Abstract
Background
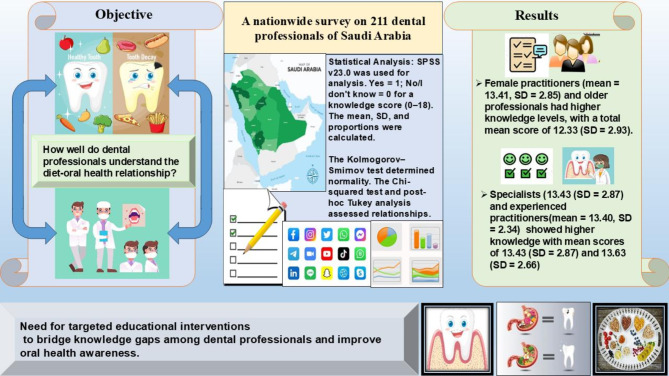
The association between diet and oral health is complex, yet understanding the influence of nutrition on oral health among dental professionals is limited. This study aimed to assess the knowledge levels of dental professionals in Saudi Arabia regarding the relationship between diet and oral health.
Methods
A cross-sectional survey was conducted among 211 dental professionals in Saudi Arabia using an 18-item questionnaire. Data analysis was performed using SPSS v23.0. Descriptive statistics were used to calculate the mean, standard deviation (SD), and proportions. The Kolmogorov–Smirnov test assessed data normality, while the Chi-squared test and post-hoc Tukey analysis were applied to evaluate associations between variables.
Results
The findings revealed that female practitioners (mean = 13.41, SD = 2.85) and older professionals had higher knowledge levels, with a total mean score of 12.33 (SD = 2.93). Significant correlations were observed between knowledge scores and age (ANOVA: F = 2.874; p = 0.024) and between knowledge scores and gender (t-test: t = 6.68, p < 0.001). Oral Medicine Specialists and Periodontists had the highest knowledge scores, with mean scores of 13.43 (SD = 2.87) and 13.63 (SD = 2.66), respectively, while General Dentists scored lower (mean = 10.49, SD = 3.12; ANOVA: F = 4.462; p < 0.001). Practitioners with less than five years of experience had significantly lower knowledge scores (mean = 11.14, SD = 3.23) compared to those with 5–10 years (mean = 13.40, SD = 2.34) and over 20 years of experience (mean = 12.69, SD = 2.22) (ANOVA: F = 5.016; p = 0.002).
Conclusion
Our findings reveal that dental professionals in Saudi Arabia have varying knowledge regarding the relationship between diet and oral health. While awareness exists, there are gaps in understanding the nutritional factors influencing oral health outcomes. Addressing these knowledge gaps through targeted educational interventions is essential, given the crucial role dental professionals play in promoting oral health and educating patients on the importance of nutrition. Enhancing this knowledge will improve patient care and contribute to better community health outcomes through informed preventive strategies and public health initiatives.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12903-024-05363-7.
Keywords: Knowledge, Oral health, Nutrition, Dental professionals, Awareness, Saudi Arabia
Background
Oral health is fundamental to an individual’s well-being and quality of life [1]. The role of Diet and nutrition in impacting oral health has become prominent [2, 3]. Oral health and nutrition share a symbiotic relationship, with diet significantly influencing oral conditions, particularly in developing dental caries. The consumption of high-sugar foods is a key factor in forming dental caries, as it contributes to the growth of harmful bacteria that produce acids, leading to tooth decay [4, 5]. A high-sugar diet is also associated with an increased risk of periodontal inflammation and other oral health problems [6, 7]. In contrast, consuming unprocessed, fibre-rich complex carbohydrates, such as raw vegetables, and calorie-restricted diets has a protective effect by reducing plaque build-up and promoting periodontal health [8–11].
Although several studies have investigated the correlation between diet and oral health [1, 5, 11, 12], there is still a lack of research on comprehending and pinpointing the precise dietary elements contributing to or alleviating oral health problems. Dental professionals play a crucial role in educating patients about diet-related preventive measures. Additionally, they can act as key influencers in community settings, promoting healthy eating habits to improve public oral health. However, there is a lack of research assessing their knowledge of how nutrition impacts oral health.
