotional regulation—the more likely both individuals are to maintain enhanced PR, thereby facilitating their adaptation to the experience with cancer.13,14 Consequently, understanding PR and highlighting the importance of maintaining mental well-being and effectively coping with illness and its associated stress, is pivotal.15
DC involves the coping styles and strategies adopted by patients and their spouses when facing the challenges of CC. The systemic-transactional model (STM) identifies positive DC as including stress communication, supportive DC, common DC, and delegated DC, while hostility, ambivalence, and protective buffering are seen as negative DC.16 In particular, stress communication, which refers to the expression one's stress, and supportive DC strategies—such as problem-focused or emotional support offered by one partner when the other is under stress—plays a significant role in managing relational stress. Delegated DC, where one partner assumes tasks and responsibilities to alleviate the other's stress, and common DC, where both partners collaboratively address stressors, have been observed to enhance marital satisfaction,17 reduce stress,18,19 and promote psychological well-being. However, research suggests that while stress communication,20 supportive DC, and common DC may foster relational harmony and alleviate stress, they may simultaneously impose a psychological or physical burden on either the patient or the partner.21 Conversely, negative DC, characterized by maladaptive interactions in response to stress, and protective buffering—where one partner hides their stress to shield the other— been linked to lower marital satisfaction,22 diminished quality of life,13 and exacerbated symptoms of anxiety and depression.23
PR is influenced not only by individual coping mechanisms, but also by the DC strategies couples employ.11 Positive DC enhances psychological wellbeing, bolsters familial resilience in the face of illness, and strengthens trust.24 It is essential to help patients and caregivers alleviate each other's stress, improve their PR, and maintain relationship stability.13 Conversely, previous studies13 have shown that negative DC strategies can increase psychological stress and conflict between patients and family members, deplete psychological resources, and have detrimental effects on both partners' PR.12 A qualitative study by Kayser et al.25 on cancer couples in the U.S., India, and China found that most Asian couples perceive the disease as beyond their control, leading them to accept or avoid it rather than adopt proactive coping strategies. This tendency may pose additional challenges for Asian breast cancer couples in managing disease-related stress. Given the cultural differences and the unique characteristics of CC as a reproductive malignancy, its impact extends beyond the patient's health and significantly affects marital relationships.26 The treatment process often involves sensitive aspects such as reproductive function and sexual health, placing substantial emotional and psychological pressure on couples.27 Therefore, the unique pathological features of CC present couples with more complex emotional and relational challenges compared to other types of cancer, emphasizing the importance of examining DC in the context of PR to better address their mental health needs.
While most studies focus on the relationship between familial resilience and DC in patients and their family caregivers, the dynamic interactions between PR and DC from a couple-centered perspective, especially between patients with cancer conditions and their spouses, have been insufficiently explored. The impact of different coping strategies on PR within these dyads has rarely been reported, leaving the question of how DC between the patient and caregiver affects the psychological well-being of the dyad unanswered.
Xinjiang, located in the northwest of China, is a province with various ethnic groups, wherein Han Chinese people constitute 42.24% of the population, and ethnic minorities account for the remaining 57.76%.28 Regional factors such as lifestyle, dietary practices, and health care conditions may contribute to the high incidence of CC in Xinjiang.29 Ethnic minorities tend towards early marriage and childbearing, or having multiple offspring post-marriage, which is intrinsically connected to their cultural traditions that encompass familial structures, matrimonial customs, and hygienic practices. The multi-ethnic cultural context potentially influences how couples navigate the diagnosis and treatment of CC. Still, existing research fails to explore coping strategies and PR within this diverse cultural framework. Therefore, this study, which investigated the relationship between DC mechanisms and PR in Xinjiang, a region characterized by ethnic diversity, contributes to the broader application of STM theory across various cultural contexts, providing a basis for developing more effective dyadic resilience interventions to enhance the mental well-being of couples coping with cervical cancer.
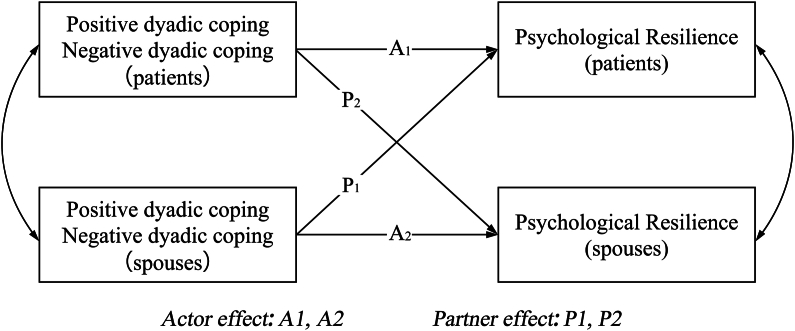
The actor-partner interdependence model (APIM) developed by Kenny et al.30 is a model researchers use to investigate how independent variables relate to dependent variables. In this model, a dependent variable related to an individual, which is influenced by an independent variable (actor effect), is also affected by an independent variable related to another entity within a defined range (partner effect). Consequently, via the APIM, the coping strategies and PR of individuals, referred to as actors, and their partners, referred to as partners, can be evaluated by exploring the interaction patterns within partners' collaborative coping processes. Therefore, the objectives of this study were to (1) examine the differences in DC and PR between individuals diagnosed with CC and their spouses and (2) investigate how the actor-partner effect between DC and PR in patients with CC and their spouses operates. This study posited two hypotheses (Fig. 1):
-
(1)
Within the actor-effect framework, the positive/negative DC strategies utilized by patients with CC and their spouses are linked to their own PR.
