Abstract
Background
This study aims to determine the impact of a childbirth educational intervention, based on empowerment theory, on childbirth experience and empowerment in women with fetal occiput posterior and occiput transverse malpositions.
Methods
A randomized controlled trial was conducted from February 2022 to December 2022 involving pregnant women with fetal occiput posterior and occiput transverse malpositions. Eligible women were randomly assigned to either the control or study group. The control group received routine care during childbirth, while the study group received routine care and a childbirth-empowering educational intervention delivered by midwives. Primary outcomes assessed were childbirth experience and patient perceptions of patient-empowering nurse behaviors in pregnant women. Secondary outcomes included pregnancy outcomes, delivery support and control, maternal coping behavior during delivery, maternal participation in delivery decisions, and perception of empowerment.
Results
A total of 137 pregnant women were enrolled, with 69 and 68 in the control and study groups, respectively. The study group showed significantly higher levels of childbirth experience and reported better patient perceptions of patient-empowering nurse behaviors than the control group. Additionally, the study group demonstrated higher levels of delivery support and control, maternal coping behavior, and specific aspects of perceived participation and patient perception of empowerment compared to the control group. There were no statistically significant differences in pregnancy outcomes between the two groups.
Conclusion
The childbirth empowering educational intervention effectively improved the childbirth experience and empowerment of women with fetal occiput posterior and occiput transverse malpositions. However, further studies are required to investigate its impact on pregnancy outcomes.
Trial registration
The study protocol was approved by the hospital ethics committee (approval number:2020140A01) and registered at the Chinese Clinical Trial Registry (registration number: ChiCTR2300070915; date of first registration: 26/04/2023).
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-024-07092-9.
Keywords: Childbirth education, Fetal malposition, Childbirth experience, Empowerment, Midwife
Background
Fetal occiput posterior and occiput transverse positions are the most common fetal head malpositions during delivery, accounting for 81.6% of labor dystocia [1]. Without appropriate management, persistent occiput posterior and occiput transverse positions could cause obstructed labor and lead to a painful, hopeless, and negative childbirth experience [2–4]. A negative childbirth experience could result in difficult breastfeeding, poor mother-infant relationships, and a high risk of maternal postpartum mental illness [5–7]. Therefore, these pregnant women should receive appropriate management to improve their childbirth experience.
Childbirth is a neuro-psycho-social event. Stress and fear could affect the labor process and the maternal psychological experience through the neurohormonal pathway [8]. Studies have shown that psychological stresses, medical interventions, and labor complications could all lead to negative childbirth experiences [9–13]. On the other hand, a better understanding of the labor process and perinatal interventions have been proven beneficial in relieving delivery pain, increasing the sense of self-control, reducing negative emotions and stress, and improving the positive childbirth experience in pregnant women [14]. It was reported that pregnant women could obtain necessary medical knowledge and respond to medical interventions by actively engaging in decision-making, thus maintaining a personal sense of accomplishment and control [15]. This process in which patients acquire the necessary knowledge, skills, attitudes, and self-awareness to improve themselves and others’ behaviors for a better quality of life is defined as empowerment [16]. During pregnancy, midwives are actively involved in pregnant women’s prenatal and peripartum care. Midwives could be ideal educators to provide pregnant women with professional care, knowledge, and childbirth empowerment [17].
During pregnancy, empowerment has been shown to improve the patient’s self-awareness, sense of self-control, self-management, and decision-making ability to achieve a high quality of life [18–20]. A previous qualitative study of pregnant women with difficult labor found that birth empowerment was a critical factor in achieving a positive childbirth experience [21]. Among various forms of empowerment, education has been widely used in different studies [22]. It was shown that empowerment education could be the most effective intervention to help women master early breastfeeding [23]. Another recent clinical trial successfully taught the empowerment of high-risk women to better understand high-risk pregnancies and related risk factors [24]. Therefore, implementing childbirth education based on the empowerment theory might improve the experience of pregnant women with the fetal occiput posterior and occiput transverse position malpositions, which have not been studied previously.
Here, we present our randomized clinical trial that applied the empowerment theory to educate pregnant women about the fetal occiput posterior and occiput transverse position malpositions. We hypothesized that empowering education in these pregnant women could improve their childbirth experience and perception of empowerment.
Methods
Study design and participants
This study was a single-center, parallel-group, randomized, controlled clinical trial conducted at Guangzhou Women and Children Medical Center, China, between February 2022 and December 2022. The study protocol was approved by the hospital ethics committee (approval number:2020140A01) and registered at the Chinese Clinical Trial Registry (registration number: ChiCTR2300070915. date of first registration: 26/04/2023 ). All study participants signed the informed consent prior to the study.
Pregnant women were included in the study if they met the following inclusion criteria, (1) between the ages of 18 and 45 years old; (2) singleton pregnancy; (3) full-term pregnancy; (4) undergoing vaginal delivery; and (5) persistent fetal occiput posterior or occiput transverse position confirmed by the ultrasound and vaginal examination when the cervix was dilated to 5 cm [25, 26]. Pregnant women were excluded from the study if they had severe pregnancy complications or severe pelvic malformations, inability to move limbs or with spinal joint abnormalities, mental illness, neurological disease, or severe vision and hearing impairment.
Study protocol
The purpose and study methods were explained to all the study participants. Baseline data were collected, including demographics, parity, and educational level.
Randomization
The random number generator in SPSS 26.0 software (SPSS, IBM, New York, USA) was used to randomly assign enrolled pregnant women into either the study group or control group at a ratio of 1:1. The process was completed by a research assistant, not involved in the data collection. The random number was kept in a sealed envelope.
