Abstract
Objective
This study aimed to examine the associations between knowledge, social support, and physical activity and explore the mediating role of physical activity self-efficacy in pregnant women with a high risk for gestational diabetes mellitus (GDM).
Methods
A cross-sectional study was conducted in Guangzhou, China, from July 2022 to May 2023. Five hundred thirty-seven pregnant women with a high risk for GDM completed the Pregnancy Physical Activity Questionnaire, Pregnancy Physical Activity Self-Efficacy Scale, Pregnancy Physical Activity Knowledge Scale, Physical Activity Social Support Scale, and a socio-demographic data sheet. The mediation effect was tested using structural equation modeling (SEM) and the bootstrap method.
Results
42.5% of pregnant women did not meet the current physical activity guidelines. Physical activity self-efficacy (β, 0.16; P<0.001), knowledge (β, 0.15; P = 0.001), social support (β, 0.10; P = 0.019), education, and type of conception were predictors of physical activity. The SEM results found that physical activity self-efficacy mediated the association between physical activity and knowledge (β, 0.24; 95% CI, 0.17 to 0.32) and social support (β, 0.30; 95% CI, 0.20 to 0.39). The data fit of the model (RMSEA = 0.067, CFI = 0.851, TLI = 0.828, χ2/df = 3.440) was acceptable.
Conclusion
This study found that the prevalence of being physically inactive was high in pregnant women with a high risk for GDM. The present study’s findings suggested that healthcare providers should try to enhance physical activity self-efficacy, knowledge, and social support of pregnant women with a high risk for GDM to improve their physical activity with a focus on physical activity self-efficacy.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-024-07068-9.
Keywords: Gestational diabetes, Physical activity, Knowledge, Self-efficacy, Social support, Mediator
Introduction
Physical activity (PA) is any bodily movement produced by skeletal muscles that requires energy expenditure [1]. Physical activity is safe and benefits the mother and fetus [2]. It can promote body metabolism, increase insulin sensitivity, improve insulin glucose transport capacity, and reduce insulin resistance [3]. Evidence suggests that physical activity can decrease the odds of developing gestational diabetes mellitus (GDM) in pregnant women [4]. GDM is a public health concern that poses long-term and short-term threats to maternal and fetal morbidity [3, 5]. GDM affects about 15% and 14.8% of pregnant women worldwide [6] and in mainland China [7], respectively. The current guidelines recommend that pregnant women with no contraindications to physical activity do a minimum of 150 min of moderate-intensity physical activity every week [8]. Physical inactivity refers to not meeting the current physical activity guidelines [9]. Unfortunately, most pregnant women worldwide are physically inactive [10]. A study in mainland China showed that 67.28% of pregnant women were physically inactive [11]. Many pregnant women with a high risk for GDM maintain a sedentary lifestyle [12].
Midwives and obstetric nurses play a vital role in facilitating pregnant women with a high risk for GDM to be physically active. The previous studies suggest that many amendable factors, including physical activity self-efficacy, knowledge, and social support, may be related to physical activity in pregnant women [13, 14]. Physical activity self-efficacy refers to an individual’s confidence in their ability to sustain physical activity under diverse circumstances. According to Bandura [15], self-efficacy is crucial for self-management and behavioural change [16]. Previous studies found that physical activity self-efficacy was positively associated with physical activity engagement [14, 17] and maybe a central mediator in overcoming barriers and enhancing physical activity among pregnant women [14]. The results of the previous studies on the association between knowledge and physical activity were inconsistent [14, 18, 19]. Some studies suggest that pregnant women are physically inactive because of a lack of knowledge [14, 18]. In contrast, another study has not found any significant associations between knowledge and physical activity [19]. McKeough [20] indicated that possessing knowledge is essential, yet it only sometimes translates to action. Mediating factors may exist between knowledge and physical activity in pregnant women with a high risk for GDM. Previous studies have also found that social support is directly related to physical activity [13, 14]. Moreover, McNeill [21] found that physical activity self-efficacy mediates the association between social support and physical activity in non-pregnant individuals. Physical activity self-efficacy may also mediate between social support and physical activity in pregnant women with a high risk for GDM.
A better understanding of mediators can help tailor interventions [22]. Mediation analysis is a set of methods to extract information about the causal mechanisms through which a predictor affects an outcome [23]. To our knowledge, no studies in mainland China have used mediation analysis to explore the potential mediator between physical activity and related factors, including physical activity self-efficacy, knowledge, and social support in pregnant women with a high risk for GDM. Thus, the present study aimed to determine the relationship between knowledge, social support, and physical activity, with a focus on the mediating role of physical activity self-efficacy in pregnant women with a high risk for GDM.