-
(2)
Within the partner effect framework, the positive/negative DC strategies of patients with CC and their spouses were linked to their partner's PR.
Fig. 1.
Hypothesis Model of Dyadic Coping and Psychological Resilience in Cervical Cancer Patients and their spouses.
Methods
Study design and participants
A convenience sampling method was used to recruit patients with cervical cancer and their spouses who were admitted to two tertiary hospitals in Urumqi City between April and June 2024. The inclusion criteria were as follows: (1) patients meeting the 2022 China National Guidelines for CC;31 (2) patients aged ≥ 20 and spouses aged ≥ 22 years,32 with spouses as primary caregivers; (3) patients with stable conditions, able to understand and answer questions independently; and (4) awareness of their condition and provision of informed consent. The exclusion criteria were as follows: (1) patients with dysfunction in other organs or a relapse of malignant tumors; (2) participants in other similar research projects; and (3) history of cognitive dysfunction or mental disorder. Patients with these conditions were excluded because cognitive dysfunction or mental disorders could compromise their ability to accurately complete questionnaires and self-report data, potentially affecting the reliability of the study results.
This research utilized G∗Power 3.1 software to determine the required sample size. The power (1-β) was set at 0.95, the significance level (α) at 0.05, and the effect size (d) at 0.5. Based on these parameters, a total sample size of 210 participants was required, with 105 participants per group for a two-tailed t-test comparing two independent means. Taking into account a 20% dropout rate, the final sample consisted of 263 participants, including 132 CC patients and 132 spouses. The study collected 196 couples. However, 19 dyads declined to participate for reasons such as lack of interest, worsening illness, and lack of availability. Ultimately, 354 valid questionnaires were collected (effective response rate = 90%.), fulfilling the requirements for structural equation modeling.
Instruments
Socio-demographic and clinical data
The researcher designed a general information questionnaire to gather demographic data such as the patient's age, monthly income level, number of children, occupation, education level, TNM disease stage, treatment method, and time since diagnosis. Non-disease-related demographic information was collected from patients' spouses.
Chinese version of the Dyadic Coping Inventory
Xu Feng et al.33 in 2016 translated and adapted the DC inventory (DCI) into Chinese, which was subsequently used to measure DC levels in couples dealing with CC. The DCI, which consists of 35 items, is categorized into five distinct dimensions. These dimensions include stress communication, supportive DC, delegated DC, common DC, and negative DC. Stress communication, supportive DC, delegated DC, and common DC are classified under a broader positive DC dimension. The questionnaire employs a 5-point Likert scale ranging from 1 (rarely) to 5 (frequently), resulting in a score ranging from 35 to 175. The Cronbach's α coefficients were 0.939 for patients with CC and 0.943 for their spouses.
Chinese version of the resilience scale
Ni Qianyu et al.34 translated and adapted the RS-14 resilience scale in 2013, and it has been used to assess PR levels in couples with CC. While utilizing the scale, which comprises 14 items evaluating personal ability and positive cognition, each item was assessed by participants using a 7-point Likert scale, resulting in scores ranging from 14 to 98, with higher scores indicating greater PR. The Cronbach's α coefficients were 0.962 for patients with CC and 0.963 for their spouses.
Data analysis
A questionnaire survey was administered by two uniformly trained nursing graduate students. The surveys were distributed face-to-face to couples during hospitalization between 19:00 and 21:00. After obtaining informed consent, patients and their spouses independently completed separate questionnaires to avoid interference. The completed questionnaires were immediately collected, checked for completeness, placed in sealed file bags, and matched with participants' hospitalization numbers. If a couple's questionnaire was invalid, both questionnaires were excluded. For individuals with vision, language, or comprehension difficulties, the investigators read each question aloud and accurately recorded participants' responses.
Ethical considerations
This study was approved by the Ethics Committee of Xinjiang Medical University (IRB No. XJYLDXR20240411001). It was subsequently approved by the heads of the hospital nursing and clinical departments where the study was conducted. The researchers explained the study's aims, significance, and content to the participants. Informed agreement was received from both the patients and their spouses. They were informed that their participation was voluntary and that they could withdraw at any time without any consequences.
Statistical analysis
For data analysis, SPSS 28.0 software was employed, whereby measurement data with a normal distribution were articulated as Mean ± SD and count data were delineated using frequency and percentage. To compare the DC and PR between couples, paired-sample t-tests were conducted. Pearson's correlation coefficient was used to investigate the relationship between DC and PR among couples.
The APIM model of PR in patients with CC and their spouses was constructed using AMOS 26.0, to focus on the impact of DC on both partners. The 95% confidence interval was estimated using the Bootstrap method with 5000 samples. The results were considered statistically significant at P < 0.05. Various criteria were used to evaluate the model's fit, including the ratio of χ2 to its degrees of freedom (χ2/df < 3.0), the Goodness of Fit Index (GFI > 0.90), the Normed Fit Index (NFI > 0.90), the Tucker–Lewis Index (TLI > 0.90), the Comparative Fit Index (CFI > 0.90), and the Root Mean Square Error of Approximation (RMSEA < 0.08).