Development of childbirth empowerment Manual
Based on the literature search, a Childbirth Empowerment Manual was formulated by five experts (three obstetricians and two midwives) with senior professional titles and more than 20 years of experience in labor and delivery. The intervention plan for empowering educational intervention was developed regarding the five-step and six strategies of empowering [27, 28]. The five steps and intervention modules are shown in Tables 1 and 2 for intrapartum and postpartum empowering education, respectively. The educational contents were, (1) Problem establishment. The midwife initially assessed the condition of the pregnant woman and then used open, guided questions to the pregnant women to help them understand the main issues. (2) Emotion expression. After establishing the problem, midwives encouraged pregnant women to express their emotions while giving positive guidance. (3) Goal setting. The goal was set to improve the understanding of fetal malpositions and self-managements in pregnant women. (4) Plan development and action. According to the goals set by the pregnant woman, guided language was used to direct pregnant women to propose methods to improve their own problems, strengthen their positive attitude, and encourage them to enter a state of self-management. The midwife made the plan regarding the birth empowerment manual. In implementing the plan, midwives communicated and gave feedback to pregnant women every 1–2 h and gave professional suggestions and affirmation according to the implementation situation. (5) Result evaluations. The midwife asked questions to enable pregnant women to review and summarize the empowerment process. Each intrapartum and postpartum empowering education took approximately one hour to complete. Pregnant women unable to complete the education process were excluded from the final analysis. The intrapartum empowering education was given once fetal malposition was diagnosed. The postpartum empowering was performed once a woman returned to the medical ward from the delivery unit or operating room.
Table 1.
Intrapartum childbirth empowering educational intervention in women with fetal occiput posterior or occiput transverse position during vaginal delivery
| Steps | Intrapartum intervention modules | |||
|---|---|---|---|---|
| Knowledge of labor and head dystocia | Understanding of head dystocia | Self-management skills | Delivery decision | |
| Problem establishment | Establish questions with open questions, such as: Do you know anything about childbirth? | Use open questions to guide pregnant women to realize issues, such as: Do you know how you are doing now? What are you most worried about right now? | Use open questions to establish questions, such as: Do you know how to change the position? Do you know how to adjust your mood? | Guide pregnant women to establish problems with open questions, such as: Based on what I have explained to you, how do you like to do now? |
| Emotion expression | Encourage pregnant women to express their true feelings and listen to their doubts and fears. | Pregnant women are encouraged to express their anxiety and confusion | Encourage pregnant women to express feelings, such as uncertainty and loss of control | Pregnant women are encouraged to express their opinions |
| Goal setting | Set goals with pregnant women to understand the delivery and head dystocia | Guide pregnant women to set goals and improve their self-awareness | Work with pregnant women to set goals, master posture management, and adjust emotions | Guide pregnant women to set goals and make decisions according to individual conditions |
| Plan development and action | Work with pregnant women to develop a plan to understand childbirth and head dystocia and provide professional knowledge support, such as sending education manuals and verbal and electronic education information. Inform pregnant women of the possible results and influencing factors of head dystocia, characteristics of labor, and possible duration and coordination skills. | Inform the pregnant woman of the current labor process and conditions, such as cervix dilation, amniotic fluid, and fetal heart rate. Give professional advice, including the advantages of vaginal birth, solving problems through position management and emotional adjustment, introducing possible difficulties in self-management, and encouraging family members to study together. | Through one-to-one demonstration, guide pregnant women to implement posture management methods, such as posture points and duration, breathing, touching, and musical analgesia | Make nursing plans together with pregnant women and their families. Inform the options and encourage pregnant women to make choices, such as position and delivery mode. Give them time to make choices. Provide professional advice for their choice. Respect the needs and choices of pregnant women. |
| Result evaluations | Pregnant women can master the relevant knowledge. | Pregnant women can correctly understand head dystocia and feel the support of medical staff and their families. | Pregnant women can actively implement body position management and adjust their emotions. | Pregnant women can actively participate in delivery decision-making. |
Table 2.
Postpartum empowering educational intervention in women with fetal occiput posterior or occiput transverse position
| Steps | Postpartum intervention modules | ||
|---|---|---|---|
| Postnatal nursing and breastfeeding-related knowledge | Knowledge and skills about breastfeeding | Breastfeeding decisions | |
| Problem establishment | Establish questions with pregnant women with open-ended questions, such as: Do you know the benefits of breastfeeding? Do you know how to carry out postpartum care? | Establish questions together with pregnant women with open-ended questions, such as: What do you think is the biggest difficulty in breastfeeding? | Establish questions with open questions, such as: Do you want to breastfeed? How do you want to breastfeed? |
| Emotion expression | Encourage pregnant women to express their doubts about breastfeeding and postpartum care. | Pregnant women are encouraged to express their lack of confidence and concern about breastfeeding. | Encourage pregnant women to express their own opinions. |
| Goal setting | Set goals with pregnant women to understand the benefits of breastfeeding and the key points of postpartum care. | Set goals together with pregnant women to correctly understand breastfeeding and master the methods of breastfeeding. | Guide pregnant women to set goals and decide according to their conditions. |
| Plan development and action | Through the education manual, oral education, and electronic education information. Inform pregnant women about breastfeeding and postpartum care benefits, such as wound care and dietary precautions. | Analyze the advantages of breastfeeding. Increase confidence by early exposure. Introduce possible difficulties in breastfeeding. Introduce breastfeeding clinics. Encourage families to learn to breastfeed together. Demonstrate breastfeeding skills | Maternal timing for breastfeeding. Understanding and respect for maternal choice. |
| Result evaluations | Pregnant women can master the relevant knowledge. | Pregnant women can correctly understand breastfeeding and build breastfeeding confidence, successfully performing their first breastfeeding. | Pregnant women can make choices according to their own wishes. |
Perinatal care and interventions
All enrolled pregnant women received routine prenatal care from midwives who had worked for more than five years in the perinatal care and delivery unit. The pregnant women in the control group received routine peripartum care. Midwives closely monitored and recorded the progress of delivery and the fetal status, including maternal cervix dilation, fetal descending, and uterine contractions. The pain was treated to ensure comfort during childbirth. The pregnant women in the study group received the childbirth educational course based on the empowerment theory. Before the study began, midwives involved in empowering education were trained on all the steps of interventions. Once a pregnant woman was confirmed to have the occiput posterior or occiput transverse position with cervical dilation ≥ 5 cm, the midwife educated and evaluated the pregnant woman based on the Childbirth Empowerment Manual.