Methods
Study design, setting, and participants
This cross-sectional study was conducted and reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE). Eligible pregnant women were recruited consecutively from July 2022 to May 2023 at the antenatal clinic of a tertiary hospital in Guangzhou, China. The inclusion criteria for the pregnant women with a high risk for GDM were: (1) 18 years and older; (2) gestational age between 5 and 13 weeks; (3) have at least one risk factor for GDM, including (a) age ≥ 35 years; (b) pre-pregnancy body mass index (BMI) ≥ 25 kg/m2; (c) polycystic ovary syndrome; (d) family history of diabetes; (e) history of unexplained stillbirth, miscarriage, or neonatal death; (f) history of delivering a large baby (birth weight ≥ 4000 g); or (g) history of GDM [24]. Women were excluded if they had any contraindications to physical activity, including unexplained persistent vaginal bleeding; severe cardiovascular, respiratory, or systemic disease; incompetent cervix; multiple pregnancies; recurrent miscarriage; symptomatic anemia; type 1 diabetes; uncontrolled hypertension and thyroid disease [25]. The sample size for a structural equation model (SEM) should be more than 200 to ensure estimation stability [26].
Measurement
Outcome
The Chinese version of the Pregnancy Physical Activity Questionnaire (PPAQ) measured pregnant women’s time spent, type, and intensity of physical activity [27]. The Chinese version of PPAQ (C-PPAQ) addresses 31 activities that were classified into four types of physical activity, including “Sports and Exercises” (8 activities), “Household and Caregiving” (13 activities), “Transportation” (5 activities) and “Occupation” (5 activities) [27]. Each activity has a specific metabolic equivalent task (MET) value (1 MET = 1 kcal/kg hour) and was classified by intensity: sedentary (< 1.5 METs), light (1.5–2.9 METs), moderate (3.0–6.0 METs), and vigorous intensity (> 6.0 METs). Energy expenditure was calculated by multiplying duration (hours) with activity intensity (METs). The content validity and test-retest intraclass correlation coefficient (ICC) of the C-PPAQ were 0.94 and 0.94, respectively [27]. According to the World Health Organization [9], this study defines not meeting the current physical activity guidelines as engaging in < 150 min/week of moderate-intensity physical activity.
Mediator
The Pregnancy Physical Activity Self-Efficacy Scale (P-PASES) measured pregnant women’s physical activity self-efficacy in the present study [28]. The P-PASES has 10 items. Each item is rated on a 5-point Likert scale, from 1 (strongly disagree) to 5 (strongly agree). The total scores range from 10 to 50. A higher score indicates a higher level of physical activity self-efficacy. Physical activity self-efficacy can be categorized into three levels: low (score ≤ 20), moderate (score ≥ 21 and score ≤ 40), and high (score ≥ 41) [29]. The Chinese version of the P-PASES is reliable with a Cronbach’s α of 0.80 [29]. The Cronbach’s α of the P-PASES was 0.91 in the present study.
Independent variables
The Pregnancy Physical Activity Knowledge Scale (P-PAKS) was used to measure physical activity knowledge [30]. The P-PAKS has 20 items, with three possible answers, “yes,” “no,” or “don’t know.” Correct answers are scored 1 point, while incorrect or “don’t know” responses are scored 0 points. A higher total score indicates a higher awareness of physical activity knowledge. Pregnant women were considered highly aware of physical activity knowledge if they correctly answered 14 or more items [30]. The reported content validity and test-retest intraclass correlation coefficient (ICC) of the P-PAKS were 0.92 and 0.81, respectively [30]. The Cronbach’s α of the P-PAKS was 0.93 in the present study.
The present study used the Physical Activity Social Support Scale (PASSS) to measure social support for physical activity [31]. The PASSS has 24 items. Items are scored on a 5-point Likert scale, with 1 indicating “strongly disagree” and 5 indicating “strongly agree.” The total scores range from 24 to 120, with a higher score indicating more social support for physical activity. Social support for physical activity can be categorized into low (score ≤ 72) and high (score>72) levels [31]. The reported Cronbach’s α and test-retest reliability of the PASSS were 0.95 and 0.88, respectively [31]. The Cronbach’s α of the PASSS was 0.94 in the present study.
Socio-demographic data were collected, including maternal age, marital status, educational attainment, employment status, and family income. Obstetric data included parity, whether the pregnancy was planned, and the type of conception. Data on physical activity included pre-pregnancy physical activity habits, engagement in antenatal physical activity classes, and intention for physical activity.
Ethical considerations and data collection
This study was approved by the Institutional Review Board of a local university. This study conforms to the provisions of the 1995 Declaration of Helsinki (as revised in Edinburgh in 2000). All participants were assured that their participation was voluntary and their data would be kept confidential. The data was collected by the first author, who worked as a research assistant (RA) at the antenatal clinic of the study hospital. The RA checked all the medical records of pregnant women booked for antenatal care in the study hospital and identified eligible pregnant women. All eligible pregnant women who came to the antenatal clinic were invited to participate in the study. The RA explained the purpose of the study, and pregnant women who signed the informed consent form were asked to complete the questionnaires in a quiet room. The RA stayed nearby to answer questions, if any, and received the completed questionnaires.