Results
Socio-demographic and clinical characteristics of the sample
Patients with CC aged between 26 and 64 years (average age 49.94 ± 8.05 years), and their spouses, whose ages ranged from 27 to 65 years (average age 51.90 ± 8.02 years), participated in the study. Most patients had been married for 30 years or more (81, 45.8%); 47.5% had ≥ 3 children. The participants' educational level was predominantly primary school or below (91, 51.4%; 74, 41.8%). Most participants were farmers (76, 42.9%; 83, 46.9%). Most couples had a monthly family income of 1000–3000 (81, 46.0%) RMB. The disease stage was predominantly stage II (84, 47.5%), with 41.2% of patients being diagnosed less than three months prior (Table 1).
Table 1.
General information about cancer couples (N = 177 dyads).
| Characteristics | Patients (n = 177) |
Spouses (n = 177) |
|---|---|---|
| n(%) | n(%) | |
| Age (years) | ||
| 21–40 | 40 (22.6) | 26 (14.7) |
| 41–50 | 59 (33.3) | 51 (28.8) |
| 50–60 | 56 (31.6) | 72 (40.7) |
| > 60 | 22 (12.4) | 28 (15.8) |
| Ethnic | ||
| Han | 57 (32.2) | 55 (31.1) |
| Ethnic group | 120 (67.8) | 122 (68.9) |
| Marriage duration (years) | ||
| ≤ 20 | 39 (22.0) | – |
| 21–29 | 57 (32.2) | – |
| ≥ 30 | 81 (45.8) | – |
| Number of children | ||
| ≤ 1 | 35 (19.8) | – |
| 2 | 58 (32.8) | – |
| ≥ 3 | 84 (47.5) | – |
| Residence | ||
| Cities and towns | 103 (58.2) | |
| Rural | 74 (41.8) | |
| Occupations | ||
| Farmer | 76 (42.9) | 83 (46.9) |
| Worker | 39 (22.0) | 15 (8.5) |
| Institutions/civil servants | 14 (7.9) | 32 (18.1) |
| Self-employed/other | 27 (15.3) | 20 (11.3) |
| Retirement | 21 (11.9) | 27 (15.3) |
| Education level | ||
| Primary school and below | 91 (51.4) | 74 (41.8) |
| Junior high school or below | 32 (18.1) | 42 (23.7) |
| Senior high school or vocational secondary school | 24 (13.6) | 34 (19.2) |
| College and above | 30 (16.9) | 27 (15.3) |
| Monthly household income (RMB) | ||
| 1000a–3000b | 81 (45.8) | – |
| 3000–5000c | 62 (35.0) | – |
| > 5000 | 34 (19.2) | – |
| TNM stages | ||
| I | 50 (28.2) | – |
| II | 84 (47.5) | – |
| ≥ III | 43 (24.3) | – |
| Times since diagnosis (months) | ||
| < 3 | 73 (41.2) | – |
| 3–6 | 65 (36.7) | – |
| 6–12 | 39 (22.0) | – |
A hyphen (“-”) indicates that the family information is shared by the patient and spouse. The following currency conversions apply: a = ¥1000 ≈ $137.14, b = ¥3000 ≈ $412.23, c = ¥5000 ≈ $687.06. T:Tumor, N:regional lymph node, M:metastasis
Comparison of the PR and DC of patients with CC and spouses
The paired t-test results showed that patients had a mean DC score of 105.50 ± 23.98, while spouses had a score of 103.34 ± 22.26, demonstrating no significant difference (P > 0.05). In examining the disparate dimensions of DC, specifically in stress communication and delegated DC (P < 0.05). In contrast, no important distinctions disparities were evident in supportive, common, or negative DC.
Patients' PR score was (63.51 ± 19.68), compared to (67.44 ± 18.97) for spouses, revealing statistically significant distinctions between the two groups (P < 0.05). Notably, patients had a significantly higher score on the personal capacity dimension when compared with their spouses (P < 0.05). However, the disparity observed in the positive cognition dimension was not statistically significant (Table 2).
Table 2.
Mean scores of variables and Dimensions (N = 177, Mean ± SD).
| Characteristics | Patients | Spouses | t | P |
|---|---|---|---|---|
| Dyadic coping | 105.50 ± 23.98 | 103.34 ± 22.26 | 0.384 | 0.701 |
| Stress communication | 23.11 ± 7.66 | 22.11 ± 7.89 | 2.036 | 0.043 |
| Supportive dyadic coping | 31.04 ± 10.95 | 31.51 ± 9.20 | −0.807 | 0.421 |
| Common dyadic coping | 13.84 ± 4.76 | 13.74 ± 4.67 | 0.290 | 0.772 |
| Delegated dyadic coping | 13.05 ± 4.26 | 12.32 ± 3.52 | 2.054 | 0.041 |
| Negative dyadic coping | 24.46 ± 9.51 | 23.66 ± 7.20 | 0.997 | 0.320 |
| Psychological resilience | 63.51 ± 19.68 | 67.44 ± 18.97 | −2.264 | 0.025 |
| Personal capacity | 42.25 ± 13.89 | 48.11 ± 13.41 | −2.339 | 0.020 |
| Positive cognition | 18.26 ± 6.20 | 19.33 ± 5.93 | −1.929 | 0.055 |
t, paired sample t test, bold indicates, P <0.05.
