Abstract
Abstract
Objective
To examine existing literature regarding health literacy levels and their association with multimorbidity and the potential underlying mechanisms behind the said association.
Design
Systematic review and meta-analysis.
Data sources
The databases MEDLINE, EMBASE, CINAHL and Science Direct were searched for articles published between 1 January 2000 and 31 October 2023 using a systematic search strategy.
Eligibility criteria
Included were all primary studies conducted in people over 18 years old with data on health literacy levels and the presence of multimorbidity. No language restrictions were used.
Data extraction and synthesis
Two authors independently extracted data and assessed the bias using the Joanna Briggs Institute critical appraisal tools.
Results
We included a total of 39 studies (36 quantitative, two qualitative and one mixed-method), representing 154 337 participants. We found a 32% proportion of limited health literacy among individuals with multimorbidity. Analysis of three articles using the Health Literacy Questionnaire tool (n=31 228) (Pooled OR 2.88 (95% CI 1.92 to 4.31)) and three articles using the Health Literacy Survey Questionnaire–European Union tool (n=35 358) (OR 1.16 (95% CI 1.07 to 1.25)) indicated that people with limited health literacy were likely to have multiple conditions. One of three articles studying underlying mechanisms reported that self-efficacy mediates the association between health literacy and multimorbidity. Additionally, substantial literature identified education and income as the most consistent determinants of health literacy among individuals with multimorbidity. Of the only two articles studying the effectiveness of health literacy-related interventions, both reported an improvement in clinical outcomes after the intervention.
Conclusions
Our review demonstrated a consistent association between health literacy and multimorbidity, indicating that people with lower health literacy levels are more likely to have multimorbidity. More evidence is needed regarding the effect of health literacy interventions on multimorbidity.
PROSPERO registration number
CRD42022301369.
Keywords: Systematic Review, EPIDEMIOLOGY, PUBLIC HEALTH, Health Education, Chronic Disease
STRENGTHS AND LIMITATIONS OF THIS STUDY
The inclusive nature of the data synthesis provided a better understanding of the association under review.
We performed a thorough literature search, using cross-reference and hand-searching techniques to ensure the inclusion of all relevant articles in the review.
The limited number of intervention studies hampered the ability to define targets for interventions.
The scarcity of studies assessing outcomes in multimorbidity hindered the assessment of the impact of health literacy on multimorbidity outcomes.
Introduction
Multimorbidity, the concurrent presence of two or more chronic conditions in an individual, is emerging globally as a significant public health challenge.1 A systematic review in 2019, which included 70 studies across 49 different countries, reported a pooled prevalence of multimorbidity as 33.1% (95% CI 30.0% to 36.3%).2 The same study reported this estimate to be 37.9% (32.5%–43.4%) among high-income countries (HICs), and 29.7% (26.4–33.0%) in low- and middle-income countries (LMICs).2 People with multimorbidity often face poor physical and mental health, longer hospital stays, lower quality of life and higher healthcare costs.3 Multimorbidity creates a complex long-term challenge for patients, their family, caregivers, healthcare providers and systems as it presents the patients and the people around them with a steep learning curve about risk, treatment and self-care.4 Contextual differences, particularly for marginalised and indigenous populations, contribute to disparities in health literacy and access to resources crucial for effective disease management.5 Addressing these disparities is essential for improving multimorbidity prevention and management strategies globally.
Health literacy, defined as the ability to access, understand, evaluate and use health information to make informed decisions in order to keep or recover one’s health, might play a crucial role in the management of multimorbidity.6 Health literacy is an important determinant of a patient’s active participation in self-management as well as patient outcomes.7 Current health literacy research, focused mainly on patients with specific chronic conditions, shows that limited health literacy is associated with poorer health behaviours and health outcomes, such as the earlier onset of disease, faster progression of disease, increased hospitalisation rates and higher health-related costs for both individuals and healthcare systems.5 8 However, although these similarities suggest the existence of a relationship between health literacy and multimorbidity, research conducted on this potential relationship seems to be limited and has shown mixed results.9 10
Insight into the relationship between health literacy and multimorbidity and its underlying mechanisms is important for the development and improvement of interventions to target health literacy.5 8 Research underlines the role of health literacy as a mediator in the association between socioeconomic status and health outcomes.10 Thus, if addressed, removing health literacy barriers could potentially compensate for the negative effect of other socioeconomic determinants of health that are related to health inequalities.11 In its mediating role, for people living with multimorbidity, it could enhance the prevention of worse health outcomes or even prevent multimorbidity altogether. Both, the Institute of Medicine in the USA and various researchers have highlighted persistent gaps in our understanding of health literacy and its relationship with chronic disease.12,18 Thereby, this comprehensive systematic review aims to analyse the existing literature on health literacy levels and their association with multimorbidity, explore the potential mechanisms behind this association and evaluate the effectiveness of health literacy interventions for individuals with multimorbidity.
Methods
Protocol and registration
We conducted a systematic review of various studies examining health literacy among multimorbid individuals, following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines,19 involving: (i) identifying the research question, (ii) identifying the relevant studies, (iii) study selection, (iv) data extraction and (v) data analysis. This review has been registered on the PROSPERO database (registration ID number: CRD42022301369); available at: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022301369..
Eligibility criteria
Studies were eligible for inclusion if they: (1) were a primary study, (2) were conducted among people aged ≥18 years, (3) reported health literacy levels of participants irrespective of the tool used to measure them and (4) reported the presence/absence of multimorbidity (presence of two or more chronic conditions) among the participants. There were no restrictions on language or study location. We excluded reviews, case reports, editorials, opinion pieces, study protocols, conference abstracts, posters, theses, book chapters, textbooks and any unpublished material. We defined health literacy as the ability of an individual to access, understand, evaluate and use health information to make informed decisions to maintain or recover one’s health.8 We defined multimorbidity as the concurrent presence of two or more chronic conditions in an individual.11
Information sources and search strategy
We conducted electronic searches of four databases that index peer-reviewed journals: MEDLINE, EMBASE, CINAHL and ScienceDirect. We limited the search to the period from 1 January 2000 to 31 October 2023. We chose this period because health literacy research has mainly accumulated since 1999. To identify the relevant studies, a comprehensive search was conducted using Keywords and Medical Subject Headings terminology for multimorbidity, polymorbidity, polypathology, pluripathology, multipathology, multicondition, multiple chronic conditions, health literacy, health knowledge and health behaviour. The complete search strategy is presented in the online supplemental table S1. Author GCD received formal training in the development of search strategies as part of his graduate studies, and the search strategy used for this review was also reviewed by a senior librarian at the Indian Council of Medical Research-Regional Medical Research Centre, Bhubaneswar. Two authors (AK and FGL-J) independently searched all four databases mentioned. Handsearching and reference checking of citations and reference lists were performed to identify potentially missing literature.