Data analysis
Data were analyzed using SPSS 25.0 (IBM, Armonk, New York, USA) and MPLUS 8.0 (Muthén & Muthén, 1998-2017). Descriptive statistics were used to present the characteristics of pregnant women and the study variables. Pearson correlation analysis explored preliminary relationships among the study variables. Differences in physical activity with different socio-demographic, obstetric, and physical activity-related characteristics were compared by an independent-sample t-test or a one-way ANOVA. All the variables with p < 0.05 in the above tests were inputted into a multivariate linear regression model to determine the factors independently associated with physical activity. The SEM was used to test the paths between physical activity and physical activity self-efficacy, knowledge, and social support. The SEM examined both direct and indirect associations among the variables. Bias-corrected bootstrapped 95% confidence intervals (CIs) were used to test the indirect effects. Indirect effects were considered significant if the bootstrapped 95% CIs excluded zero [32]. The bootstrap analysis utilized 5000 samples for estimates. The indices employed to assess the model fit included the root mean square error of approximation (RMSEA; < 0.08), comparative fit index (CFI; > 0.90), Tucker Lewis index (TLI; > 0.90), and χ2/degrees of freedom (df) ratio (χ2/df < 3) [33].
Results
Sample characteristics
Of the 558 eligible pregnant women with a high risk for GDM, 18 refused to participate in the study. Three of the 540 pregnant women who agreed to participate in the study did not complete the questionnaires. Therefore, 537 pregnant women with a high risk for GDM were included in this study, with a response rate of 96.2%. Table 1 shows the sociodemographic and obstetric characteristics of pregnant women with a high risk for GDM. All women were married and had a mean (SD) age of 31.52 (4.50) years. Most pregnant women with a high risk for GDM received an education from a junior college or above (75.4%) and were employed full-time (69.3%). Most pregnant women had a planned pregnancy (84.0%) and a spontaneous conception (72.1%). Nearly half of the pregnant women intended to engage in physical activity during their pregnancies (49.7%).
Table 1.
Sociodemographic, obstetric and physical activity related characteristics of the pregnant women with a high risk for GDM (N = 537)
| Characteristics | n (%) |
|---|---|
| Age (years) | |
| <35 | 383 (71.3) |
| ≥ 35 | 154 (28.7) |
| Education | |
| ≤ High school | 132 (24.6) |
| ≥ Junior college | 405 (75.4) |
| Employment | |
| Housewife | 129 (24.0) |
| Part-time | 36 (6.7) |
| Full time | 372 (69.3) |
| Monthly household income (per person per month) | |
| <¥6000 (about US$822) | 149 (27.7) |
| ¥ 6000-¥10,000 (about US$822–US$1370) | 207 (38.5) |
| ≥¥10,000 (aboutUS$1370) | 181 (33.7) |
| Parity | |
| Nulliparity | 321 (59.8) |
| Multiparity | 216 (40.2) |
| Planned pregnancy | |
| Yes | 451 (84.0) |
| No | 86 (16.0) |
| Type of conception | |
| Assisted reproductive technology | 150 (27.9) |
| Spontaneous | 387 (72.1) |
| Pre-pregnancy physical activity habits | |
| Yes | 187 (34.8) |
| No | 350 (65.2) |
| Attending antenatal physical activity classes | |
| Yes | 212 (39.5) |
| No | 325 (60.5) |
| Intention for physical activity | |
| Yes | 267 (49.7) |
| No | 270 (50.3) |
Description of the study variables
Table 2 presents the study variables’ mean and SD. Of the 537 pregnant women with a high risk for GDM, 228 (42.5%) reported being physically inactive; 19 (3.5%), 450 (83.8%), and 68 (12.7%) pregnant women reported low level, moderate level, and high level of physical activity self-efficacy, respectively; more than half of the pregnant women (n = 271, 50.5%) had a low awareness of knowledge; and nearly one-third pregnant women (n = 149, 27.9%) had a low level of social support for physical activity.
Table 2.
Mean, standard deviation (SD), and correlation of physical activity, physical activity self-efficacy, knowledge, and social support (N = 537)
| Variable | Mean (SD) | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| 1. Physical activity (MET-h/week) | 138.67 (83.70) | - | |||
| 2. Knowledge | 12.81 (4.35) | 0.26* | - | ||
| 3. Social support | 80.06 (16.52) | 0.37* | 0.23* | - | |
| 4. Physical activity self-efficacy | 34.19 (7.36) | 0.28* | 0.32* | 0.37* | - |
Associations between physical activity and physical activity self-efficacy, knowledge, and social support
Table 2 also presents the relationships between physical activity self-efficacy, knowledge, social support, and physical activity. Significant associations existed among physical activity self-efficacy, knowledge, social support, and physical activity. The multiple regression model evaluated the relationships between physical activity and physical activity self-efficacy, knowledge, and social support by adjusting age, type of conception, education, and intention for physical analysis (Table 3). Table 4 presents the results of the multiple regression model. Physical activity self-efficacy, knowledge, social support, education, and type of conception were predictors of physical activity in pregnant women with a high risk for GDM.
Table 3.
Differences in physical activity among various socio-demographic, obstetric, and physical activity-related characteristics sub-groups (N = 537)
| Variable | Physical activity | Test value | P |
|---|---|---|---|
| Mean (SD) | |||
| Age (years) | t = 2.64 | 0.009 | |
| <35 | 144.68 (85.56) | ||
| ≥ 35 | 123.71 (77.14) | ||
| Type of conception | t = 4.62 | <0.001 | |
| Assisted reproductive technology | 112.37 (68.26) | ||
| Spontaneous | 148.86 (86.93) | ||
| Education | t = -3.46 | 0.001 | |
| ≤ High school | 117.02 (87.82) | ||
| ≥ Junior college | 145.73 (81.18) | ||
| Intention for physical activity | t = -2.67 | 0.008 | |
| Yes | 129.15 (80.17) | ||
| No | 148.30 (86.21) |
Table 4.
