Abstract
Background
Psychological capital (PsyCap) is a positive internal resource for individuals, playing a crucial role in mental health. Evaluating nurses’ psychological capital is important for understanding their mental well-being, as they face unique occupational stressors. However, existing PsyCap questionnaires are developed for various other professions such as enterprise employees, teachers, patients, teenagers, and civil servants, making them less suitable for the nursing profession. The main aim of this study is to develop and validate a Psychological Capital Questionnaire specifically tailored to the nursing occupation in Chinese clinical settings.
Methods
This is a multi-stage, cross-sectional study conducted between March 2022 and May 2023. Preliminary items of the scale were generated through a literature review, theoretical research, and the Delphi method. The final questionnaire was validated through two rounds of data collection. In the first stage, 236 nurses were selected using purposive sampling for item analysis, exploratory factor analysis (EFA)and reliability testing. In the second stage, data were collected from 494 nurses using convenience sampling to conduct confirmatory factor analysis (CFA).
Results
The final questionnaire contains 30 items, with six factors extracted by EFA, accounting for 77.59% of the total variance. The confirmatory factor analysis showed good model fit, with the following indices: χ²/df = 4.052, GFI = 0.836, CFI = 0.938, TLI = 0.926, NFI = 0.919, RMSEA = 0.079, RMR = 0.030. The reliability measures were high, with a Cronbach’s α of 0.976, split-half coefficient of 0.976, and test-retest reliability of 0.941 and 0.963.
Conclusions
The Psychological Capital Questionnaire for Nurses exhibits strong psychometric properties, making it a valuable tool for assessing the psychological capital of nurses in Chinese clinical settings.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12912-024-02633-1.
Keywords: Instrument development, Psychological capital, Nurses, Psychometrics
Introduction
Psychological capital, as a novel concept in psychology, emphasizes the importance of a positive mindset and emotions [1]. It refers to an individual’s positive psychological state that consisting of the four positive psychological capacities of hope, optimism, resilience, and self-efficacy [2]. As a psychological resource, it profoundly impacts individuals’ lives and work. The exploration of psychological capital has become a topic of great interest to administrators in practice, especially healthcare discipline [3]. The growing empirical evidence has confirmed that psychological capital of nurses not only effects their physical and mental health but is also intimately associated with the organizational performance and patient outcomes [4–6]. In addition, the low psychological capital among nurses is related to substantial negative career outcomes, like job burnout, turnover intention and compassion fatigue, and then effect the safety and quality of nursing [7, 8]. Thus, understanding and evaluation of the nurses’ psychological capital are important to identify their positive psychological traits, improve mental health, adapt to the professional development, and ensure the provision of optimum care. However, lack of the standardized tests has always been an issue in evaluating the psychological capital among nursing staff.
The development of psychological capital measurement tools is of great significance to understand its structure. Up to now, virtually all research on psychological capital has made use of a self-report measure of psychological capital, the Psychological Capital Questionnaire (PCQ-24), which is developed by Luthans [2]. The PCQ-24 items describe the broad problem or situation of positive psychology that individual may experience at work and in life, and a range of adaptations have been conducted for other specific contexts, occupational groups, languages and cultures [9]. The PCQ-24 consists of 24 general items of which respondents have to rate based on they actually felt. The total score was computed by aggregating the 24 items, and a weighted average score was used to evaluate psychological capital [10]. While the PCQ-24 have proven to be very useful and is widely recognized as a measure of psychological capital, its original purpose was to measure the psychological capital of employees in the western organizational context.
Nurses, as an important force of the health care system, play an irreplaceable role in improving the quality of life of patients [11]. They are expected to have higher professional skills and psychological enduring capacity than employees of the enterprises, educators, administrators and other occupations because of the different working environments and the context of the services [7, 12]. In daily work, the main responsibility of nurses is to cooperate with other healthcare workers to guarantee the safety and quality of therapeutic process and care. Moreover, nurses must maintain a friendly attitude, suppress their true mental emotions and to make patients feel they are being properly and safely cared. The psychological capital of nurses includes not only general psychological resources (hope, self-efficacy, resilience, optimism and so on) but also communication, teamwork and other mental abilities (emotional intelligence, compassion, responsibility etc.) [13, 14]. In addition, the psychological resources associated with handling work-related stress and negative emotion, including subjective well-being, courage, gratitude, forgiveness, mindfulness, are also very important for nurses [15]. Based on these factors, existing measurement tools cannot cover the assessment of nurses’ psychological capital.
To our knowledge, only one published tool to quantitatively measure nurses’ psychological capital in the hospital settings, the Nurse Psychological Capital Scale (NPCS) [16]. This scale is developed in the context of Chinese culture and includes 43 items and 3 dimensions: work task-oriented psychological capital, interpersonal relationship-oriented psychological capital and learning development-oriented psychological capital. The psychometric properties of the NPCS are analyzed following the return of 577 of 619 nurses approached, a 93.2% response rate. Three factors explained 68.71% of the variance and the alpha coefficient for the full 43 items was 0.975. Although this scale is developed in nursing practice and has good reliability and validity, it has too many entries; this may cause respondents to feel tired and lose patience, thus affecting the quality of the survey results. In addition, the demanding nature of the nursing profession, nurses face several challenges, including long working hours, high patient loads, emotional labor, and burnout, which can all negatively impact their psychological capital. These challenges make it crucial to have a more concise, yet equally effective tool for assessing nurses’ PsyCap. Thus, this study seeks to further explore the structure of nurses’ psychological capital based on the PCQ-24, develop a more efficient and psychometrically sound instrument, and look forward to generalizing the findings globally. The newly developed questionnaire should provide reliable data for assessing nurses’ PsyCap in Chinese clinical settings and help in designing strategies to enhance psychological well-being and resilience among nurses.
