Abstract
Background and objectives
The immersive virtual reality (VR) simulator is advantageous because it is cost-effective, realistic, can be controlled directly by the user, and can be integrated into education and training in otorhinolaryngology. The present study explored the feasibility of incorporating VR pure-tone audiometry (PTA) into an audiologist training curriculum, and assessed audiology experts’ willingness to use a VR PTA.
Materials and methods
A total of 31 audiologists (16 skilled audiologists and 15 undergraduate students) participated in the study, using a developed VR PTA application with a Meta Quest 2 device. A digital twin technique was applied for a realistic environment. The study measured key components of the VR system and behavioral intention to use VR PTA and traditional PTA using a modified version of the Technology Acceptance Model survey. The survey outcomes for VR PTA and the traditional PTA were compared, using a paired t-test and W test.
Results
The general characteristics of the participants were homogeneous. In the homogeneity test, no statistically significant differences were found between the ratings of VR PTA and traditional PTA. The comparison between VR PTA and traditional PTA revealed no significant differences between skilled audiologists and undergraduate students for all variables.
Conclusions
The VR PTA and traditional PTA had no differences in of VR system characteristics and behavioral intention to use. The efficacy of the VR PTA was validated, and previous experience with traditional PTA was not affected by adopting VR PTA. Further studies are needed to assess performance enhancements in audiological testing through VR simulation.
Keywords: Virtual reality, Digital twin, Pure-tone audiometry, Virtual simulation, Medical education
Highlights
-
•
VR PTA provide immersive environments for training of hearing tests.
-
•
VR PTA is validated in terms of features and feasibility as audiometry.
-
•
Audiologists aim to use VR PTA, showing no difference from traditional audiometry.
1. Introduction
Nowadays virtual reality (VR) simulators are increasingly used in training for various tasks. Training in a VR environment is realistic, cost-effective and ask for active participation of the trainee. Pure-tone audiometry (PTA) is a fundamental diagnostic tool in audiology for assessing an individuals' hearing sensitivity across a spectrum of frequencies. It is the gold standard for hearing assessments in audiological practice because of its objectivity, reliability, and ability to quantify hearing thresholds [1]. Hearing tests are pivotal in evaluating auditory capabilities and detecting potential impairment, fostering effective communication and collaboration within the audiology profession. Standardized hearing tests not only facilitate data exchange but also serve as a foundation for benchmarking, monitoring hearing health trends, informing evidence-based interventions and public health policies. However, the standardization of PTA is challenging due to biases (i.e., different setting across the institute and individualized test method) among audiologists [2]. To address this issue, it is important to educate audiologists about standardized protocols and tools which are based on real clinical data. By upgrading audiologists’ proficiency in PTA through comprehensive training, we can mitigate bias and ensure consistent and reliable evaluations. This educational initiative is crucial [3] for standardization in hearing testing, ultimately enhancing the quality of audiological care and tailoring interventions to individual needs.
With advancing technology, attention to training and/or clinical trials has increased. Various attempts have been made to apply traditional learning contents with the-state-of-the-art technology in medical education. A representative tool for training is the simulator. Using a simulator for training students can help achieve an effective practical education [4]. In the past decade, web-based and non-immersive training simulation have been adapted, demonstrating the feasibility of simulation for both surgical and audiological training [[5], [6], [7], [8]]. Initially, various audiometry methods, including web-based audiometry [5,7,[9], [10], [11]], as well as smartphone applications [12], were explored. Huang and colleagues highlighted the potential negative impact of traditional text-based education methods on learner motivation [6,13], necessitating the exploration of effective training methods [4,14].
Virtual reality (VR) is defined as the immersed real-time simulation of the user in an interactive environment that mimics reality, that is, simulation is extensively integrated into sensory-focused techniques [15]. This definition of VR emphasizes the use of VR for its immersive, interactive, and sensory-rich capabilities. The burgeoning role of VR simulators in medical education is a paradigm shift, providing a transformative platform for experiential learning that is both effective and ethically sound. The VR simulator is advantageous because it is cost-effective, realistic, and can be controlled directly by the students [4,16]. The main components of VR consisted of virtual environments, immersion, interaction, and sensory feedback [17]. Recent view of VR had III which represented Immersion, Interaction, and Imagination [18,19]. The concept of III of VR is central to understanding user engagement and technology acceptance in educational settings. Immersion defined as the stimulation of multiple sensory channels within a virtual environment. Immersion could be ranged from low (non-realistic) to high (realistic). Interaction which characterized by the real-time response of the virtual environment to user inputs was related to the level of interaction between user and VR system. Imagination referred to the capability of user to perceive non-existent things in real environment. Ünsaler and colleagues systematically reviewed the feasibility and validity of VR simulation in various specialties of otology such as temporal bone dissection, temporal bone simulator for mastoidectomy, and myringotomy [20]. The findings suggested that the VR simulator could improve pre-surgical planning, anatomical knowledge, and confidence of trainees. Moreover, the use of VR simulation in the medical education gave more educational opportunities for trainees which enhanced their proficiency [4].
Numerous studies have investigated the feasibility of hearing tests using VR simulators, such as the Hearing in Noise Test and sensory-focused tinnitus treatment [21,22]. However, there is a gap in the literature regarding VR-based hearing test in PTA, which is considered the gold-standard for determining the degree and type of hearing loss. A study by Sanderson (2013) investigated the feasibility of employing non-immersive VR-based pure-tone audiometry (VR PTA) with undergraduate students in audiology. The aim was to identify the interactivity between user and avatar in a virtual space and the confidence of routine PTA, including masking [23]. The study suggested that the use of VR PTA was feasible but could not replace traditional PTA training. Using the features of VR systems, including an immersive test environment and interactive user-simulation responses, the VR PTA simulation could provide a better understanding of audiometry construction and procedures, offering high proficiency without cost, space, and patient inconvenience limitations. We have developed an innovative VR simulator that offers a multitude of benefits and is designed to enhance the educational experience for audiologists-in-training. Firstly, the VR environment accurately recreates the real-world settings of audiometry, including the familiar sound booth (both inside and outside) and the meticulous details of interior spaces. This replication ensures that audiologists become accustomed to the environments they will encounter in their professional practice. Secondly, the inclusion of lifelike avatars representing men and women, further enriches the VR experience. These avatars exhibit reactions that closely resemble those of real patients, providing a dynamic and authentic dimension to the training. The incorporation of real working algorithms for PTA with accurate button functionalities ensures a hands-on and realistic simulation of the audiometric testing process [21]. This attention to detail aligns with the standard protocols of hearing tests established by the Korean Hearing Standard Center, which are rooted in the international ISO 8253-1 standard [24]. The implementation of this VR simulator in audiologist training holds immense potential to fulfill our objectives of achieving standardization in audiologists’ capabilities. The primary aim of this study was to assess the feasibility of incorporating VR PTA into audiology training curriculum. In addition, we aimed to examine the intention to use VR PTA with group of adult skilled audiologists and undergraduate students. Through a comprehensive investigation, we aim to evaluate the feasibility and potential acceptance of VR PTA as an effective tool in the education and training of audiologists.