Correlations between psychological resilience and dyadic coping
A positive correlation was observed between patients with CC and their spouses' PR (r = 0.285, P < 0.01). Patients' positive DC was correlated with that of their spouses (r = 0.697, P < 0.01), same with patients' negative DC (r = 0.215, P < 0.01). In the analysis, positive DC among patients with CC correlated with both their own and their spouses' PR (r = 0.568, 0.623; P < 0.05). Similarly, spouses' positive DC correlated with their own PR and their partners' (r = 0.668, 0.529; P < 0.01). Notably, negative DC in patients with CC and their spouses was negatively correlated with their own respective PR (r = −0.187, −0.390; P < 0.01; Table 3).
Table 3.
Relationship between dyadic coping and psychological resilience scores among cervical cancer patients and their spouses (r).
| Variables | Patient |
Spouse |
|||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | ||
| Patient | 1.Psychological resilience | 1 | |||||
| 2.Positive dyadic coping | 0.568∗∗ | 1 | |||||
| 3.Negative dyadic coping | −0.187∗ | −0.198∗∗ | 1 | ||||
| Spouse | 4.Psychological resilience | 0.285∗∗ | 0.623∗∗ | −0.145 | 1 | ||
| 5.Positive dyadic coping | 0.668∗∗ | 0.697∗∗ | −0.277∗∗ | 0.529∗∗ | 1 | ||
| 6.Negative dyadic coping | −0.039 | −0.280∗∗ | 0.215∗∗ | −0.390∗∗ | −0.181∗ | 1 | |
∗∗P<0.01, ∗P<0.05.
Actor-Partner interdependence model
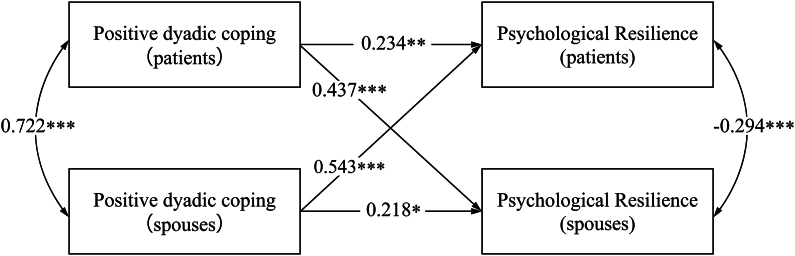
Acceptable fit indices for APIM Model 1 were observed: χ2/df = 2.044, RMSEA = 0.077, GFI = 0.920, TLI = 0.968, NFI = 0.955, and CFI = 0.967. Fig. 2 illustrates the standardized coefficients.
Fig. 2.
The Actor-Partner interdependence Model of Psychological Resilience and Positive Dyadic Coping in Cervical Cancer patients and their spouses, ∗P < 0.05, ∗∗P < 0.01, ∗∗∗P < 0.001.
As depicted in Fig. 2, positive DC by patients with CC and their partners significantly increases their own respective PR (actor effects: β = 0.234, P < 0.01; β = 0.218, P < 0.05). Patients and partners' supportive DC significantly enhanced their partners' PR (partner effects: β = 0.473, P < 0.001; β = 0.543, P < 0.001). There is a positive correlation in the mutual influence of positive DC between patients with CC and their spouses (β = 0.722, P < 0.001). An association was observed between spouses' positive DC and both their own PR and the patients' PR (β = 0.239, P < 0.01).
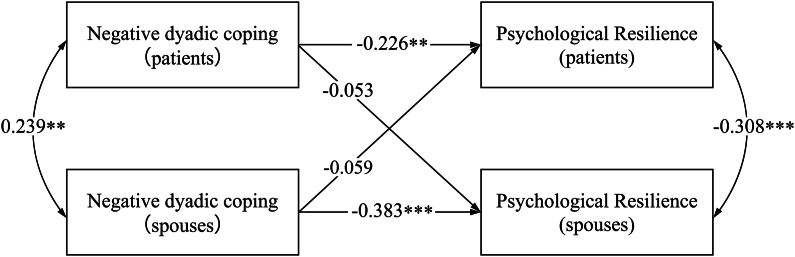
Acceptable fit indices for APIM model 2 were observed: χ2/df = 1.217, RMSEA = 0.035, GFI = 0.903, TLI = 0.985, NFI = 0.933, and CFI = 0.987. Fig. 3 illustrates the standardized coefficients.
Fig. 3.
The Actor-Partner interdependence Model of Psychological Resilience and Negative Dyadic Coping in Cervical Cancer patients and their spouses, ∗P < 0.05, ∗∗P < 0.01, ∗∗∗P < 0.001.
As depicted in Fig. 3, negative DC by both patients with CC and their partners significantly lowers their own respective PR (actor effects: β = −0.226, P < 0.01; β = −0.383, P < 0.001). Regarding partner effects, negative DC by patients and their partners did not significantly predict the other partner's PR.