Multiple regression analysis on physical activity in pregnant women with a high risk for GDM (N = 537)
| Independent variables | B | SE | β | t | P | 95% CI for B | |
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Constant | 6.49 | 21.15 | 0.31 | 0.759 | -35.06 | 48.04 | |
| Physical activity self-efficacy | 1.86 | 0.52 | 0.16 | 3.59 | <0.001 | 0.84 | 2.88 |
| Knowledge | 2.92 | 0.85 | 0.15 | 3.45 | 0.001 | 1.26 | 4.58 |
| Social support | 0.52 | 0.22 | 0.10 | 2.36 | 0.019 | 0.09 | 0.95 |
| Educationa | |||||||
| ≤ High school | -15.10 | 8.07 | -0.08 | -1.98 | 0.048 | -31.85 | -0.15 |
| ≥ Junior college | Reference category | ||||||
| Type of conceptionb | |||||||
| Assisted reproductive technology | -23.52 | 7.72 | -0.13 | -3.05 | 0.002 | -38.69 | -8.36 |
| Spontaneous | Reference category | ||||||
Overall R2 = 0.137; model fit: F = 17.969, p < 0.001, Statistically significant at p < 0.05
aEducation: ≥ Junior college = 0, ≤ High school = 1
bType of conception: Spontaneous = 0, Assisted reproductive technology = 1
VIF: 1.065 ~ 1.297; Bold values indicate statistical significance (p < 0.05)
The mediation effect of physical activity self-efficacy in the associations between physical activity and knowledge and social support
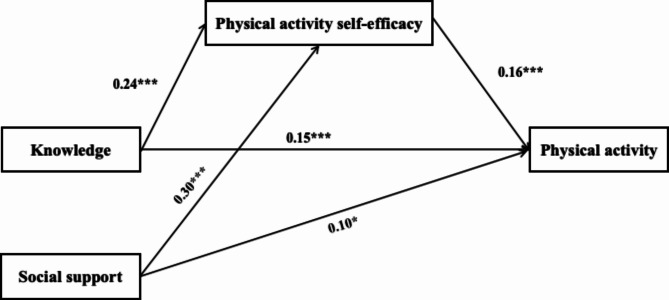
The data fit of the SEM model (RMSEA = 0.067, CFI = 0.851, TLI = 0.828, χ2/df = 3.440) was acceptable. As shown in Table 5; Fig. 1, Physical activity self-efficacy (β, 0.16; 95% CI, 0.07 to 0.24), knowledge (β, 0.15; 95% CI, 0.07 to 0.24), and social support (β, 0.10; 95% CI, 0.01 to 0.19) had a direct effect on physical activity. Knowledge (β, 0.24; 95% CI, 0.17 to 0.32) and social support (β, 0.30; 95% CI, 0.20 to 0.39) directly affected physical activity self-efficacy. Physical activity self-efficacy mediated the relationship between physical activity and knowledge (β, 0.04; 95% CI, 0.02 to 0.06) and social support (β, 0.05; 95% CI, 0.02 to 0.08) among pregnant women with a high risk for GDM.
Table 5.
Direct and indirect effects (N = 537)
| Path | β | SE | 95% CI | P |
|---|---|---|---|---|
| Direct effects | ||||
| Physical activity self-efficacy → Physical activity | 0.16 | 0.04 | [0.07, 0.24] | < 0.001 |
| Knowledge → Physical activity | 0.15 | 0.04 | [0.07, 0.24] | < 0.001 |
| Social support → Physical activity | 0.10 | 0.04 | [0.01, 0.19] | 0.023 |
| Knowledge → Physical activity self-efficacy | 0.24 | 0.04 | [0.17, 0.32] | < 0.001 |
| Social support → Physical activity self-efficacy | 0.30 | 0.05 | [0.20, 0.39] | < 0.001 |
| Indirect effects | ||||
| Knowledge → Physical activity | ||||
| Total effect | 0.19 | 0.04 | [0.12, 0.28] | < 0.001 |
| Indirect effect (Knowledge → Physical activity self-efficacy → Physical activity) | 0.04 | 0.01 | [0.02, 0.06] | 0.001 |
| Direct effect | 0.15 | 0.04 | [0.07, 0.24] | < 0.001 |
| Social support → Physical activity | ||||
| Total effect | 0.15 | 0.04 | [0.06, 0.23] | 0.001 |
| Indirect effect (Social support→ Physical activity self-efficacy → Physical activity) | 0.05 | 0.02 | [0.02, 0.08] | 0.003 |
| Direct effect | 0.10 | 0.04 | [0.01, 0.19] | 0.023 |
Note. Data are reported as standardized coefficients. *P < 0.05, **P < 0.01, ***P < 0.001
Fig. 1.