To date, no study has evaluated dental professionals’ understanding of the role of diet and nutrition in oral health in Saudi Arabia. This study aims to assess their knowledge of the impact of dietary factors on oral health.
Methodology
Study design and setting
This cross-sectional, questionnaire-based study received formal approval from the Jazan University Standing Committee on the Ethics of Scientific Research (REC-45/05/895, HAPO-10-Z-001). The study complied with the principles established in the Helsinki Declaration. The study targeted participants with valid dental licenses who practise in Saudi Arabia in private clinics, government institutions, and teaching hospitals.
Development and content of the questionnaire
The questionnaire, designed to assess dental professionals’ knowledge of diet and oral health, was developed after a comprehensive review of relevant literature and underwent face and content validation by experts in the fields of nutrition and dentistry. Following a pilot test involving 20 professionals, internal reliability was established with a Cronbach’s alpha of 0.81. The final questionnaire consisted of 18 closed-ended items with responses categorized as ‘Yes’, ‘No’, or ‘I don’t know’ in the supplementary Table 1.
Data collection process
The final 18-item questionnaire was distributed through popular social media platforms, including Facebook, Twitter, and WhatsApp, to capture a broad representation of the dental profession in Saudi Arabia. An introduction prefaced the questionnaire, outlining the study’s objectives, voluntary participation, and the confidentiality of the collected data. Participants accessed the questionnaire via a Google Form link, which included an “agree” button to start and a “disagree” button to exit the survey. All items were positively phrased, except for three (Q6, Q9, and Q11), which were framed negatively to evaluate participants’ understanding and critical thinking skills by discerning correct information despite the negative wording.
Inclusion and exclusion criteria
Dental professionals who currently practice in Saudi Arabia in governmental organisations, private practices, and teaching institutions and possess valid licenses were eligible to participate. Professionals who were not licensed were not included. Our initial goal was to enrol 384 participants based on a calculation that considered a 95% confidence level, a 5% margin of error, an 80% power, and a prevalence of knowledge on the topic among 50% of the targeted population.
Statistical analysis
The response data were acquired as an MS Excel spreadsheet and subsequently imported into Statistical Package for Social Sciences (SPSS) software, version 23.0 (IBM Corp. in Armonk, NY, USA). In addition to being processed and analysed as qualitative data, the “Yes” responses were given a score of one, while the other responses (“No” and “I don’t know” were given zero. Accordingly, the overall knowledge score was further converted into a quantitative variable, ranging from zero to 18. The qualitative data were presented as means and standard deviations (SD), while the quantitative data were presented as frequencies and proportions. The qualitative data was assessed for normality using Kolmogorov–Smirnov test. The Chi-squared test was used at each study stage to assess the correlation between the knowledge acquired and various variables. The post-hoc Tukey analysis was implemented to ensure that multiple comparisons were made.
Results
Demographic characteristics
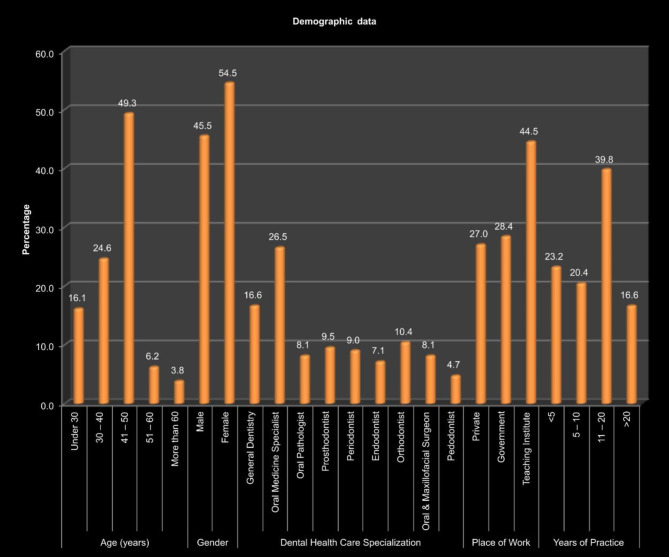
For practical reasons, we could only include 211 participants in the study. Figure 1 presents the distribution of sociodemographic variables. As indicated above, 211 dental professionals participated in the study, with 54.5% females. Around 16% of the participants were under 30 years, 25% were aged 30–40 years, 49% were aged 41–50 years, 6% were aged 51–60, and only around 4% were aged 60. Regarding specialisation, around 27% were Oral Medicine Specialists, 17% were General Dentists, and 10% were Orthodontists; other specialities represented around 46%. Regarding practice settings, around 45% were affiliated with teaching institutes, 28% to government institutions, and 27.0% were working in private practice. Approximately 23% of respondents reported having less than 5 years of practice, while 20% had 5 to 10 years, 40% had 11 to 20 years, and 17% had more than 20 years practice.