Outcome measurements
Outcomes were evaluated and recorded within one day after the birth by the dedicated midwives who were unaware of the group assignment.
Primary outcomes
The primary outcomes included childbirth experience and patient perceptions of patient-empowering nurse behaviors in pregnant women.
The 2016 Chinese version of the Childbirth Experience Questionnaire (CEQ, version 2.0) was used to evaluate the maternal childbirth experience [29]. The scale included four dimensions (competence, participation, professional support, and safety perception), with 25 items in each dimension. Among them, 22 items were scored from 1 to 4 points corresponding to “complete disagreement” to “complete agreement.” Three items used the visual simulation scoring method, from 0 to 10 with 0 to 41, 5 to 62, 7 to 83, and 9 to 104. The Cronbach’s α coefficient was 0.81. The total score ranged from 25 to 100, with a higher score indicating a better maternal childbirth experience.
The Chinese version of the Patient Perceptions of Patient-Empowering Nurse Behaviors Scale was used to measure the perceptions of patient-empowering midwife behaviors in pregnant women [30]. It included six dimensions (authorization empowerment, information authorization empowerment, support authorization empowerment, resource, and opportunity authorization empowerment, informal authorization empowerment, and formal authorization empowerment) with a total of 35 items. The Likert 11 scoring method was used, with “never” and “always” corresponding to 0 to 10, respectively. A higher score indicated more perceived empowerment. The Cronbach’s α coefficient was 0.960.
Secondary outcomes
The secondary outcomes included pregnancy outcomes, delivery support and control, maternal coping behavior during delivery, maternal participation in the delivery decision, and perception of empowerment.
The pregnancy outcomes included delivery mode, gestational weeks, labor duration, maternal perineal laceration, presence of perineal lateral incision, postpartum blood loss, neonatal body weight, and Apgar score at 1 min and 5 min after birth.
The revised Support and Control in Birth scale was used to evaluate the maternal delivery support and control levels [31]. The scale adopted the Likert 5 rating method, from “complete disagreement” to “complete agreement” corresponding to 1 to 5. It had three dimensions (delivery support, internal control, and external control) with 33 items, including 9 reverse points [3, 4, 6–8, 12, 14, 18, 21] and a total score of 33–165. A higher score indicated better maternal delivery support and control. The Cronbach’sα coefficient was 0.916, and the test-retest reliability was 0.933.
The Childbirth Coping Behavior Scale, which included 16 items from the simplified Chinese version of the Self-efficacy Scale, was used to assess the degree of maternal coping behavior during delivery [32]. This scale adopted the Likert 4 scoring method. The pregnant women answered each item, with responses divided into never, rarely, sometimes, or frequent (scored 1 to 4 points). The sum of the scores from each item was the total score, ranging from 16 to 64 points. The Cronbach’sα coefficient was 0.86.
The Chinese version of Perceived Involvement in Care Scale had a Cronbach’s α coefficient of 0.73 to measure maternal participation in the delivery decision selection [33]. The scale had 13 items in three dimensions (physician encouragement and participation in decision-making, patient information acquisition initiative, and patient participation in decision-making). The total score was the sum of 13 items, with < 5 for low perceptual participation, 5 to 9 for moderate, and 10 to 13 for high perceptual participation.
The Chinese version of the Patient Perceptions of Empowerment Scale was used to evaluate the perception of empowerment in pregnant women [34, 35]. It included four dimensions (information, decision-making, individualization, and self-management), comprising 11 items. The evaluation method adopted the Likert 5 scoring method, with “complete disagreement” to “complete agreement” corresponding to 1 to 5, and a total score of 11–55. A higher score suggested a higher empowerment level. The Cronbach’ α coefficient was 0.81. The content validity index was 0.95.
Statistical analysis
Since we had two primary outcomes (childbirth experience and patient perceptions of patient-empowering nurse behaviors in pregnant women), we calculated the sample size estimation twice in PASS (version 15.0) as the followings, (1) the childbirth experience as the primary outcome. Based on a previous study [36] on the variable of childbirth experience, considering mean score 1 = 2.71, mean score 2 = 3.25 (assuming 20% increase in response to the intervention), standard deviation (SD) 1 = SD 2 = 0.73, two-sided test, with α = 0.05, a power of 90%, we required 40 cases in each group to reach a statistically significant difference between two groups. Considering a 20% lost-to-follow-up rate, we planned to collect at least 50 cases in each group. (2) patient perceptions of patient-empowering nurse behaviors in pregnant women as the primary outcome. Based on a previous study [37], the mean scores in the control and study groups were 226.9 and 264.5, with the SD of 46.5 and 44.7, respectively. In a two-sided test, with α = 0.05 and a power of 90%, we required 34 cases in each group to observe a statistically significant difference between two groups. Considering a 20% lost-to-follow-up rate, at least 43 cases were required in each group. After comparing the results from these two calculations, we decided to collect at least 50 pregnant women in each group to ensure our study had an adequate power for both primary outcomes.
Data analyses were performed by a statistician unaware of the group assignment. Continuous data are presented as mean ± SD or median with interquartile range and compared by the Student t-test or Mann-Whitney U test, depending on the normality test results by the Kolmogorov-Smirnov test. Categorical data are presented as numbers with percentages and compared by the Chi-square analysis or Fisher exact test. All the statistical analyses were performed in SPSS. A P < 0.05 was considered statistically significant.