2. Materials and methods
2.1. Participants
A total of 31 (female: 16, male: 15) audiologists participated in the current study. Of these, 16 were skilled audiologists, with over 3–15 years of experience conducting hearing tests including traditional PTA, who were working at a hearing aid distributor facility, national medical center, or local hospital. As part of hearing symposium, the audiologists participating in the current study were included in the hands-on session for the VR PTA training, conducted under the supervision of experts.
The remaining 15 participants were undergraduate students enrolled in a course of practice in behavioral audiometry. Before the semester initiation, the VR PTA training was assigned as a part of the course curriculum a 2-week program. The first week of the program was an introduction and practicum, and the second week was the examination. After learning the basic principle and practicum about PTA, such as masking, all the undergraduate students received 3 h of VR PTA training at each class supervised by the professor.
To control the differences in PTA knowledge, the skilled audiologists and the undergraduate students took the theoretical class for behavioral audiometry. Therefore, the only difference between two groups was the experience of clinic and practice with patients with hearing loss. Moreover, previous experience and types of the VR device was controlled. All the data were anonymized prior to analysis. All procedures for the present study were approved by the Institutional Review Board of the Wonju Severance Christian Hospital (approval number #CR323068).
2.2. Virtual reality pure-tone audiometry
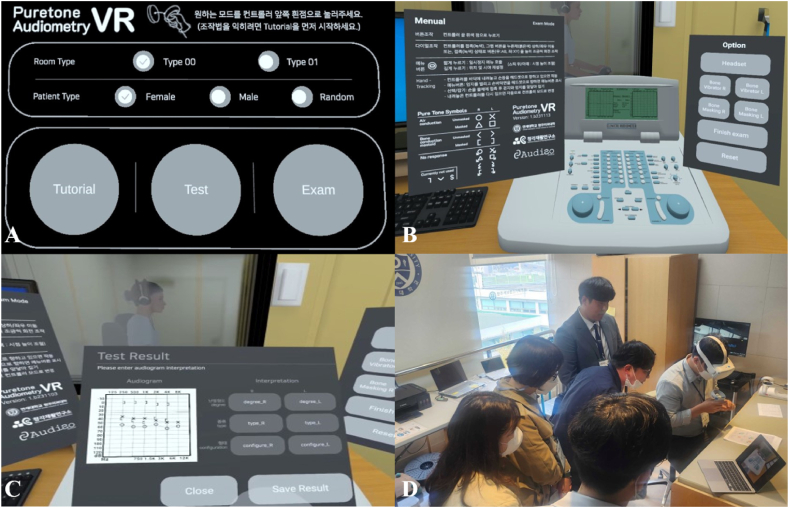
The VR PTA application was developed as the simulator for audiometry by using Unity (Juliani et al., 2018). Using Meta Quest 2 (Meta Platforms) which is at the moment the best-selling head-mounted display (As of 2023, the Meta Quest 2 device holds a market share of over 50 %; Worldwide Top 5 AR/VR Headset Companies, 2023Q2 UnitMarket Share) with high quality, affordability, and wireless usage. The user can experience immersive virtual environments with PTA setting. VR PTA was applied to a digital twin technology which can be referred to as a “digital equivalent of the physical product” [25,26]. Using this new technology, the actual space of the hearing lab in the Wonju Severance Christian Hospital was measured. After a three-dimensional (3D) scanning of the actual space, a 3D modeling and optimization was developed. In detail, the pipeline of create VR environment consisted of 4 steps such as 1) 3D scanning of real world environment, objects and devices using photogrammetry and LiDAR Scanning, 2) photograph in 360 degree of environment, 3) modelling of 3D space with sculping-based 3D modeling, and 4) gathering of real time rendering simulator and shading using Unity. In addition, the VR PTA used real time representation which could resemble real time interaction between the user and objects (such as an audiometer). All geometric structures in the VR PTA were optimized to the processor limits of the hardware, and the insufficient and/or less realistic structure of the system was compensated using mapping. Although the VR PTA is currently available in the Korean language, designing of a multi-language function (i.e., English) is under development. The VR PTA can be assessed in Meta store as App Lab (https://www.meta.com/ko-kr/experiences/6822059414492106/?utm_source=oculus&utm_medium=share). Because the frame rate under 75 Hz could cause dizziness in the user, the target frame rate of the VR PTA was set to 75–120 Hz. Although the VR PTA of the current version only provides air and bone conduction and masking function, further development for the speech audiometry is ongoing.
In this immersive VR environment, the user could interact with audiometry (GSI 61, Grason-Stadler, Eden Prairie, MN, USA), settings, and guidelines. There were three courses in the VR PTA including tutorial, test, and exam (see Fig. 1). The tutorial course provided a basic manual of VR PTA simulation, such as how to manipulate the dial and/or button on audiometry. The test course was designated to evaluate the full audiogram based on the hearing loss data of a real patient. The user conducted routine PTA and interacted with the patient avatar along with the manipulation of the audiometer. After completing the audiogram, the user could compare the completed audiogram to the real patient's audiogram. That is, the user can self-evaluate the audiogram. In the exam course, a brief and concise patient profile such as age, gender, and chief complaint were provided. Similar to the test course, the user conduct PTA and complete their audiogram according to the response of avatar. At the end of exam course, the user selected the degree, type, and configuration of hearing loss of the conducted audiogram. After the assessment, the audiogram was saved in the Meta Quest 2, enabling the supervisor to evaluate the results of audiogram. All participants performed three courses of the VR PTA and conducted the questionnaires.