Methods
Research design
This study is a multi-stage, cross-sectional questionnaire design, guided by the STROBE checklist for reporting cross-sectional studies.
Phase 1: Theoretical basis and item development
The positive organizational behavior (POB) guided the choice of topics addressed in the instrument. POB, proposed by Luthans in 2002, has been defined as “the study and application of positively oriented human resource strengths and psychological capacities that can be measured, developed, and effectively managed for performance improvement” [17]. To distinguish from other positive approaches reported in previous literature, the following criteria are set for including constructs in this definition of POB: (a) positive orientation; (b) exploitable; (c) measurable; (d) can be effectively managed; (e) have a positive effect on work-related performance and satisfaction [13]. Based on these criteria, four psychological resources have been determined as the positive psychological capital constructs, including hope, self-efficacy, resilience and optimism [2]. Recently, other related psychological resources such as well-being, courage, gratitude, forgiveness, mindfulness, emotional intelligence, compassion have also been found to meet these criteria to varying degrees [13, 18]. Therefore, this study further explored the unique components of nurses’ psychological capital and developed the Psychological Capital Questionnaire for Nurses (PCQN) based on the standard of POB.
We reviewed a variety of existing measures and literature to identify the feature words and initial items related to psychological capital. 10 features related to nurses’ psychological capital were obtained, including respect, cooperation, responsibility, hope, confidence, love, good at communication, emotional stability, resilience and compassion. These feature words were screened and combined, and six dimensions of confidence, hope, respect, emotional stability, responsibility and resilience were preliminarily determined. Subsequently, the items from previous instruments of psychological capital were summarized to assure that all important positive psychological resources were contained. Based on this, we generated 18 Hope, 12 Confidence, 15 Resilience, 14 Respect, 20 Responsibility and 18 Emotional Stability items for consideration. After discussions and revisions by the research group, an initial PCQN with 6 dimensions and 38 items was developed. This 38-item measure was considered ready for content validity testing.
Phase 2: Preliminarily evaluating the items
From March to July 2022, sixteen experts were invited to verify the content validity of the initial items in the PCQN. The Delphi method was chosen for this phase because it is a structured, iterative process that gathers feedback from a panel of experts through multiple rounds of consultation. This method helps to achieve consensus on complex issues by allowing experts to anonymously provide their input, ensuring that suggestions and opinions are considered without the influence of group dynamics. It is particularly effective for developing new tools or frameworks where expert judgment is critical. The criteria for choosing experts are as follows: (a) master degree or above; (b) associate professor or above professional qualifications; (c) with more than 10 years of experience in the nursing administration practice, nursing education, psychology and management; and (d) be familiar with the development process of the questionnaire. All experts agreed and participated voluntarily. The final expert group included 3 nursing managers, 2 experienced senior nurses, 5 professors in psychology, 3 professors in organizational behavior and 3 professors of management. A five- point rating questionnaire was used to rate the clarity and relevance of each item (1 = ‘not important’ to 5 = ‘very important’). They are also required to suggested revisions and whether any important content needs to be added. Two rounds of Delphi expert correspondence were conducted by E-mail before consensus was achieved. There were 100% (16/16) and 62.5% (10/16) experts to came up with constructive suggestions in Round One and Round Two, respectively. The rejection criteria of items were: relevancy < 3, standard deviation > 1 or coefficient of variation > 25% [19]. Other controversial items were revised through discussion in the study group.
According to the suggestions of the first round of experts, the dimensions of “Respect” and “Emotional Stability” were merged into the dimension of “Emotional Intelligence”, and the dimension of “Optimism” was added. In addition, we deleted 11items for their low relevancy (I think myself quite successful in my work at the moment. / When communicating with colleagues and leaders, I have the confidence to state my work clearly. / I can think of many ways to solve difficult problems at work, etc.), added 12 items, and the language of 14 items was corrected. In the second round of expert consultation, all experts agree on the dimensions of the questionnaire, but only put forward modification suggestions for the items, such as changing “I work hard to make my work goal a reality” into “I work hard to achieve the work goal”, etc. Furthermore, five items were deleted based on the expert suggestions (If I think something can go wrong, even if I’m careful, it will. / When I am ignored by team members, subjected to workplace violence or disrespectful behavior, I can cope with it calmly. / I would like to use some of my personal time to get my work done. / My words and actions are related to the overall image of the department. / When I am emotionally unstable, I will seek the support of others to adjust my emotions.). In the dimension of Responsibility, one item “I will take the initiative to understand the patient’s illness and psychological condition” was added, while in the Emotional Intelligence dimension, an item “I can treat all nursing objects equally” was added. After 2 rounds of Delphi, a draft questionnaire was formed, which included 6 dimensions and 36 items.
The draft questionnaire formed by Delphi method are applied to 50 registered nurses from a tertiary hospital for a pilot survey in Chengdu, Sichuan Province, China, to test comprehensibility, readability and response errors. The participants in the pilot study are requested first to finish the draft questionnaire, then given suggestions from the format, content and language expression of the questionnaire. In the process, we found that the language expression of five items was inaccurate or inappropriate based on the feedback of the participants. These items are amended through research group consultation, and the initial questionnaire with 36 items and 6 dimensions is finalized.