Results
Participant enrollment and baseline comparisons
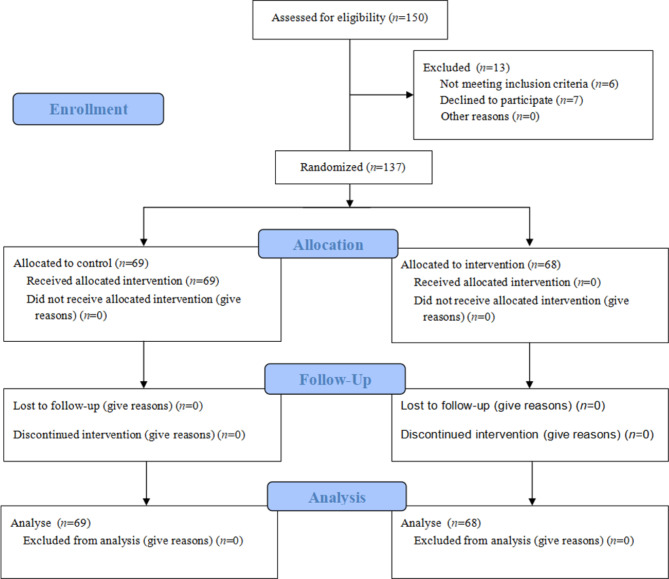
The study assessed 150 pregnant women. Among them, 13 patients were excluded (6 did not meet the inclusion criteria and 7 refused to participate into the study). Finally, 137 pregnant women were enrolled into the study, with 69 and 68 allocated to the control and study groups, respectively (Fig. 1). No participants were lost to follow-up or dropped off from the final analysis. Baseline characteristics were comparable between the two groups, with no statistically significant differences observed (Table 3).
Fig. 1.
CONSORT flowchart
Table 3.
Baseline characteristic comparisons between the study and control groups
| Characteristics | Total (n = 137) |
Control group (n = 69) | study group (n = 68) | P |
|---|---|---|---|---|
| Age, year, M ± SD | 30.4 ± 4.1 | 30.1 ± 3.4 | 30.7 ± 4.2 | 0.366 |
| Gravidity, median (IQR) | 2 (1, 2) | 1 (1, 2.5) | 2 (1, 2) | 0.721 |
| Parity, median (IQR) | 1 (1, 2) | 1 (1, 2) | 1 (1, 2) | 0.729 |
| Delivery experience, n (%) | 0.808 | |||
| Nulliparity | 96 (70.1) | 49 (71.0) | 47 (69.1) | |
| Multiparity | 41 (29.9) | 20 (29.0) | 21 (30.9) | |
| Educational level, n (%) | 0.793 | |||
| Middle school and below | 14 (10.2) | 6 (8.7) | 8 (11.8) | |
| Junior college | 59 (43.1) | 28 (40.6) | 31 (45.6) | |
| Undergraduate | 58 (42.3) | 32 (46.4) | 26 (38.2) | |
| Master or above | 6 (4.4) | 3 (4.3) | 3 (4.4) |
M ± SD, mean ± standard deviation; IQR, interquartile range
Primary outcome comparisons
The study group demonstrated significantly higher scores across all four dimensions of childbirth experience compared to the control group, indicating a notably better maternal childbirth experience in the study group than the control group (Table 4). Furthermore, the study group exhibited higher scores across all dimensions of patient perceptions of patient-empowering midwife behaviors compared to the control group, with statistical significance (Table 4). We further calculated the effect sizes and 95% confidence intervals. Except for safety perception measurement in childbirth experience, all other measurements showed significant better performance in the study group compared with the control group (Table 4).
Table 4.
Primary outcome comparisons between two groups
| Primary outcomes | Control group (n = 69) | Study group (n = 68) | P | Effect size | 95% Confidence interval |
|---|---|---|---|---|---|
| Childbirth experience | 70.86 ± 5.6 | 78.38 ± 6.0 | <0.001 | -8.000 | -10.000 to -6.000 |
| Competence | 22.3 ± 2.9 | 24.8 ± 2.9 | <0.001 | -3.000 | -4.000 to-3.000 |
| Participation | 13.9 ± 2.4 | 16.6 ± 2.4 | <0.001 | -2.000 | -3.000 to -1.000 |
| Professional support | 20.2 ± 2.3 | 21.8 ± 2.5 | <0.001 | -2.000 | -3.000 to -2.000 |
| Safety Perception | 14.5 ± 2.0 | 15.13 ± 1.5 | 0.033 | -0.000 | -1.000 to1.000 |
| Patient perceptions of patient-empowering midwife behaviors | 211.0 ± 85.0 | 302.6 ± 46.0 | <0.001 | -106.000 | -132.000 to -72.000 |
| Authorization | 23.6 ± 9.9 | 34.3 ± 6.2 | <0.001 | -12.000 | -15.000 to -9.000 |
| Information authorization | 34.9 ± 10.1 | 45.6 ± 5.8 | <0.001 | -13.000 | -15.000 to -7.000 |
| Support authorization | 42.4 ± 17.1 | 60.7 ± 10.3 | <0.001 | -22.000 | -27.000 to -15.000 |
| Resource and opportunity authorization | 53.3 ± 22.8 | 78.1 ± 13.7 | <0.001 | -29.000 | -35.000 to -21.000 |
| Informal authorization | 34.0 ± 16.5 | 49.5 ± 9.0 | <0.001 | -17.000 | -24.000 to -12.000 |
| Formal authorization | 23.0 ± 11.0 | 34.4 ± 6.0 | <0.001 | -13.000 | -17.000 to -9.000 |
Values are mean ± standard deviation
Secondary outcome comparisons
The pregnancy outcomes had no statistically significant differences between the two groups (Table 5). Other secondary outcome comparisons showed that the study group had better maternal delivery support and control and better maternal coping behavior than the control group (Table 6). Only one dimension in the perceived participation level (physicians encourage participation in decision-making levels) had a statistically significant difference between the control and study group. In the patient perception of empowerment, except for one dimension of self-management, all other dimensions were statistically higher in the study group than in the control group.
