Dear Editor:
Scrub typhus is a mite-borne disease caused by Orientia tsutsugamushi. The common manifestations of scrub typhus include fever, pneumonia, liver dysfunction, and acute kidney injury [1]. Leukopenia and urinary tract infection (UTI) caused by O. tsutsugamushi have rarely been reported. Herein, we reported four scrub typhus cases presenting as UTIs with leukopenia in Shandong Province, China.
Case 1
A 67-year-old man presented to the hospital claiming fever, fatigue, muscle soreness, and cough. Enlarged lymph nodes in the groin and skin lesion produced by arthropod bite was observed. Laboratory results showed bronchitis, leukopenia, hematuria, and proteinuria, with the urine WBC (white blood cell) and RBC (red blood cell) counts being 19 and 89, respectively. Elevated AST (glutamic oxaloacetic transaminase), ALT (glutamic-pyruvic transaminase), and LDH (lactate dehydrogenase) were also observed (Table_1). He was suspected infected with severe fever with thrombocytopenia syndrome virus (SFTSV) or Brucella sp., then favipiravir and doxycycline were applied. However, subsequent tests were negative for both. On the 12th day, the symptoms were relieved and he left the hospital.
Case 2
A 70-year-old woman was admitted with fever, dizziness, fatigue, and muscle soreness for 26 days. Arthropod-bite lesion was recorded and skin rash was observed on the back, hip, and inner thigh. Laboratory results revealed leukopenia, hematuria, and proteinuria, with the urine WBC and RBC counts being 63 and 72, respectively. She was clinically diagnosed with rickettsial infection, invasive pulmonary aspergillosis, and septic shock. Meropenem, voriconazole, and doxycycline were applied. Since the 13th day, her laboratory indicators returned to normal. She left the hospital on the 15th day.
Case 3
A 50-year-old woman complaint fever, malaise, headache, chill, anorexia, joint soreness, throat dryness, and nausea for 7 days. Skin lesion, conjunctival congestion, and enlarged tonsils were also described. Hematuria, and proteinuria were indicated by urinalysis, with the urine WBC and RBC counts being 66 and 32, respectively. Routine blood tests also indicated leukopenia, thrombocytopenia, elevated PCT, and elevated LDH. Viral infection was suspected. Favipiravir and piperacillin tazobactam were used. Additionally, granulocyte colony-stimulating factor was applied to increase the WBC. On the 5th day, her body temperature became normal, and she was set free from the hospital.
Case 4
A 77-year-old woman was admitted with fever, fatigue, palpitation, and nausea. Arthropod-bite skin lesion was observed. Routine blood tests showed leukopenia, thrombocytopenia, elevated PCT, ALT, AST, and LDH. Meanwhile, laboratory data also showed hematuria, and proteinuria, with the urine WBC and RBC counts being 74 and 307, respectively. SFTSV infection and viral encephalitis were suspected. Favipiravir and ceftriaxone were applied for antiviral and antibacterial therapy. Glycerin fructose, albumin, and furosemide were also used for supportive treatment. On the 6th day, she was transferred to the ICU. However, the symptoms still worsened. On the 9th day, the patient gave up treatment and left the hospital.
Table 1.
Results of laboratory tests of the five patients on admission day and the retrospective serological test results.
| Reference Value | Case 1 | Case 2 | Case 3 | Case 4 | |
|---|---|---|---|---|---|
| Age | 67 | 70 | 50 | 77 | |
| Gender | male | female | female | female | |
| Blood test | |||||
| RBC (109/L) | 4.3–5.8 (male) | 3.98 | 2.55 | 4.08 | 3.73 |
| 3.0–5.0 (female) | |||||
| WBC (109/L) | 4–10 | 1.37 | 2.68 | 2.00 | 2.10 |
| PLT (109/L) | 125–350 | 28 | 110 | 90 | 53 |
| PCT (ng/mL) | 0–0.05 | 0.224 | 0.061 | 0.092 | 2.33 |
| ALT (IU/L) | 9–50 | 403 | 29 | 48 | 100 |
| AST (IU/L) | 15–40 | 228 | 53 | 45 | 53 |
| LDH (IU/L) | 120–250 | 930 | 447 | 380 | 566 |
| Urinalysis | |||||
| Urine Protein | – (negative) | +3 | +– | +1 | +2 |
| Urine Occult Blood | – (negative) | +2 | +2 | +– | +3 |
| Urine WBC Count | 0–28 | 19 | 63 | 66 | 74 |
| Urine RBC Count | 0–17 | 89 | 72 | 32 | 307 |
| IgG titer | 1:512 | 1:128 | 1:512 | 1:128 | |
| IgM titer | – | 1:64 | – | – | |
Abbreviations: RBC, red blood cell; WBC, white blood cell; PLT, platelet; PCT, procalcitonin; ALT, glutamic-pyruvic transaminase; AST, glutamic oxaloacetic transaminase; LDH, lactate dehydrogenase.