Fig. 1.
Structure and function of the virtual reality pure-tone audiometry. A: Test mode and environment setting, B: Overview of virtual reality simulation, C: Test result of audiometry, D: Part of hands-on session for skilled audiologists.
To provide a convenient user experience, both the touch controller and hands tracking controller were provided. Although the hardware such as Meta Quest 2 basically provided a two-hand controller, typical audiometry was conducted manually. To overcome the heterogeneity of manual use on the VR PTA, the hand tracking controller function was made available and the user could easily manipulate the audiometry using their hands. In addition, the actual profiles of patients with hearing loss were used in the VR PTA as expressed by the avatar. Approximately 100,000 data on demographic information and matched hearing profiles such as audiogram, diagnosed degree, type, and configuration of hearing were adjusted. The VR PTA user could use audiometry simulations on hearing status, including air and bone conduction PTA and masking based on data from real patient data. Especially for the masking, clinically difficult cases such as masking dilemma were implemented for an experienced user in clinic.
2.3. Traditional pure-tone audiometry
To compare the feasibility and acceptance of the VR PTA for audiologists, previous experience with traditional PTA was included as control. In the current study, traditional PTA was defined as physically activated, manipulated, and commonly used audiometry equipment in the field of audiology and otology, such as GSI-61. It is obvious that the familiarity of traditional audiometry was higher than the VR PTA. Moreover, the participants of this study commonly certified the 2-year practicum course which addressed the manual and actual test of traditional PTA. Thus, the traditional PTA was selected as a reference for the VR PTA. All participants were conducted the questionnaire based on their clinical experience about traditional PTA.
2.4. Questionnaire
To investigate the main factors of VR simulation and efficacy, a modified version of the technology acceptance model (TAM) survey [27] was applied (see the Supplement 1). The TAM model, first introduced by Davis in 1989, was grounded in the Theory of Reasoned Action (TRA). Widely used to predict and explain user behavior towards technology. TAM has been validated in numerous studies across different fields, making it a robust framework for evaluating new technologies, including educational tools like VR simulators [19]. The model emphasis on user perceptions aligns well with the goal of assessing the feasibility and acceptance of VR PTA in audiologist training programs. By leveraging the TAM model, the present study ensures a systematic and validated approach to measuring the feasibility of VR PTA, providing valuable insights into its potential for integration into audiology training curricula. The TAM survey aimed to identify related effect among multidimensional factors on adaptation of new technology [27]. Although the components of TAM survey consisted of perceived ease of use (PEOU), perceived usefulness (PU), and intention to use (IU), various factors of the VR system such as sound, interaction, imagination, and immersion were added [19]. The current study was operationalized through the comparison of VR PTA with traditional PTA using the aforementioned outcome variables. That is, we investigated whether the VR PTA could achieve comparable results to traditional PTA in terms of user experience and acceptance.
A total of 43 items were included in the modified TAM survey for VR simulation. Specifically, three items for previous experience of VR device, five items for sound domain, six items for interaction domain, four items for imagination domain, four items for immersion domain, ten items for PEOU, six items for PU, three items for IU, and two items for subjective feedback. The Cronbach's alpha test was carried out to identify the reliability of variables on the VR PTA questionnaire and all domains showed high reliability from 0.81 to 0.92.
Another survey instrument was used for traditional PTA (see the Supplement 2). The construct of instrument was similar to the VR simulator. The modified version of TAM survey for traditional PTA contained four factors: sound, PEOU, PU, and IU. The survey for traditional PTA was revised with minor contextual correction such as term change for VR simulator into traditional PTA. We included a total of twenty-four items: five for sound domain, 10 for PEOU, 6 for PU, and 3 for IU. As with the questionnaire for the VR PTA, the reliability of the questionnaire for the traditional PTA was also evaluated using Cronbach's alpha test, with coefficients ranging from 0.79 to 0.88. The modified version of TAM survey for both VR simulation and traditional PTA was administered with a 5-points Likert scale (ranging from 1 which indicated “strongly disagree” to 5 which meant “strongly agree”). All participants were administered the modified version of TAM survey at the end point of the hands-on session and/or class. Two types of TAM survey, one each for the VR PTA and traditional PTA were administered. The participants used the VR PTA survey for their usage and traditional PTA for reference. All participants performed each questionnaire after final practicum of the VR PTA using paper and pencil.
2.5. Data and statistical analysis
To identify the feasibility and potential acceptance of VR PTA over traditional PTA, a homogeneity test was conducted using a paired t-test. The general characteristics (i.e., age, gender, previous experience of VR device, types of VR device used, and depending on glasses) and the outcome measures of the TAM survey of participants (i.e., sound, interaction, imagination, immersion, PEOU, PU, and IU) were used as variables. In addition, the independent t-test was used for between group comparison. All variables were pre-processed for the statistical analysis using R project for statistical computing version 4.3.2. The categorical variables were analyzed using nonparametric statistical methods, such as the chi-squared test. The interval scale variables were evaluated using parametric statistical methods, such as the paired t-test. In the event that a variable is deemed to be not normally distributed, a non-parametric test, such as the W test, is employed. In summary, the paired t-test was applied to the main outcomes such as sound, interaction, PEOU for VR PTA questionnaire and PEOU for traditional PTA questionnaire. Statistical significance was defined as p < 0.05.
3. Results
3.1. Characteristics of the enrolled participants
The general characteristics of enrolled participants were demonstrated in Table 1. Among the demographical information, the mean age of skilled audiologist (mean: 38.33 years, SD: 4.40) and undergraduate student (Mean: 22.07 years, SD: 1.58) were significantly different (t = 0.5189, p < 0.001). The ratio of sex was not significantly different (χ2 = 0.819, df = 1, p = 0.366). For the potential factors which could influence the results of VR PTA, previous experience of VR device (χ2 = 1.009, df = 1, p = 0.604), types of VR device (χ2 = 2.762, df = 4, p = 0.598), and wearing glasses (χ2 = 3.476, df = 1, p = 0.062) were not significantly different between skilled audiologists and undergraduate students.
Table 1.