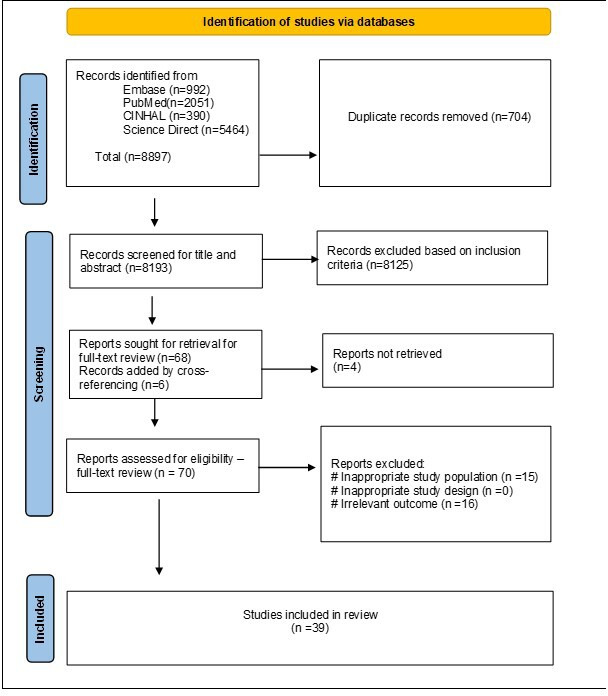
Study selection
All the retrieved citations were first imported from the electronic searches to EndNote, where duplicate entries were removed; the resulting entries were then uploaded to Rayyan software. Two independent researchers (AK and FGL-J) screened the titles and abstracts of the retrieved studies to identify all articles potentially eligible for inclusion. Uncertainty or disagreement was settled by consensus with a third reviewer (AC). Next, two researchers (AK and FGL-J) conducted full-text screening of the previously identified articles. Again, any uncertainty or disagreement was settled by consensus with a third reviewer (AC). The articles that were excluded, as well as the grounds for their exclusion, are detailed according to the PRISMA 2020 statement; this is presented in a PRISMA flow diagram (figure 1).
Figure 1. Prisma flow diagram.
Data collection
We extracted the necessary information about the study characteristics and the results of the included studies using a predetermined and standardised data extraction form. We extracted information regarding authors, publication, country, study design, study area, sample size, publication year, sociodemographic factors, level of health literacy, etc. Two independent reviewers (AK and FGL-J) conducted the data extraction blindly after the study selection had been completed. They also extracted information for assessing the risk of bias. We identified and resolved discrepancies by discussion. When data was insufficient or missing, or full text was not available, we used email to ask the corresponding authors of the original articles to provide the relevant information.
Methodological quality and risk of bias assessment
Two independent researchers (AK and FGL-J) assessed the methodological quality and the risk of bias among the included studies using the Joanna Briggs Institute (JBI) Critical Appraisal tools, a set of questionnaires used to assess the risk of bias in studies such as cross-sectional, cohort, randomised controlled trials, quasi-experimental, qualitative and mixed-method studies.12 Studies were then graded and classified as having ‘low’, ‘moderate’ or ‘high’ risk of bias. According to the JBI critical assessment score, the majority of our studies (score >70%) were considered to have a low risk of bias, and one study was considered to have a moderate risk of bias (score 50%–69%).12 Details can be found in the online supplemental table S2-6. No articles were excluded by reason of the quality assessment.
Data analysis
Because of the heterogeneity between the tools used to measure health literacy levels, performing a quantitative synthesis incorporating all the studies was considered unsuitable. To assess the levels of health literacy among people with multimorbidity, we calculated pooled mean health literacy scores with 95% CIs per domain from the studies that had used the Health Literacy Questionnaire (HLQ) tool (n=12). To assess the association between health literacy levels and multimorbidity, we performed random effects meta-analyses with MetaXL V.5.3 (EpiGear) software in MS Excel 2016 and IBM SPSS V.27. For dichotomous data, the effect sizes were expressed as ORs, and for continuous data as weighted mean differences. We reported all effect estimates with their 95% CI. We assessed heterogeneity using Cochrane’s Q and I2 statistics.
Quantitative synthesis was not possible for the remaining articles. Instead, we narratively synthesised these using ‘The Causal Pathways Linking Health Literacy to Health Outcomes’ model by Paasche-Orlow.13 We searched for and extracted information dealing with the three main groups of mediators proposed by the model: ‘Access and Utilisation of Healthcare’, ‘Provider-Patient Interaction’ and ‘Self-care’ and their reported role in the outcome groups: clinical, behavioural and patient-provider interaction.
Patient and public involvement
None.
Results
Literature search
Across all databases, our search yielded 8897 studies (figure 1). After removing 704 duplicates, 8193 articles remained. Following the screening of titles and abstracts, we identified 68 studies. An additional search of reference lists led to the inclusion of six additional publications, resulting in a total of 74 articles for full-text review. Of these, four articles could not be retrieved, and 31 were excluded for having either an irrelevant population or irrelevant outcomes (figure 1). Consequently, 39 studies met the inclusion criteria and were included in the review: 36 quantitative studies,1014,48 two qualitative studies49 50 and one mixed-methods study.51
Study characteristics
The majority of the research was conducted in HICs (22 studies), followed by middle-income countries (17 studies: 10 from upper-middle-income countries and 7 from LMIC (table 1)). When classifying the studies by WHO regions, it was observed that 14 studies were conducted in the European region (142 982 patients, representing 92.64% of the total patient population), 12 in the Western Pacific region (7750 patients, 5.02%), seven in the American region (952 patients, 0.62%), four in the South-East Asian region (890 patients, 0.58%), one in the African region (10 patients, 0.01%) and one in Kosovo (1753 patients, 1.14%). This accounts for a total of 154 337 individuals across the included studies, with individual study populations ranging from 10 to 102 006 participants. All included studies defined multimorbidity as individuals living with two or more chronic diseases. Table 1 provides an overview of the main characteristics of the included studies.