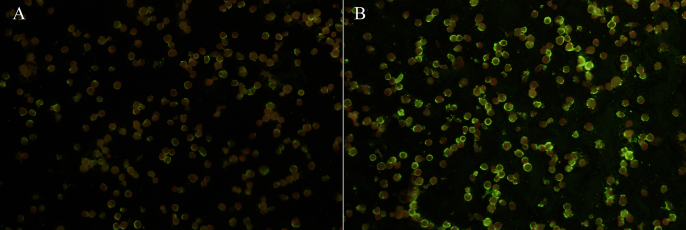
In a retrospective study, the serum samples of the patients were collected to screen for vector-borne pathogens. Immunofluorescence assay (IFA) test using an O. tsutsugamushi IFA IgG/IgM Kit (Fuller, USA) showed that all four cases were positive for O. tsutsugamushi. Recent or active infections were confirmed for cases 1, 2, and 3 (IgG titers of ≥1:512, or IgM titers of ≥1:64), while case 4 was infected at an undermined time (IgG titers of ≥1:128) (Table_1 and Figure_1). No other vector-borne pathogens were detected.
In this study, all four patients showed some symptoms in common: Hematuria, proteinuria, and increases in urinary WBC and RBC (except for the urinary WBC of Case 1), suggesting UTIs which has been rarely reported in these patients. In 2021, Liu et al. has reported a scrub typhus case presenting as a UTI [2]. As was previously reported, O. tsutsugamushi replicates in the vascular endothelium and mononuclear macrophages of humans, thus affecting almost all organs including the urinary system [3]. We suspect that this may be the mechanism of scrub typhus-associated UTIs. Leukopenia has been considered a criterion to differentiate SFTS against scrub typhus [4,5]. In our study, all four patients showed leukopenia, suggesting that leukopenia might be common in certain populations/areas and it might not always be a suitable criterion to differentiate scrub typhus and SFTS.
CRediT authorship contribution statement
Cuiping Wu: Data curation, Project administration, Resources. Miao Lu: Investigation, Methodology. Xuejun Dong: Data curation, Resources. Yitong Jiang: Investigation. Bo Liang: Data curation, Resources. Kun Li: Conceptualization, Data curation, Writing – original draft, Writing – review & editing.
Ethical approval statement
This work was approved by the Ethic Committee of Weifang Yidu Central Hospital.
Consent for publication
Not applicable.
Availability of data and material
Not applicable.
Funding
This work was funded by the National Nature Science Foundation of China (Grant No. 82361148725) and the National Key Research and Development Program (Grant No. 2021YFC2301202).
Declaration of competing interest
All authors declare no conflict of interest.
Handling Editor: Patricia Schlagenhauf
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.nmni.2024.101548.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
figs1.
References
- 1.Sun H., Lei L., Li J., Niu H., Yang J., Chen M. Clinical treatment of patients with scrub typhus-induced liver injury and intracranial infection. J Int Med Res. 2023;51(11) doi: 10.1177/03000605231214503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu M.F., Liu Y., Xu D.R., Wan L.G., Zhao R. mNGS helped diagnose scrub typhus presenting as a urinary tract infection with high D-dimer levels: a case report. BMC Infect Dis. 2021;21(1):1219. doi: 10.1186/s12879-021-06889-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeung Y.S., Kim C.M., Yun N.R., Kim S.W., Han M.A., Kim D.M. Effect of latitude and seasonal variation on scrub typhus, South Korea, 2001–2013. Am J Trop Med Hyg. 2016;94(1):22–25. doi: 10.4269/ajtmh.15-0474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim M.C., Chong Y.P., Lee S.O., Choi S.H., Kim Y.S., Woo J.H., et al. Differentiation of severe fever with thrombocytopenia syndrome from scrub typhus. Clin Infect Dis. 2018;66(10):1621–1624. doi: 10.1093/cid/cix1119. [DOI] [PubMed] [Google Scholar]
- 5.Sul H., Yun N.R., Kim D.M., Kim Y.K., Kim J., Hur J., et al. Development of a scoring system to differentiate severe fever with thrombocytopenia syndrome from scrub typhus. Viruses. 2022;14(5):1093. doi: 10.3390/v14051093. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.