Abstract
Abstract
Objectives
This study aimed to explore the spatial and temporal distribution of hepatitis C and its influencing factors in Chongqing, providing a scientific basis for the relevant departments to formulate targeted preventive measures for the high prevalence of hepatitis C in the region and population.
Design
We collected data on hepatitis C cases in Chongqing (located in the southwest of China) from 2014 to 2020, and analysed the spatiotemporal heterogeneity of hepatitis C incidence in different populations and identified factors that might influence the incidence of hepatitis C by constructing a Bayesian spatiotemporal model.
Settings
The study subjects included clinically diagnosed cases and confirmed cases of hepatitis C with current address in Chongqing and onset date between 1 January 2014 and 31 December 2020.
Participants
The study used aggregated data, including 33 900 clinically diagnosed cases and confirmed cases of hepatitis C.
Results
From 2014 to 2020, the high-risk areas of hepatitis C were primarily concentrated in the main and new urban areas of Chongqing. In contrast, the low-risk areas were mainly found in southeast and northeast Chongqing. There was also an increasing trend in the risk of incidence in the low-risk areas. Analysis of different populations revealed that men aged 45–59 years had a higher risk of developing hepatitis C in the main urban area compared with other age groups. Additionally, the risk for this population group showed an increasing trend in the southeast and northeast of Chongqing as well as the main urban area. Among women, the rising trend of hepatitis C risk was stronger for those aged 30–44 years in southeast Chongqing and for those aged 45–59 years in northeast Chongqing compared with other age groups. The analysis of influencing factors found that gross domestic product per capita, population density and the proportion of tertiary industry were associated with an increased risk of hepatitis C.
Conclusions
High-risk areas for hepatitis C virus were mainly located in the main and new urban areas of Chongqing, where the male prime-age population was the focus of prevention and treatment. In the future, the relevant authorities should concentrate on high-risk areas and at the same time strengthen screening and serological surveys for hepatitis C in low-risk areas and various populations, and raise public awareness of prevention, so as to reduce the incidence of hepatitis C.
Keywords: INFECTIOUS DISEASES, Epidemiology, Public health
STRENGTHS AND LIMITATIONS OF THIS STUDY.
This study used a Bayesian spatiotemporal model to explore the spatiotemporal heterogeneity of hepatitis C incidence and its factors.
This study explored the spatiotemporal characteristics of hepatitis C virus incidence across different gender and age groups.
The prevalence of hepatitis C was not characterised in this paper for different genotypes.
This study analysed social factors affecting hepatitis C but failed to include the patients’ distribution from infection to onset.
The study focused on Chongqing, China, limiting its global reference value.
Introduction
Viral hepatitis C (hepatitis C) is a systemic infectious disease caused by hepatitis C virus (HCV) infection with predominantly liver damage,1 which is one of the leading causes of cirrhosis, hepatocellular carcinoma and liver-related death.2 3 It can be transmitted through blood transfusion, sexual contact and needle sharing for injection drug use. Hepatitis C is extremely harmful to the health and lives of patients and is a serious social and public health problem worldwide. According to the WHO report, 58 million people worldwide suffered from chronic hepatitis C in 2019, and about 290 000 deaths attributed to related diseases.4 China has one of the worst HCV epidemics in the world, with the highest reported number of cases worldwide.1 In recent years, thanks to initiatives such as antiviral treatment, improved health facilities and increased public awareness, the number of reported cases of hepatitis C in China has remained relatively stable at around 2 00 000 cases per year,5 but the reported incidence of hepatitis C in southwest China has shown a certain upward trend.6,8 Therefore, it is necessary to explore the spatial and temporal characteristics of hepatitis C incidence and related influencing factors to provide a scientific basis for the prevention and treatment of hepatitis C.
Previous studies on the spatial epidemiology of hepatitis C focused on the epidemiological characterisation of hepatitis C-related morbidity9 or mortality,10 used spatial analysis methods such as spatial autocorrelation analysis and spatial scan statistics to determine the spatial and temporal clustering of hepatitis C.11,13 Although these studies provided a clear depiction of the temporal or aggregation of hepatitis C infection, they did not simultaneously consider the risk and trends of incidence across time, space or spatiotemporal interactions. Additionally, they failed to consider regional adjacencies and were unable to dissect the underlying determinants influencing hepatitis C. In contrast, the Bayesian spatiotemporal model incorporates the proximity information and decomposes the overall spatial relative risk (RR), the general temporal trend and the local trend from the spatiotemporal coupling process. This approach facilitates a detailed examination of the spatiotemporal heterogeneity of hepatitis C incidence at the country level, thereby enhancing the precision of the model’s estimates.14 In addition, a study assessing the burden of hepatitis C disease in China from 1990 to 2019 showed that the distribution of hepatitis C disease burden was characterised differently in different gender and age groups.15 However, most of the current studies were based on the general population and had not explored the spatial epidemiological characteristics at the country level for different gender and age groups. Some studies showed that hepatitis C incidence was closely related to socioeconomic factors,12 such as regional gross domestic product (GDP) per capita, population density and health facility availability, which could play a role in the incidence of hepatitis C. However, researchers have not reached a consensus in this regard due to differences in research periods or regions. For example, a study by Liu16 showed a negative association between regional annual per capita income and hepatitis C incidence, but no association was found in studies in Guangzhou17 and Shandong.18 Therefore, it is necessary to analyse the spatiotemporal distribution and potential influencing factors of hepatitis C in different subgroups of the population and to explore the spatiotemporal heterogeneity in different regions and populations.