Table 1. Key characteristics of studies included in the review.
| Author/year | Country | Region | Study design | Health literacy assessment tool | Sample size | Mean age (±SD)/ median |
| Abd-Rahim et al, 202114 | Malaysia | UMIC | Cross-sectional | HLS-SF12 | 413 | 67 (NA) |
| Demir et al, 202215 | Turkey | UMIC | Cross-sectional | HLS-EU-Q47 | 208 | 65 median |
| Dinh et al, 202016 | Vietnam | LMIC | Cross-sectional | HLQ | 600* | 61.54 (15.3) |
| Dinh et al, 202217 | Vietnam | LMIC | Cross-sectional | HLQ | 367 | 58.8 (16.9) |
| Dinh et al, 202318 | Vietnam | LMIC | Cross-sectional | HLQ | 600* | 61.54 (15.3) |
| Eckman et al, 201219 | USA | HIC | Randomised trial | REALM | 170 | 59.97 (10.46) |
| Eton et al, 201920 | USA | HIC | Cross-sectional | HRQL | 91 | 65 median |
| Friss et al, 201921 | Denmark | HIC | Cross-sectional | HLQ | 2111 | 67.2 (13.3) |
| Griese et al, 202222 | Germany | HIC | Cross-sectional | HLS19-NAV | 1105 | 60.26 (NA) |
| Griva et al, 202023 | Singapore | HIC | Cohort | HLQ | 221 | 59 (9.81) |
| Gurgel do Amaral et al, 202224 | Netherlands | HIC | Cross-sectional | Interview | 2742 | 52.7 (15.7) |
| Hajek et al, 202325 | Germany | HIC | Cross-sectional | NRW80+ | 1484 | 86.3 (4.5) |
| Hermans et al, 202126 | Belgium | HIC | Cross-sectional | HLS19-Q12 | 102 006 | (NA) |
| Hopman et al, 201663 | Netherlands | HIC | Cross-sectional | HLQ | 1092 | 65.58 (13.33) |
| Hudon et al, 201228 | Canada | HIC | Cross-sectional | NVS/DBMA | 103 | 49.9 (7.1) |
| Liu et al, 202029 | China | UMIC | Cross-sectional | CCHL | 637 | 72.21 (5.76) |
| Maduka et al, 202030 | USA | HIC | Cross-sectional | BHLS | 271 | 57 median |
| Matima et al, 201849 | South Africa | UMIC | Qualitative study | Interview | 10 | 46.9 (8.8) |
| Naik et al, 201131 | USA | HIC | Cross-sectional | S-TOFLA | 100 | 72.74 (NA) |
| Pedersen et al, 202132 | Denmark | HIC | Cross-sectional | HLQ | 28 627 | 55 (15.7) |
| Rheault et al, 202151 | Australia | HIC | Mixed-method study | HLQ+interview | 200* | 55 (15.7) |
| Rheault et al, 201933 | Australia | HIC | Cross-sectional | HLQ | 200* | 55 (15.7) |
| Schaeffer et al, 202134 | Germany | HIC | Cross-sectional | HLS-GER 2 | 2151 | 50.82 (18.47) |
| Selvakumar et al, 202335 | Malaysia | UMIC | Cross-sectional | HLS-SF12 | 346 | 67.1 (NA) |
| Shreshta et al, 201836 | Nepal | LMIC | Cross-sectional | HLS-EU-ASIA-Q | 426 | 56.6 (11.58) |
| Stomer et al, 202050 | Norway | HIC | Qualitative study | HLQ | 12 | 66 median |
| Stomer et al, 202037 | Norway | HIC | Cross-sectional | HLQ | 187 | 67 (13.0) |
| Suarilah et al, 202238 | Indonesia | LMIC | Cross-sectional | MMHLQ | 226 | 56.61 (7.48) |
| Sun et al, 202239 | China | UMIC | Cross-sectional | HLS-PCD | 471 | 73.22 (8.53) |
| Teles et al, 202140 | Turkey | UMIC | Cross-sectional | HLS-EU-Q47 | 530 | (NA) |
| Toci et al, 201541 | Kosovo | UMIC | Cross-sectional | Interview | 1753 | 73.4 (6.3) |
| Tomita et al, 202210 | Japan | HIC | Cross-sectional | CCHL | 3678 | 52.3 (18.2) |
| Wang et al, 202342 | China | UMIC | Cross-sectional | C-MLS | 328 | 74.9 (7.37) |
| Wieczorek et al, 202343 | Switzerland | HIC | Cross-sectional | HLS-EU-Q16 | 1615 | 67.5 (0.44) |
| Woodard et al, 201444 | USA | HIC | Cross-sectional | FHL | 183 | 67.9 (7.89) |
| Wu et al, 202345 | China | UMIC | Cross-sectional | eHEALS | 289 | 68.61 (5.36) |
| Yadav et al, 2020a46 | Nepal | LMIC | Cross-sectional | HLQ | 238* | 59.18 (12.19) |
| Yadav et al, 2020b47 | Nepal | LMIC | Cross-sectional | HLQ | 238* | 59.18 (12.19) |
| Yeung et al, 201748 | USA | HIC | Quasi-experimental design | REALM-SF/SAHLSA-50 | 34 | 51.8 (8.4) |
These articles made use of the same populations for their studies and were considered only once for our analysis.
BHLSBrief Health Literacy ScreenCCHLChinese Citizen Health Literacy QuestionnaireC-MLSChinese Version of the Medication Literacy ScaleeHEALSe-health literacy scaleFHLfunctional health literacyHICshigh-income countriesHLQHealth Literacy QuestionnaireHLSHealth Literacy SurveyHLS–EUHealth Literacy Survey Questionnaire–European UnionHLS-GER 2Health Literacy Survey Germany 2HLS-PCDHealth Literacy Scale for Patients with Chronic DiseasesHLS-SFHealth Literacy Survey Questionnaire Short FormHRQLhealth related quality of lifeLMICslow-middle-income countriesMMHLQMandarin Multidimensional Health Literacy QuestionnaireNAVnavigational health literacyNRWsurvey on quality of life and subjective well-being of the very old in North Rhine-WestphaliaNVSnewest vital signREALMRapid Estimate of Adult Literacy in MedicineREALM-SFRapid Estimate of Adult Literacy in Medicine-Short FormSAHLSAShort Assessment of Health Literacy- 50S-TOFLAshort test of functional health literacy in adultsUMICsupper-middle-income countries
Health literacy levels among individuals with multimorbidity
Assessment tools
The included studies employed various methods and tools to assess health literacy. The most frequently used tool was the HLQ, reported in 12 studies, out of which two studies used HLQ in LMICs, contextualised the tool based on the settings. Following that were the European Health Literacy Questionnaire (HLS-EU) and its variants, used in 10 studies (table 1). Four studies used in-depth interviews. While two studies assessed health literacy using the Rapid Estimate of Adult Literacy in Medicine-Short Form (REALM-SF) and one study used the abbreviated version of the Test of Functional Health Literacy in Adults (S-TOFHLA) (table 1). Additionally, 10 studies employed unique health literacy measurement tools (table 1).