Table 5.
Pregnancy outcome comparisons between two groups
| Pregnancy outcomes | Control group (n = 69) |
Study group (n = 68) |
P |
|---|---|---|---|
| Mode of delivery, n (%) | 0.189 | ||
| Vaginal delivery | 26 (37.7) | 29 (42.6) | |
| C-section | 15 (21.7) | 21 (30.9) | |
| Assisted vaginal delivery | 28 (40.6) | 18 (26.5) | |
| Perineal lateral incision, n (%) | 37 (53.6) | 30 (44.1) | 0.266 |
| Perineal laceration, n (%) | 0.252 | ||
| No | 53 (76.8) | 54 (79.4) | |
| I°lacerated wound | 10 (14.5) | 13 (19.1) | |
| II°lacerated wound | 5 (7.2) | 1 (1.5) | |
| III°lacerated wound | 1 (1.4) | 0 (0.0) | |
| Neonatal body weight, gram, M ± SD | 3192.9 ± 361.0 | 3242.2 ± 357.8 | 0.423 |
| Labor duration, hours, M ± SD | 5.3 ± 0.7 | 4.8 ± 0.7 | 0.194 |
| Neonatal Apgar score, median (IQR) | |||
| 1 min | 10 (9, 10) | 10 (9, 10) | 0.335 |
| 5 min | 10 (10, 10) | 10 (10, 10) | 0.176 |
| Postpartum blood loss, mL, median (IQR) | 300.0 (250.0, 362.5) | 250.0 (200.0, 380.0) | 0.132 |
| Gestational weeks, median (IQR) | 39.7 (38.7, 40.4) | 39.7 (39.0, 40.3) | 0.693 |
M ± SD, mean ± standard deviation; IQR, interquartile range
Table 6.
Secondary outcome comparisons between two groups
| Secondary outcomes | Control group (n = 69) |
Study group (n = 68) |
P |
|---|---|---|---|
| Maternal delivery support and control | 100.8 ± 18.2 | 121.4 ± 17.6 | <0.001 |
| Delivery support | 44.0 ± 9.6 | 51.1 ± 7.2 | <0.001 |
| Internal control | 26.7 ± 5.3 | 33.1 ± 6.2 | <0.001 |
| External control | 30.1 ± 7.6 | 37.3 ± 9.0 | <0.001 |
| Maternal coping behavior | 42.2 ± 10.4 | 54.6 ± 8.9 | <0.001 |
| Patient perceived involvement | 8.0 ± 3.2 | 8.7 ± 2.9 | 0.173 |
| Physicians encourage participation in decision-making levels | 3.1 ± 1.8 | 4.2 ± 1.4 | <0.001 |
| Patient information acquisition initiative | 2.1 ± 1.0 | 2.1 ± 1.0 | 0.825 |
| Degree of patient involvement in decision-making | 2.8 ± 1.6 | 2.4 ± 1.8 | 0.163 |
| Patient perception of empowerment | 38.5 ± 8.8 | 45.3 ± 7.4 | <0.001 |
| Information | 10.5 ± 2.3 | 12.6 ± 2.1 | <0.001 |
| Decision-making | 7.8 ± 1.8 | 8.8 ± 1.5 | 0.001 |
| Individuation | 9.5 ± 3.3 | 12.5 ± 2.8 | <0.001 |
| Self-management | 10.8 ± 2.4 | 11.4 ± 2.4 | 0.093 |
Values are mean ± standard deviation
Discussions
This study represents the first investigation into the impact of childbirth education based on empowerment theory on the childbirth experience and empowerment levels of pregnant women with fetal occiput posterior or occiput transverse malpositions. The results of our study demonstrated that the childbirth experience and perceived empowerment in the study group were significantly higher compared to the control group. Additionally, there were notable increases in the levels of delivery support and control and coping in the study group.
Our intervention program adopted a comprehensive approach by actively involving both pregnant women and midwives in the process. Through empowerment-based childbirth education and the utilization of an empowerment manual, we sought to promote a collaborative and supportive environment during childbirth. The positive outcomes observed in the study group suggest that empowering women through education and collaboration with midwives can lead to enhanced childbirth experiences and increased feelings of empowerment. Our findings contribute to the existing literature highlighting empowerment’s benefits during childbirth.
In 2018, the World Health Organization recommended improving intrapartum care to promote a positive childbirth experience [38]. A new maternal care model is needed for a healthy and satisfactory childbirth experience [39]. It was reported that continuous, high-quality care and support during childbirth by midwives [40, 41], adequate medical information [42], patient participation in joint decision-making [43], and increased confidence in breastfeeding [44] could be the most effective strategies for creating a positive childbirth experience. Birth education and empowerment could improve maternal labor support, self-control, and delivery coping [20, 45, 46]. However, there is little literature on integrating effective strategies in pregnant women with fetal malpositions commonly resulting in poor childbirth experience. Therefore, we focused on how to deliver care to meet the requirements of pregnant women with fetal malpositions in the present study. We created a childbirth-empowering educational program that integrated midwife intervention, self-awareness, goal setting, and plan development and action. Our results showed significantly improved childbirth experience and perceptions of empowerment, maternal delivery support, control, and coping ability after the educational intervention.
A recent meta-analysis of 36 studies from 15 countries found that a positive childbirth experience was critical for maternal and fetal health during pregnancy [47]. The maternal childbirth experience could be improved by an educational curriculum implementing family planning [48]. When the delivery process is out of the expectation of pregnant women with fetal malpositions, the birth may induce guilt and a sense of failure. Therefore, it was proposed that pregnant women provide a “peer” care model during delivery [6]. This “peer” involves participating in the communication and companionship of pregnant women, constantly adjusting the relationship between pregnant women and the “peer” according to the actual situation to develop a common goal. In the present study, we used the midwives as the “peer” to the pregnant women with fetal malpositions and created an empowerment care model, which helps mothers to set different goals in different stages of labor and strive to adapt to the delivery process. Our study showed increased feelings of delivery support and control, coping behavior, self-control decision-making, and perceived empowerment in pregnant women. These findings suggested that incorporating empowerment and childbirth education into the intervention could effectively improve the birth experience.