Phase 3: The psychometric testing
The item analysis with correlation coefficient method, Cronbach’s α coefficient and critical ratio method (CR value) were conducted to screen items. The criteria are as follows [20]: (a) items with correlation coefficient < 0.400 with the total score of the scale are excluded; (b) if the total Cronbach’s α coefficient increases significantly after removing this item, then this item will be deleted; (c) the total score of the questionnaire is arranged in ascending order, and 27% of the samples before and after were selected as high group and low group. Independent-sample T test is used to test the two groups, and items with no significant difference in scores between the two groups were deleted.
The exploratory factor analysis (EFA) and confirmatory factor analysis (CFA) were conducted based on different sample groups to check construct validity of the questionnaire. Before conducting EFA, the suitability of the data was assessed through Kaiser Meyer Olkin (KMO) coefficient and Bartlett’s sphericity test. The EFA was performed via principal component analysis to identity the factor structure questionnaire. The criterion of factor extraction are as follows [21]: (a) the contribution rate of cumulative variance > 50%; (b) eigenvalue > 1, factor load ≥ 0.400; (c) delete the double load entry, that is, the same entry load value on two or more common factors at the same time > 0.400, and the difference between factor loadings < 0.1. The CFA was conducted to evaluated the stability of factor model. The evaluative criteria of model fitting indexes are as follows [15]: (a) χ2/df < 5; (b) Goodness-of-fit index (GFI), Comparative fit index (CFI), Normed fit index (NFI), Tueker-Lewis index (TLI), and Incremental fit index (IFI), all > 0.8; (c) Root-mean-square error of approximation (RMSEA) < 0.08; (d) Root mean square residual (RMR) < 0.05.
Cronbach’s alpha coefficient was used to test the reliability of the questionnaire and the Cronbach’s alpha coefficient greater than 0.7 indicates that the questionnaire has a good reliability [22]. Furthermore, the Spearman–Brown split- half coefficient was carried out to test the stability of items. 30 respondents were selected and marked to survey again later half a month for check questionnaire’s temporal stability.
Population and sample
From November 2022 to May 2023, participants were recruited by convenience sampling from five tertiary hospital in Chengdu, Sichuan Province, China. Registered nurses who have been engaged in clinical nursing in existing department for at least 1 year are included and all respondents agreed and participated voluntarily. Nurses who are not on duty during the survey, assistant nurses and nurses who suffered serious illness or life events in the last 6 months are excluded.
Data collection
Two rounds of data collection were performed from November 2022 to May 2023. The first round of questionnaire was conducted between September and December 2022, to evaluate the initial psychometric properties and refine the initial items. The second round of survey was performed Between January and May 2023, to verify the stability of the internal structure of PCQN. According to the questionnaire design principle, the sample size should be 5 ~ 10 times of the questionnaire items, and a minimum sample size of 200 is recommended for CFA [23]. Therefore, at least 200 participants should be required for each round of investigation. We collected date by an online questionnaire platform with a self-reported electronic questionnaire. Before an official investigation, the electronic questionnaire was sent to nursing managers of each hospital by E- mail for permission and assistance. With permission, the members of the research group fully informed participants that this survey was anonymous and voluntary, as well as the investigation content and purpose. In addition, there are also instructions on the first page of the questionnaire. Nurses who are willing to participate in the survey can scan the QR code or click the WeChat link to fill in the questionnaire. Questionnaire completion and return were deemed as informed consent. In the first round of surveys, a total of 255 questionnaires were distributed, and 236 valid questionnaires were returned, with an effective response rate of 92.5%. In the second round of survey, a total of 517 questionnaires were sent out, and 494 questionnaires were effectively recovered, with an effective response rate of 95.5%.
Data analysis
All data are double-entered by Excel software, the SPSS24.0 and AMOS26.0 software are used to conducted data analysis. The reliability of experts is judged by the coefficient of expert familiarity, Kendall coordination and authority coefficient. The participants’ characteristics and questionnaire score are described by mean, standard deviation, percentage or rate. Item analysis, reliability test and EFA are carried out on the questionnaire with the first round of survey data. CFA and reliability test are conducted through the data from the second round of investigation, and P < 0.05 is considered to be statistically significant.
Results
General characteristics of participants
In the first round of the survey, 236 participants were involved, with a majority being female (90.7%). Their ages ranged from 21 to 59 years, with a mean age of 28.82 ± 5.80 years. In the second round, 494 participants took part, including 33 males (6.7%) and 461 females (93.3%), with a mean age of 31.47 ± 6.89 years. Detailed demographic information is provided in Table 1.
Table 1.