Pooled proportion and mean health literacy scores among individuals with multimorbidity
Due to the lack of a uniform tool to assess health literacy levels across all study types, pooled mean scores were not calculated as the scoring patterns were irregular. We calculated pooled mean scores exclusively for studies using the HLQ tool (n=12). Since no more than two studies used a similar variant of the HLS-EU questionnaire or its variants, pooled scores were not computed for them.
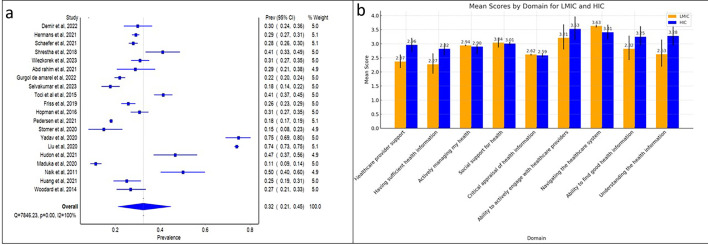
Pooled proportion of individuals with multimorbidity with limited health literacy
Based on the proportion of multimorbid individuals with limited health literacy, we calculated pooled proportion of limited health literacy from 20 cross-sectional studies providing data on limited health literacy as 32% (95% CI 21% to 45%) (figure 2a).
Figure 2. Pooled proportion and mean health literacy scores among individuals with multimorbidity. (a) Proportion of limited health literacy among individuals with multimorbidity. (b) Pooled mean health literacy scores based on HLQ in LMIC and HIC. HIC, high-income country; HLQ, Health Literacy Questionnaire; LMIC, low-middle-income country.
Sensitivity analysis
A sensitivity analysis was carried out because of the notable heterogeneity (p=0.000, I2=100%). The pooled proportion of limited health literacy was found to be 29% (95% CI 28% to 30%, Q=4.91, p=0.97, I2=0%) after ruling out the studies which were causing the heterogeneity.
Pooled mean health literacy scores based on HLQ-9
The HLQ measures health literacy across nine domains by averaging likert-type responses to a set of questions per domain. Domains 1 to 5 use 5-point scales, resulting in scores ranging from 1 to 5 on a continuous scale. Domains 6 to 9 use 4-point scales. Despite this difference, higher domain scores indicate stronger health literacy.
A total of eight studies provided information related to the mean health literacy scores. Accordingly, a subgroup analysis was performed based on HICs and LMICs. In comparison to HIC, all the HLQ domains had lower pooled mean health literacy scores for LMIC except social support for health and navigating the healthcare system (figure 2b). As for the combined health literacy scores, highest pooled mean health literacy scores were observed for the ability to actively engage with healthcare providers and navigate the healthcare system domains whereas the lowest health literacy scores were observed for having sufficient health information (figure 2b).
For studies using HLS-EU variants, proportions of patients with multimorbidity having limited health literacy ranged from 19.0% to 58.8%.1015,17 40 42
Association between health literacy and multimorbidity
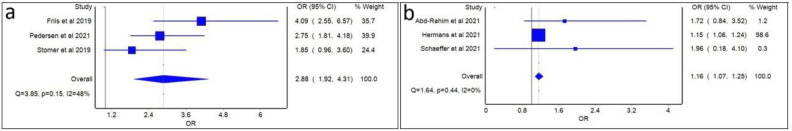
Six studies provided data on the relationship between health literacy and multimorbidity. A random-effects meta-analysis of the studies using the HLQ tool (n=3) revealed a significant association between low health literacy and multimorbidity (pooled OR 2.88 (95% CI 1.92 to 4.31)) (figure 3a).21 32 37 Similarly, a meta-analysis of studies using the HLS-EU tool (n=3) showed a significant association between low health literacy and multimorbidity (OR 1.16 (95% CI 1.07 to 1.25)) (figure 3b).14 26 34
Figure 3. Forest plots for random effect meta-analysis of the associations of limited health literacy and multimorbidity assessed with HLQ and HLS. (a) Forest plots for random effect meta-analysis of the associations of limited health literacy and multimorbidity assessed with HLQ. (b) Forest plots for random effect meta-analysis of the associations of limited health literacy and multimorbidity assessed with HLS. HLQ, Health Literacy Questionnaire; HLS, Health Literacy Survey.
Underlying mechanism of association between health literacy and multimorbidity
Among individuals with multimorbidity, health literacy was observed to mediate the relationship between social support and self-management, as well as between social support and self-efficacy, while self-efficacy further mediated the connection between health literacy and treatment outcomes.20 35
Determinants of health literacy
12 studies reported on the determinants of health literacy among individuals with multimorbidity.14,1822 29 34 39 40 47 51 Higher education and income emerged as the strongest factors of higher levels of health literacy across various settings, whether in high-income or middle-income countries. Other determinants included age (specifically, being under 65 years), residence (living in rural areas), gender, social support and ethnicity (particularly for indigenous populations) determining higher levels of health literacy. Marital status did not appear to impact health literacy levels among these individuals.
Education
In studies using the HLQ-9 tool to assess health literacy, higher education status influenced all domains except for social support for health. These domains included: support from healthcare providers,18 21 41 51 having sufficient health information,18 21 41 51 actively managing one’s health,18 41 51 critical appraisal of health information,17 18 41 51 engaging with healthcare providers, navigating the healthcare system,18 41 51 ability to find good health information18 21 41 51 and understanding health information.18 21 41 51
Similar observations were reported in studies employing the HLS-EU and its variants, as well as those using unique health literacy assessment tools.14 15 22 34 39 40
Income
Income was the second most consistent determinant of health literacy. Lower health literacy was observed in groups with an income of <US$240 in LMICs. For studies using the HLQ-9, income influenced all domains except for support from healthcare providers and actively managing one’s health.16 17 47 Similar findings were reported in studies using unique health literacy tools.34 39
Age
A study from an LMIC using the HLQ-9 suggested that being under 65 years positively influenced domains such as support from healthcare providers,17 social support for health,17 engaging with healthcare providers,16 navigating the healthcare system,16 the ability to find good health information16 and understanding health information.16 Conversely, a study from an HIC revealed that health literacy was influenced by being over 65 years.22
Residence
Living in rural areas influenced HLQ-9 domains such as support from healthcare providers,17 51 having sufficient health information,17 51 social support for health17 51 and critical appraisal of health information.51 Studies using the HLS-EU and its variants also found similar results.15 40
Ethnicity and social support
Ethnicity was not a major determinant for most HLQ-9 domains, except for social support for health, which was influenced by being part of an indigenous or Dalit population.21 41 Additionally, three studies reported social support as a positive determinant of health literacy.18 22 29
Gender and marital status
Two studies conducted in HICs suggested that gender had no influence on health literacy.17 51 Contrastingly, a study from a UMIC using the HLS-EU tool found that male gender was a determinant of health literacy.40 However, another study from an LMIC reported that the HLQ-9 domains of having sufficient health information, the ability to find good health information21 and understanding health information17 21 51 were influenced by female gender, suggesting cultural factors impact health literacy levels. Regardless of the settings, marital status had no influence on health literacy.17 21 51
Health literacy and outcomes
Table 2 presents a narrative synthesis of information dealing with the three main groups of mediators proposed by a model in Paasche-Orlow’s ‘Causal Pathways Linking Health Literacy to Health Outcomes’.13 These are ‘Access and Utilisation of Healthcare’, ‘Provider-Patient Interaction’ and ‘Self-care’ groups. We grouped our outcomes into three categories: clinical, behavioural and patient-provider interaction.