Discussion
Dyadic coping and psychological resilience in cervical cancer patients and their spouses
The results revealed low-scoring overall DC scores for CC patients (105.50 ± 23.98) and their partners (103.34 ± 22.26), significantly lower than those reported by Chen et al.35 This can be attributed to most patients being in the early stages of the illness, where uncertainties surrounding treatment and prognosis, coupled with low controllability, adversely impact their DC abilities.36 On the other hand, most surveyed couples reside in rural areas of Xinjiang and have lower educational levels, which limits their access to medical resources and accurate information about the disease, leading to misconceptions that hinder effective DC.37
Consistent with prior research,38 our study indicates that the PR scores of patients with CC are significantly lower compared to their spouse (P < 0.05). This discrepancy likely arises from the localization and treatment of CC, which involves damage to or removal of female reproductive organs, leading to negative emotional responses. Female patients, often play multiple family and social roles. When illness disrupts these roles, adaptive capabilities are reduced, leading to lower PR levels.8 Additionally, to avoid burdening their spouses, these patients frequently conceal their emotions, which further diminishes their PR levels. Spouses of patients with CC serving as primary caregivers and decision-makers in treatment, tend to recover their resilience swiftly after the initial shock of diagnosis, subsequently providing emotional and practical support to the patients.39
Actor-Partner interdependence mediation model of dyadic coping and psychological resilience in cervical cancer patients and their spouses
The study indicated that positive DC between patients and their spouses enhanced PR, whereas negative DC diminished PR. This suggests that individuals' perceptions of their couples' DC are linked to their own PR. These results align with previous research that utilized the APIM to examine dyadic data in couples.13
This study demonstrated that DC was linked to PR through the contributions of both actors and partners in patients with CC and their spouses. This revealed that positive DC behaviors in patients with CC could transform PR into a protective factor, creating a buffering effect that enables patients to mobilize positive psychological resources against disease threats, similar to previous studies.13 Additionally, as primary caregivers, spouses are pivotal in mitigating disease-related stress. Their engagement in positive DC behaviors significantly contributed to patients feeling supported, eliciting positive feedback, enhancing caregivers' sense of value, and promoting positive psychological changes.40 Concerning partner effects, positive DC by both patients and spouses significantly enhanced the other partner's PR. A plausible explanation is that when patients with CC, through common DC, stress communication, and supportive DC, provided their spouses with positive feedback, they could normalize adversity and strengthen their inner resilience, thus activating their psychological defense mechanisms.41 Treatments for CC, which involve the female reproductive organs, can engender feelings of inferiority during treatment and in daily life.42 However, when spouses adopted positive DC strategies, they provided emotional solace and psychological support and bolstered patients' self-confidence and coping capacities. This alleviates feelings of inferiority, fosters positive emotions, and reinforces PR.13 This cycle of mutual support and positive DC ultimately enhances both partners' PR and adaptability to adversity.
Our study indicates that negative DC in patients with CC and their spouses led to actor effects on PR. However, the partner effects were not significant, which is consistent with previous research.43 Analyzing the underlying reasons, it is evident that CC involves female reproductive organs, leading patients to exhibit negative emotional or affective responses to their impairment or loss. To avoid further burdening their spouses, patients often conceal their emotions, resorting to denial and avoidance coping strategies.44 This, in turn, hinders self-disclosure and diminishes the couple's coping abilities, potentially causing emotional instability in both partners.45 The inability to adequately respond to each other's emotional needs hampers the weakening of familial cooperation.24 In addition, among minority ethnic groups, men who uphold profound family values and assume substantial economic and domestic responsibilities are inclined to prioritize pragmatic problem-solving rather than emotional expression, especially when confronted with the illness of their spouses. Furthermore, owing to the typically high number of children in these families, the allocation of men's time and energy across numerous familial duties becomes more dispersed, consequently impeding their ability to concentrate on the psychological needs of the patient, thereby resulting in the neglect of mental health support. Men typically shoulder their life and illness pressures independently, are not adept at expressing emotions or providing solace, and are reluctant to discuss illness-related issues with their wives. They often avoid emotional communication and discussions about coping with illness-induced stress, preferring to conceal their own negative emotions.44 Consequently, when one partner confronts negative thoughts and behavior, the other senses dependency and responds with protection and care instead of experiencing stress.46 These actions were intended to shield each other from negative emotional impacts. Accordingly, clinical caregivers must identify patients with CC and their spouses who adopt negative DC strategies, paying close attention to sex differences in their disease coping processes. Guiding couples in coping skills training is essential to enhance communication and coordination of coping strategies between partners.
Limitations
This study had several limitations. First, ethnic categories were not delineated during data collection, and future research could explore disparities among different ethnic groups. Since the majority of the study participants were diagnosed with early-stage cancer, the generalizability of the findings to patients with advanced cancer is limited. Future research should involve longitudinal studies to explore dynamic trends among variables at different disease stages. Finally, the study included only patients diagnosed with CC and their spouses in Xinjiang, a province with diverse ethnic groups in Western China. Considering the cultural differences between these groups, caution should be exercised when applying the results of this study to other cultures or populations.
Conclusions
By employing APIM, this study investigated how DC and PR interact and affect one another among CC patients and spouses from dyadic angles. By transitioning from the individual to the dyadic level, this research addresses the limitations of previous studies, which indicate that positive DC strategies adopted by CC patients and their spouses affect their PR and partners' resilience. Clinical staff can enhance support for CC patients and their spouses through targeted interventions. For instance, organized couple-focused sessions encourage shared problem-solving and emotional communication, strengthening DC for both partners. Incorporating stress-management techniques, such as guided breathing exercises and mindfulness tailored for couples, effectively alleviates emotional strain. Therefore, resilience-building exercises, such as cognitive behavioral therapy (CBT), enhance coping skills. These interventions, offered both in-person and online, assist in alleviating anxiety and emotional stress, enhance coping abilities and foster healthier relationships during challenging times. Besides, institutions should implement structured screening protocols to identify couples with low DC levels early and integrate regular follow-up programs that facilitate long-term monitoring. Additionally, health care institutions should invest in training programs to equip clinical staff with the skills needed to deliver couple-focused interventions and encourage multidisciplinary collaboration to ensure comprehensive support for patients and their spouses. These strategies will improve patient outcomes and promote emotional and psychological well-being.