We demonstrated that pregnant women receiving empowerment intervention care had higher perceived empowerment levels postpartum. This was similar to the findings from other studies on empowerment educational interventions [49, 50]. Empowerment is a process of making individuals undergo active behavior change, which has long been used for clinical disease management and control [51]. Empowerment education usually has five steps: problem determination, emotional catharsis, goal setting, confirmation plan, and behavior evaluation [52]. In our study, the determination of questions was carried out through discussions and interviews. The main problems and health needs of pregnant women were identified through open and guided questions. Health educators could find the current health status and potential issues in pregnant women through questions and analysis. In addition, the health educators used language, listening, and non-verbal ways to guide pregnant women to express their own feelings. The health educators gave full emotional support to pregnant women through communication to stimulate self-management awareness. Meanwhile, the health educators also encouraged the sense of responsibility of self-health management in pregnant women to facilitate problem-solving. In the goal-setting stage, health educators guided pregnant women to set goals for solving their health issues through conversations and give necessary neutral and professional suggestions, despite the final decision of the pregnant women. This method could help pregnant women determine reasonable and feasible goals and strengthen their self-management that could lead to a positive attitude. Confirmation of the plan means regular communication and feedback in solving problems. During the implementation process, health educators tentatively gave specific professional suggestions to ensure the correct and effective self-health behavior changes in pregnant women. Finally, through the behavior evaluation, we could affirm the goal to strengthen confidence, resulting in a benign cycle to improve self-assessment and find and solve problems proactively. Our study showed that empowerment education and care could be part of the intrapartum and postpartum care standard for women with fetal occiput posterior and occiput transverse malpositions. Midwives could play an essential role in empowerment education [24]. However, the empowerment level of midwives was not measured in this study, and further research on the relationship between midwife empowerment level and empowerment outcomes is needed in the future.
Previous studies on the relationship between the levels of empowerment and pregnancy outcomes were controversial. Some studies have found that women with higher levels of empowerment had more medical resources and could achieve better pregnancy outcomes [53, 54], but a meta-analysis did not report a link between women empowerment and improved prenatal care use [55]. We did not find any statistically significant differences between the study and control groups in the present study. The effects of maternal empowerment on pregnancy outcomes require further studies.
Limitations and prospects
Some limitations should be considered when interpreting our findings. First, the present study was conducted in a single center, which could limit the generalizability of our findings. Second, we only evaluated the short-term outcomes within one day during the postpartum period. The long-term effects of empowerment education are unknown. Third, we did not measure the level of empowerment in the midwives who were the “peer” the pregnant women. Future multicenter research with long-term follow-up periods should be performed to confirm our findings and investigate the impact of empowerment care on the relationship between the “peer” and the pregnant woman.
Conclusion
The results of this study demonstrated that childbirth-empowering educational intervention significantly improved maternal childbirth experience and empowerment levels. Moreover, there was a notable increase in delivery support and control, as well as maternal coping behavior. These findings contributed valuable insights to the existing literature on the positive effects of empowerment during childbirth. Implementing such educational interventions by midwives can be a promising approach to enhance the overall childbirth experience and empower women with fetal occiput posterior and occiput transverse malpositions. Further research in this area will continue to deepen our understanding and provide evidence for the beneficial impact of empowerment-focused interventions in maternal care.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Abbreviations
- CEQ
Childbirth Experience Questionnaire
- SD
Standard deviation
Author contributions
Xiuhong Wang: Conceptualization; Data curation; Roles/Writing - original draft; Project administrationXueyan Wang: Formal analysis; Roles/Writing - original draftXiaofeng Wan: InvestigationXueheng Weng: SupervisionCailing Lv: InvestigationJinguo Zhai: Methodology; Writing- review & editingAll of the authors have read and approved the manuscript.
Funding
This study received funding from Natural Science Foundation of Guangdong Province, Guangdong (2025).
Data availability
The datasets generated and analyzed during the present study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study protocol was approved by the hospital ethics committee (approval number:2020140A01) and registered at the Chinese Clinical Trial Registry (registration number: ChiCTR2300070915). All study participants signed the informed consent prior to the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Xiuhong Wang and Xueyan Wang contributed equally to this work.
References
- 1.Liu XH, Qi HB. Dystocia[M]. Beijing: People’s Publishing House; 2015. pp. 123–9. [Google Scholar]
- 2.Pilliod RA, Caughey AB. Fetal malpresentation and malposition: diagnosis and management. Obstet Gynecol Clin North Am. 2017;44(4):631–43. [DOI] [PubMed] [Google Scholar]
- 3.Nahaee J, Abbas-Alizadeh F, Mirghafourvand M, Mohammad-Alizadeh-Charandabi S. Pre- and during- labour predictors of dystocia in active phase of labour: a case-control study. BMC Pregnancy Childbirth. 2020;20(1):425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang K, Dai L, Wu M, Zeng T, Yuan M, Chen Y. Women’s experience of psychological birth trauma in China: a qualitative study. BMC Pregnancy Childbirth. 2020;20(1):651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Myers ER, Sanders GD, Coeytaux RR. Labor Dystocia[M]. Rockville (MD): Agency for Healthcare Research and Quality (US). 2020.