Fig. 1.
Descriptive analysis of the socio-demographic variables
Figure 1 presents a descriptive analysis of the socio-demographic characteristics of the study participants. The age distribution shows that the majority (49.3%) of dental professionals were aged 41–50 years, while smaller groups included those under 30 years (16.1%), 30–40 years (24.6%), 51–60 years (6.2%), and over 60 years (3.8%). The gender composition comprised 45.5% males and 54.5% females. The distribution of dental health care specializations indicated that the largest group were Oral Medicine Specialists, followed by General Dentists and other specializations.
Questionnaire responses
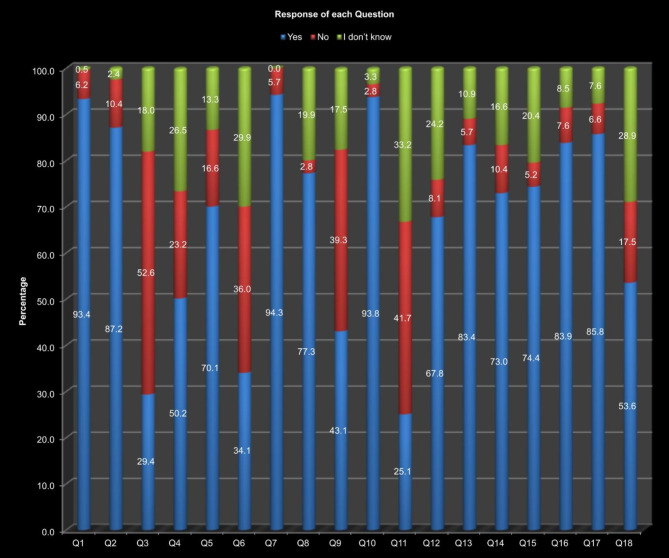
Figure 2; Table 1 summarize the responses to the questionnaire items. The items with the highest knowledge level (highest percentage of “Yes” responses) were about calcium’s role in alveolar bone density (94.3%), the positive impact of Vitamin C-rich foods on gingival inflammation (93.8%), and the link between high-glycemic foods and increased risk of periodontal inflammation and dental caries (93.4%).
Fig. 2.
Summary of responses of 18 questionnaire responses (‘Yes’, ‘No’, ‘I don’t know’)
Table 1.