General characteristics of enrolled participants (n = 31).
| Variables | Skilled audiologist (n = 16) | Undergraduate students (n = 15) | p-value |
|---|---|---|---|
| Age (years, mean ± SD) | 38.33 ± 4.40 | 22.07 ± 1.58 | < 0.001∗ |
| Sex (Male: Female) | 9:7 | 6:9 | 0.366 |
| Previous experience of VR device (numbers, %) | |||
| No experience | 3 (18.75 %) | 1 (6.67 %) | 0.604 |
| Under five times | 12 (75.00 %) | 13 (86.67 %) | |
| More than five times | 1 (6.25 %) | 1 (6.67 %) | |
| Countless | 0 (0.00 %) | 0 (0.00 %) | |
| Types of VR device used (numbers, %) | |||
| Wireless | 10 (47.62 %) | 6 (40.00 %) | 0.598 |
| Wired | 4 (19.05 %) | 2 (13.33 %) | |
| Attractions | 6 (28.57 %) | 3 (20.00 %) | |
| Head-mounted display | 0 (0.00 %) | 2 (13.33 %) | |
| Others | 1 (4.76 %) | 2 (13.33 %) | |
| Depending on glasses (Yes: No) | 7:9 | 2:13 | 0.062 |
Note: Values are expressed as mean ± standard deviation for continuous variables and number with percentage for categorical variables. VR, virtual reality; PTA, pure-tone audiometry; ∗statistically significant.
3.2. Homogeneity of virtual reality pure-tone audiometry
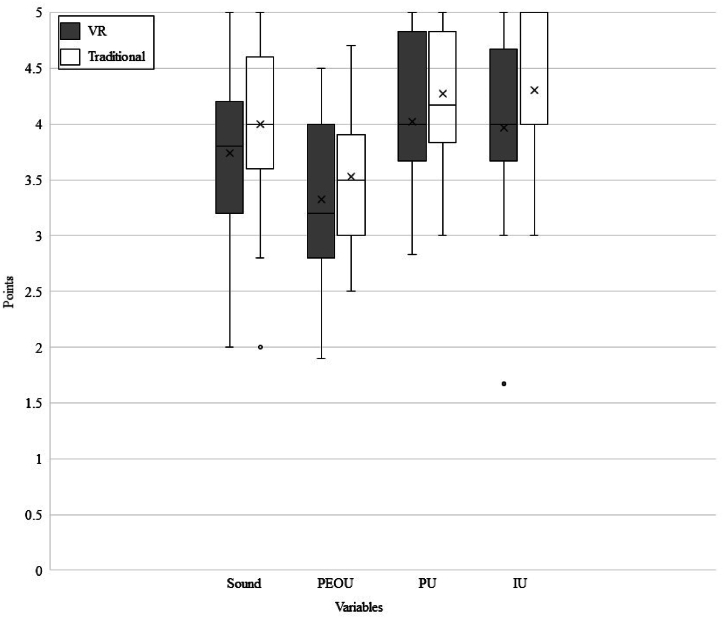
To investigate the feasibility of VR PTA and compare the traditional PTA device, a revised version of TAM survey was administered. Fig. 2illustrates the overall results of TAM survey for the VR PTA and traditional PTA. The results of the homogeneity tests demonstrated that there were no statistically significant differences between the various types of PTA for any variable. PU (p = 0.168) showed the highest score among the variables for both traditional PTA and the VR PTA. IU (p = 0.077) showed 4.30 points (SD: 0.62) for traditional PTA and 3.97 points (SD: 0.77) for the VR PTA. Sound (p = 0.190) showed 4.00 points (SD: 0.75) for traditional PTA and 3.74 points (SD: 0.73) for the VR PTA. PEOU (t = −1.240, df = 30, p = 0.225) was the lowest score among the variables for both the VR PTA and traditional PTA. Although the overall trend of the results implied that traditional PTA showed higher score than the VR PTA, the differences were not statistically significant. Thus, homogeneity of the VR PTA and traditional PTA was confirmed.
Fig. 2.
Results of revised version of TAM survey which compared the virtual reality and traditional pure-tone audiometry. Mean, IQR (interquartile range), and 95 % CI (confidence interval) of Sound showed 3.74, 0,90, and 3.48–4.00 for VR and 4.00, 0.80, and 3.74–4.26 for Traditional. PEOU showed 3.33, 1.05, and 3.08–3.58 for VR and 3.53, 0.90, and 3.32–3.74 for Traditional. PU showed 4.02, 1.08, and 3.77–4.27 for VR and 4.27, 0.92, and 4.07–4.47 for Traditional. IU showed 3.97, 0.83, and 3.70–4.24 for VR and 4.30, 1.00, and 4.08–4.52 for Traditional.
3.3. Between group comparison for virtual reality and traditional pure-tone audiometry
The between group comparison for virtual reality and traditional pure-tone audiometry was conducted to check for any statistical differences between skilled audiologists and undergraduate students.
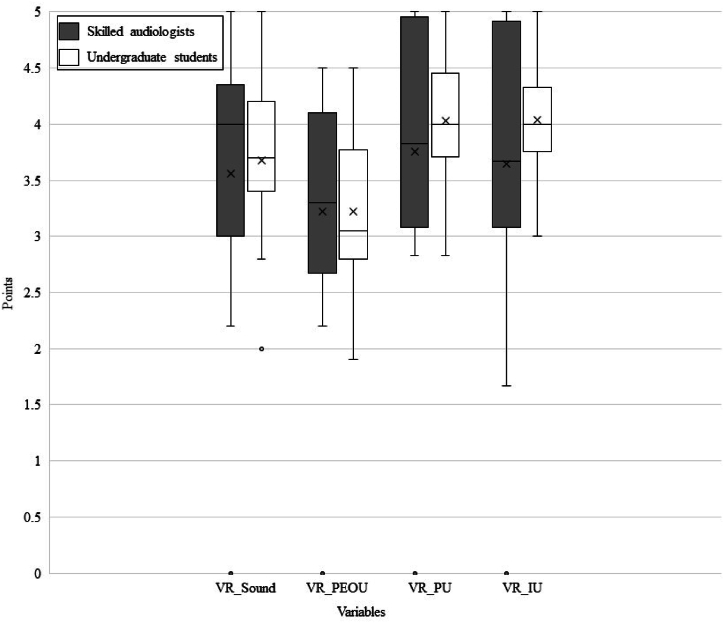
Similar to the homogeneity test, the results of between group comparison for the VR PTA showed that there were no significant differences for all variables. PU (p = 0.604) showed highest score for skilled audiologists and undergraduate students. IU (p = 0.474) showed that the undergraduate students had slightly higher score than skilled audiologists. Sound (p = 0.707) and PEOU (t = 1.178, df = 29, p = 0.248) showed that skilled audiologists showed higher score than undergraduate students. However, the differences of descriptive statistics between two groups were small and not statistically significantly different (see Fig. 3).