- 6.Kissler K, Jones J, McFarland AK, Luchsinger J. A qualitative meta-synthesis of women’s experiences of labor dystocia. Women Birth. 2020;33(4):e332–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dahan O. Navigating intensive altered states of consciousness: how can the set and setting key parameters promote the science of human birth? Front Psychiatry. 2023;14:1072047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Olza I, Uvnas-Moberg K, Ekström-Bergström A, Leahy-Warren P, Karlsdottir SI, Nieuwenhuijze M, et al. Birth as a neuro-psycho-social event: an integrative model of maternal experiences and their relation to neurohormonal events during childbirth. PLoS ONE. 2020;15(7):e0230992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhuk SI, Shchurevska OD. Maternal psychosocial stress and labor dystocia. Wiad Lek. 2020;73(7):1334–8. [PubMed] [Google Scholar]
- 10.Dahan O. The riddle of the extreme ends of the birth experience: birthing consciousness and its fragility. Curr Psychol. 2023;42(1):262–72. [Google Scholar]
- 11.Hosseini Tabaghdehi M, Kolahdozan S, Keramat A, Shahhossein Z, Moosazadeh M, Motaghi Z. Prevalence and factors affecting the negative childbirth experiences: a systematic review. J Matern Fetal Neonatal Med. 2020;33(22):3849–56. [DOI] [PubMed] [Google Scholar]
- 12.Johansson C, Finnbogadóttir H. First-time mothers’ satisfaction with their birth experience - a cross-sectional study. Midwifery. 2019;79:102540. [DOI] [PubMed] [Google Scholar]
- 13.Adler K, Rahkonen L, Kruit H. Maternal childbirth experience in induced and spontaneous labour measured in a visual analog scale and the factors influencing it; a two-year cohort study. BMC Pregnancy Childbirth. 2020;20(1):415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hassanzadeh R, Abbas-Alizadeh F, Meedya S, Mohammad-Alizadeh-Charandabi S, Mirghafourvand M. Perceptions of primiparous women about the effect of childbirth preparation classes on their childbirth experience: a qualitative study. Midwifery. 2021;103:103154. [DOI] [PubMed] [Google Scholar]
- 15.Downe S, Finlayson K, Oladapo OT, Bonet M, Gülmezoglu AM. What matters to women during childbirth: a systematic qualitative review. PLoS ONE. 2018;13(4):e0194906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Funnell MM, Anderson RM, Arnold MS, Barr PA, Donnelly M, Johnson PD, et al. Empowerment: an idea whose time has come in diabetes education. Diabetes Educ. 1991;17(1):37–41. [DOI] [PubMed] [Google Scholar]
- 17.Wigert H, Nilsson C, Dencker A, Begley C, Jangsten E, Sparud-Lundin C, et al. Women’s experiences of fear of childbirth: a metasynthesis of qualitative studies. Int J Qual Stud Health Well-being. 2020;15(1):1704484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dewi H. Empowerment of pregnancy care for pregnant women_ a concept analysis. Idea Nurs J. 2019;4(2):2087–879. [Google Scholar]
- 19.Castro EM, Van Regenmortel T, Vanhaecht K, Sermeus W, Van Hecke A. Patient empowerment, patient participation and patient-centeredness in hospital care: a concept analysis based on a literature review. Patient Educ Couns. 2016;99(12):1923–39. [DOI] [PubMed] [Google Scholar]
- 20.Lagendijk J, Been JV, Ernst-Smelt HE, Bonsel GJ, Bertens LCM, Steegers EAP. Client-tailored maternity care to increase maternal empowerment: cluster randomized controlled trial protocol; the healthy pregnancy 4 All-2 program. BMC Pregnancy Childbirth. 2019;19(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sjödin M, Rådestad I, Zwedberg S. A qualitative study showing women’s participation and empowerment in instrumental vaginal births. Women Birth. 2018;31(3):e185–9. [DOI] [PubMed] [Google Scholar]
- 22.Shoghi M, Shahbazi B, Seyedfatemi N. The Effect of the family-centered empowerment model (FCEM) on the Care Burden of the parents of children diagnosed with Cancer. Asian Pac J Cancer Prev. 2019;20(6):1757–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hadisuyatmana S, Has EMM, Sebayang SK, Efendi F, Astutik E, Kuswanto H, et al. Women’s empowerment and determinants of early initiation of breastfeeding: a scoping review. J Pediatr Nurs. 2021;56:e77–92. [DOI] [PubMed] [Google Scholar]
- 24.Aliabadi S, Shayan A, Refaei M, Tapak L, Moradveisi L. The effect of individual counseling based on the GATHER principles on perceived stress and empowerment of the mothers with high-risk pregnancies: an experimental study. BMC Psychiatry. 2022;22(1):396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Vries B, Phipps H, Kuah S, Pardey J, Ludlow J, Bisits A, et al. Transverse occiput position: using manual rotation to aid normal birth and improve delivery OUTcomes (TURN-OUT): a study protocol for a randomised controlled trial. Trials. 2015;16:362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kissler K, Hurt KJ. The pathophysiology of Labor Dystocia: theme with variations. Reprod Sci. 2023;30(3):729–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Funnell MM, Tang TS, Anderson RM. From dsme to dsms: developing empowerment-based diabetes self-management support. Diabetes Spectr. 2007;20(4):221–6. [Google Scholar]
- 28.Kuo CC, Wang RH. Appraisal of the application of empowerment elements and strategies: the example of chronic metabolic diseases. Hu Li Za Zhi. 2013;60(1):78–86. [DOI] [PubMed] [Google Scholar]
- 29.Dencker A, Taft C, Bergqvist L, Lilja H, Berg M. Childbirth experience questionnaire (CEQ): development and evaluation of a multidimensional instrument. BMC Pregnancy Childbirth. 2010;10:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jerofke T, Weiss M. Development and psychometric analysis of the patient perceptions of patient-empowering nurse Behaviours Scale (PPPNBS). J Adv Nurs. 2016;72(11):2923–36. [DOI] [PubMed] [Google Scholar]
