Abstract
Introduction
Asymptomatic diaphragmatic hernia is generally rare among adults. Nonetheless, a subset of these patients can live a normal life and be exposed to many diseases, including obesity. When this rare event happens, surgical management can offer a solution to both problems simultaneously.
Presentation of the case
We present the rare case of an obese patient with an asymptomatic chronic traumatic diaphragmatic hernia who desired bariatric surgery. After an extensive preoperative workout, we were able to repair the 5 × 4,5 × 3 cm diaphragmatic defect and complete a gastric sleeve at the same operative time without complications.
Discussion
Simultaneous repair of diaphragmatic hernia and sleeve gastrectomy in obese patients has proven to be safe and effective. Although the literature is extremely scarce, with few case reports to our knowledge and after extensive literature research, this is the first case of a repair of traumatic diaphragmatic defect with concurrent sleeve gastrectomy.
Conclusion
Concurrent bariatric and thoracoscopic traumatic diaphragmatic hernia repair is a rare combination but is feasible and safe as long as it's done in fully equipped specialized centers with expert surgeons.
Keywords: Bariatric surgery, Diaphragmatic hernia, Laparoscopic, Obesity, Sleeve, Thoracoscopic surgery
Highlights
-
•
Combined use of thoracoscopy with laparoscopic bariatric surgery is a rare combination but is feasible
-
•
Simultaneous repair of diaphragmatic hernia and sleeve gastrectomy in obese patients has proven to be safe and effective.
-
•
Communication and proper surgical planning within the medical team will define a patient's outcome
1. Introduction
Acquired diaphragmatic hernia is an uncommon condition that frequently occurs following blunt (0.8–6 %) or penetrating (17 %) trauma; this can cause a rupture of the diaphragm, resulting in herniation of abdominal contents into the thoracic cavity [1,2]. In an acute setting diaphragmatic ruptures are usually larger and patients will suffer from respiratory symptoms, but when the lesion is small enough it may not be noticed or be obscured by other more life-threatening scenarios and may continue to grow until it causes complications [3].
Therefore, surgery is recommended to prevent severe complications which include respiratory failure, bowel incarceration and strangulation [3,4].
Although rare, it can be life-threatening. Therefore, surgery is recommended to prevent bowel incarceration and strangulation [1]. We present the case of an obese 34-year-old female with a past medical history of a gunshot wound to her left thorax. She sought bariatric surgery; nonetheless, a diaphragmatic hernia was discovered. After a joint effort of cardiothoracic and bariatric surgeons, the diaphragmatic hernia was repaired, and a simultaneous sleeve gastrectomy was performed.
This work has been reported in line with the SCARE criteria [5].
2. Case report
The patient is a 34-year-old female with a past medical history of a gunshot wound to her left thorax. She was assaulted when she was 16 years old in a remote location and was only managed with a chest tube. At that time, she recalled having no financial aid and that being in a remote place made healthcare practically unattainable. She remembered that after her chest tube was removed, she had no medical follow-up or controls, and she doesn't remember having a Computed Tomography (CT) scan or an x-ray.
Thankfully, after this incident, she lived a completely normal life. She never had any respiratory symptoms or weakness, and she made a full recovery from this unfortunate event but without any follow up.
Years passed, and she started to gain weight. Despite numerous attempts, which included exercise and a nutritional regime, her weight continued to increase. Due to this, she sought bariatric surgery, and presented to our hospital which is a high-volume bariatric and gastrointestinal surgical facility.