Mediation model of knowledge, physical activity self-efficacy, social support, and physical activity with standardized coefficients *P < 0.05, **P < 0.01, ***P < 0.001
Discussion
This study examined the associations between physical activity self-efficacy, knowledge, social support, and physical activity and further explored the mediating effect of physical activity self-efficacy among pregnant women with a high risk for GDM. The present study found that nearly half of pregnant women with a high risk for GDM were physically inactive. This aligns with a prior study from Wuhan, China, which reported that 42.9% of pregnant women did not meet the current physical activity guidelines [34]. Studies from other nations-developed and developing [35, 36]-uniformly note reduced physical activity levels in pregnant women despite using different measurement instruments and assessment methodologies. The present study, consistent with the previous studies [34, 36], indicated that being physically inactive was a significant public health concern among pregnant women with a high risk for GDM, requiring healthcare professionals’ attention.
The present study found that knowledge was a predictor and directly associated with physical activity. Janakiraman [37] also reported that a lack of knowledge about physical activity was a barrier to being physically active. A previous qualitative study observed that pregnant women’s motivation to engage in physical activity waned due to a lack of awareness regarding its impact on maternal and infant health [20]. The present study’s findings, consistent with the previous studies [20, 37], suggested the importance of adequate knowledge in promoting physical activity. Unfortunately, over half of the pregnant women with a high risk for GDM in the present study had inadequate pregnancy physical activity knowledge. This may be because healthcare providers in the local hospital provided pregnant women with limited pregnancy physical activity knowledge. The most common sources of physical activity knowledge for pregnant women were the Internet rather than healthcare professionals [38], which could be inaccurate, confusing, and overwhelming. Healthcare providers in local hospitals may lack updated pregnancy physical activity knowledge to give effective counseling [39]. A continued education program on current physical activity guidelines for pregnant women may help local healthcare providers provide expert counseling.
The present study also found that social support was a predictor and directly associated with physical activity. Prior studies have consistently found that partners, family, friends, and healthcare professionals were sources of social support for pregnant women’s physical activity [13, 40]. Sjögren Forss & Stjernberg [41] indicated that pregnant women and their partners shared similar physical activity patterns. The partner or husband of the pregnant woman was the most significant person who provided social support for physical activity. The pregnant women who received more social support from their partners were more likely to increase their physical activity. However, nearly one-third of the pregnant women with a high risk for GDM in the present study had a low level of social support for physical activity. This finding suggested that on top of providing support to pregnant women with a high risk for GDM, healthcare providers could invite husbands/partners to become actively involved in pregnant women’s physical activity.
The present study also found that physical activity self-efficacy was a predictor and directly associated with physical activity. This result was consistent with the previous studies [13, 14]. Garland [42] and Cramp & Bray [43] also found that pregnant women with higher physical activity self-efficacy tend to engage more in physical activities. This result was also consistent with Bandura’s self-efficacy theory, which proposed that individuals with higher levels of self-efficacy tend to handle more challenging tasks, exert more effort, and perform better in the face of challenges [15].
Furthermore, the present study found that physical activity self-efficacy mediated between knowledge and physical activity. Piaseu [44] also indicated that merely providing individuals with knowledge about healthy behaviours does not guarantee a change in their behaviours. The present study also found that physical activity self-efficacy mediated the association between social support and physical activity. The finding was supported by Bandura’s self-efficacy theory, which suggested that physical activity self-efficacy might mediate between social support and physical activity [15]. Verloigne [45] and Ren [46] also observed physical activity self-efficacy as a mediator between peer/parental support and physical activity in a study on adolescents.
The findings of the present study emphasized the importance of physical activity self-efficacy. However, most pregnant women with a high risk for GDM in the present study had a moderate level of physical activity self-efficacy; some even had a low level. These findings suggested that healthcare providers should develop strategies to enhance pregnant women’s physical activity self-efficacy. Flannery [39] suggested that pregnant women enjoyed meeting other women and expressed interest in physical activity classes tailored for pregnancy. Moreover, perceiving others’ successful engagement in target activities can significantly enhance pregnant women’s physical activity self-efficacy [47]. Healthcare professionals may provide pregnant women with a high risk for GDM with physical activity classes to enhance their knowledge, social support, and physical activity self-efficacy.
The present study also found that education of high school or below and using assisted reproductive technology were predictors of physical activity in pregnant women with a high risk for GDM. These results suggest that physical activity enhancement programmes should target pregnant women with a high risk for GDM who have a high school education or below and who have used assisted reproductive technology.
Limitations and practice implications
There are several limitations in the present study. The present study used a cross-sectional design, which did not infer a cause-effect relationship. Longitudinal studies need to be conducted to provide more evidence about the findings obtained from this study in the future. Secondly, the participants in this study were recruited from a teaching hospital in the urban city of Guangzhou. The findings of the present study may not be applied to pregnant women with a high risk for GDM in rural China. Furthermore, all measures were based on self-report, which could introduce recall errors and subjective bias.
Despite these limitations, the present study is the first to explore the mediating effect of physical activity self-efficacy on the association between knowledge, social support, and physical activity in pregnant women with a high risk for GDM. These findings contribute to a better understanding of the interactive mechanisms underlying complex factors of physical activity. Importantly, this research provides a valuable theoretical and methodological approach by emphasizing physical activity self-efficacy’s role in enhancing physical activity in pregnant women with a high risk of GDM.