CRediT authorship contribution statement
Tianruixue Zhang: Conceptualization; Methodology; Data curation; Formal analysis; Writing – Original draft preparation. Ping Yan: Resource, Validation, Review & Editing, Funding acquisition. Zhisheng Huang: Resources and Software, Methodology. Li Liu: Quality appraisal, Review & editing. Yanhui Zhou: Conceptualization, Methodology, Writing & Review. Yuqiao Xiao & Guiyuan Ma: Review & Editing. Jia Xu & ZiXuan Liu: Collect, and Data curation; Can Gu: Supervision, Methodology, Project Administration, Review and Editing. All authors had full access to all the data in the study, and the corresponding author had final responsibility for the decision to submit for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Ethics statement
Ethical approval was obtained from the Ethics Review Committee of Xinjiang Medical University (IRB No. XJYLDXR20240411001). All participants provided written informed consent.
Funding
This study was supported by National Nature Science Foundation in China (82272924), China Medical Board Open Competition Program (#20–369), China Community Health Serives Program (2023YC01), Hunan Provincial Nature Science Foundation (2022JJ30774), Research and Innovation Team Project, Xinjiang Medical University (Grant No. XYD2024C06). Foundation of Philosophy and social sciences of Hunan Province (19YBA348). The founders had no role in considering the study design or in the collection, analysis, interpretation of data, writing of the report, or decision to submit the article for publication.
Data availability statement
The data for the results of this study are available at the authors' request. The data are not publicly available due to privacy restrictions, as they contain sensitive information regarding both patients with cervical cancer and their spouses. Specifically, the data include personal health information, psychosocial coping strategies, and detailed questionnaire responses, which could lead to the identification of participants and reveal private aspects of their relationships and mental health.
Declaration of generative AI and AI-assisted technologies in the writing process
No AI tools/services were used during the preparation of this work.
Declaration of competing interest
The authors declare no conflict of interest. The corresponding author, Prof. Can Gu, is an editorial board member of Asia–Pacific Journal of Oncology Nursing. The article was subject to the journal's standard procedures, with peer review handled independently of Prof. Can Gu and their research groups.
Acknowledgments
The author extends sincere appreciation to the patients and their spouses who contributed their time to this study, as well as to the clinical nurses whose support in the data collection process was invaluable.
References
- 1.Zheng R.S., Chen R., Han B.F., et al. Cancer incidence and mortality in China, 2022. Zhonghua Zhongliu Zazhi. 2024;46(3):221–231. doi: 10.3760/cma.j.cn112152-20240119-00035. [DOI] [PubMed] [Google Scholar]
- 2.Zeng H., Zheng R., Sun K., et al. Cancer survival statistics in China 2019–2021: a multicenter, population-based study. J National Cancer Center. 2024 doi: 10.1016/j.jncc.2024.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang C.M., Sung F.C., Mou C.H., Liao C.H., Wang P.H., Shieh S.H. Anxiety and depression risk in Taiwan women with breast cancer and cervical cancer. Front Oncol. 2022;12 doi: 10.3389/fonc.2022.946029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peterson C.E., Silva A., Goben A.H., et al. Stigma and cervical cancer prevention: a scoping review of the U.S. literature. Prev Med. 2021;153 doi: 10.1016/j.ypmed.2021.106849. [DOI] [PubMed] [Google Scholar]
- 5.Chen X., Wang Z., Zhou J., et al. The impact of self-perceived burden, caregiver burden, and dyadic coping on negative emotions in colorectal cancer patient-spousal caregiver dyads: a dyadic analysis. Front Psychol. 2023;14 doi: 10.3389/fpsyg.2023.1238924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bodschwinna D., Ernst J., Mehnert-Theuerkauf A., Gündel H., Weissflog G., Hönig K. Dyadic coping and social support: various types of support in hematooncological patients and their spouses-Associations with psychological distress. Psycho Oncol. 2021;30(7):1041–1050. doi: 10.1002/pon.5631. [DOI] [PubMed] [Google Scholar]
- 7.Ketcher D., Otto A.K., Vadaparampil S.T., Heyman R.E., Ellington L., Reblin M. The psychosocial impact of spouse-caregiver chronic health conditions and personal history of cancer on well-being in patients with advanced cancer and their caregivers. J Pain Symptom Manag. 2021;62(2):303–311. doi: 10.1016/j.jpainsymman.2020.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Landolt S.A., Weitkamp K., Roth M., Sisson N.M., Bodenmann G. Dyadic coping and mental health in couples: a systematic review. Clin Psychol Rev. 2023;106 doi: 10.1016/j.cpr.2023.102344. [DOI] [PubMed] [Google Scholar]
- 9.Sun H., Qin Y., Hengudomsub P. Factors associated with resilience in spousal caregivers of patients with cancer: an integrative review. Nurs Open. 2021;8(5):2131–2141. doi: 10.1002/nop2.771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ke J., Lin J., Lin X., Chen W.T., Huang F. Dyadic effects of family resilience on quality of life in patients with lung cancer and spousal caregivers: the mediating role of dyadic coping. Eur J Oncol Nurs. 2023;66 doi: 10.1016/j.ejon.2023.102400. [DOI] [PubMed] [Google Scholar]