Chongqing is located in southwestern China, and in a study by Qian,19 although Chongqing was not a hotspot for hepatitis C incidence, its increasing trend in risk was faster than the overall increasing trend in China and had a tendency to become a hotspot. Therefore, this paper explored the spatiotemporal distribution characteristics of hepatitis C in different populations using spatial autocorrelation analysis and Bayesian spatiotemporal model based on surveillance data from 2014 to 2020 in Chongqing, and included covariates to analyse the factors that might influence the incidence of hepatitis C on the basis of Bayesian spatiotemporal model, with a view to provide some reference for relevant departments to formulate hepatitis C prevention and control measures.
Materials and methods
Study area
Chongqing, one of the four major municipalities directly under the central government of China, is situated in southwestern China. Its socioeconomic development, population distribution and allocation of healthcare resources are relatively unbalanced, with more pronounced disparities among regions. Considering the above factors, Chongqing is divided into four regions: the main urban area (including 9 districts such as Yuzhong District), the new urban area (including 12 districts/countries such as Jiangjin District), the northeast (including 11 districts/countries such as Wanzhou District) and the southeast (including 6 districts/countries such as Qianjiang District) as shown in online supplemental figure 1. The main and new urban areas are relatively flat, economically developed, densely populated and rich in medical resources, while the northeastern and southeastern areas of Chongqing are mainly mountainous terrain, with poorer economic levels, lower population densities and a relative lack of medical resources. Detailed information on each region was shown in online supplemental table S1.
Data collection
The surveillance data for hepatitis C in Chongqing from 2014 to 2020 were derived from the reported cases in the China Disease Prevention and Control Information System (Disease Surveillance Information Reporting Management System). This data included the basic social demographic and clinical information, with case definitions based on the unified diagnostic criteria established by the Chinese Ministry of Health.20 The study excluded suspected cases from the case classification and included all clinically diagnosed and confirmed cases for analysis. The socioeconomic data of each district/country during the same period was obtained from the Chongqing Statistical Yearbook. A total of seven explanatory variables were selected from three aspects—economy, population and health—for the analysis of factors influencing the incidence of hepatitis C. These variables included per capita GDP, urban disposable income, population density, urbanisation rate, the proportion of tertiary industry and so on.
Statistical analysis
Data cleaning was performed using Excel 2016 and SAS V.9.4 software. The incidence rate of hepatitis C was defined as the number of cases divided by the number of resident populations in each district/country. ArcMap V.10.7 was used for spatial autocorrelation analysis. WinBugs14 software was used for analysis based on a Bayesian spatiotemporal model as well as for the identification of various factors influencing the development of hepatitis C. The visual representation of the above analysis results was done in ArcMap V.10.7 software.
Spatial autocorrelation analysis
Spatial autocorrelation analysis refers to the degree of correlation between the values of the same attribute of a variable on neighbouring spatial area units,21 and generally includes global spatial autocorrelation and local spatial autocorrelation analysis. Global spatial autocorrelation reflects the degree of spatial aggregation of attribute variables across the entire study area, while local spatial autocorrelation analysis assesses the degree of spatial aggregation within specific local areas. This can identify the specific types and locations of the aggregation areas. In this articl, we used Moran’s I index to illustrate the degree of spatial variation between the areas and their surrounding regions. The I value is between −1 and 1. I > 0 indicates the existence of spatial positive autocorrelation, with values closer to 1 signing a stronger degree of aggregated distribution. Conversely, values approaching −1 denote a more dispersed distribution. I = 0 suggests a random spatial distribution, indicating no correlation.22 The local Moran’s I index is employed to further analyse the similarity or difference between the incidence rate of a given district unit and that of the surrounding districts. In this study, it was used to measure the degree of spatial dependence between the morbidity of hepatitis C in one district and its neighbouring districts, and to determine its spatial aggregation pattern in the local context, including four types of local spatial relationships: high-high aggregation, high-low aggregation, low-high aggregation and low-low aggregation.23
Bayesian spatiotemporal model
Bayesian spatiotemporal model is based on Bayesian statistical ideas and uses prior distributions to represent the temporal and spatial variation in disease risk in terms of random effects. This model further refines the relationship between relevant factors and disease occurrence, and serves as a crucial tool for analysing the spatiotemporal effects of disease.24 To mitigate potential overdispersion due to varying incidences of hepatitis C across different regions, this study employed a Bayesian spatiotemporal hierarchical model based on Poisson distribution to model the number of cases , where ,. denotes the actual value of , denotes the expected number of incidences in region i at moment t, and denotes the RR of the disease, which is equal to the ratio of the actual number of incidences to the expected number of incidences in region i at moment t. Supposed there are k () factors influencing the onset and progression of a particular disease, a model is constructed using the logarithmic form of :
where is the intercept; and denote spatial structural and non-structural effects, respectively, where denotes the correlation effect between each district/country, which is distributed a priori as a conditional auto-regressive process with an spatial adjacency matrix W. If region i is adjacent to region j, then , otherwise . denotes the heterogeneity of the region itself, whose prior distribution obeys the normal distribution , and is the spatial risk of disease, which is influenced by economic conditions, medical resources and other relevant factors within the study period. denotes the time effect whose prior distribution usually obeys an auto-regressive process, and responds to the entire time trend common to all districts/countries; denotes the spatiotemporal interaction effect, whose prior distribution obeys the normal distribution , and responds to the trend of disease risk over time in each district/country. represents the k-th influencing factor of region i. is the corresponding regression coefficient, whose prior distribution obeys a normal distribution .