Summary of responses of 18 questionnaire (‘Yes’, ‘No’, ‘I don’t know’)
| Question | Yes | No | I don’t know | |||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Q1. High-glycaemic food consumption increases the risk of Periodontal inflammation and Dental caries. | 197 | 93.4 | 13 | 6.2 | 1 | 0.5 |
| Q2. Chewing raw vegetables aids in reducing plaque build-up, preventing the development of caries and gingival inflammation. | 184 | 87.2 | 22 | 10.4 | 5 | 2.4 |
| Q3. Individuals having a vegetarian diet have healthier gums and better oral hygiene compared to non-vegetarians | 62 | 29.4 | 111 | 52.6 | 38 | 18.0 |
| Q4. Dietary fats, such as saturated fats, trans fats, and omega-6 fatty acids, influence the risk of periodontal inflammation and oral health problems. | 106 | 50.2 | 49 | 23.2 | 56 | 26.5 |
| Q5. Consumption of unprocessed, fibre-rich complex carbohydrates helps reduce the risk of periodontal inflammation and improves oral health | 148 | 70.1 | 35 | 16.6 | 28 | 13.3 |
| Q6. Omega-3 fatty acids are known for their anti-inflammatory properties, not potentially beneficial in reducing periodontal inflammation and improving oral health | 72 | 34.1 | 76 | 36.0 | 63 | 29.9 |
| Q7. Calcium has a role in the density of the alveolar bone that supports the teeth. | 199 | 94.3 | 12 | 5.7 | - | - |
| Q8. Increased dietary intake of beta-carotene and vitamin A positively impacts periodontal healing. | 163 | 77.3 | 6 | 2.8 | 42 | 19.9 |
| Q9. High serum levels of vitamin B12, folate and iron are associated with swelling of the tongue, papillary atrophy, surface ulceration | 91 | 43.1 | 83 | 39.3 | 37 | 17.5 |
| Q10. Vitamin C-rich foods reduce gingival and periodontal inflammation and support healthy gingival homeostasis | 198 | 93.8 | 6 | 2.8 | 7 | 3.3 |
| Q11. Probiotic bacteria found in yoghurt do not contribute to preserving periodontal health. | 53 | 25.1 | 88 | 41.7 | 70 | 33.2 |
| Q12. Dietary magnesium deficiency increases the prevalence of periodontitis. | 143 | 67.8 | 17 | 8.1 | 51 | 24.2 |
| Q13. Deficiency in vitamin B1 (Thiamine) results in cracked lips and angular cheilosis (cracking at the corners of the mouth) | 176 | 83.4 | 12 | 5.7 | 23 | 10.9 |
| Q14.Vitamin B3 (Niacin) deficiency leads to tongue inflammation, angular cheilosis, and ulcerative gingivitis. | 154 | 73.0 | 22 | 10.4 | 35 | 16.6 |
| Q15. Periodontal disease, anaemia, sore tongue, and burning in the oral cavity are linked to vitamin B6 deficiency. | 157 | 74.4 | 11 | 5.2 | 43 | 20.4 |
| Q16. B12 deficiency manifests as symptoms like angular cheilosis, halitosis, bone loss, bleeding gums, and painful ulcers in the mouth | 177 | 83.9 | 16 | 7.6 | 18 | 8.5 |
| Q17. Iron deficiency causes red, burning tongue, dysphagia (difficulty in swallowing), or angular cheilosis. | 181 | 85.8 | 14 | 6.6 | 16 | 7.6 |
| Q18. Leukoplakia is linked to low serum vitamin A, C, B12, and folic acid levels. | 113 | 53.6 | 37 | 17.5 | 61 | 28.9 |
Table 1 shows the distribution of responses for each questionnaire item, including the questions with the highest percentage of “Yes,” “No,” and “I don’t know” responses. Key findings include a high agreement on questions regarding the impact of high-glycaemic food on periodontal inflammation (93.4% “Yes”), the role of calcium in alveolar bone density (94.3% “Yes”), and the positive effects of vitamin C on gingival health (93.8% “Yes”). In contrast, there was notable uncertainty regarding the role of omega-3 fatty acids in reducing periodontal inflammation (36.0% “No” and 29.9% “I don’t know”) and the association of probiotic bacteria with periodontal health (41.7% “No”)
Regarding the negatively phrased items, around 36% of respondents recognised the potential benefits of omega-3 fatty acids in oral health, 42% reported the presence of possible benefits of probiotics in maintaining periodontal health, and 39% didn’t correlate the high serum levels of vitamin B12, folate, and iron with oral lesions.