Fig. 3.
Results of between group comparison for the virtual reality pure-tone audiometry. Mean, IQR (interquartile range), and 95 % CI (confidence interval) of Sound showed 3.80, 1.20, and 3.40–4.20 for skilled audiologists and 3.68, 0.80, and 3.34–4.02 for undergraduate students. PEOU showed 3.43, 1.10, and 3.06–3.80 for skilled audiologists and 3.23, 0.93, and 2.89–3.57 for undergraduate students. PU showed 4.01, 1.59, and 3.58–4.44 for skilled audiologists and 4.03, 0.58, and 3.74–4.32 for undergraduate students. IU showed 3.89, 1.34, and 3.41–4.37 for skilled audiologists and 4.04, 0.41, and 3.76–4.32 for undergraduate students.
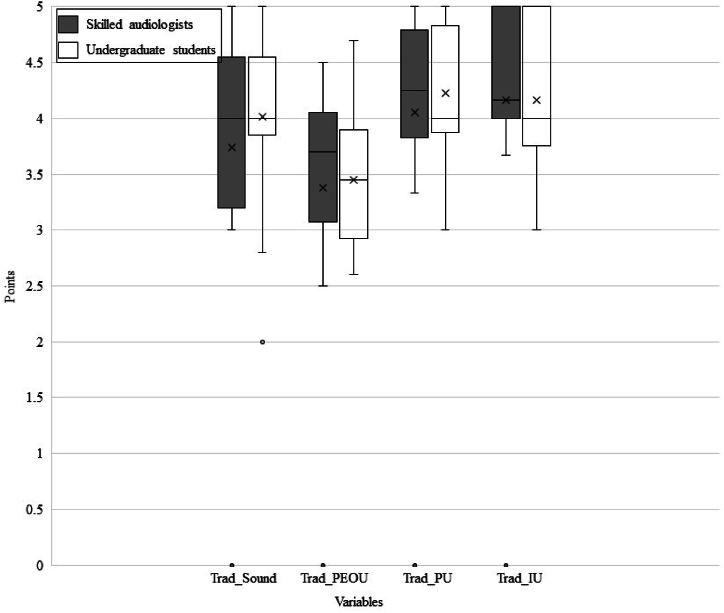
The results of between group comparison for the traditional PTA also demonstrated that there were no statistical differences between skilled audiologists and undergraduate students. Unlike the homogeneity test and between group comparison for the VR PTA, the IU was the highest score (p = 0.269) for skilled audiologists and undergraduate students. PU (p = 0.720) was showed 4.34 points (SD: 0.50) for skilled audiologists and 4.20 points (SD: 0.63) for undergraduate students. Sound (p = 0.856) showed 3.99 points (SD: 0.71) for skilled audiologists and 4.01 points (SD: 0.81) for undergraduate students. As expected, PEOU (t = 0.949, df = 29, p = 0.350) was lowest score for skilled audiologists and undergraduate students. The between group comparisons showed no statistically significant results, the skilled audiologists showed slightly higher IU (see Fig. 4). This suggested that the skilled audiologists had higher IU for traditional PTA because they had experience using it.
Fig. 4.
Results of between group comparison for the traditional pure-tone audiometry. Mean, IQR (interquartile range), and 95 % CI (confidence interval) of Sound showed 3.99, 1.30, and 3.62–4.36 for skilled audiologists and 4.01, 0.50, and 3.63–4.39 for undergraduate students. PEOU showed 3.61, 0.70, and 3.31–3.91 for skilled audiologists and 3.45, 0.93, and 3.15–3.75 for undergraduate students. PU showed 4.32, 0.84, and 4.06–4.58 for skilled audiologists and 4.23, 0.87, and 3.93–4.53 for undergraduate students. IU showed 4.44, 1.00, and 4.16–4.72 for skilled audiologists and 4.17, 1.08, and 3.84–4.50 for undergraduate students.
3.4. Subjective analysis of virtual reality pure-tone audiometry
Although the characteristics of the VR PTA were quantified using a questionnaire, the subjective satisfaction and related information of the VR PTA was also collected. Three features including interaction, imagination, and immersion which main components of immersive VR technology were measured to quantify the quality of VR simulation. Table 2 demonstrated the features, pros and cons of the VR PTA, and usage time for each group. For the total usage time of the VR PTA, skilled audiologists had 3 h in hands-on session and undergraduate students had 16 h in the part of class. Among the three features related to the VR system, both groups showed that immersion was the highest variable and Imagination and interaction were followed. These results suggested that skilled audiologist and undergraduate student were highly immersed in the VR system.
Table 2.
Features, Pros, and Cons and of the VR PTA for skilled audiologists and undergraduate students.
| Skilled audiologists (n = 16) | Undergraduate students (n = 15) | |
|---|---|---|
| Total usage time of VR PTA | 3 h in hands-on session | 16 h in class |
| Interaction (points, mean ± SD) | 3.87 ± 0.61 | 3.75 ± 0.73 |
| Imagination (points, mean ± SD) | 4.25 ± 0.72 | 3.85 ± 0.69 |
| Immersion (points, mean ± SD) | 4.30 ± 0.81 | 4.10 ± 0.35 |
| Pros |
|
|
| Cons_device |
|
|
| Cons_application |
|
|
Note: Values are expressed as mean ± standard deviation for continuous variables. VR, virtual reality; PTA, pure-tone audiometry.