In constructing the Bayesian spatiotemporal model, three distinct models with different effects could be developed based on the fundamental form of Bayesian spatiotemporal model: the spatial effect model (), the space–time effect model (), and the spatiotemporal interaction effect model . The deviance information criterion (DIC) was used to select the most suitable Bayesian model for this study. A smaller DIC value indicates a better model fit.
Patient and public involvement
The patients and the public were not involved in the design of the study.
Results
Descriptive analysis
From 2014 to 2020, a total of 33 900 cases of hepatitis C were reported in Chongqing. The reported incidence rate increased from 12.18 per 100 000 to 17.26 per 100 000, with an average annual incidence rate of 15.66 per 100 000. The areas with the highest incidence were concentrated in the main urban area, characterised by a more developed economy and high population density, followed by the new urban area. From 2014 to 2020, the average annual incidence rate was 18.63 per 100 000 for men and 12.55 per 100 000 for women, yielding a male-to-female ratio of 1.56. In every year within this period, men exhibited a higher incidence rate than women. The age of patients with hepatitis C was predominantly concentrated in the 30–59 years age group, as shown in table 1. The occupational distribution was dominated by farmers, accounting for 33.32% of the total number of cases during the study period, as illustrated in online supplemental table S2.
Table 1. Incidence rate of hepatitis C per 100 000 people in Chongqing, 2014–2020.
| Features | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 |
| Region | |||||||
| Main urban | 21.21 | 23.64 | 22.80 | 25.39 | 25.21 | 25.63 | 25.47 |
| New urban | 14.17 | 17.11 | 18.51 | 16.82 | 15.91 | 17.63 | 19.24 |
| The northeast | 5.71 | 6.27 | 9.47 | 10.02 | 11.92 | 10.86 | 11.79 |
| The southeast | 2.99 | 4.88 | 5.97 | 7.91 | 6.02 | 5.58 | 5.39 |
| Gender | |||||||
| Male | 14.52 | 16.33 | 18.73 | 19.61 | 19.99 | 19.89 | 21.18 |
| Female | 9.67 | 11.94 | 13.43 | 13.50 | 13.03 | 12.92 | 13.18 |
| Age | |||||||
| 0–29 | 2.65 | 2.99 | 2.94 | 2.84 | 2.35 | 2.25 | 1.91 |
| 30–44 | 26.44 | 28.84 | 32.41 | 30.27 | 29.71 | 24.38 | 23.33 |
| 45–59 | 18.10 | 23.19 | 26.95 | 27.04 | 29.57 | 31.48 | 35.63 |
| ≥60 | 9.37 | 11.42 | 14.65 | 15.71 | 15.14 | 16.31 | 16.20 |
| Total | 12.18 | 14.19 | 16.15 | 16.62 | 16.59 | 16.47 | 17.26 |
Spatial autocorrelation analysis
The global spatial autocorrelation results (online supplemental table S3) indicated that Moran’s I values ranged from 0.27 to 0.43 during 2014 and 2020. All Moran’s I indices passed the significance test (p < 0.05), suggesting the presence of spatial aggregation of hepatitis C incidence at the country level. The results of further local autocorrelation analysis were shown in online supplemental figure 2. The high-high clusters were mainly distributed in the main urban area of Chongqing, while the low-low clusters were predominantly found in the northeast and parts of the southeast of Chongqing.
Bayesian spatiotemporal analysis
Based on the criterion of minimising DIC, a Bayesian model incorporating spatiotemporal interaction effect was ultimately selected for modelling (online supplemental table S4).