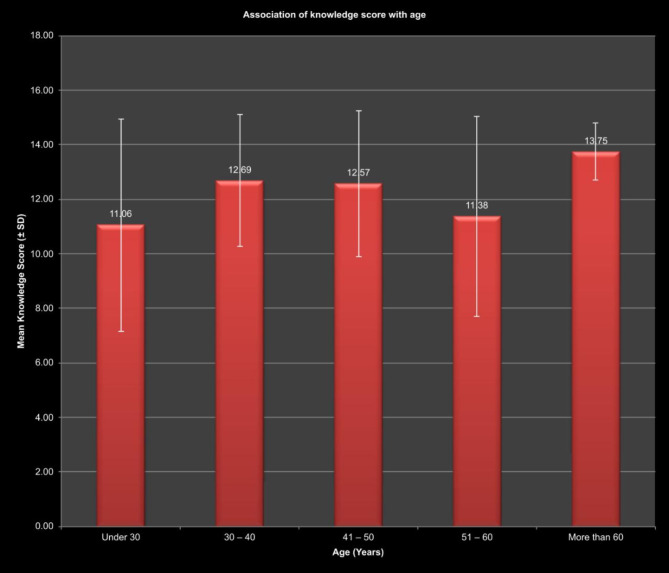
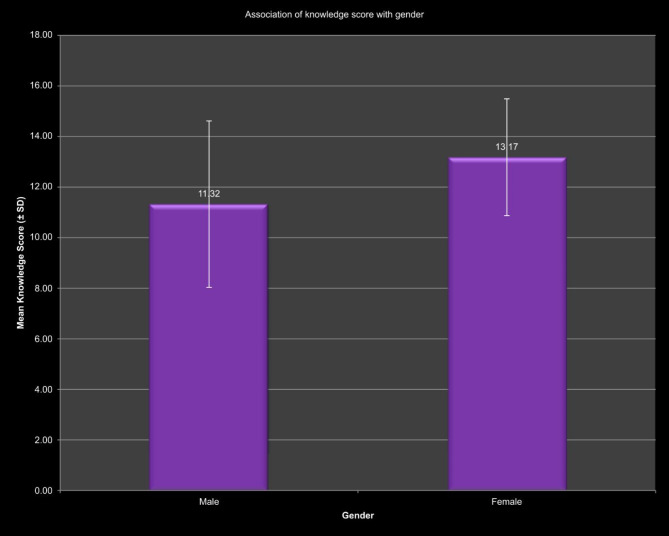
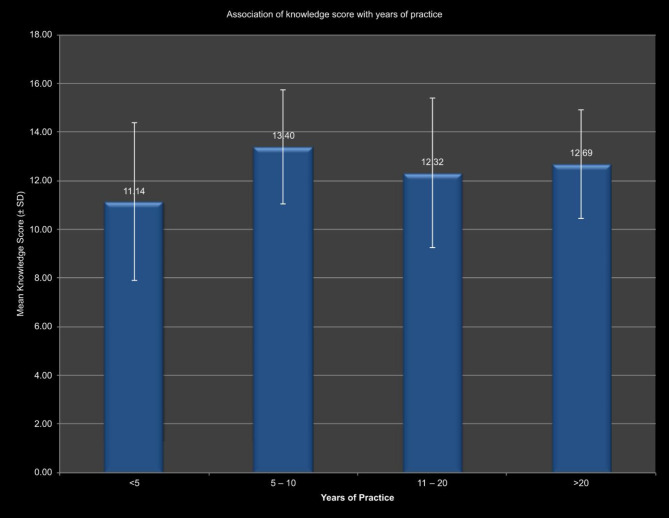
The mean ± SD and median with inter-quartile range (IQR) of the overall knowledge score were 12.23 ± 0.93 and 13 (11–15), ranging from 3 to 18. Table 2 presents the overall knowledge score by different grouping factors: age groups, gender, and years of experience. Those who aged older than 60 years revealed better knowledge (13.75 ± 1.04) than those under 30 years did (11.06 ± 3.89; P = 0.024). Statistically, the other comparisons by age group were not different. Gender-wise, females revealed better knowledge than males (13.75 ± 1.04 and 11.32 ± 3.28, respectively; P < 0.001). The overall knowledge scores for those who had 5 to 10 years of experience (13.40 ± 2.34) and those with more than 20 years of experience (12.69 ± 2.22) were higher than the scores of those with less than 5 years of experience (11.14 ± 3.23; P = 0.002).