Table 2. Causal pathway linking health literacy to health outcomes—mediators and outcomes of multimorbidity.
| Health outcomes | Mediator | Health literacy | References |
| Clinical indicators | |||
| 1.1 Treatment burden | Access and utilisation of healthcare, self-care | Health literacy independently predicts high treatment burden among individuals with multimorbidity | Eton et al, Friss et al, Selvakumar et al20 21 35 |
| 1.2 Medication adherence | Access and utilisation of healthcare, self-care | Health literacy reported as having a positive influence on medication adherence. | Yeung et al, Surailah et al, Selvakumar et al35 38 48 |
| 1.3 No. of chronic conditions | Access and utilisation of healthcare, self-care | Health literacy (difficulty in understanding health information) observed to be an independent indicator of number of chronic conditions. | Gurgel do Amarel et al, Liu et al, Friss et al, Pedersen et al21 24 29 32 |
| 1.4 Quality of life | Access and utilisation of healthcare, self-care, patient-provider interaction | Health literacy was observed as a predictor of health-related quality of life | Hajek et al25 |
| Behavioural indicators | |||
| 2.1 Knowledge related to chronic disease | Patient-provider interaction, | Health literacy reported to be the strongest predictor of knowledge related to chronic diseases | Liu et al, Maduka et al, Shrestha et al, Woodard et al, Yadav et al29 30 36 44 47 |
| 2.2 Self efficacy | Access and utilisation of healthcare, self-care | Self-efficacy mediated the relationship between health literacy and treatment adherence as well as treatment outcomes among patients with multimorbidity. | Liu et al, Wu et al, Wang et al29 42 45 |
| 2.3 Self-care | Patient-provider interaction | An inverse relationship was reported between health literacy and self-care among individuals with multimorbidity | Toci et al, 201541 |
| Patient-provider interaction outcome | |||
| 3.1 Understanding about health information | Patient-provider interaction | Patient-provider engagement influenced health literacy of individuals with multimorbidity.Relationship with healthcare provider found to be a determinant of health literacy | Dimir et al, Dinh et al, Stomer et al, Pedersen et al, Friss et alDimir et al, Dinh et al, Stomer et al, Pedersen et al, Friss et al15 15 16 16 21 21 32 32 50 50 |
Health literacy interventions among individuals with multimorbidity
Among the selected studies, only two studies assessed the role of an intervention to improve health literacy among multimorbid individuals. Both of these studies were conducted in the USA. In their study among multimorbid patients, Yeung et al48 reported a beneficial role of a health literacy education tool on medication adherence, and Eckman et al19 observed that the incorporation of an educational programme into clinical visits for patients with chronic disease improved disease-specific knowledge and outcomes.19 48
Discussion
Our systematic review appraised available evidence related to health literacy among individuals with multimorbidity. We observed limited health literacy in this population and a significant association between health literacy and multimorbidity. Health literacy mediated the relationship between social support and self-care, as well as self-management, which in turn impacted outcomes. Education and income were the most consistent determinants of health literacy among individuals with multimorbidity. Additionally, health literacy independently predicted treatment burden, medication adherence, health-related quality of life, number of chronic conditions, knowledge related to chronic conditions and healthcare utilisation.
Measurement tools and contextualisation
We identified a heterogeneous collection of literature that reported different tools for measuring health literacy. This diversity was expected, given that the concept of health literacy was first introduced in 1974.52 Initially, various interpretations and definitions of health literacy emerged, leading to the development of different measurement tools.6 Among the identified tools, the HLQ-9 and the HLS-EU were the most commonly used instruments for assessing health literacy among individuals with multimorbidity.
While these tools had broad applicability in HICs, their use in LMICs was found to be limited and required contextualisation. Most studies conducted in LMICs used unique health literacy tools or adapted existing tools to fit the local context. The healthcare systems in LMICs differ significantly from those in HICs in terms of resources, infrastructure, access to care, workforce, health outcomes and disease burden.53 Consequently, the constructs used for health literacy assessment in HICs may be less relevant in LMICs. To effectively measure health literacy in LMICs, it is crucial to contextualise tools to reflect local circumstances, ensuring cultural relevance and appropriateness. Addressing these contextual differences allows health literacy assessments to more accurately identify needs and improve health outcomes in LMICs.
Trends and implications
This review highlighted a concerning trend of limited health literacy among individuals with multimorbidity. Specifically, studies using the HLQ-9 tool found that multimorbid individuals often lacked sufficient health information, regardless of the setting. Additionally, in low- and middle-income settings, there was also a limited understanding of health information. Having sufficient health information and understanding it thoroughly are crucial skills for people with multimorbidity, as they often need to navigate multiple sources of information to understand each disease they are dealing with.11
This underscores the importance of critical health literacy, which comprises advanced personal skills, comprehensive health knowledge, effective interactions with healthcare providers and the ability to make informed decisions. These skills impact health outcomes, increase healthcare utilisation and contribute to health inequalities.54 To address these challenges and strengthen individuals’ critical health literacy, it is essential to implement interventions that empower them to evaluate arguments effectively.55 This includes providing them with the tools and skills necessary to analyse and comprehend health-related information proficiently. By doing so, individuals can better navigate the complexities of managing their health conditions, make informed decisions about their care and ultimately improve their health outcomes.56
Association between multimorbidity and health literacy
The review demonstrated a significant association between multimorbidity and low health literacy in two subgroup analyses involving HLQ and HLS health literacy assessment tools. These findings are similar to those of Berkman et al, who observed that health literacy is associated with poor health outcomes.7 This reinforces the idea that health literacy is a key determinant of health and plays a crucial role in the management of multimorbid conditions. We observed that individuals with chronic conditions have limited health literacy compared with their counterparts without these conditions.