- 11.Chen J.J., Wang Q.L., Li H.P., Zhang T., Zhang S.S., Zhou M.K. Family resilience, perceived social support, and individual resilience in cancer couples: analysis using the actor-partner interdependence mediation model. Eur J Oncol Nurs. 2021;52 doi: 10.1016/j.ejon.2021.101932. [DOI] [PubMed] [Google Scholar]
- 12.Qin F., Wei T., Zhao X., et al. Relationship between family resilience and dyadic coping in colorectal cancer patients and their spouses, based on the actor-partner interdependence model. Eur J Oncol Nurs. 2024;70 doi: 10.1016/j.ejon.2024.102622. [DOI] [PubMed] [Google Scholar]
- 13.Deng X., Liu Q., Geng L., Li J., Wang M., Wan Y. Dyadic coping, resilience, and quality of life in young and middle-aged couples after gynecologic cancer: an actor-partner interdependence mediation model. Eur J Oncol Nurs. 2024;70 doi: 10.1016/j.ejon.2024.102601. [DOI] [PubMed] [Google Scholar]
- 14.Ştefǎnuţ A.M., Vintilǎ M., Tudorel O.I. The relationship of dyadic coping with emotional functioning and quality of the relationship in couples facing cancer-A meta-analysis. Front Psychol. 2020;11 doi: 10.3389/fpsyg.2020.594015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Festerling L., Buentzel J., Fischer von Weikersthal L., et al. Resilience in cancer patients and how it correlates with demographics, psychological factors, and lifestyle. J Cancer Res Clin Oncol. 2023;149(8):5279–5287. doi: 10.1007/s00432-022-04480-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gmelch S., Bodenmann G., Meuwly N., Ledermann T., Steffen-Sozinova O., Striegl K. Dyadisches Coping Inventar (DCI): Ein Fragebogen zur Erfassung des partnerschaftlichen Umgangs mit Stress. Journal of Family Research. 2008;20:185–202. doi: 10.20377/jfr-264. [DOI] [Google Scholar]
- 17.Krok D., Telka E., Moroń M. Marital satisfaction, partner communication, and illness acceptance among couples coping with breast cancer: a dyadic approach. Psycho Oncol. 2023;32(8):1240–1247. doi: 10.1002/pon.6174. [DOI] [PubMed] [Google Scholar]
- 18.Wendołowska A., Steć M., Czyżowska D. Supportive, delegated, and common dyadic coping mediates the association between adult attachment representation and relationship satisfaction: a dyadic approach. Int J Environ Res Publ Health. 2022;19(13) doi: 10.3390/ijerph19138026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zietlow A.L., Eckstein M., Hernández C., et al. Dyadic coping and its underlying neuroendocrine mechanisms - implications for stress regulation. Front Psychol. 2018;9:2600. doi: 10.3389/fpsyg.2018.02600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhi S., Gu W., Miao R., et al. Associations between dyadic communication and dyadic coping of patients with cervical cancer and their spouses: a study utilizing the actor-partner interdependence model. Support Care Cancer. 2024;32(2):90. doi: 10.1007/s00520-023-08304-2. [DOI] [PubMed] [Google Scholar]
- 21.Chen M., Gong J., Cao Q., Luo X., Li J., Li Q. A literature review of the relationship between dyadic coping and dyadic outcomes in cancer couples. Eur J Oncol Nurs. 2021;54 doi: 10.1016/j.ejon.2021.102035. [DOI] [PubMed] [Google Scholar]
- 22.Lai G.J., Tan K., Tan M., Cheong G., Cheng C., Mathew M. Dyadic positive and negative religious coping among older Singaporean couples and marital satisfaction. J Fam Psychol. 2023;37(2):268–274. doi: 10.1037/fam0001025. [DOI] [PubMed] [Google Scholar]
- 23.Badr H., Herbert K., Bonnen M.D., Asper J.A., Wagner T. Dyadic coping in patients undergoing radiotherapy for head and neck cancer and their spouses. Front Psychol. 2018;9:1780. doi: 10.3389/fpsyg.2018.01780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang H., Yue H., Ren M., Feng D. Dyadic effects of family-functioning and resilience on quality of life in advanced lung cancer patients and caregivers: an actor-partner interdependence mediation model. Eur J Oncol Nurs. 2021;52 doi: 10.1016/j.ejon.2021.101963. [DOI] [PubMed] [Google Scholar]
- 25.Kayser K., Cheung P.K., Rao N., Chan Y.C., Chan Y., Lo P.H. The influence of culture on couples coping with breast cancer: a comparative analysis of couples from China, India, and the United States. J Psychosoc Oncol. 2014;32(3):264–288. doi: 10.1080/07347332.2014.897292. [DOI] [PubMed] [Google Scholar]
- 26.Yang Z., Lai Y., Xiong C., et al. Illness perception and intimate relationships in patients with cervical cancer: the mediating role of dyadic coping. Support Care Cancer. 2024;32(8):557. doi: 10.1007/s00520-024-08762-2. [DOI] [PubMed] [Google Scholar]
- 27.Ma Y., Chen S., Dong H., et al. Relationship between resilience, social support, existential well-being and negative emotions in cervical cancer patients: a mediation analysis. J Cancer. 2024;15(11):3418–3426. doi: 10.7150/jca.91260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.SBoXUA Region. Main data of the seventh national population census of Xinjiang uygur autonomous region. 2024. https://tjj.xinjiang.gov.cn/tjj/tjgn/202106/4311411b68d343bbaa694e923c2c6be0.shtml