General demographic data
| Variables | Categories | The first round of investigation (n = 236) |
The second round of investigation (n = 494) |
||||
|---|---|---|---|---|---|---|---|
| N | % | M ± SD | N | % | M ± SD | ||
| Gender | Male | 22 | 9.3 | 33 | 6.7 | ||
| Female | 214 | 90.7 | 461 | 93.3 | |||
| Age (year) | 20 ~ 30 | 167 | 70.8 | 28.82 ± 5.80 | 279 | 56.5 | 31.47 ± 6.89 |
| 31 ~ 40 | 60 | 25.4 | 173 | 35.0 | |||
| 41 ~ 50 | 5 | 2.1 | 29 | 5.9 | |||
| > 50 | 4 | 1.7 | 13 | 2.6 | |||
| Marital status | Unmarried | 119 | 50.4 | 168 | 34.0 | ||
| Married | 113 | 47.9 | 314 | 63.6 | |||
| Others | 4 | 1.7 | 12 | 2.4 | |||
| Education level | 3-year college | 32 | 13.6 | 51 | 10.3 | ||
| 4-year university | 190 | 80.5 | 418 | 84.6 | |||
| Master’s or higher | 14 | 5.9 | 25 | 5.1 | |||
| Work experience (years) | 1 ~ 5 | 139 | 58.9 | 6.56 ± 6.14 | 178 | 36.0 | 9.89 ± 7.71 |
| 6 ~ 10 | 53 | 22.5 | 84 | 17.0 | |||
| > 10 | 44 | 18.6 | 232 | 47.0 | |||
| Title | Nurse | 199 | 84.3 | 382 | 77.3 | ||
| Nurse in charge | 26 | 11 | 83 | 16.8 | |||
| Deputy chief nurse or above | 11 | 4.7 | 29 | 5.9 | |||
| Salary (RMB) | < 4000 | 35 | 14.8 | 44 | 8.9 | ||
| 4001 ~ 6000 | 58 | 24.6 | 64 | 13.0 | |||
| 6001 ~ 8000 | 71 | 30.1 | 123 | 24.9 | |||
| 8001 ~ 10,000 | 47 | 19.9 | 128 | 25.9 | |||
| > 10,000 | 25 | 10.6 | 135 | 27.3 | |||
| Department |
Internal medicine ward |
81 | 34.3 | 160 | 32.4 | ||
| Surgical ward | 41 | 17.4 | 62 | 12.6 | |||
| Maternity ward | 17 | 7.2 | 24 | 4.9 | |||
| Pediatric ward | 10 | 4.2 | 16 | 3.2 | |||
| Emergency room | 12 | 5.1 | 12 | 2.4 | |||
| ICU | 17 | 7.2 | 41 | 8.3 | |||
| Operating room | 15 | 6.4 | 17 | 3.4 | |||
| Oncology department | 2 | 0.8 | 3 | 0.6 | |||
| psychiatry department | 1 | 0.4 | 1 | 0.2 | |||
|
Outpatient department |
11 | 4.7 | 122 | 24.7 | |||
| Others | 29 | 12.3 | 36 | 7.3 | |||
Content validity
Six experts in Delphi are invited to evaluate the content validity of the questionnaire. Experts rated each item on its relevance to the dimension to which it belongs, based on their own experience. The item-level content validity index (I-CVI) and the average scale level content validity index (S-CVI) in the questionnaire were calculated according to the scores. The eligibility criteria are I-CVI > 0.780 and S-CVI ≥ 0.800. In this study, the I- CVI of scale ranged from 0.833 ~ 1.000, and the S- CVI is 0.956.
Item analysis
Correlation analysis shows that the correlation coefficient between the items ranged from 0.647 to 0.884 and the correlation coefficient between the items and the total score of the questionnaire is 0.852 ~ 0.948 (all P < 0.05). There was no significant increase in Cronbach’s α confidence after any of the items were dropped; There are statistically significant differences among the items in the high and low groups (all P < 0.05), and the T-values ranged from 10.231 to 19.918 (all T-values > 3.000). Thus, no items can be deleted in the item analysis.
Exploratory factor analysis
The KMO value is 0.957, Bartlett sphericity test χ2 value is 6797.802 (P < 0.001), indicating that the data are suitable for factor analysis. A total of 6 factors are extracted, and the load value of each item on the corresponding factor is greater than 0.400, and the cumulative variance contribution rate is 77.587%. According to the theoretical model and load value of the items, 6 items whose attribution is unclear (cross-load) are deleted (two items are removed each from the Optimism and Emotional Intelligence, and one item each from Hope and Resilience dimensions). After discussion by the panel meeting, some items are re-assigned and renamed. Finally, a formal questionnaire with 6 dimensions and 30 items are developed, including Hope (7 items), Cooperative Communication (6 items), Emotional Intelligence (5 items), Responsibility (4 items), Resilience (4 items) and Confidence (4 items), see Table 2 for more details.
Table 2.