Conclusion
This study found that the prevalence of being physically inactive was high in pregnant women with a high risk for GDM. Physical activity self-efficacy, knowledge, social support, education, and type of conception were the predictors of physical activity in pregnant women with a high risk for GDM. Furthermore, Physical activity self-efficacy mediated the association between physical activity and knowledge and social support. Healthcare providers should try to enhance physical activity self-efficacy, knowledge, and social support of pregnant women with a high risk for GDM to improve their physical activity with a focus on physical activity self-efficacy.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Acknowledgements
The researchers thank the National Natural Science Foundation for funding this research project. They would also like to thank the pregnant women who participated in the study.
Author contributions
All authors approved the manuscript’s content and have contributed significantly to the research and writing. Lu Chen and Rong-rong Han contributed equally to this work and should be considered co-first authors. Lu Chen, Rong-rong Han, and Ling-ling Gao were responsible for the study’s conception and design. Lu Chen performed the data collection. Lu Chen and Rongrong Han were accountable for analyzing the data. Lu Chen, Xin Chen, Bai-ling Fu, Ling-ling Gao, and Bernice O C Lam Nogueira have participated in interpreting data. Lu Chen has drafted the manuscript. Ling-ling Gao and Bernice O C Lam Nogueira revised the manuscript.
Funding
This study was supported by the research grant ‘Development and evaluation of a precise intervention on physical inactivity to prevent gestational diabetes mellitus based on the ecological model’ (Grant No. 72174216) from the National Natural Science Foundation of China.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
This study obtained ethical approval from the Institutional Review Board of the School of Nursing, Sun Yat-Sen University (L2022SYSU-HL-057). Clinical trial number is not applicable. Eligible pregnant women signed an informed consent form before participating in the study and were assured of confidentiality.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Bernice O. C. Lam Nogueira, Email: lamnog@mpu.edu.mo.
Ling-ling Gao, Email: gaoll@mail.sysu.edu.cn.
References
- 1.World Health Organization. (2022). Global status report on physical activity 2022. https://www.who.int/publications-detail-redirect/9789240059153
- 2.Hinman SK, Smith KB, Quillen DM, Smith MS. Exercise in Pregnancy: A Clinical Review. Sports health. 2015;7(6):527–31. 10.1177/1941738115599358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McIntyre HD, Catalano P, Zhang C, Desoye G, Mathiesen ER, Damm P. Gestational diabetes mellitus. Nat Reviews Disease Primers. 2019;5(1):47. [DOI] [PubMed] [Google Scholar]
- 4.Mijatovic-Vukas J, Capling L, Cheng S, Stamatakis E, Louie J, Cheung NW, Markovic T, Ross G, Senior A, Brand-Miller JC, Flood VM. Associations of Diet and Physical Activity with Risk for Gestational Diabetes Mellitus: A Systematic Review and Meta-Analysis. Nutrients. 2018;10(6):698. 10.3390/nu10060698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saravanan P, Diabetes in Pregnancy Working Group, Maternal Medicine Clinical Study Group, & Royal College of Obstetricians and Gynaecologists, UK. Gestational diabetes: opportunities for improving maternal and child health. Lancet Diabets Endocrionol. 2020;8(9):793–800. 10.1016/S2213-8587(20)30161-3. [DOI] [PubMed] [Google Scholar]
- 6.Yuen L, Saeedi P, Riaz M, Karuranga S, Divakar H, Levitt N, Yang X, Simmons D. Projections of the prevalence of hyperglycaemia in pregnancy in 2019 and beyond: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107841. 10.1016/j.diabres.2019.107841. [DOI] [PubMed] [Google Scholar]
- 7.Gao C, Sun X, Lu L, Liu F, Yuan J. Prevalence of gestational diabetes mellitus in mainland China: A systematic review and meta-analysis. J diabetes Invest. 2019;10(1):154–62. 10.1111/jdi.12854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yang X, Li H, Zhao Q, Han R, Xiang Z, Gao L. Clinical Practice Guidelines That Address Physical Activity and Exercise During Pregnancy: A Systematic Review. J Midwifery Women’s Health. 2022;67(1):53–68. 10.1111/jmwh.13286. [DOI] [PubMed] [Google Scholar]