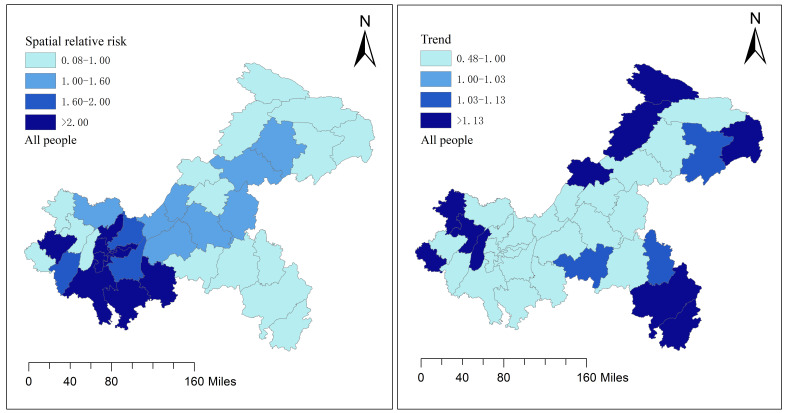
Spatiotemporal distribution of RR of hepatitis C in the whole population
Online supplemental figure 3 showed the trend of the RR of hepatitis C incidence in Chongqing over time from 2014 to 2020. The red line in the figure indicated a general increase of the RR of hepatitis C incidence over this period. Figure 1 depicts the spatial effects and spatiotemporal trend distribution of hepatitis C risk across the whole population of Chongqing. It was observed that areas with a high risk of hepatitis C were mainly concentrated in the main and new urban areas, while areas with a low risk were mainly located in southeast and northeast Chongqing. Additionally, a few low-risk areas were identified within the new urban area. The spatiotemporal trend map showed that the increasing trend in hepatitis C risk in low-risk areas was more rapid and higher compared with the overall trend.
Figure 1. Spatial effect and temporal trend of relative risk in the whole population. was the spatial risk of hepatitis C, which was influenced by economic conditions, medical resources and other relevant factors within the study period; described the trend of disease risk over time in each district/country.
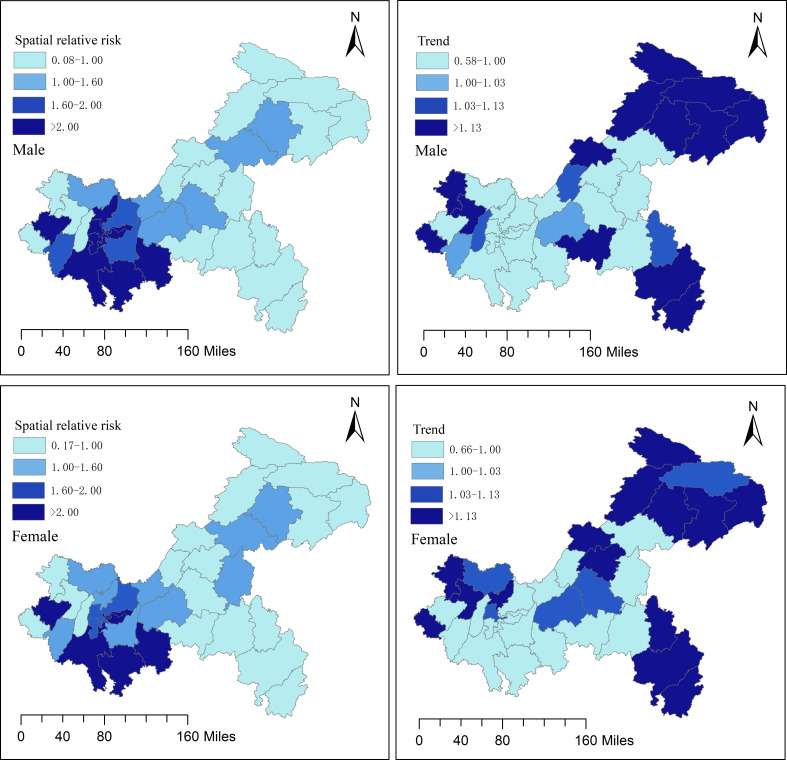
Spatiotemporal distribution of RR of hepatitis C in different gender groups
The RR of hepatitis C incidence among both male and female populations in Chongqing demonstrated a general increasing trend from 2014 to 2020 (online supplemental figure 4). Figure 2 shows the spatial effects and spatiotemporal trend distribution of hepatitis C incidence risk across genders. It was evident that the risk and trend distribution of hepatitis C incidence among different genders closely mirrored that of the overall population. In comparison, it was found that the RR of hepatitis C incidence in males was higher than in females within the main urban area.
Figure 2. Spatial effect and temporal trend of relative risk in different gender populations.
Spatiotemporal distribution of RR of hepatitis C in different age groups of men
The temporal trends of the RR of hepatitis C incidence across different age groups of men in Chongqing from 2014 to 2020 were depicted in online supplemental figure 5. All age groups showed an increasing trend, except for the 0–29 age group, which showed an overall decreasing trend. Online supplemental figure 6 showed the spatial effect and spatiotemporal trend distribution of the RR of hepatitis C incidence across different age groups of males in Chongqing. It could be observed that the spatial effect was more pronounced in the main urban area for males aged 45–59 years compared with other age groups. Additionally, this age group exhibited a higher increasing trend in the RR of hepatitis C incidence in the main urban area than the other age groups.