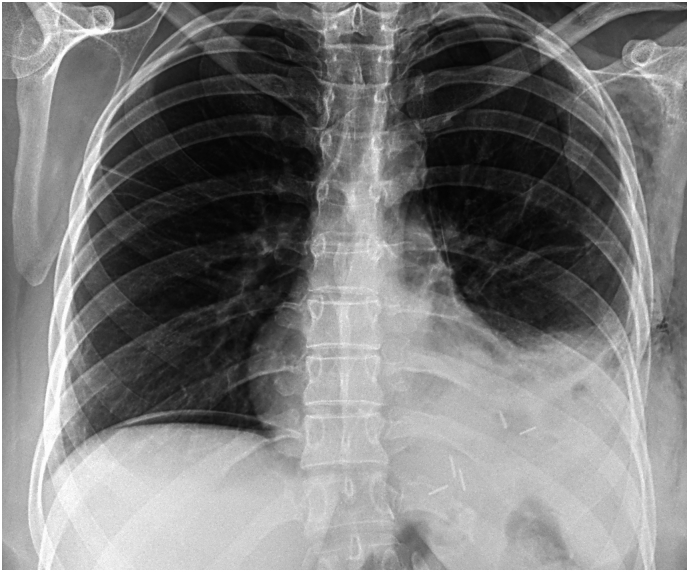
On evaluation, she had a weight of 87 kg and a height measuring 152 cm, her BMI was 37.7 kg/m2. Her physical examination revealed diminished breath sounds on auscultation of the left lower chest; therefore, a chest x-ray was requested. It showed multiple air-filled loops within the left hemithorax, with an indistinct ipsilateral hemidiaphragm. There was a slight mediastinal shift to the right, and the right lung was clear (Fig. 1A). Due to this, a contrast-enhanced CT showed what was suspected: a 5 × 4,5 × 3 cm central diaphragmatic defect with intrathoracic herniation of the stomach, colonic splenic flexure, small bowel, and extensive amounts of the mesentery (Fig. 1B, Fig. 1C). With these findings, a cardiothoracic assessment was needed, and surgery was required.
Fig. 1A.

X-ray, multiple air-filled loops within the left hemithorax are seen.
Fig. 1B.
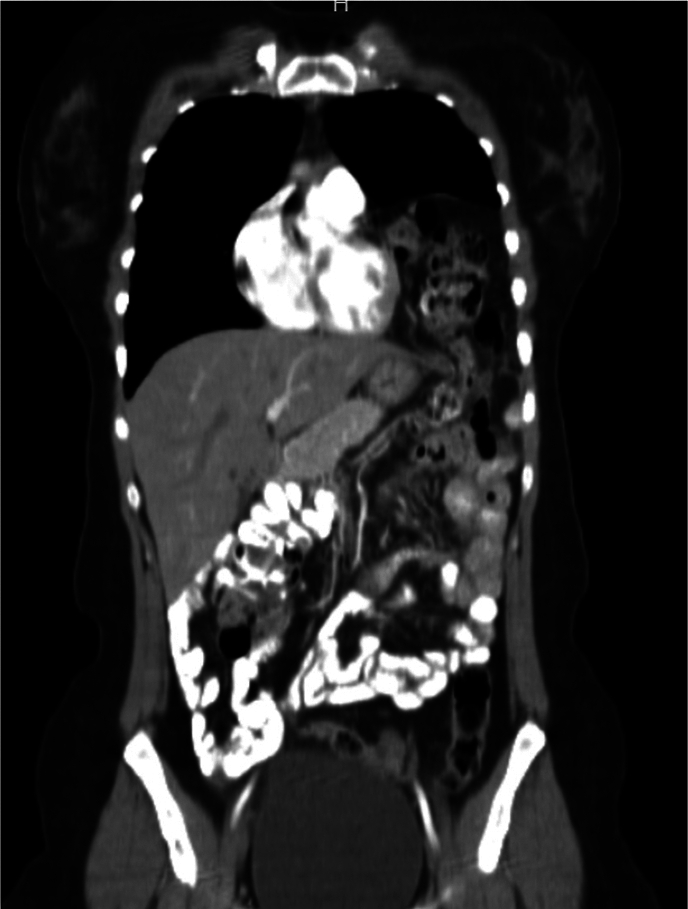
CT shows the diaphragmatic hernia with the bowel within.
Fig. 1C.