- 29.Wang Y., Cai Y.B., James W., Zhou J.L., Rezhake R., Zhang Q. Human papillomavirus distribution and cervical cancer epidemiological characteristics in rural population of Xinjiang, China. Chin Med J. 2021;134(15):1838–1844. doi: 10.1097/cm9.0000000000001441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kenny D.A., Ledermann T. Detecting, measuring, and testing dyadic patterns in the actor-partner interdependence model. J Fam Psychol. 2010;24(3):359–366. doi: 10.1037/a0019651. [DOI] [PubMed] [Google Scholar]
- 31.National Health Commission Of The People's Republic Of C National guidelines for diagnosis and treatment of cervical cancer 2022 in China (English version) Chin J Cancer Res. 2022;34(3):256–269. doi: 10.21147/j.issn.1000-9604.2022.03.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.The civil code of the people's Republic of China. 2024. http://www.npc.gov.cn/npc//c2/c30834/202006/t20200602_306457.html
- 33.Xu F., Hilpert P., Randall A.K., Li Q., Bodenmann G. Validation of the Dyadic Coping Inventory with Chinese couples: factorial structure, measurement invariance, and construct validity. Psychol Assess. 2016;28(8):e127–e140. doi: 10.1037/pas0000329. [DOI] [PubMed] [Google Scholar]
- 34.Qianyu N., Tian J. Evaluation on reliability and validity of 14-item resilience scale. Chin J Public Health. 2013;29(10):1524–1527. doi: 10.11847/zgggws2013-29-10-38. [DOI] [Google Scholar]
- 35.Chen W., Li H., Cai J.Z., Qin N. Association between dyadic coping and quality of life in breast cancer patients and their spouses: an actor-partner interdependence mediation model. Asian Nurs Res. 2024;18(1):44–50. doi: 10.1016/j.anr.2024.01.007. [DOI] [PubMed] [Google Scholar]
- 36.Wang C., Wacharasin C., Hengudomsub P. Self-efficacy as mediators of the association between dyadic coping and quality of life among spousal caregiver of patients with cervical cancer. Asia Pac J Oncol Nurs. 2024;11(3) doi: 10.1016/j.apjon.2023.100354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mijiti Y., Yusupu H., Liu H., et al. Survey on cervical cancer knowledge and its influencing factors among 2,578 women in Shache county, Kashi, China. BMC Wom Health. 2023;23(1):246. doi: 10.1186/s12905-023-02390-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li Y., Wang K., Yin Y., Li Y., Li S. Relationships between family resilience, breast cancer survivors' individual resilience, and caregiver burden: a cross-sectional study. Int J Nurs Stud. 2018;88:79–84. doi: 10.1016/j.ijnurstu.2018.08.011. [DOI] [PubMed] [Google Scholar]
- 39.Dsouza J.P., Van den Broucke S., Pattanshetty S., Dhoore W. Factors explaining men's intentions to support their partner's participation in cervical cancer screening. BMC Wom Health. 2022;22(1):443. doi: 10.1186/s12905-022-02019-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Suo R., Zhang L., Tao H., Ye F., Zhang Y., Yan J. The effects of dyadic coping and marital satisfaction on posttraumatic growth among breast cancer couples. Support Care Cancer. 2021;29(9):5425–5433. doi: 10.1007/s00520-021-06121-z. [DOI] [PubMed] [Google Scholar]
- 41.Lim J.W., Shon E.J., Paek M., Daly B. The dyadic effects of coping and resilience on psychological distress for cancer survivor couples. Support Care Cancer. 2014;22(12):3209–3217. doi: 10.1007/s00520-014-2334-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ji J., Zhu H., Zhao J.Z., Yang Y.Q., Xu X.T., Qian K.Y. Negative emotions and their management in Chinese convalescent cervical cancer patients: a qualitative study. J Int Med Res. 2020;48(9) doi: 10.1177/0300060520948758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ştefănuţ A.M., Vintilă M., Bădău L.M., et al. Perception of disease, dyadic coping, and the quality of life of oncology patients in the active treatment phase and their life partners: an approach based on the actor-partner interdependence model. Front Psychol. 2023;14 doi: 10.3389/fpsyg.2023.1069767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shang M., Cai T., Meng Y., Wang Q., Cui Y., Zhang F. Dyadic coping in young and middle-aged women with gynecological cancer: a latent class analysis. Support Care Cancer. 2022;31(1):47. doi: 10.1007/s00520-022-07515-3. [DOI] [PubMed] [Google Scholar]
- 45.Oh S., Ryu E. Does holding back cancer-related concern affect couples' marital relationship and quality of life of patients with lung Cancer?An actor-partner interdependence mediation modeling approach. Asian Nurs Res. 2019;13(4):277–285. doi: 10.1016/j.anr.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 46.Valente M., Chirico I., Ottoboni G., Chattat R. Relationship dynamics among couples dealing with breast cancer: a systematic review. Int J Environ Res Publ Health. 2021;18(14) doi: 10.3390/ijerph18147288. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data for the results of this study are available at the authors' request. The data are not publicly available due to privacy restrictions, as they contain sensitive information regarding both patients with cervical cancer and their spouses. Specifically, the data include personal health information, psychosocial coping strategies, and detailed questionnaire responses, which could lead to the identification of participants and reveal private aspects of their relationships and mental health.