Factor analysis of the psychological capital questionnaire for nurses (N = 236)
| Items | Factor loading | |||||
|---|---|---|---|---|---|---|
| F1 | F2 | F3 | F4 | F5 | F6 | |
| 1. In my current job, I feel like everything always goes my way | 0.766 | |||||
| 2. I always look at the positive side of my work | 0.709 | |||||
| 3. When I need help, the people around me always give me a helping hand | 0.642 | |||||
| 4. I think most of the patients are kind, understanding and willing to cooperate with the nurses | 0.646 | |||||
| 5. I work hard to achieve my work goals | 0.623 | |||||
| 6. I am always energetic to accomplish my work goals | 0.556 | |||||
| 7. Even if the problem is very difficult, I still try to solve it | 0.452 | |||||
| 8. I think unity is strong, and we can get twice the result with half the effort | 0.821 | |||||
| 9. I’m good at dealing with different patients | 0.799 | |||||
| 10. I have strong communication skills | 0.772 | |||||
| 11. If a colleague is in need, I will try my best to provide him or her with useful help | 0.765 | |||||
| 12. I think it is a very happy thing to cooperate with my colleagues to finish the work | 0.662 | |||||
| 13. I can keep a good relationship with my colleagues and leaders | 0.654 | |||||
| 14. I don’t usually bring negative emotions from my life to work | 0.785 | |||||
| 15. When a patient tells me something private, I listen with all my heart without showing rejection, exclusion or discrimination | 0.761 | |||||
| 16. When I face patients, I can feel their mental distress | 0.749 | |||||
| 17. I can deal with unpleasantness at work calmly | 0.692 | |||||
| 18. I am able to respond to what the patients are saying in time that make the patients feel understand | 0.687 | |||||
| 19. I can do serious and meticulous in the process of finishing the nursing work | 0.716 | |||||
| 20. I will seriously participate in the training activities of the hospital | 0.714 | |||||
| 21. In my spare time, I will take the initiative to learn the latest nursing knowledge and skills | 0.655 | |||||
| 22. I will take the initiative to understand the patient’ state of the illness and mental | 0.548 | |||||
| 23. I always do my best to solve nursing problems | 0.625 | |||||
| 24. I can recover quickly from setbacks and go on | 0.565 | |||||
| 25. I can usually handle stress at work | 0.561 | |||||
| 26. I can deal with all kinds of emergencies positively and safely | 0.511 | |||||
| 27. I think the work I do is meaningful to the development of the organization | 0.749 | |||||
| 28. I believe that I have the ability to analyze and solve difficult problems at work | 0.663 | |||||
| 29. I can handle work affairs with composure | 0.600 | |||||
| 30. I have full confidence for the development of nursing profession | 0.467 | |||||
F1: Hope; F2: Collaborative Communication; F3: Emotional Intelligence; F4: Responsibility; F5: Resilience; F6: Confidence
Confirmatory factor analysis
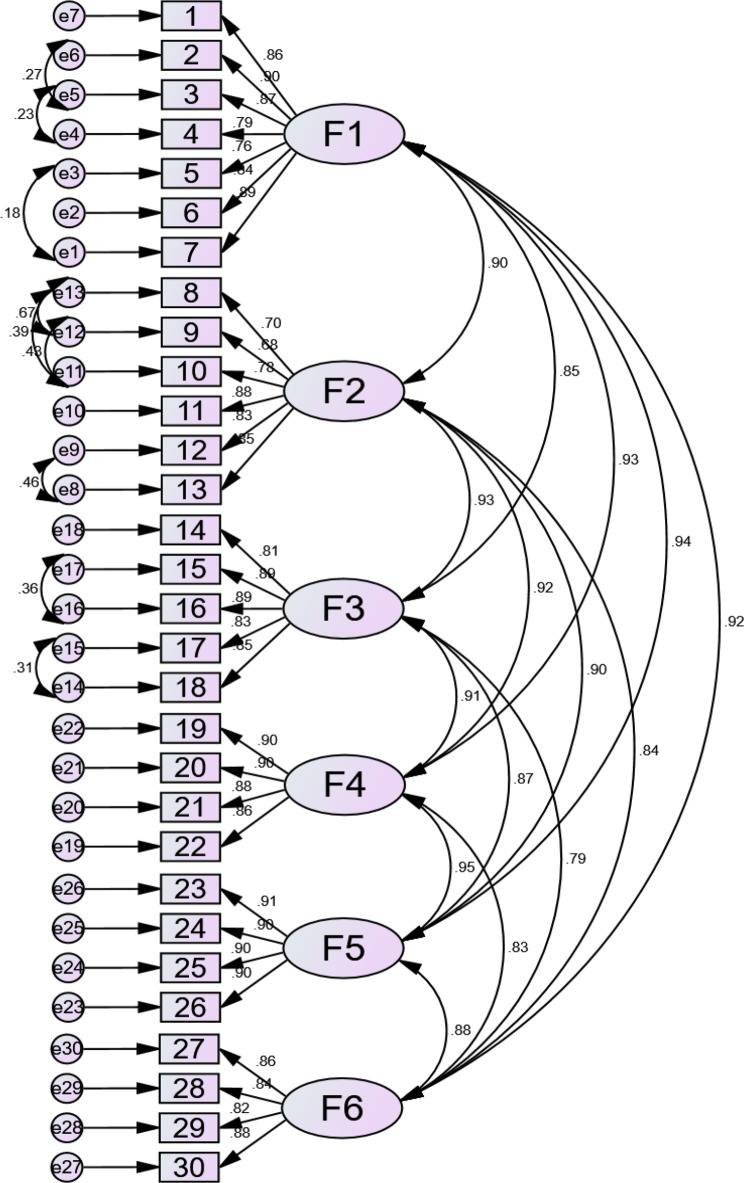
We conducted a CFA by using maximum likelihood methods to evaluate the fitness of the 30- item and six- factor structure found with EFA. In CFA, several important model fit indices reveal the model are reasonable, such as χ2/df = 4.052, GFI = 0.836, CFI = 0.938, TLI = 0.926, NFI = 0.919, RMSEA = 0.079, RMR = 0.030. On the basis of the modification indices, several paths of covariance between items and error were added to improve the model fitting. The CFA model is shown in Fig. 1.
Fig. 1.
Confirmatory factor analysis of the psychological capital questionnaire for nurses
Reliability analysis
In the first round of data, the total Cronbach’s α coefficient is 0.976, and the Cronbach’s α coefficient of the six dimensions is 0.864 ~ 0.821. In the second round of survey, the total Cronbach’s α coefficient is 0.983, and the Cronbach’s α coefficient of the six dimensions is 0.918 ~ 0.946. More details are presented in Table 3.
Table 3.