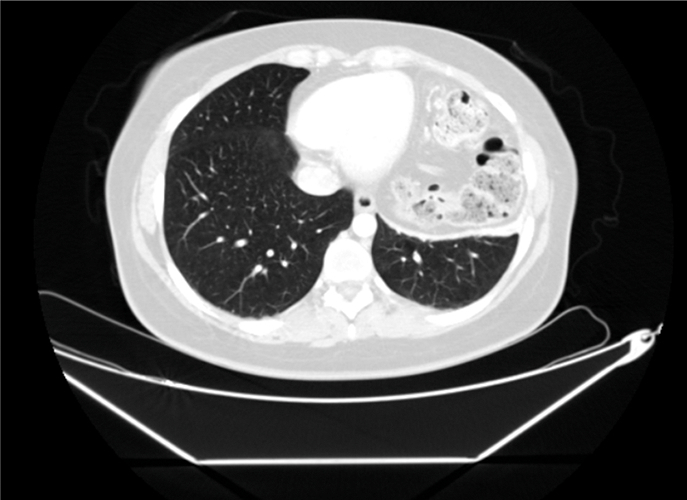
CT shows the size of the diaphragmatic.
Due to this, and since the patient sought bariatric surgery and was asymptomatic from her diaphragmatic hernia, she underwent a comprehensive preoperative workout and medical weight loss. (She lost 5 kg in 2 months, changed her eating and exercise routines with the help of a psychologist and nutritionist.)
She had no history of reflux, her barium swallow showed no signs of a hiatal hernia, and the upper endoscopy showed no anomalies; therefore, a conjoined effort of cardiothoracic and bariatric surgeons was needed, and a diaphragmatic hernia repair via VATS (Video Assisted Thoracoscopic Surgery) with a sleeve gastrectomy was planned. After prophylactic antibiotic was administered (Cefazolin 2 g), VATS was performed using double lumen intubation, the patient was placed in a right lateral decubitus position, and a 4–5 cm long incision was placed in the 5th intercostal space anterior axillary line. A wound retractor was used to set both the instruments and the thoracoscope. Another trocar was placed in the 3rd intercostal space anterior axillary line so the surgeon could mobilize the hernia sac. The lung was retracted, and after removing adhesions using a bipolar electrosurgical instrument (Covidien LigaSure), the hernia sac was released entirely revealing the 5 × 4,5 × 3 cm defect. The diaphragmatic defect was sutured using interrupted nonabsorbable 2–0 polyester sutures and reinforced with an oxidized regenerated cellulose fabric and nonabsorbable polypropylene mesh (Proceed, J&J). A 26 Fr chest tube was placed, and the lung was re-inflated without complications (Fig. 2A). Afterward, we positioned the patient in a supine position. We placed a 12 mm supraumbilical port for the staples and two 5 mm ports, one on the midclavicular line on the left side of the abdomen and the other in the midclavicular line on the right side. As per routine, a 36-French Bougie was used. The incisura was identified, and we proceeded to enter the lesser sac; the omentum was detached from the greater curvature and the dissection continued upward, ligating the short vessels and mobilizing the fundus. At this point, the hernia sac was seen in the abdomen (Fig. 2B). The bougie was advanced up to the first part of the duodenum, and using six 60 mm purples staplers (EndoGIA Ultra XL, Medtronic) the sleeve was completed. The staple line was then reinforced using a nonabsorbable monofilament suture. A methylene blue test was performed, and no leaks were identified. A Penrose drain was placed, and the surgery was completed (187 min) without complications (Fig. 2C).
Fig. 2A.