Various opinions were collected about the VR PTA to determine the pros and cons. For the cons of the VR PTA, the device related issues and application related issues were distinguished. Opinion of the pros were 1) without limitations for time and space resources, 2) better understanding of the PTA derived from the realistic situation, 3) immersive environments and resources in the simulation, and 4) chance to practice with clinical data of patients with hearing loss. The cons for the VR PTA, especially for the device included 1) hard level of operating controller and fine manipulation of the dial in the simulation, 2) inconvenience of user wearing glasses, 3) mild dizziness with long-usage time of VR simulation, 4) pain in the neck due to relatively heavy device, and 5) blurred focus for some users even after the focus dial was adjusted. For the application which in line with the VR PTA, the most common opinion was the lack of type of audiometry because the current version of the VR PTA only implemented the GSI-61 audiometry. Also, suggestions on speech audiometry and simple response of avatar were absent. Especially for the response pattern of avatar, majority of participants complained that the avatar responded only set algorithms. In other words, the response of the avatar was honest and predictable.
4. Discussion
The current study investigated the feasibility of VR PTA in both clinics and medical education for skilled audiologists and undergraduate students. A modified version of the TAM survey provided key factors of the VR technology and behavioral intention to use it, ease of use, and usefulness. The result of between intervention (i.e., VR PTA and traditional PTA) comparison suggested that the comparison between the VR PTA and traditional PTA was not significantly different. To identify the possible effect of usage time and clinical experience on the result, the subgroup analysis was conducted using between group comparison on the VR PTA. The subgroup analysis results showed that there was no statistical difference between the two groups which suggested the main factor of VR and behavioral intention to use of the VR PTA was not different, regardless of the clinical experience. Thus the validity of the VR PTA was checked, and the feasibility was confirmed in both the clinical and educational setting.
4.1. Homogeneity of virtual reality pure-tone audiometry
Although the traditional PTA had relatively higher scores on all variables, the findings were not statistically significant. The general characteristics of the participants were homogeneous, hence, the current results suggest that the previous experience and/or types of VR device did not influence the results of the comparisons. The findings of the current study demonstrated that all audiologists agreed and/or strongly agreed on efficacy of the VR PTA in terms of sound, ease of use, usefulness and these combined results led to the behavioral intention to use. Among the common variables, the PU and IU showed higher score than other variables. The audiologists recognized the usefulness of the PTA and were willing to use it, regardless of the form of PTA such as VR device and traditionally treated device. The present study findings are similar to that reported by the Ünsaler et al. (2023). VR based simulators for cadaveric dissection did not show superiority over traditional methods, but there were certain advantages of using VR based simulators. Also, Ünsaler and colleagues suggested that VR technique could be an intermediate step in training for otorhinolaryngology [20]. To address the efficacy of the VR PTA, a validation process is needed. Especially for the validation process, concurrent validity which is defined as the comparison of the simulator to the gold standard, in this case, the traditional PTA. In other words, if there was no significant differences between intervention comparison such as the experimental intervention (the VR PTA) and control intervention (traditional PTA), it is reasonable to say that the VR PTA is feasible to use.
4.2. Group comparison for virtual reality and traditional pure-tone audiometry
Group comparison between clinic audiologists and students who majored in audiology demonstrated that there were no significant differences between the two groups (VR PTA and traditional PTA). Although the differences in scores were not large, skilled audiologists showed higher IU for traditional PTA than undergraduate students. This could be due to the differences in experience for PTA use. Obviously, skilled audiologists had more experience about PTA in clinics and were more familiar with traditional PTA. Moreover, skilled audiologist showed higher score than undergraduate students for all variables, except for the IU for the VR PTA which showed similar scores in both groups. Between group comparison for the VR PTA suggested that the VR PTA was feasible in both clinical and educational setting, regardless of the previous experience of audiometry. Zhao and colleagues investigated the effectiveness of VR education with comparison of traditional methods. They demonstrated that the pass rate of medical education was significantly higher when the VR system applied. As the subgroup analysis revealed that the use of VR system was effective, regardless of the professions such as freshmen, postgraduate, and hospital resident [3]. The result of Zhao et al. (2021) was similar with the finding of the current study which suggested that the application of VR system in education and/or clinic was efficient, independent of the professional expertise. These results may be derived from the characteristics of VR system such as III. Due to the interaction, imagination, and immersion of simulation using VR, it attracts strong student satisfaction for learning and knowledge acquisition [[28], [29], [30], [31]]. With various attempts to introduce the VR system, it is not just advantageous for motivating learner involvement and improving understanding of specific learning situations [32], but it substantially improves instructional effectiveness [33] and learning outcomes [34]. According to Lu et al. (2005), due to the growing complexity of contemporary medicine and the rapid pace of advancement, medical students are increasingly turning to VR training settings to simulate medical procedures [35].
4.3. Pros and cons of virtual reality pure-tone audiometry
The subjective analysis of the VR PTA showed that there were advantages and disadvantages of the use of the VR PTA. Positive feedback from subjects such as no limitation in time and space to perform audiometry, better understanding of audiometry related to sufficient time to observe and attractiveness of simulator and immersive environment and resources of VR PTA supported the finding of Baniasadi and colleagues [17]. They reported that there are several reasons for the advantage of the VR simulator, such as the improvement of the training performance without the limitation of time and space. However, no one will use VR simulator unless it is attractive and immersive. In this aspect, the VR PTA in the current study was highly immersive for the end users and provided an interactive learning experience that can enhance the understanding and retention of audiometry.
Despite the advantages of VR PTA, there were disadvantages of VR PTA, especially the device and application itself. Most of the cons of the VR device could be easily overcome by conducting the tutorial and increasing familiarity with the VR system. However, about 30–80 % of the users who experienced the VR device and function experienced VR-induced motion sickness or cybersickness, which includes dizziness, nausea, sweating, eye fatigue and subjective discomfort [17,36,37]. The frame rate of the VR simulator is closely related to motion sickness or cybersickness. A high frame rate of the VR simulator (at least 60 frames per second or higher) could be effective to reduce the side effect of VR device and feature to overcome the discomfort and dizziness experienced during or after using VR PTA [38]. Although the current version of VR PTA achieved 60 frames per second, further development is ongoing to achieve a targeted frame rate of 75–120 Hz on VR PTA.
4.4. Limitations of the study and future directions
There were various limitations of the current study. One of the limitations was the lack of long-term usage time. Although the VR PTA was used as the part of curriculum for undergraduate students and special hands-on session for skilled audiologists, the total duration of using VR PTA was relatively short. Thus, further studies are needed to evaluate the effectiveness of VR PTA with long-term duration. The other limitation was the effect of VR PTA on the actual performance such as pass rate for the students and accuracy of the audiogram as skilled audiologist. While the comparison of actual performance before and after intervention was not of primary interest in the current study, studies to quantify the change of performance on the use of VR simulation are needed.