Spatiotemporal distribution of RR of hepatitis C in different age groups of women
The temporal trends of the RR of hepatitis C incidence in different age groups of women in Chongqing from 2014 to 2020 were depicted in online supplemental figure 7. All age groups showed an increasing trend, except for the 0–29 age groups, which showed an overall decreasing trend. Online supplemental figure 8 showed the spatial effect and temporal trend distribution of hepatitis C incidence risk among different age groups of women in Chongqing. It could be seen that the increasing trend of hepatitis C incidence risk among women aged 30–44 years was higher than other age groups in the southeast of Chongqing, which had a low incidence risk. Similarly, the increasing trend of hepatitis C incidence risk among women aged 45–59 years was higher than other age groups in the northeast of Chongqing, which also had a low incidence risk.
Analysis of influencing factors
In the univariate analysis (table 2), GDP per capita, population density, urbanisation rate and the proportion of tertiary industry were significantly and positively associated with the RR of hepatitis C, while disposable income and health expenditure of urban residents were not significantly associated with the RR of hepatitis C. Due to the strong correlation between GDP per capita and urbanisation rate (r = 0.868), as well as between urbanisation rate and population density (r = 0.870), three variables (GDP per capita, population density and the proportion of tertiary industry) were ultimately included in the model for multivariate analysis.
Table 2. Results of univariate regression analysis.
| Variable | Regression coefficient | 95% CI |
| GDP per capita (1000 yuan) | 0.012 | (0.010, 0.014) |
| Disposable income of urban residents (1000 yuan) | −0.002 | (−0.006, 0.001) |
| Population density (1000 people/km2) | 0.035 | (0.018, 0.049) |
| Urbanisation rate (%) | 0.030 | (0.030, 0.0312) |
| The proportion of tertiary industry (%) | 0.006 | (0.004, 0.007) |
| Number of beds in health institutions per 1000 population (Pieces) | 0.006 | (−0.001, 0.015) |
| Health expenditure (billion yuan) | 0.015 | (−0.012, 0.043) |
GDPgross domestic productpcspieces
Table 3 presented the results of the multivariate analysis. GDP per capita was associated with an increased RR of hepatitis C. Each 1000 yuan increase in GDP per capita was associated with a 1.2% (95% CI 0.1%, 1.3%) increase in the RR of hepatitis C incidence. Population density was associated with an increased RR of hepatitis C incidence, with a 1.6% (95% CI 0.2%, 3.2%) increase for every 1000 additional people per km2. The proportion of tertiary industry was also associated with an increased RR of hepatitis C. Each 1% increase in the proportion of tertiary industry was associated with a 0.8% (95% CI 0.6%, 1.0%) increase in the RR of hepatitis C.
Table 3. Results of multivariate regression analysis.
| Variable | Regression coefficient | 95% CI |
| GDP per capita (1000 yuan) | 0.012 | (0.001, 0.013) |
| Population density (1000 people/km2) | 0.016 | (0.002, 0.032) |
| The proportion of tertiary industry (%) | 0.008 | (0.006, 0.010) |
GDPgross domestic product
Discussion
Based on the number of reported hepatitis C cases and demographic data in Chongqing from 2014 to 2020, this study used spatial autocorrelation analysis and a Bayesian spatiotemporal model to analyse the spatiotemporal distribution characteristics and influencing factors of hepatitis C incidence in Chongqing.
The results showed that the overall incidence of hepatitis C in Chongqing exhibited an increasing trend between 2014 and 2020, with the average annual reported incidence rate higher than the national average19 and neighbouring provinces such as Guizhou6 and Chengdu.25 The high-risk areas for hepatitis C incidence were concentrated in the main and new urban areas, and men aged 45–59 years exhibited a higher risk of incidence in the main urban area compared with other age groups. Studies have shown that as the economy of China grows, there was a significant concentration of urban populations, exacerbating the spread of diseases such as hepatitis C and HIV, which are transmitted through blood and sexual contact.26 27 More developed tertiary sectors also meant that more people were exposed to sexually transmitted risk factors, thus increasing the risk of hepatitis C infection. This study analysed the factors influencing the development of hepatitis C and found that GDP per capita and the proportion of tertiary industry were significantly and positively correlated with the risk of hepatitis C in Chongqing. The tertiary industry refers to the service industry, which mainly includes the accommodation, catering and hotel industry, cultural, sports and entertainment industries, as well as the pedicure and hairdressing industry.16 With the continuous development of the economy, the healthcare service industry has gradually emerged and has even become a characteristic industry in some areas. However, if the tools used are not thoroughly sterilised, it can be detrimental to people’s health and potentially lead to the spread of infectious diseases. Surveys showed that the overall health status of public health facilities in China was generally good. However, certain places, such as footbaths and beauty salon places, exhibited low hygiene qualification rates and incomplete disinfection of public supplies.28 29 Related studies showed that some unhygienic living habits or inadequate disinfection of public supplies could increase the risk of hepatitis C infection,30 such as sharing razors, undergoing damaging cosmetic procedures and receiving pedicures. Therefore, the health sector should strengthen the management of hygienic sterilisation of tools and supplies used in the healthcare industry. In addition, in recent years, due to the rapid development of the urban economy, many rural populations migrated to the cities in search of better employment opportunities, greatly increasing the population density in the cities. This significantly increased the population density in urban