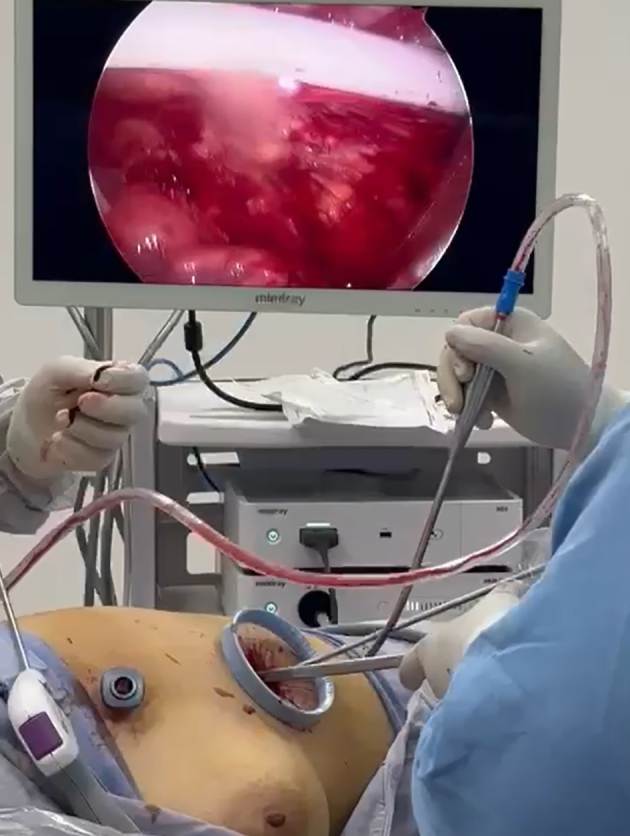
Thoracoscopy, the wound retractor is seen.
Fig. 2B.
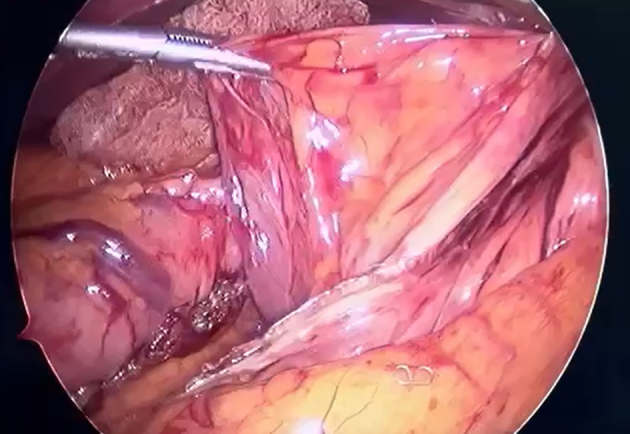
Laparoscopy, the hernia sac is visible beside the sleeve.
Fig. 2C.

Surgical Wounds are seen with the drain and chest tube.
Her postoperative course was uneventful. She started drinking liquids 6 h after surgery and had no complications. The chest tube and Penrose drain were removed due to low and serous production on postoperative day 3, and she was discharged after the liquid diet was tolerated and pain was controlled on postoperative day 4 (Fig. 3). A 10-day course of low-weight heparin was also administered to prevent thrombosis as per routine.
Fig. 3.
Postoperative X-ray without pneumothorax.
The patient is under regular follow ups with the nutritionist and psychologist and 4 months after surgery, the patient is doing well without complications.
3. Discussion
Asymptomatic diaphragmatic hernia is usually rare to be discovered among adults; there are usually two main types of diaphragmatic hernias: congenital, which is generally life-threatening after birth and requires emergency surgery, and acquired, which, in most cases due to trauma, or iatrogenic after laparoscopic or thoracoscopic surgeries [1,2]. The presentation of these hernias is varied; many will present immediately after trauma or in some days or sometimes many years after trauma [1,3]. Penetrating trauma is the most common cause of these injuries; however, blunt trauma can cause diaphragmatic rupture in up to 5 % of the cases [1,3,4]. In most patients, diaphragmatic trauma is associated with other injuries, including damage to other organs, rib fractures, and great vessels [2,3]. In our case, 18 years had passed since the trauma before the patient came to us. Due to the size and location of the hernia, it was decided to perform surgery.
The liver's anatomic location minimizes the possibility of right-sided incarceration; therefore, most hernias appear on the left side [1,6], as our patient experienced.
Most authors agree that all symptomatic patients, and even those who are asymptomatic and detected incidentally, should undergo surgical repair due to the serious risk of strangulation, leading to severe morbidity and mortality [2,7]. As it was done in our case.
A wait-and-see approach can be considered in a select group of patients when the risk of surgery outweighs its benefits, especially in the elderly when there are no symptoms of incarceration, and there is no digestive tract herniation [2,8].