The implementation of the VR simulator in audiologist training holds immense potential to fulfill our objectives of achieving standardization in the capabilities of audiologists. By immersing audiologists in realistic environments, providing exposure to diverse patient avatars, and incorporating authentic algorithms aligned with standardized protocols, the VR simulator ensures a comprehensive and standardized training experience. As audiologists undergo training and attain qualifications verified through this innovative tool, the benefits extend directly to the patients they will eventually examine. Audiologists trained with the VR simulator are equipped with a standardized skill set, ensuring a consistent level of proficiency across various aspects of audiometric testing. This not only enhances the quality of the capabilities of audiologists but also contributes to the overall standardization of audiological care. Patients undergoing examinations by audiologists trained with the VR simulator can expect a higher level of accuracy, reliability, and adherence to established protocols. Furthermore, the VR simulator serves as a means of verifying the qualifications of audiologists, ensuring that they meet predefined standards and benchmarks. This verification process adds a layer of assurance to both audiologists and patients, fostering a sense of trust in the competency and reliability of audiometric assessments [2]. The benefits derived from training audiologists with the VR simulator ultimately translate to improved patient care. Patients can have confidence in the proficiency and standardized capabilities of their audiologists, leading to more accurate diagnoses, personalized interventions, and an overall enhanced healthcare experience. The integration of VR technology in audiologist training not only elevates professional standards but also directly impacts the well-being and satisfaction of the patients they serve.
5. Conclusion
In conclusion, the perceived ease of use, perceived usefulness, and intention to use of a VR application for examination of a pure tone audiogram is comparable to that of traditional pure-tone audiometry and was not dependent on previous experience with traditional PTA. This evidence indicates that the VR application is suitable to use it as a training tool for pure-tone audiometry.
CRediT authorship contribution statement
Chanbeom Kwak: Writing – original draft, Visualization, Formal analysis, Data curation. Jinsook Kim: Writing – review & editing, Methodology, Formal analysis, Data curation. Hyunsook Jang: Writing – review & editing, Methodology, Formal analysis, Data curation. Woojae Han: Writing – review & editing, Visualization. Young Joon Seo: Writing – review & editing, Project administration, Funding acquisition, Conceptualization.
Data availability
The data that has been used is confidential.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
This work is supported by a research grant from "Regional Innovation Strategy (RIS)" through the National Research Foundation of Korea(NRF) funded by the Ministry of Education (MOE) (2022RIS-005), National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. NRF-2020R1A2C1009789) and Yonsei university Wonju College of Medicine (YUWCM 2022-02).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2024.e40795.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Musiek F.E., Shinn J., Chermak G.D., Bamiou D.E. Perspectives on the pure-tone audiogram. J. Am. Acad. Audiol. 2017;28(7):655–671. doi: 10.3766/jaaa.16061. [DOI] [PubMed] [Google Scholar]
- 2.Kocian A., Cattani G., Chessa S., Grolman W. An artificial patient for pure-tone audiometry. EURASIP J. Audio Speech Music Process. 2018;2018:1–11. [Google Scholar]
- 3.Zhao G., Fan M., Yuan Y., Zhao F., Huang H. The comparison of teaching efficiency between virtual reality and traditional education in medical education: a systematic review and meta-analysis. Ann. Transl. Med. 2021;9(3) doi: 10.21037/atm-20-2785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jung E.Y., Park D.K., Lee Y.H., Jo H.S., Lim Y.S., Park R.W. Evaluation of practical exercises using an intravenous simulator incorporating virtual reality and haptics device technologies. Nurse Educ. Today. 2012;32(4):458–463. doi: 10.1016/j.nedt.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 5.Lieberth A.K., Martin D.R. The instructional effectiveness of a web-based audiometry simulator. J. Am. Acad. Audiol. 2005;16(2):79–84. doi: 10.3766/jaaa.16.2.3. [DOI] [PubMed] [Google Scholar]
- 6.Huang H.M., Liaw S.S., Lai C.M. Exploring learner acceptance of the use of virtual reality in medical education: a case study of desktop and projection-based display systems. Interact. Learn. Environ. 2016;24(1):3–19. [Google Scholar]
- 7.Masalski M., Kręcicki T. Self-test web-based pure-tone audiometry: validity evaluation and measurement error analysis. J. Med. Internet Res. 2013;15(4) doi: 10.2196/jmir.2222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maytin M., Daily T.P., Carillo R.G. Virtual reality lead extraction as a method for training new physicians: a pilot study. Pacing Clin. Electrophysiol. 2015;38(3):319–325. doi: 10.1111/pace.12546. [DOI] [PubMed] [Google Scholar]
- 9.Honeth L., Bexelius C., Eriksson M., Sandin S., Litton J.E., Rosenhall U.…Bagger-Sjöbäck D. An internet-based hearing test for simple audiometry in nonclinical settings: preliminary validation and proof of principle. Otol. Neurotol. 2010;31(5):708–714. doi: 10.1097/MAO.0b013e3181de467a. [DOI] [PubMed] [Google Scholar]
- 10.Calandruccio L., Weidman D. Online simulation education for audiometry training. Am. J. Audiol. 2022;31(1):1–10. doi: 10.1044/2021_AJA-21-00121. [DOI] [PubMed] [Google Scholar]