areas, thereby exacerbating the burden of infectious diseases and facilitating their spread. The findings of this study were consistent with observation that farmer patients accounted for one-third of all cases and that population density was a risk factor for the development of hepatitis C. Some studies reported31 that most of the rural population working in cities were male, with over 50% being older than 40 years. This demographic exhibited low health awareness, engaged more readily in unprotected sex and were more likely to accept unorthodox healthcare services. These behaviours were attributed to the lower education levels, distance from their spouses and low economic incomes, all of which could lead to an increased risk of infections.32 Relevant departments should widely publicise the core messages of hepatitis C prevention and treatment for this population group, and raise the awareness of hepatitis C and encourage self-protection measures among the population. In addition, although the diagnostic criteria for hepatitis C specify anti-HCV and HCV-RNA testing as the basis for clinical diagnosis and confirmation of hepatitis C cases, relevant studies have found that the rate of HCV-RNA testing in tertiary hospitals is higher than that in non-tertiary hospitals and that tertiary hospitals have a relatively higher level of hepatitis C diagnosis and treatment.33 34 The main and new urban areas of Chongqing have better and more intensive medical resources, with tertiary hospitals and designated hospitals for infectious diseases mainly concentrated in the main and new urban areas. Relatively higher levels of hepatitis C detection and treatment, as well as ease of access in urban areas, have resulted in relatively high rates of diagnosis and reporting of hepatitis C, and maybe another reason why the main and new urban areas are at high risk of hepatitis C incidence.
The analysis of the spatial and temporal trends of the population in different regions revealed that the risk of hepatitis C incidence in low-risk areas exhibited a certain increasing trend. Notably, the risk of hepatitis C incidence among men aged 45–59 years showed an increasing trend in the main urban area with a high risk of incidence, as well as in the low-risk areas. The rising trend in the RR of hepatitis C incidence was more pronounced in women aged 30–44 years in the Southeast and in women aged 45–59 years in the Northeast compared with other age groups. Taken together, the results indicated that the risk of hepatitis C tended to spread from the main and new urban areas to the northeast and southeast. Due to the relatively poor healthcare resources in the southeast and northeast of Chongqing, there were likely issues such as physicians’ limited knowledge of hepatitis C screening, diagnostic processes and management standards.35 This could have led to the loss of patients with hepatitis C, thereby increasing the risk of hepatitis C infection in the population. Relevant departments should strengthen the attention of country hospitals to the diagnosis and treatment of hepatitis C, and enhance the training of doctors in hepatitis C-related knowledge. Second, with the continuous development of society and the increasing attention of the state, people’s health literacy had greatly improved. However, some studies found that the level of infectious disease prevention and control literacy among middle-aged and older individuals remained low.36 37 Therefore, it is necessary to strengthen the dissemination of health knowledge regarding infectious diseases among the population and focus on fostering healthy behaviours of residents.
There are some limitations of this study. First, this study did not analyse the epidemiological characteristics of different genotypes of hepatitis C, despite evidence suggesting that the distribution of hepatitis C genotypes varies across different regions.14 Further research can explore the spatiotemporal distribution characteristics of hepatitis C genotypes in different regions and among various populations. Second, this paper only discussed the factors influencing the development of hepatitis C from the aspect of social environment, while the transmission of hepatitis C is mainly through blood and sexual transmission, so this aspect such as injection history and risky sexual behaviours should be included in the study to obtain a more accurate explanation. Third, this study failed to include the distribution of patients with hepatitis C from infection to onset for analysis to trace the real influences on patients’ morbidity, which could be adjusted for healthcare resources using the estimated case values and include the distribution from infection to onset in subsequent studies, as well as examining the relationship with socioeconomic indicators. Fourth, this study did not consider the possibility that differences in testing rates could lead to biases in the spatial distribution of hepatitis C between urban and rural areas, and the impact of regional differences in testing on the findings needs to be considered in future studies. Finally, this study focused on Chongqing as the research area. While the findings can provide some insights for other similar megacities, their applicability to smaller cities or global contexts is limited.
Conclusions
The study found that the overall risk of hepatitis C in Chongqing showed an increasing trend, with high-risk areas primarily concentrated in the main and new urban areas, while low risk areas were mainly located in northeast and southeast Chongqing. The trend of hepatitis C incidence varied by region and population characteristics, with an increasing risk observed in low-risk areas, potentially due to socioeconomic, demographic or health-related factors. Therefore, when formulating hepatitis C prevention and control measures, the health department should tailor strategies to different regions and populations, and implement integrated prevention and control.
supplementary material
Acknowledgements
The authors thank all the funders of this study and all researchers related to the article.