Reliability coefficient of the psychological capital questionnaire for nurses
| Dimension/ Questionnaire | The first round of investigation (n = 236) |
The second round of investigation (n = 494) |
||||
|---|---|---|---|---|---|---|
| Cronbach’s α | Split-half reliability | Test-retest reliability | Cronbach’s α | Split-half reliability | Test-retest reliability | |
| Hope | 0.921 | 0.845 | 0.877 | 0.946 | 0.894 | 0.939 |
| Confidence | 0.864 | 0.890 | 0.786 | 0.908 | 0.924 | 0.857 |
| Responsibility | 0.905 | 0.871 | 0.882 | 0.936 | 0.915 | 0.963 |
| Resilience | 0.913 | 0.909 | 0.831 | 0.945 | 0.944 | 0.971 |
| Collaborative Communication | 0.903 | 0.822 | 0.893 | 0.913 | 0.775 | 0.910 |
| Emotional Intelligence | 0.905 | 0.849 | 0.896 | 0.934 | 0.895 | 0.958 |
| Total Questionnaire | 0.976 | 0.941 | 0.963 | 0.983 | 0.959 | 0.985 |
Final instrument
The PCQN consists of 30 items and six dimensions: Hope (7 items), Cooperative Communication (6 items), Emotional Intelligence (5 items), Responsibility (4 items), Resilience (4 items) and Confidence (4 items). This questionnaire follows the scoring method of the PCQ-24. It is a 6- item Likert- type scale with responses from 1 = strongly disagree to 6 = strongly agree that evaluates the psychological capital of nurses. The total score is 30 ~ 180 points, the higher the score, the higher the psychological capital of nurses. The total score of the questionnaire is converted into the mean score as the criterion, the total mean score < 3, indicating low psychological capital of nurses; 3 ~ 4 indicates that the level of psychological capital is medium; > 4 points, indicating that the psychological capital of nurses is at a high level.
Discussion
Positive psychological capital has been a major focus for many decades. Better evaluation of psychological capital will contribute to better support for nurses and improve their mental health and professional happiness [24]. However, the psychological capital structure of different occupational groups presents different characteristics and the measurement tools of nurses’ psychological capital are relatively scarce. Thus, the purpose of this study is to develop the PCQN and test the psychometric properties, a new generic, theory-based measure of self-report designed for use to measure psychological capital of nurses. This questionnaire designed to measure psychological capital is anticipated to be valuable for nursing staff in Asia.
In this study, the draft of PCQN is developed through two rounds of Delphi and preliminary survey. The authority coefficients of the two rounds of expert are 0.847 and 0.875, respectively, and there are constructive suggestions from experts, which ensured the reliability and authority of this questionnaire. Furthermore, the content validity of questionnaire is evaluated with the I- CVI and S- CVI levels and both are above the acceptable lower limit [25]. These results revealed that the items represented the structure adequately.
Through exploratory factor analysis and confirmatory factor analysis, a six-factor PCQN including Hope, Cooperative Communication, Emotional Intelligence, Responsibility, Resilience and Confidence was formed. Factor 1 is named “Hope” because it includes items that reflect nurses’ positive attitude towards achieving career goals in a nursing context. In our study, hope is an ability to maintain positive expectations about the future, believing in one’s capacity to achieve goals and showing willingness to strive for them. We consider hope as a mental health promotion resource of nurses and is something positive and focuses on the development of nursing profession; it can relieve nurses’ burnout, fatigue and improve the quality of life. Factor 2, which included six items, is labelled “Cooperative Communication”, because it includes not only communication with patients, colleague, leaders but also teamwork ability. For nursing staff, cooperation communication is an important way to solve nurse-patient conflict and improve patient satisfaction [26, 27]. Factor 3 is named “Emotional Intelligence” because it includes items showing the nurse’s perception and understanding of the patient’s emotions. We consider emotional intelligence is a combination of both abilities and personality traits and it plays a key role in understanding the demands of patients and can effectively manage nurses’ emotional and behavioral intentions. Factor 4 is named “Responsibility”, and the responsibility refers to an attitude to himself, family, work and society. This factor includes nurses’ attitudes towards completing nursing skills training, performing nursing procedure and understanding the conditions of patients. Responsible nurses tend to recognize that the importance of their work in the organization and make it their goal to achieve the organization’s goals [28]. Factor 5, which includes 4 items, is labelled “Resilience” because it includes items that reflect an ability to bounce back or even overcome adversity. In this study, resilience is considered as a positive psychological resource that can help nurses recover quickly from adversity. Several studies suggest that resilience is a dynamic process that can help nurses adopt positive coping strategies to job burnout and emotional exhaustion [29, 30]. Finally, factor 6, which includes 4 items, is named “Confidence”, and this factor describes nurses’ confidence in the development of their nursing profession. It includes the nurse to self–affirmation and nursing career development expectations. In a word, these six factors form a synergistic resource, which is considered as crucial elements of nurses’ psychological capital.
In this study, the reliability is evaluated using Cronbach’s alpha coefficients, Spearman–Brown split- half coefficients and Test-retest reliability coefficients. The Cronbach’s alpha coefficients and Spearman–Brown split- half coefficients of the PCQN are above Minimum recommended value (> 0.7), indicating the internal consistency of this questionnaire is fine. Moreover, the Test-retest reliability results manifest that the questionnaire has good temporal stability. In conclusion, the PCQN has good reliability and validity, and can accurately and truly reflect the psychological capital of nurses.
The findings from this study align with prior research on psychological capital measurement tools, while introducing new dimensions specifically relevant to nursing. For instance, the total variance explained by the six-factor model in the PCQN (77.587%) exceeds that of the NPCS developed by Zhang et al. [16]. This higher variance suggests that the PCQN offers a more comprehensive representation of nurses’ psychological capital, covering additional dimensions such as Cooperative Communication and Responsibility, which are critical in nursing practice but not thoroughly covered in previous instruments. In addition, the six dimensions of the PCQN contrast with the four dimensions of the existing PCQ-24, while there is some conceptual overlap between the two instruments because of the commonalities of psychological capital in different populations. However, our study identified Emotional Intelligence, Responsibility, and Cooperative Communication as distinct factors relevant to the nursing context. These findings highlight the unique psychological demands of nursing, such as the need to communicate effectively with patients and colleagues and the responsibility associated with patient care, which are less emphasized in general psychological capital measures. Non-congruent findings arise in the dimension of optimism. While optimism is a core factor in most psychological capital measures, the emphasis in our study shifted towards Emotional Intelligence, which includes understanding and managing not only one’s own emotions but also those of patients. This shift could be explained by the emotionally charged environment nurses work in, which requires more nuanced emotional regulation skills than other profession. Emotional intelligence, therefore, becomes a critical psychological resource in nursing, addressing both interpersonal and intrapersonal challenges.