However, it remains difficult to conclude whether multimorbidity is a cause or an effect of inadequate health literacy since most of the included studies in this review were cross-sectional. Improvements in chronic conditions are often driven by lifestyle changes, with prevention and early screening being of primary importance.57 We observed that health literacy influences the social support an individual with multimorbidity receives, as well as their belief in their ability to manage their health (self-efficacy) and their self-management practices. Moreover, self-efficacy also determines health literacy’s influence on positive treatment outcomes. This interconnectedness emphasises the importance of addressing health literacy alongside social support and self-efficacy to achieve better results in managing chronic conditions.58
Communication and competence in multimorbidity management
Effective multimorbidity management and the enhancement of self-management practices require insight into both patient skills and the performance of healthcare systems and professionals in providing information that is easily accessible and comprehensible.59 Communication and counselling competence are critical in multimorbidity management, demanding specific skills from both patients and providers.60 Health literacy is a composite entity, where numerous factors are involved, and limited health literacy may act as a barrier to effective patient care.13
Factors such as knowledge related to chronic conditions, the number of chronic conditions, health-related quality of life and healthcare utilisation were found to be associated with health literacy. Similar observations were reported by Davey et al, who noted that health literacy influenced patients’ knowledge related to diabetes mellitus and ischaemic heart disease.61 Additionally, Liu et al in China suggested the importance of health literacy in preventing comorbidities, rather than just preventing a first chronic condition.62 Lastly, we found only two records demonstrating the effectiveness of health literacy interventions among individuals with multimorbidity, both of which represent HICs.19 48 Thus, more evidence is required to assess the impact of such interventions on outcomes among individuals with multimorbidity in LMICs.
Conclusion
This is the first comprehensive review to report global health literacy levels among individuals with multimorbidity, involving an extensive systematic hand search of literature, performed by a multidisciplinary team. This approach increased the validity of our study and offered a deeper and more comprehensive understanding of the role of health literacy in patients with multimorbidity. However, our evidence mainly reflects the situation in high- and middle-income countries, and the lack of evidence from low-income countries impedes a comprehensive depiction of the findings across the globe. The included articles reported the use of various tools to measure health literacy, but without a uniform method to classify health literacy levels’ adequacy. The variety of health literacy tools for measuring different aspects of health literacy restricted the extensiveness of the meta-analysis.
Future research directions
This review demonstrated an association between limited health literacy and multimorbidity. However, further assessment of the impact of different multimorbidity clusters on core health literacy is needed across all levels of healthcare. Identifying whether people with limited health literacy and certain multimorbidity patterns are at greater risk of worse health outcomes can lead to the creation of specific interventions to support these patients. Understanding these clusters is a potential path towards improving the management of multimorbidity and setting priorities.
Alongside this, it is essential to identify individuals with multimorbidity who have limited health literacy. This demands a uniform method to classify the adequacy of health literacy, taking into account the patient’s skills and the complexity of information. A possible course of action for future research could involve the contextualisation of widely used tools to enable more comprehensive comparisons of health literacy levels.
Finally, more longitudinal studies are needed to assess the trajectory of multimorbidity and health literacy, as the chronology of multimorbidity occurrence may also be significantly related to health literacy. Understanding how health literacy evolves over time in relation to multimorbidity can provide deeper insights into effective management strategies and interventions.
supplementary material
Acknowledgements
AC would like to thank Subhasish Naik and Kajal Samantaray for their contribution to this review.
Footnotes
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-073181).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: Not applicable.
Patient and public involvement: Patients and/or the public were not involved in the design, conduct, reporting or dissemination plans of this research.
Contributor Information
Arohi Chauhan, Email: arohi.chauhan@phfi.org.
Fernando Gregorio Linares-Jimenez, Email: f.g.linares.jimenez@umcg.nl.
Girish Chandra Dash, Email: julululu@gmail.com.
Janine de Zeeuw, Email: j.de.zeeuw@umcg.nl.
Archana Kumawat, Email: readmearchana@gmail.com.
Pranab Mahapatra, Email: drpranab@outlook.com.
Andrea F de Winter, Email: a.f.de.winter@umcg.nl.
Sailesh Mohan, Email: smohan@phfi.org.
Marjan van den Akker, Email: m.vandenAkker@allgemeinmedizin.uni-frankfurt.de.
Sanghamitra Pati, Email: drsanghamitra12@gmail.com.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.van den Akker M, Buntinx F, Knottnerus JA. Comorbidity or multimorbidity. Eur J Gen Pract. 1996;2:65–70. doi: 10.3109/13814789609162146. [DOI] [Google Scholar]
- 2.Nguyen H, Manolova G, Daskalopoulou C, et al. Prevalence of multimorbidity in community settings: A systematic review and meta-analysis of observational studies. J Comorb. 2019;9:2235042X19870934. doi: 10.1177/2235042X19870934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pati S, Sinha R, Panda M, et al. Profile of multimorbidity in outpatients attending public healthcare settings: A descriptive cross-sectional study from Odisha, India. J Family Med Prim Care. 2021;10:2900–14. doi: 10.4103/jfmpc.jfmpc_2436_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garin N, Koyanagi A, Chatterji S, et al. Global Multimorbidity Patterns: A Cross-Sectional, Population-Based, Multi-Country Study. J Gerontol A Biol Sci Med Sci. 2016;71:205–14. doi: 10.1093/gerona/glv128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poureslami I, Nimmon L, Rootman I, et al. Health literacy and chronic disease management: drawing from expert knowledge to set an agenda. Health Promot Int. 2016:daw003. doi: 10.1093/heapro/daw003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nielsen-Bohlman L, Panzer AM, Kindig DA. Health literacy: a prescription to end confusion. Washington (DC): National Academic Press (US); 2004. [PubMed] [Google Scholar]
- 7.Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 8.Kickbusch I, JrM P, Apfel F, et al. Health literacy: the solid facts. Copenhagen: World Health Organization Regional Office for Europe; 2013. p. 73. [Google Scholar]