- 9.Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, Carty C, Chaput JP, Chastin S, Chou R, Dempsey PC, DiPietro L, Ekelund U, Firth J, Friedenreich CM, Garcia L, Gichu M, Jago R, Katzmarzyk PT, Lambert E, Willumsen JF. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. British J Sports Med. 2020;54(24):1451–1462. 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed]
- 10.Silva-Jose C, Sánchez-Polán M, Barakat R, Gil-Ares J, Refoyo I. Level of Physical Activity in Pregnant Populations from Different Geographic Regions: A Systematic Review. J Clin Med. 2022;11(15):4638. 10.3390/jcm11154638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lü Y, Feng Y, Ma S, Jiang Y, Ma L. Changes in physical activity across pregnancy among Chinese women: a longitudinal cohort study. BMC Womens Health. 2021;21(1):236. 10.1186/s12905-021-01377-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bianchi C, de Gennaro G, Romano M, Baronti W, Aragona M, Battini L, Bottone P, Del Prato S, Bertolotto A. Exercise during pregnancy: how much active are pregnant women at risk of gestational diabetes despite few contraindications? Gynecol endocrinology: official J Int Soc Gynecol Endocrinol. 2021;37(2):101–4. 10.1080/09513590.2020.1775196. [DOI] [PubMed] [Google Scholar]
- 13.Chen L, Deng YF, Fan MQ, Yuan HB, Meng LR, Gao LL. Assisted reproductive technology and physical activity among Chinese pregnant women at high risk for gestational diabetes mellitus in early pregnancy: A cross-sectional study. Res Nurs Health. 2024;47(3):324–34. 10.1002/nur.22369. [DOI] [PubMed] [Google Scholar]
- 14.Yang X, Han R, Song Y, Zhang J, Huang H, Zhang J, Wang Y, Gao L. The Mediating Role of Physical Activity Self-Efficacy in Predicting Moderate-Intensity Physical Activity in Pregnant People at High Risk for Gestational Diabetes. J Midwifery Women’s Health. 2024;69(3):403–13. 10.1111/jmwh.13589. [DOI] [PubMed] [Google Scholar]
- 15.Bandura A. Self-efficacy: The exercise of control. East China Normal University, Shanghai; 2003 [In Chinese]. [Google Scholar]
- 16.Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29(4):823–9. 10.2337/diacare.29.04.06.dc05-1615. [DOI] [PubMed] [Google Scholar]
- 17.Yu P, Zhou L, Meng F, Xu Y, Jiang Y, Zhou Y. Developmental trajectories of health-promoting behaviours among pregnant women: A longitudinal study. J Clin Nurs. 2023;32(1–2):234–42. 10.1111/jocn.16214. [DOI] [PubMed] [Google Scholar]
- 18.Gebretatyos H, Amanuel S, Ghirmai L, Gebreyohannes G, Tesfamariam EH. Effect of health education on healthy nutrition and physical activity among female teachers aged 40–60 years in Asmara, Eritrea: a quasiexperimental study. J Nutr Metab. 2020;2020(5721053). 10.1155/2020/5721053. [DOI] [PMC free article] [PubMed]
- 19.Rimal RN. Longitudinal Influences of Knowledge and Self-efficacy on Exercise Behavior: Tests of a Mutual Reinforcement Model. J Health Psychol. 2001;6(1):31–46. 10.1177/135910530100600103. [DOI] [PubMed] [Google Scholar]
- 20.McKeough R, Blanchard C, Piccinini-Vallis H. Pregnant and Postpartum Women’s Perceptions of Barriers to and Enablers of Physical Activity During Pregnancy: A Qualitative Systematic Review. J Midwifery Women’s Health. 2022;67(4):448–62. 10.1111/jmwh.13375. [DOI] [PubMed] [Google Scholar]
- 21.McNeill LH, Wyrwich KW, Brownson RC, Clark EM, Kreuter MW. Individual, social environmental, and physical environmental influences on physical activity among black and white adults: a structural equation analysis. Annals Behav medicine: publication Soc Behav Med. 2006;31(1):36–44. 10.1207/s15324796abm3101_7. [DOI] [PubMed] [Google Scholar]
- 22.Bauman AE, Sallis JF, Dzewaltowski DA, Owen N. Toward a better understanding of the influences on physical activity: the role of determinants, correlates, causal variables, mediators, moderators, and confounders. Am J Prev Med. 2002;23(2 Suppl):5–14. 10.1016/s0749-3797(02)00469-5. [DOI] [PubMed] [Google Scholar]
- 23.Mokhayeri Y, Mansournia MA. Methodological point on mediation analysis. Int J Epidemiol. 2019;48(5):1730–1. 10.1093/ije/dyz104. [DOI] [PubMed] [Google Scholar]
- 24.Xie X, Kong BH, Duan T, Lin ZQ, Di W, Ma D, Cao YX, Qi HB. Obstetrics and gynecology. 9th ed. People’s Medical Publishing House; 2018.
- 25.Professional Committee of Gestational Diabetes Mellitus, Chinese Maternal and Child Health Association. Expert consensus on exercise during pregnancy (draft). Chin J Perinat Med. 2021;24(9):641–5. Obstetrics Subgroup, Society of Obstetrics and Gynecology, Chinese Medical Association. [Google Scholar]
- 26.Kline RB. Principles and practice of structural equation modeling. 2nd ed. The Guilford Press; 2005.