Simultaneous repair of diaphragmatic hernia and sleeve gastrectomy in our patient proved to be safe and effective. Although the literature is extremely scarce, in one case report by Alqahtani et al., they performed a sleeve on a patient with Morgani Hernia [4]. Nonetheless, to our knowledge and after extensive literature research, this is the first case of a repair of traumatic diaphragmatic defect with concurrent sleeve gastrectomy.
The case highlights the safety of concurrent diaphragmatic hernia repair and bariatric surgery performed by experienced surgeons in tertiary centers.
4. Conclusions
Bariatric surgery has emerged as one of the main tools to control and treat obesity; as the obesity epidemic advances, many people will need this treatment, including patients who already have comorbidities, pathologies, and previous trauma.
Our physician's duty is to provide patients with the best treatments and professionals in the best places. This case shows us that this type of concurrent surgery is possible with good communication within the medical team and proper surgical planning.
CRediT authorship contribution statement
FL is the main author and wrote the manuscript, RM and JZ gathered the data and analysed it. GM was in charge of completing the first draft and gathered the images.
Consent
Written informed consent was obtained from the patient and our hospital for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
Approval was obtained from the ethics committee of our hospital and is available for review by the Editor-in-Chief of this journal on request.
Guarantor
Gabriel A. Molina, MD, MD, Department of General Surgery, Division of Bariatric, CIBA Hospital, Tijuana-Mexico & Universidad San Francisco (USFQ) Quito-Ecuador, gabomolina32@gmail.com, + 593 998352532
Patient perspective
The patient was surprised to know that she had carried the diaphragmatic hernia for most of her life, as she didn't have any symptoms; nonetheless, she understood how serious that could be. After her initial assessment, she was relieved that she could have both surgeries at the same time and was thrilled to know that everything went as planned. She became highly thankful to the medical team after a successful surgery.
Sources of funding
None.
Declaration of competing interest
The authors declare no conflicts of interest to disclose.
References
- 1.Gu P., Lu Y., Li X., Lin X. Acute and chronic traumatic diaphragmatic hernia: 10 years’ experience. PloS One. 2019;14(12) doi: 10.1371/journal.pone.0226364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adereti C., Zahir J., Robinson E., Pursel J., Hamdallah Isam. A case report and literature review on incidental Morgagni hernia in bariatric patients: to repair or not to repair? Cureus. 2023 doi: 10.7759/cureus.39950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katwal S., Ghimire A., Shrestha K. Traumatic diaphragmatic hernia in rural Nepal: a rare case report illuminating diagnostic challenges and healthcare discrepancies. Radiology case reports. 2023;18(12):4268–4271. doi: 10.1016/j.radcr.2023.08.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alqahtani A., Aljohani Emad, Almadi Fahad, Billa S. Laparoscopic sleeve gastrectomy with concomitant Morgagni hernia repair. Journal of Surgical Case Reports. 2019;2019(7) doi: 10.1093/jscr/rjz204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sohrabi C., Mathew G., Maria N., Kerwan A., Franchi T., Agha R.A. The SCARE 2023 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int J Surg Lond Engl. 2023;109(5):1136. doi: 10.1097/JS9.0000000000000373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palma R., Angrisani F., Santonicola Antonella, Iovino P., Ormando Vittorio Maria, Maselli R., Angrisani L. Case report: laparoscopic nissen-sleeve gastrectomy in a young adult with incidental finding of Morgagni-Larrey hernia. Front. Surg. 2023;10 doi: 10.3389/fsurg.2023.1227567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goudarzi H., Hemmatizadeh Mahsa, Anbara Taha. Surgical technique of congenital diaphragmatic hernia following sleeve gastrectomy; a case report study. Int. J. Surg. Case Rep. 2022;99:107671. doi: 10.1016/j.ijscr.2022.107671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhasin D.K., Nagi B., Gupta N.M., Singh K. Chronic intermittent gastric volvulus within the foramen of Morgagni. Am. J. Gastroenterol. 1989;84(9):1106–1108. [PubMed] [Google Scholar]