- 11.Renganath P.P., Ramkumar V. Validation of web-based audiometry version of HEARZAP. PLoS One. 2023;18(3) doi: 10.1371/journal.pone.0283519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Masalski M., Grysiński T., Kręcicki T. Hearing tests based on biologically calibrated mobile devices: comparison with pure-tone audiometry. JMIR mHealth and uHealth. 2018;6(1) doi: 10.2196/mhealth.7800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McArdle G., Bertolotto M. Assessing the application of three-dimensional collaborative technologies within an e-learning environment. Interact. Learn. Environ. 2012;20(1):57–75. [Google Scholar]
- 14.Tsai W.W., Fung C.P., Tsai S.L., Jeng M.C., Doong J.L. The assessment of stability and reliability of a virtual reality-based intravenous injection simulator. Comput. Inf. Nurs. 2008;26(4):221–226. doi: 10.1097/01.NCN.0000304804.46369.5a. [DOI] [PubMed] [Google Scholar]
- 15.Maggio M.G., Latella D., Maresca G., Sciarrone F., Manuli A., Naro A.…Calabrò R.S. Virtual reality and cognitive rehabilitation in people with stroke: an overview. J. Neurosci. Nurs. 2019;51(2):101–105. doi: 10.1097/JNN.0000000000000423. [DOI] [PubMed] [Google Scholar]
- 16.Agazio J.B., Pavlides C.C., Lasome C.E., Flaherty N.J., Torrance R.J. Evaluation of a virtual reality simulator in sustainment training. Mil. Med. 2002;167(11):893–897. [PubMed] [Google Scholar]
- 17.Baniasadi T., Ayyoubzadeh S.M., Mohammadzadeh N. Challenges and practical considerations in applying virtual reality in medical education and treatment. Oman Med. J. 2020;35(3) doi: 10.5001/omj.2020.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sheridan T.B. Proceedings of the ACM Symposium on Virtual Reality Software and Technology. 2000, October. Interaction, imagination and immersion some research needs; pp. 1–7. [Google Scholar]
- 19.Barrett A.J., Pack A., Quaid E.D. Understanding learners' acceptance of high-immersion virtual reality systems: insights from confirmatory and exploratory PLS-SEM analyses. Comput. Educ. 2021;169 [Google Scholar]
- 20.Ünsaler S., Meriç Hafız A., Gökler O., Özkaya Y.S. Virtual reality simulation-based training in otolaryngology. Virtual Real. 2023;27(3):2561–2567. [Google Scholar]
- 21.Malinvaud D., Londero A., Niarra R., Peignard P., Warusfel O., Viaud-Delmon I.…Bonfils P. Auditory and visual 3D virtual reality therapy as a new treatment for chronic subjective tinnitus: results of a randomized controlled trial. Hear. Res. 2016;333:127–135. doi: 10.1016/j.heares.2015.12.023. [DOI] [PubMed] [Google Scholar]
- 22.Seol H.Y., Kang S., Lim J., Hong S.H., Moon I.J. Feasibility of virtual reality audiological testing: prospective study. JMIR Serious Games. 2021;9(3) doi: 10.2196/26976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sanderson E.A. University of Canterbury; Thesis: 2013. Evaluating the Use of A Virtual Reality Patient Simulator an an Educational Tool in an Audiological Setting. [Google Scholar]
- 24.Suh M.J., Lee J., Cho W.H., Jin I.K., Kong T.H., Oh S.H.…Seo Y.J. Improving accuracy and reliability of hearing tests: an exploration of international standards. Journal of Audiology & Otology. 2023;27(4):169. doi: 10.7874/jao.2023.00388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grieves M. Digital twin: manufacturing excellence through virtual factory replication. White paper. 2014;1(2014):1–7. [Google Scholar]
- 26.Liu M., Fang S., Dong H., Xu C. Review of digital twin about concepts, technologies, and industrial applications. J. Manuf. Syst. 2021;58:346–361. [Google Scholar]
- 27.Venkatesh V., Davis F.D. A theoretical extension of the technology acceptance model: four longitudinal field studies. Manag. Sci. 2000;46(2):186–204. [Google Scholar]
- 28.Silén C., Wirell S., Kvist J., Nylander E., Smedby Ö. Advanced 3D visualization in student-centred medical education. Med. Teach. 2008;30(5):e115–e124. doi: 10.1080/01421590801932228. [DOI] [PubMed] [Google Scholar]
- 29.Tworek J.K., Jamniczky H.A., Jacob C., Hallgrímsson B., Wright B. The LINDSAY Virtual Human Project: an immersive approach to anatomy and physiology. Anat. Sci. Educ. 2013;6(1):19–28. doi: 10.1002/ase.1301. [DOI] [PubMed] [Google Scholar]
- 30.Yammine K., Violato C. A meta‐analysis of the educational effectiveness of three‐dimensional visualization technologies in teaching anatomy. Anat. Sci. Educ. 2015;8(6):525–538. doi: 10.1002/ase.1510. [DOI] [PubMed] [Google Scholar]
- 31.Anderson S.J., Jamniczky H.A., Krigolson O.E., Coderre S.P., Hecker K.G. Quantifying two-dimensional and three-dimensional stereoscopic learning in anatomy using electroencephalography. npj Science of Learning. 2019;4(1):10. doi: 10.1038/s41539-019-0050-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shim K.C., Park J.S., Kim H.S., Kim J.H., Park Y.C., Ryu H.I. Application of virtual reality technology in biology education. J. Biol. Educ. 2003;37(2):71–74. [Google Scholar]
- 33.Levinson A.J., Weaver B., Garside S., McGinn H., Norman G.R. Virtual reality and brain anatomy: a randomised trial of e‐learning instructional designs. Med. Educ. 2007;41(5):495–501. doi: 10.1111/j.1365-2929.2006.02694.x. [DOI] [PubMed] [Google Scholar]
- 34.Merchant Z., Goetz E.T., Keeney-Kennicutt W., Kwok O.M., Cifuentes L., Davis T.J. The learner characteristics, features of desktop 3D virtual reality environments, and college chemistry instruction: a structural equation modeling analysis. Comput. Educ. 2012;59(2):551–568. [Google Scholar]
- 35.Lu J., Pan Z., Lin H., Zhang M., Shi J. Virtual learning environment for medical education based on VRML and VTK. Comput. Graph. 2005;29(2):283–288. [Google Scholar]
- 36.Roy M.J., Sticha D.L., Kraus P.L., Olsen D.E. Simulation and virtual reality in medical education and therapy: a protocol. Cyberpsychol. Behav. 2006;9(2):245–247. doi: 10.1089/cpb.2006.9.245. [DOI] [PubMed] [Google Scholar]
- 37.Pottle J. Virtual reality and the transformation of medical education. Future healthcare journal. 2019;6(3):181. doi: 10.7861/fhj.2019-0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Parsons T.D., Rizzo A.A. Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: a meta-analysis. J. Behav. Ther. Exp. Psychiatr. 2008;39(3):250–261. doi: 10.1016/j.jbtep.2007.07.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that has been used is confidential.