- 9.Balakrishnan S, Karmacharya I, Ghimire S, et al. Prevalence of multimorbidity and its correlates among older adults in Eastern Nepal. BMC Geriatr. 2022;22:425. doi: 10.1186/s12877-022-03115-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tomita S, Aoki T, Ohde S, et al. Association between health literacy and multimorbidity: a nationwide, cross-sectional study of a Japanese population. BMJ Open. 2022;12:e052731. doi: 10.1136/bmjopen-2021-052731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Skou ST, Mair FS, Fortin M, et al. Multimorbidity. Nat Rev Dis Primers. 2022;8:48. doi: 10.1038/s41572-022-00376-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moola S, Munn Z, Sears K, et al. Conducting systematic reviews of association (etiology) Int J Evid Based Healthc. 2015;13:163–9. doi: 10.1097/XEB.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 13.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007;31 Suppl 1:S19–26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 14.Abd-Rahim SNH, Mohamed-Yassin M-S, Abdul-Razak S, et al. The Prevalence of Limited Health Literacy and Its Associated Factors among Elderly Patients Attending an Urban Academic Primary Care Clinic in Malaysia. Int J Environ Res Public Health. 2021;18:9044. doi: 10.3390/ijerph18179044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Demir N, Koz S, Ugurlu CT. Health literacy in chronic kidney disease patients: association with self-reported presence of acquaintance with kidney disease, disease burden and frequent contact with health care provider. Int Urol Nephrol. 2022;54:2295–304. doi: 10.1007/s11255-022-03124-5. [DOI] [PubMed] [Google Scholar]
- 16.Dinh HTT, Nguyen NT, Bonner A. Health literacy profiles of adults with multiple chronic diseases: A cross-sectional study using the Health Literacy Questionnaire. Nurs Health Sci. 2020;22:1153–60. doi: 10.1111/nhs.12785. [DOI] [PubMed] [Google Scholar]
- 17.Dinh HTT, Nguyen NT, Bonner A. Healthcare systems and professionals are key to improving health literacy in chronic kidney disease. J Ren Care. 2022;48:4–13. doi: 10.1111/jorc.12395. [DOI] [PubMed] [Google Scholar]
- 18.Dinh TTH, Bonner A. Exploring the relationships between health literacy, social support, self-efficacy and self-management in adults with multiple chronic diseases. BMC Health Serv Res. 2023;23:923. doi: 10.1186/s12913-023-09907-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eckman MH, Wise R, Leonard AC, et al. Impact of health literacy on outcomes and effectiveness of an educational intervention in patients with chronic diseases. Patient Educ Couns. 2012;87:143–51. doi: 10.1016/j.pec.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 20.Eton DT, Anderson RT, Cohn WF, et al. Risk factors for poor health-related quality of life in cancer survivors with multiple chronic conditions: exploring the role of treatment burden as a mediator. Patient Relat Outcome Meas. 2019;10:89–99. doi: 10.2147/PROM.S191480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Friis K, Lasgaard M, Pedersen MH, et al. Health literacy, multimorbidity, and patient-perceived treatment burden in individuals with cardiovascular disease. A Danish population-based study. Patient Educ Couns. 2019;102:1932–8. doi: 10.1016/j.pec.2019.05.013. [DOI] [PubMed] [Google Scholar]
- 22.Griese L, Schaeffer D, Berens EM. Navigational health literacy among people with chronic illness. Chronic Illn. 2023;19:172–83. doi: 10.1177/17423953211073368. [DOI] [PubMed] [Google Scholar]
- 23.Griva K, Yoong RKL, Nandakumar M, et al. Associations between health literacy and health care utilization and mortality in patients with coexisting diabetes and end‐stage renal disease: A prospective cohort study. British J Health Psychol. 2020;25:405–27. doi: 10.1111/bjhp.12413. [DOI] [PubMed] [Google Scholar]
- 24.Gurgel do Amaral MS, Reijneveld SA, Meems LMG, et al. Multimorbidity prevalence and patterns and their associations with health literacy among chronic kidney disease patients. J Nephrol. 2022;35:1709–19. doi: 10.1007/s40620-021-01229-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hajek A, König H-H. Frequency and Correlates of Multimorbidity Among the Oldest Old: Study Findings from the Representative 'Survey on Quality of Life and Subjective Well-Being of the Very Old in North Rhine-Westphalia (NRW80+).'. Clin Interv Aging. 2023;18:41–8. doi: 10.2147/CIA.S388469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hermans L, Van den Broucke S, Gisle L, et al. Mental health, compliance with measures and health prospects during the COVID-19 epidemic: the role of health literacy. BMC Public Health. 2021;21:1365. doi: 10.1186/s12889-021-11437-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Huang LY, Lin YP, Glass GF, et al. Health literacy and patient activation among adults with chronic diseases in Singapore: A cross-sectional study. Nurs Open. 2021;8:2857–65. doi: 10.1002/nop2.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hudon C, Fortin M, Poitras M-E, et al. The relationship between literacy and multimorbidity in a primary care setting. BMC Fam Pract. 2012;13:33. doi: 10.1186/1471-2296-13-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu Y, Meng H, Tu N, et al. The Relationship Between Health Literacy, Social Support, Depression, and Frailty Among Community-Dwelling Older Patients With Hypertension and Diabetes in China. Front Public Health. 2020;8:280. doi: 10.3389/fpubh.2020.00280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Maduka DO, Swanson MR, Markey K, et al. Health Literacy Among In-Care Older HIV Diagnosed Persons with Multimorbidity: MMP NYS (Excluding NYC) AIDS Behav. 2020;24:1092–105. doi: 10.1007/s10461-019-02627-0. [DOI] [PubMed] [Google Scholar]
- 31.Naik AD, Street RL, Castillo D, et al. Health literacy and decision making styles for complex antithrombotic therapy among older multimorbid adults. Pat Educ Couns. 2011;85:499–504. doi: 10.1016/j.pec.2010.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pedersen SE, Aaby A, Friis K, et al. Multimorbidity and health literacy: A population-based survey among 28,627 Danish adults. Scand J Public Health. 2023;51:165–72. doi: 10.1177/14034948211045921. [DOI] [PubMed] [Google Scholar]
- 33.Rheault H, Coyer F, Jones L, et al. Health literacy in Indigenous people with chronic disease living in remote Australia. BMC Health Serv Res. 2019;19:523. doi: 10.1186/s12913-019-4335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schaeffer D, Berens E-M, Vogt D, et al. Health Literacy in Germany - Findings of a Representative Follow-up Survey. Dtsch Arztebl Int. 2021;118:723–8. doi: 10.3238/arztebl.m2021.0310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Selvakumar D, Sivanandy P, Ingle PV, et al. Relationship between Treatment Burden, Health Literacy, and Medication Adherence in Older Adults Coping with Multiple Chronic Conditions. Medicina (Kaunas) 2023;59:1401. doi: 10.3390/medicina59081401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shrestha A, Singh SB, Khanal VK, et al. Health Literacy and Knowledge of Chronic Diseases in Nepal. Health Lit Res Pract . 2018;2:e221–30. doi: 10.3928/24748307-20181025-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stømer UE, Gøransson LG, Wahl AK, et al. A cross‐sectional study of health literacy in patients with chronic kidney disease: Associations with demographic and clinical variables. Nurs Open. 2019;6:1481–90. doi: 10.1002/nop2.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Suarilah I, Lin CC. Factors influencing self-management among Indonesian patients with early-stage chronic kidney disease: A cross-sectional study. J Clin Nurs. 2022;31:703–15. doi: 10.1111/jocn.15930. [DOI] [PubMed] [Google Scholar]