Limitations
This study has several limitations. Firstly, the sample was composed solely of nurses from China, which may limit the generalizability of the findings to nurses in other regions or cultural contexts. Additionally, the sample had a significant gender imbalance, with very few male participants, which may not fully represent the diversity of the nursing workforce. Another limitation lies in the subjective interpretation of the Exploratory Factor Analysis (EFA) results, as decisions regarding item retention and the labeling of factors were based on factor loadings, which can introduce bias. Consequently, the final version of the PCQN requires further validation. Moreover, the cross-sectional design of the study allowed for the examination of reliability and validity at a single point in time but did not enable assessment of the temporal stability of the PCQN or establish causal relationships. Longitudinal studies are needed to evaluate the stability and robustness of the questionnaire over time. Future research should also explore the applicability of the PCQN in different cultural contexts by including nurse samples from various countries. Additionally, investigating the relationships between the PCQN and other measures of psychological capital would provide further insights into its broader implications and validity.
Conclusion
The PCQN, developed with six dimensions and 30 items, demonstrates strong psychometric properties and offers a useful tool for assessing the psychological capital of nurses in the Chinese clinical setting. The inclusion of nursing-specific factors such as Cooperative Communication, Responsibility, and Emotional Intelligence makes the PCQN particularly relevant for nursing systems, as these elements are essential for effective patient care and nurse well-being. The higher explained variance and robust internal consistency indicate that the PCQN is better suited than generic psychological capital measures to capture the unique psychological resources required in the nursing profession.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Special thanks to the participants of this study for their time and contribution. We also appreciate the financial support from the Humanities and Social Sciences of Ministry of Education Planning Fund, Sichuan Research Center of Applied Psychology of Chengdu Medical College and Southwest Medical University: Key Research Bases for Humanities and Social Science of the Education Department in Sichuan Province—Sichuan Hospital Management and Development Research Center.
Author contributions
JLW: conceptualization, visualization, writing original draft, supervision, revising, editing and approving manuscript. ZQY: conceptualization, visualization, data analysis and curation, writing original draft, review and editing. MJ: design, data collection and analysis, writing original draft, review and editing. LZ: data analysis, visualization, writing original draft, review and editing. HH: data analysis, writing original draft. MT: data collection and analysis, writing original draft. QQR: data analysis, writing original draft. All authors are involved in drafting the manuscript or revising it critically for important intellectual content and agreed on the final version.
Funding
This work was supported by the Humanities and Social Science Research Planning Fund of the Ministry of Education of the People’s Republic of China [grant numbers: 22YJA630087], Sichuan Research Center of Applied Psychology of Chengdu Medical College [grant numbers: CSXL-24101] and Southwest Medical University: Key Research Bases for Humanities and Social Science of the Education Department in Sichuan Province—Sichuan Hospital Management and Development Research Center (Number: SCYG2024-47).
Data availability
Research data cannot be shared at this time due to privacy or ethical restrictions.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and was obtained and approved by Ethics Committee of Chengdu university of Traditional Chinese Medicine (Number: 2020-KL084; Date: Dec. 28, 2020). At the same time, all participants were enrolled in the survey based on informed consent and voluntariness. To ensure the privacy of the respondents, questionnaire was anonymous. In addition, this study adhered to national legal and institutional requirements.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Zhongqing Yuan Co-first author.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jialin Wang, Email: wangjialin@cdutcm.edu.cn.
Zhongqing Yuan, Email: 2859252454@qq.com.