Footnotes
Funding: This research was funded by Chongqing Municipal Health Commission Project (Grant No. 2020WTXM01).
Prepublication history and additional supplemental material for this paper are available online. To view these files, please visit the journal online (https://doi.org/10.1136/bmjopen-2023-077935).
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not applicable.
Ethics approval: All data in our study excluded any individual or household-level information. The data used were deidentified and aggregated at the population level, ensuring patient privacy. Additionally, this study was observational, we did not conduct any form of intervention or treatment on the subjects. We merely analysed existing data to explore the spatiotemporal distribution characteristics of hepatitis C and its influencing factors. Therefore, ethical approval was not required for this research.
Data availability free text: The data of hepatitis C cases analysed in this study were obtained from the Chongqing Centre for Disease Control and Prevention, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the above institution.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Contributor Information
Saijuan Chen, Email: 1959587676@qq.com.
Qiuting Wang, Email: 630191908@qq.com.
Yunyi An, Email: 1163378761@qq.com.
Ying Chen, Email: 2571341095@qq.com.
Hua Liu, Email: 925253608@qq.com.
Weijie Tan, Email: 1398023365@qq.com.
Xinyun Zhou, Email: 1289283641@qq.com.
Dianguo Xing, Email: 26890216@qq.com.
Yan Zhang, Email: zhangyan@cqmu.edu.cn.
Data availability statement
Data are available upon reasonable request.
References
- 1.Blach S, Terrault NA, Tacke F, et al. Global change in hepatitis C virus prevalence and cascade of care between 2015 and 2020: a modelling study. Lancet Gastroenterol Hepatol. 2022;7:396–415. doi: 10.1016/S2468-1253(21)00472-6. [DOI] [PubMed] [Google Scholar]
- 2.El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012;142:1264–73. doi: 10.1053/j.gastro.2011.12.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perz JF, Armstrong GL, Farrington LA, et al. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol. 2006;45:529–38. doi: 10.1016/j.jhep.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 4.WHO Progress report on hiv, viral hepatitis and sexually transmitted infections. 2019
- 5.Hei FX, Ye SD, Ding GW, et al. Epidemiological Analysis on Reported Hepatitis C Cases in China from 2012 to 2016. Biomed Environ Sci. 2018;31:773–6. doi: 10.3967/bes2018.103. [DOI] [PubMed] [Google Scholar]
- 6.Ding X, Gao QR. Epidemiological characteristics of viral hepatitis C in Tongren City, Guizhou Province, 2006-2020. Mod Prev Med. 2022;49:1003–5. [Google Scholar]
- 7.Peng Z, Wu SR., SR Epidemiological characteristics of viral hepatitis C in Chengdu, 2005-2017. Mod Prev Med. 2019;46:585–7. [Google Scholar]
- 8.Qiu ZF, Peng XB. Epidemiological characteristics of viral hepatitis C in a district of Chongqing from 2010 to 2015. J Trop Med. 2017;17:811–3. [Google Scholar]
- 9.Pereira FM, Santos FLN, Almeida M da C de, et al. Seroprevalence and Spatial Distribution of Hepatitis C Virus in Bahia, Brazil. Am J Trop Med Hyg. 2021;105:991–8. doi: 10.4269/ajtmh.20-1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yue T, Zhang Q, Cai T, et al. Trends in the disease burden of HBV and HCV infection in China from 1990-2019. Int J Infect Dis. 2022;122:476–85. doi: 10.1016/j.ijid.2022.06.017. [DOI] [PubMed] [Google Scholar]
- 11.Best N, Richardson S, Thomson A. A comparison of Bayesian spatial models for disease mapping. Stat Methods Med Res. 2005;14:35–59. doi: 10.1191/0962280205sm388oa. [DOI] [PubMed] [Google Scholar]
- 12.Butt ZA, Mak S, Gesink D, et al. Applying core theory and spatial analysis to identify hepatitis C virus infection “core areas” in British Columbia, Canada. J Viral Hepat. 2019;26:373–83. doi: 10.1111/jvh.13043. [DOI] [PubMed] [Google Scholar]
- 13.Stopka TJ, Goulart MA, Meyers DJ, et al. Identifying and characterizing hepatitis C virus hotspots in Massachusetts: a spatial epidemiological approach. BMC Infect Dis. 2017;17:294. doi: 10.1186/s12879-017-2400-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Daw MA, Buktir Ali LA, Daw AM, et al. The geographic variation and spatiotemporal distribution of hepatitis C virus infection in Libya: 2007-2016. BMC Infect Dis. 2018;18:594. doi: 10.1186/s12879-018-3471-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li SH, Zhang RX. Assessment of the disease burden of viral hepatitis C in China, 1990-2019. Chin J Infect Control. 2022;21:971–6. [Google Scholar]