- 39.Sun S, Lu J, Wang Y, et al. Gender differences in factors associated with the health literacy of hospitalized older patients with chronic diseases: A cross-sectional study. Front Public Health. 2022;10:944103. doi: 10.3389/fpubh.2022.944103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Teles M, Kaya S. Health literacy of cardiology patients: determinants and effects on patient outcomes. Soc Work Health Care. 2021;60:656–73. doi: 10.1080/00981389.2021.2014615. [DOI] [PubMed] [Google Scholar]
- 41.Toci E, Burazeri G, Jerliu N, et al. Health literacy, self-perceived health and self-reported chronic morbidity among older people in Kosovo. Health Promot Int. 2015;30:667–74. doi: 10.1093/heapro/dau009. [DOI] [PubMed] [Google Scholar]
- 42.Wang W, Luan W, Zhang Z, et al. Association between medication literacy and medication adherence and the mediating effect of self-efficacy in older people with multimorbidity. BMC Geriatr. 2023;23:378. doi: 10.1186/s12877-023-04072-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wieczorek M, Meier C, Vilpert S, et al. Association between multiple chronic conditions and insufficient health literacy: cross-sectional evidence from a population-based sample of older adults living in Switzerland. BMC Public Health. 2023;23:253. doi: 10.1186/s12889-023-15136-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Woodard LD, Landrum CR, Amspoker AB, et al. Interaction between functional health literacy, patient activation, and glycemic control. Patient Prefer Adherence. 2014;8:1019–24. doi: 10.2147/PPA.S63954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wu Y, Wen J, Wang X, et al. Chinese Community Home-Based Aging Institution Elders’ Self-Management of Chronic Non-Communicable Diseases and Its Interrelationships with Social Support, E-Health Literacy, and Self Efficacy: A Serial Multiple Mediation Model. Patient Prefer Adherence. 2023;17:1311–21. doi: 10.2147/PPA.S412125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yadav UN, Lloyd J, Hosseinzadeh H, et al. Self-management practice, associated factors and its relationship with health literacy and patient activation among multi-morbid COPD patients from rural Nepal. BMC Public Health. 2020;20:300. doi: 10.1186/s12889-020-8404-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yadav UN, Lloyd J, Hosseinzadeh H, et al. Levels and determinants of health literacy and patient activation among multi-morbid COPD people in rural Nepal: Findings from a cross-sectional study. PLoS One. 2020;15:e0233488. doi: 10.1371/journal.pone.0233488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yeung DL, Alvarez KS, Quinones ME, et al. Low–health literacy flashcards & mobile video reinforcement to improve medication adherence in patients on oral diabetes, heart failure, and hypertension medications. J Am Pharm Assoc (2003) 2017;57:30–7. doi: 10.1016/j.japh.2016.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Matima R, Murphy K, Levitt NS, et al. A qualitative study on the experiences and perspectives of public sector patients in Cape Town in managing the workload of demands of HIV and type 2 diabetes multimorbidity. PLoS One. 2018;13:e0194191. doi: 10.1371/journal.pone.0194191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stømer UE, Wahl AK, Gøransson LG, et al. Exploring health literacy in patients with chronic kidney disease: a qualitative study. BMC Nephrol. 2020;21:314. doi: 10.1186/s12882-020-01973-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rheault H, Coyer F, Bonner A. Chronic disease health literacy in First Nations people: A mixed methods study. J Clin Nurs. 2021;30:2683–95. doi: 10.1111/jocn.15757. [DOI] [PubMed] [Google Scholar]
- 52.Tones K. Health literacy: new wine in old bottles? Health Educ Res. 2002;17:287–90. doi: 10.1093/her/17.3.287. [DOI] [PubMed] [Google Scholar]
- 53.Mounier-Jack S, Mayhew SH, Mays N. Integrated care: learning between high-income, and low- and middle-income country health systems. Health Policy Plan. 2017;32:iv6–12. doi: 10.1093/heapol/czx039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rubinelli S, Ort A, Zanini C, et al. Strengthening Critical Health Literacy for Health Information Appraisal: An Approach from Argumentation Theory. Int J Environ Res Public Health. 2021;18:6764. doi: 10.3390/ijerph18136764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.van der Heide I, Poureslami I, Mitic W, et al. Health literacy in chronic disease management: a matter of interaction. J Clin Epidemiol. 2018;102:134–8. doi: 10.1016/j.jclinepi.2018.05.010. [DOI] [PubMed] [Google Scholar]
- 56.Sykes S, Wills J, Rowlands G, et al. Understanding critical health literacy: a concept analysis. BMC Public Health. 2013;13:150. doi: 10.1186/1471-2458-13-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sinha R, Pati S. Addressing the escalating burden of chronic diseases in India: Need for strengthening primary care. J Family Med Prim Care. 2017;6:701–8. doi: 10.4103/jfmpc.jfmpc_1_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ann-Marie Lynch M, Vinceroy Franklin G. Strategies to reduce hospital mortality in lower and middle income countries (LMICs) and resource-limited settings. 2019. Health literacy: an intervention to improve health outcomes. [Google Scholar]
- 59.van der Gaag M, Heijmans M, Spoiala C, et al. The importance of health literacy for self-management: A scoping review of reviews. Chronic Illn. 2022;18:234–54. doi: 10.1177/17423953211035472. [DOI] [PubMed] [Google Scholar]
- 60.Pati S, Sinha R, Mahapatra P. Health Communication and Inter-professional Care in Context of Multimorbidity Management: Assessment of Health Professional Curricular Focus in India. Front Commun. 2021;6 doi: 10.3389/fcomm.2021.661930. [DOI] [Google Scholar]
- 61.Davey J, Holden CA, Smith BJ. The correlates of chronic disease-related health literacy and its components among men: a systematic review. BMC Public Health. 2015;15:589. doi: 10.1186/s12889-015-1900-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Liu L, Qian X, Chen Z, et al. Health literacy and its effect on chronic disease prevention: evidence from China’s data. BMC Public Health. 2020;20:690. doi: 10.1186/s12889-020-08804-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hopman P, Schellevis FG, Rijken M. Health-related needs of people with multiple chronic diseases: differences and underlying factors. Qual Life Res. 2016;25:651–60. doi: 10.1007/s11136-015-1102-8. [DOI] [PubMed] [Google Scholar]