- 31.Ford E, Ayers S, Wright DB. Measurement of maternal perceptions of support and control in birth (SCIB). J Womens Health (Larchmt). 2009;18(2):245–52. [DOI] [PubMed] [Google Scholar]
- 32.Ip WY, Tang CS, Goggins WB. An educational intervention to improve women’s ability to cope with childbirth. J Clin Nurs. 2009;18(15):2125–35. [DOI] [PubMed] [Google Scholar]
- 33.Lerman CE, Brody DS, Caputo GC, Smith DG, Lazaro CG, Wolfson HG. Patients’ perceived involvement in Care Scale: relationship to attitudes about illness and medical care. J Gen Intern Med. 1990;5(1):29–33. [DOI] [PubMed] [Google Scholar]
- 34.Lewin D, Piper S. Patient empowerment within a coronary care unit: insights for health professionals drawn from a patient satisfaction survey. Intensive Crit Care Nurs. 2007;23(2):81–90. [DOI] [PubMed] [Google Scholar]
- 35.Yeh MY, Lin SH, Tung TH. Psychometric evaluation of the Chinese version of the patient perceptions of empowerment scale (PPES). Biomed Res Int. 2014;2014:867451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ghanbari-Homayi S, Fardiazar Z, Meedya S, Mohammad-Alizadeh-Charandabi S, Asghari-Jafarabadi M, Mohammadi E, et al. Predictors of traumatic birth experience among a group of Iranian primipara women: a cross sectional study. BMC Pregnancy Childbirth. 2019;19(1):182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ma FF. [Effect of empowerment education on exclusive breastfeeding in women having a second child at advanced age]. Shandong: Qingdao University; 2021. [Google Scholar]
- 38.WHO recommendations. Intrapartum care for a positive childbirth experience[M]. Geneva: World Health Organization; 2018. [PubMed] [Google Scholar]
- 39.Smith V, Daly D, Lundgren I, Eri T, Begley C, Gross MM, et al. Protocol for the development of a salutogenic intrapartum core outcome set (SIPCOS). BMC Med Res Methodol. 2017;17(1):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McKelvin G, Thomson G, Downe S. The childbirth experience: a systematic review of predictors and outcomes. Women Birth. 2021;34(5):407–16. [DOI] [PubMed] [Google Scholar]
- 41.Taheri M, Takian A, Taghizadeh Z, Jafari N, Sarafraz N. Creating a positive perception of childbirth experience: systematic review and meta-analysis of prenatal and intrapartum interventions. Reprod Health. 2018;15(1):73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Viirman F, Hess Engström A, Sjömark J, Hesselman S, Sundström Poromaa I, Ljungman L, et al. Negative childbirth experience in relation to mode of birth and events during labour: a mixed methods study. Eur J Obstet Gynecol Reprod Biol. 2023;282:146–54. [DOI] [PubMed] [Google Scholar]
- 43.Cheng WJ, Hung KC, Ho CH, Yu CH, Chen YC, Wu MP, et al. Satisfaction in parturients receiving epidural analgesia after prenatal shared decision-making intervention: a prospective, before-and-after cohort study. BMC Pregnancy Childbirth. 2020;20(1):413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hinic K. Predictors of Breastfeeding confidence in the early Postpartum Period. J Obstet Gynecol Neonatal Nurs. 2016;45(5):649–60. [DOI] [PubMed] [Google Scholar]
- 45.Liang HM, Gau ML, Chen CP. [Effectiveness of a Labor-Admission Education Program on anxiety, uncertainty, Locus of Labor Control, and Labor Outcomes in pregnant women]. Hu Li Za Zhi. 2019;66(2):36–47. [DOI] [PubMed] [Google Scholar]
- 46.Kowalska J, Dulnik M, Guzek Z, Strojek K. The emotional state and social support of pregnant women attending childbirth classes in the context of physical activity. Sci Rep. 2022;12(1):19295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Finlayson K, Crossland N, Bonet M, Downe S. What matters to women in the postnatal period: a meta-synthesis of qualitative studies. PLoS ONE. 2020;15(4):e0231415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ahmadpour P, Moosavi S, Mohammad-Alizadeh-Charandabi S, Jahanfar S, Mirghafourvand M. Effect of implementing a birth plan on maternal and neonatal outcomes: a randomized controlled trial. BMC Pregnancy Childbirth. 2022;22(1):862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yadav AK, Sahni B, Jena PK. Education, employment, economic status and empowerment: implications for maternal health care services utilization in India. J PUBLIC AFFAIRS. 2021;21(3).
- 50.Li Z, Chen Q, Yan J, Liang W, Wong WCW. Effectiveness of motivational interviewing on improving care for patients with type 2 diabetes in China: a randomized controlled trial. BMC Health Serv Res. 2020;20(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tang TS, Gillard ML, Funnell MM, Nwankwo R, Parker E, Spurlock D, et al. Developing a new generation of ongoing: diabetes self-management support interventions: a preliminary report. Diabetes Educ. 2005;31(1):91–7. [DOI] [PubMed] [Google Scholar]
- 52.Guan H. Empowerment education and its application in health education.Journal of Nursing Science.
- 53.Khatiwada J, Muzembo BA, Wada K, Ikeda S. Dimensions of women’s empowerment on access to skilled delivery services in Nepal. BMC Pregnancy Childbirth. 2020;20(1):622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bliznashka L, Udo IE, Sudfeld CR, Fawzi WW, Yousafzai AK. Associations between women’s empowerment and child development, growth, and nurturing care practices in sub-saharan Africa: a cross-sectional analysis of demographic and health survey data. PLoS Med. 2021;18(9):e1003781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shibre G, Zegeye B, Yeboah H, Bisjawit G, Ameyaw EK, Yaya S. Women empowerment and uptake of antenatal care services: a meta-analysis of demographic and health surveys from 33 sub-saharan African countries. Arch Public Health. 2021;79(1):87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and analyzed during the present study are available from the corresponding author on reasonable request.