- 16.Liu Y, Chen LZ. Spatial distribution characteristics of hepatitis C incidence in Hunan Province from 2011 to 2015 and its application of spatial lag regression model. Occup Health. 2016;32:2826–30. [Google Scholar]
- 17.Zhao YT, Xu MZ. Analysis of influencing factors of hepatitis C infection in Guangzhou. Prev Med. 2019;31:162–4. [Google Scholar]
- 18.Gu X, Yin TT. Study on epidemiological trends and influencing factors of viral hepatitis C in Shandong Province, 2007-2016. Chin J Epidemiol. 2018;39:1146–51. doi: 10.3760/cma.j.issn.0254-6450.2018.09.002. [DOI] [PubMed] [Google Scholar]
- 19.Qian J, Yue M, Huang P, et al. Spatiotemporal heterogeneity and impact factors of hepatitis B and C in China from 2010 to 2018: Bayesian space-time hierarchy model. Front Cell Infect Microbiol. 2023;13:1115087. doi: 10.3389/fcimb.2023.1115087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Health and Family Planning Commission of The People’s Republic of China WS 213-2018 Diagnosis for hepatitis C. J Clin Hepatol. 2018;34:1619–21. doi: 10.3969/j.issn.1001-5256.2018.08.006. [DOI] [Google Scholar]
- 21.Kirby RS, Delmelle E, Eberth JM. Advances in spatial epidemiology and geographic information systems. Ann Epidemiol. 2017;27:1–9. doi: 10.1016/j.annepidem.2016.12.001. [DOI] [PubMed] [Google Scholar]
- 22.Anselin L. Local Indicators of Spatial Association—LISA. Geogr Anal. 1995;27:93–115. doi: 10.1111/j.1538-4632.1995.tb00338.x. [DOI] [Google Scholar]
- 23.Chen W, Yang J, Jiang J, et al. A spatial analysis of the epidemiology of HIV-infected students in Zhejiang province, China. BMC Infect Dis. 2021;21:430. doi: 10.1186/s12879-021-06033-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zheng Y. Application of Bayesian spatiotemporal model in disease spatiotemporal data analysis. Chin J Prev Med. 2010;44:1136–9. [Google Scholar]
- 25.Xi J, Duan ZH. Epidemiological characteristics and prediction analysis of viral hepatitis C in Chengdu from 2012 to 2021. J Prev Med Inf. 2023;3:248–52. [Google Scholar]
- 26.Qiao X. Economic Development, Risky Behavior and Aids Epidemic. S C J Econ. 2011;0:54–67. [Google Scholar]
- 27.Tucker JD, Chen X-S, Peeling RW. Syphilis and Social Upheaval in China. N Engl J Med . 2010;362:1658–61. doi: 10.1056/NEJMp0911149. [DOI] [PubMed] [Google Scholar]
- 28.Shi AP, Xu L. Analysis of hygiene test results of public supplies in public places in Zhangjiagang City, 2013-2015. Chin J Disinfect. 2017;34:492–3. [Google Scholar]
- 29.Zhang WB, Niu QD. Investigation on sanitary condition of public articles in public places of Hebei province, 2020. Chin J Front Health Quar. 2020;45:305–7. [Google Scholar]
- 30.Qu LX, Shi Y, Chen KY, et al. Analysis of integrated HCV surveillance in Shanghai, 2014-2019. Zhong Liu Xing Bing Xue Za Zhi. 2021;42:626–31. doi: 10.3760/cma.j.cn112338-20200802-01009. [DOI] [PubMed] [Google Scholar]
- 31.Statistics., N.B.o Migrant workers monitoring survey report. 2021
- 32.Ding GW, Ye SD, Hei FX, et al. Sentinel surveillance for viral hepatitis C in China, 2016-2017. Zhonghua Liu Xing Bing Xue Za Zhi. 2019;40:41–5. doi: 10.3760/cma.j.issn.0254-6450.2019.01.009. [DOI] [PubMed] [Google Scholar]
- 33.Feng XF, Yu HL. Current status of hepatitis C diagnosis and treatment in Chinese medical institutions. Chin J AIDS STD. 2020;26:247–9. [Google Scholar]
- 34.Wen J, Ding GW. A study on the current status of hepatitis C diagnosis and treatment among patients attending nine hospitals in five provinces in China. Chin J AIDS STD. 2018;24:581–4. [Google Scholar]
- 35.Chen YX, Wu C. Establishment and implementation of hepatitis C screening and referral channels in the hospitals. Zhonghua Gan Zang Bing Za Zhi. 2020;28:820–3. doi: 10.3760/cma.j.cn501113-20200925-00531. [DOI] [PubMed] [Google Scholar]
- 36.Guo J, Zhu L. Infectious disease-related health literacy and its influencing factors among migrant populations in China: a cross-sectional analysis. Chin J Public Health. 2021;37:209–13. [Google Scholar]
- 37.Liu YX, ShenY LH, et al. Study on the trend of health literacy and its influencing factors in Chongqing, 2012-2016. Chin J Dis Control Prev. 2020;24:929–33. [Google Scholar]