- 27.Xiang M, Konishi M, Hu H, Takahashi M, Fan W, Nishimaki M, Ando K, Kim HK, Tabata H, Arao T, Sakamoto S. Reliability and Validity of a Chinese-Translated Version of a Pregnancy Physical Activity Questionnaire. Matern Child Health J. 2016;20(9):1940–7. 10.1007/s10995-016-2008-y. [DOI] [PubMed] [Google Scholar]
- 28.Bland HW, Melton BF, Marshall ES, Nagle JA. Measuring exercise self-efficacy in pregnant women: psychometric properties of the pregnancy-exercise self-efficacy scale (P-ESES). J Nurs Meas. 2013;21(3):349–59. 10.1891/1061-3749.21.3.349. [DOI] [PubMed] [Google Scholar]
- 29.Yang HM, Deng YF, Gao LL. Reliability and validity of the Chinese version of the Pregnancy Exercise Self-efficacy Scale. Chin J Nurs. 2017;52(5):632–6. [Google Scholar]
- 30.Liu QP, Gou BH, Xiao Q. Investigation on cognition of pregnant women to exercise during pregnancy. Chin J Mod Nurs. 2012;19(13):1528–31. [Google Scholar]
- 31.Xiang ZX, Han RR, Zhao Q, Yang X, Gao LL. Adaptation and psychometric evaluation of the Social Support Scale for Exercise among pregnant women. Chin Nurs Manage. 2022;22(7):998–1002. [Google Scholar]
- 32.Macho S, Ledermann T. Estimating, testing, and comparing specific effects in structural equation models: the phantom model approach. Psychol Methods. 2011;16(1):34–43. 10.1037/a0021763. [DOI] [PubMed] [Google Scholar]
- 33.Hair JF, Babin BJ, Anderson RE, Black WC. Multivariate data analysis. 8th ed. Cengage Learning; 2019.
- 34.Xiang M, Zhang J, Liang H, Zhang Z, Konishi M, Hu H, Nishimaki M, Kim HK, Tabata H, Shimizu H, Arao T, Sakamoto S. Physical activity and dietary intake among Chinese pregnant women: an observational study. BMC Pregnancy Childbirth. 2019;19(1):295. 10.1186/s12884-019-2452-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Santo EC, Forbes PW, Oken E, Belfort MB. Determinants of physical activity frequency and provider advice during pregnancy. BMC Pregnancy Childbirth. 2017;17(1):286. 10.1186/s12884-017-1460-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nguyen CL, Pham NM, Lee AH, Nguyen PTH, Chu TK, Ha AVV, Duong DV, Duong TH, Binns CW. Physical activity during pregnancy is associated with a lower prevalence of gestational diabetes mellitus in Vietnam. Acta Diabetol. 2018;55(9):955–62. 10.1007/s00592-018-1174-3. [DOI] [PubMed] [Google Scholar]
- 37.Janakiraman B, Gebreyesus T, Yihunie M, Genet MG. Knowledge, attitude, and practice of antenatal exercises among pregnant women in Ethiopia: A cross-sectional study. PLoS ONE. 2021;16(2):e0247533. 10.1371/journal.pone.0247533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gao LL, Larsson M, Luo SY. Internet use by Chinese women seeking pregnancy-related information. Midwifery. 2013;29(7):730–5. 10.1016/j.midw.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 39.Flannery C, McHugh S, Anaba AE, Clifford E, O’Riordan M, Kenny LC, McAuliffe FM, Kearney PM, Byrne M. Enablers and barriers to physical activity in overweight and obese pregnant women: an analysis informed by the theoretical domains framework and COM-B model. BMC Pregnancy Childbirth. 2018;18(1):178. 10.1186/s12884-018-1816-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shum KW, Ang MQ, Shorey S. Perceptions of physical activity during pregnancy among women: A descriptive qualitative study. Midwifery. 2022;107:103264. 10.1016/j.midw.2022.103264. [DOI] [PubMed] [Google Scholar]
- 41.Sjögren Forss K, Stjernberg L. Physical Activity Patterns Among Women and Men During Pregnancy and 8 Months Postpartum Compared to Pre-pregnancy: A Longitudinal Study. Front public health. 2019;7:294. 10.3389/fpubh.2019.00294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Garland M, Wilbur J, Semanik P, Fogg L. Correlates of Physical Activity During Pregnancy: A Systematic Review with Implications for Evidence-based Practice. Worldviews evidence-based Nurs. 2019;16(4):310–8. 10.1111/wvn.12391. [DOI] [PubMed] [Google Scholar]
- 43.Cramp AG, Bray SR. A prospective examination of exercise and barrier self-efficacy to engage in leisure-time physical activity during pregnancy. Annals Behav medicine: publication Soc Behav Med. 2009;37(3):325–34. 10.1007/s12160-009-9102-y. [DOI] [PubMed] [Google Scholar]
- 44.Piaseu N, Schepp K, Belza B. Causal analysis of exercise and calcium intake behaviors for osteoporosis prevention among young women in Thailand. Health Care Women Int. 2002;23(4):364–76. 10.1080/0739933029008937. [DOI] [PubMed] [Google Scholar]
- 45.Verloigne M, Cardon G, De Craemer M, D’Haese S, De Bourdeaudhuij I. Mediating Effects of Self-Efficacy, Benefits and Barriers on the Association between Peer and Parental Factors and Physical Activity among Adolescent Girls with a Lower Educational Level. PLoS ONE. 2016;11(6):e0157216. 10.1371/journal.pone.0157216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ren Z, Hu L, Yu JJ, Yu Q, Chen S, Ma Y, Lin J, Yang L, Li X, Zou L. The Influence of Social Support on Physical Activity in Chinese Adolescents: The Mediating Role of Exercise Self-Efficacy. Child (Basel Switzerland). 2020;7(3):23. 10.3390/children7030023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kim J, Eys M, Robertson-Wilson J. If they do it, so can I’: a test of a moderated serial mediation model of descriptive norms, self-efficacy, and perceived similarity for predicting physical activity. Psychol Health. 2021;36(6):701–18. 10.1080/08870446.2020.1789641. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.