References
- 1.Yuan Z, Zhang X, Wang F, Jin M, Teng M, He H, Wang J. Levels of psychological capital among nurses: a systematic review and meta-analysis. Int Nurs Rev. 2023;70(1):89–96. [DOI] [PubMed] [Google Scholar]
- 2.Luthans F, WK, CB. Positive psychological capital: beyond human and social capital. Bus Horiz. 2004;47(1):45–50. [Google Scholar]
- 3.Teng M, Wang J, Jin M, Yuan Z, He H, Wang S, Ren Q. Psychological capital among clinical nurses: a latent profile analysis. Int Nurs Rev 2023. [DOI] [PubMed]
- 4.Elliott R, Fry M. Psychological capital, well-being, and patient safety attitudes of nurses and midwives: a cross-sectional survey. Nurs Health Sci. 2021;23(1):237–44. [DOI] [PubMed] [Google Scholar]
- 5.Flinkman M, Coco K, Rudman A, Leino-Kilpi H. Registered nurses’ psychological capital: a scoping review. Int J Nurs Pract. 2023;29(5):e13183. [DOI] [PubMed] [Google Scholar]
- 6.Zeng L, Feng F, Jin M, Xie W, Li X, Li L, Peng Y, Wang J. Psychological capital and organizational citizenship behavior among nurses during the COVID-19 epidemic: mediation of organizational commitment. BMC Nurs. 2023;22(1):172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yao X, Lin Y, Zhang C, Wang X, Zhao F. Does Psychological Capital Mediate Occupational stress and coping among nurses in ICU. West J Nurs Res. 2022;44(7):675–83. [DOI] [PubMed] [Google Scholar]
- 8.Zhang X, Chen S, Zheng Z, Zhao M, Song L, Zhao Y, Wang Z. The relationship between psychological capital, burnout and perceived stress in junior nurses: a latent profile analysis. Front Public Health. 2024;12:1374941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McDaniels B, Lee CL, Bishop M. Evaluating the Psychometric properties of the Psychological Capital Questionnaire (PCQ) in patients with Parkinson’s Disease. J Parkinson’s Disease. 2022;12(1):221–8. [DOI] [PubMed] [Google Scholar]
- 10.Harms PD, Luthans F. Measuring implicit psychological constructs in organizational behavior: an example using psychological capital. J Organ Behav. 2012;33(4):589–94. [Google Scholar]
- 11.Leng M, Wei L, Shi X, et al. Mental distress and influencing factors in nurses caring for patients with COVID-19. Nurs Crit Care. 2021;26(2):94–101. [DOI] [PubMed] [Google Scholar]
- 12.Singh A. Psychological capital among nursing Faculty: implications for practice. Nurse Educ. 2023;48(6):336–41. [DOI] [PubMed] [Google Scholar]
- 13.Youssef-Morgan CM, Luthans F. Psychological capital and well-being. Stress Health. 2015;31(3):180–8. [DOI] [PubMed] [Google Scholar]
- 14.Kong LN, Liao HP, Liu DX, Chen SZ. Relationship of Organizational Support, Psychological Capital, and Engagement among clinical nursing teachers. Nurse Educ. 2023;48(4):E105–9. [DOI] [PubMed] [Google Scholar]
- 15.Jin M, Zhang Y, Wang F, et al. A cross sectional study of the impact of psychological capital on organisational citizenship behaviour among nurses: mediating effect of work engagement. J Nurs Manage. 2022;30(5):1263–72. [DOI] [PubMed] [Google Scholar]
- 16.Lu X, Wang L, Xu G, Teng H, Li J, Guo Y. Development and initial validation of the psychological capital scale for nurses in Chinese local context. BMC nurs. 2023;22(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luthans F. Positive organizational behavior: developing and managing psychological strengths. ACAD MANAGE PERSPECT. 2002;16(1):57–72. [Google Scholar]
- 18.Hu R, Li Y, Huang J, Zhang Y, Jiang R, Dunlop E. Psychological capital and breakthrough innovation: the role of tacit knowledge sharing and task interdependence. Front Psychol. 2023;14:1097936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baele CA, Fontaine JRJ. The Moral Distress-Appraisal Scale: Scale development and validation study. J Adv Nurs. 2021;77(10):4120–30. [DOI] [PubMed] [Google Scholar]
- 20.Celebi Cakiroglu O, Baykal U. Development and psychometric properties of the attitude scale towards female workers in the healthcare settings. J Adv Nurs. 2021;77(7):3238–53. [DOI] [PubMed] [Google Scholar]
- 21.Hara Y, Asakura K, Yamada M, Takada N, Sugiyama S. Development and psychometric evaluation of the nurses’ work values Scale. Nurs Open. 2023;10(10):6957–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mori Y, Sasaki M, Ogata Y, Togari T. Development and psychometric validation of an educational support assessment scale for novice home healthcare nurses. BMC Med Educ. 2023;23(1):326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bolarinwa OA. Sample size estimation for health and social science researchers: the principles and considerations for different study designs. Niger Postgrd Med J. 2020;27(2):67–75. [DOI] [PubMed] [Google Scholar]
- 24.Ren Z, Zhang X, Li X, He M, Shi H, Zhao H, Zha S, Qiao S, Li Y, Pu Y, et al. Relationships of organisational justice, psychological capital and professional identity with job burnout among Chinese nurses: a cross-sectional study. J Clin Nurs. 2021;30(19–20):2912–23. [DOI] [PubMed] [Google Scholar]
- 25.Luo Y. Development and validation of professional competency scale for military nurses: an instrument design study. BMC Nurs. 2022;21(1):90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Höglander J, Holmström IK, Lövenmark A, Van Dulmen S, Eide H, Sundler AJ. Registered nurse-patient communication research: an integrative review for future directions in nursing research. J Adv Nurs. 2023;79(2):539–62. [DOI] [PubMed] [Google Scholar]
- 27.Philip S, Woodward-Kron R, Manias E. Overseas qualified nurses’ communication with other nurses and health professionals: an observational study. J Clin Nurs. 2019;28(19–20):3505–21. [DOI] [PubMed] [Google Scholar]
- 28.Patrician PA, Bakerjian D, Billings R, Chenot T, Hooper V, Johnson CS, Sables-Baus S. Nurse well-being: a concept analysis. Nurs Outlook. 2022;70(4):639–50. [DOI] [PubMed] [Google Scholar]
- 29.Castillo-González A, Velando-Soriano A, De La Fuente-Solana EI, Martos-Cabrera BM, Membrive-Jiménez MJ, Lucía RB. Cañadas-De La Fuente GA. Relation and effect of resilience on burnout in nurses: a literature review and meta-analysis. Int Nurs Rev. 2024;71(1):160–7. [DOI] [PubMed] [Google Scholar]
- 30.Nassar YM, Eshah N, Al-Maqableh HO, Nashwan AJ, Rayan A, Alhawajreh MJ. Workplace resilience and compassionate care among Jordanian private sector nurses. BMC Nurs. 2024;23(1):634. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Research data cannot be shared at this time due to privacy or ethical restrictions.