Table 2.
Differences in knowledge score by age, gender, and years of practice
| Age (Years) | N | Mean Knowledge Score | ± SD | Minimum | Maximum | P value |
|---|---|---|---|---|---|---|
| Under 30ǂ | 34 | 11.06a | 3.892 | 3 | 17 | p = 0.024 |
| 30–40 | 52 | 12.69a, c | 2.422 | 8 | 16 | |
| 41–50 | 104 | 12.57a, c | 2.683 | 7 | 18 | |
| 51–60 | 13 | 11.38a, c | 3.664 | 7 | 18 | |
| More than 60 | 8 | 13.75b, c | 1.035 | 13 | 15 | |
| Gender£ | ||||||
| Male | 96 | 11.32 | 3.282 | 3 | 18 | p < 0.001 |
| Female | 115 | 13.17 | 2.302 | 7 | 18 | |
| Years of Practiceǂ | ||||||
| < 5 | 49 | 11.14a | 3.234 | 4 | 17 | p = 0.002 |
| 5–10 | 43 | 13.40b | 2.342 | 3 | 16 | |
| 11–20 | 84 | 12.32a, b | 3.070 | 7 | 18 | |
| > 20 | 35 | 12.69b | 2.220 | 9 | 18 | |
Table 2 shows the differences in knowledge scores across age, gender, and years of practice among dental professionals. Statistically significant variations were observed in the mean knowledge scores by age group (p = 0.024). ǂ: One-Way ANOVA Test Mean scores with different superscript small letters are statistically different upon pairwise comparisons using the post-hoc Tukey test. £: Independent t-test
Figure 3 well represents the association between age and mean knowledge scores among dental professionals. ANOVA analysis indicates significant differences in knowledge scores across age groups. The highest mean score was observed in the 60 + age group, while the lowest was in the under-30 age group.
Fig. 3.
Association of knowledge score and the age of the participants
The association between gender and mean knowledge scores is demonstrated in Fig. 4. ANOVA analysis reveals a significant difference in knowledge scores between males and females, with females demonstrating statistically significantly higher knowledge scores than males.
Fig. 4.
Association between gender and knowledge scores of dental professionals
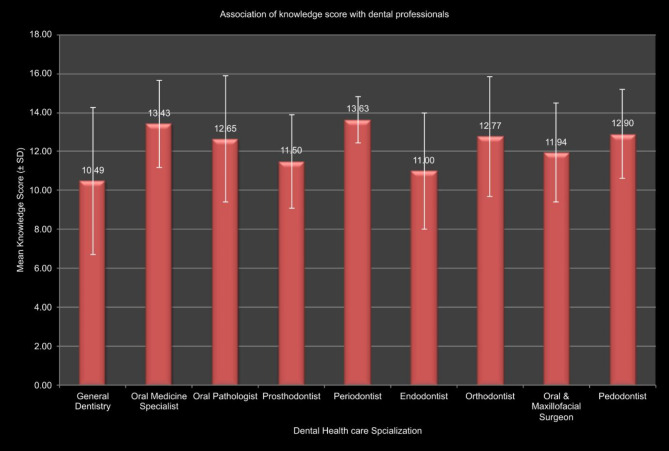
The association between knowledge scores and dental health care specialization revealed significant differences (ANOVA: F = 4.462, p < 0.001). Periodontists and Oral Medicine Specialists had the highest mean knowledge scores (13.63 ± 1.165 and 13.43 ± 2.239, respectively). In contrast, General Dentists had the lowest mean score (10.49 ± 3.768). Other specializations, such as Oral Pathologists (12.65 ± 3.220) and Orthodontists (12.77 ± 3.085), showed intermediate scores.
Figure 5 illustrates the association between knowledge scores and dental healthcare specialization. ANOVA results indicate a significant difference in knowledge scores across specialities (F = 4.462, p < 0.001). Post-hoc Tukey analysis shows that General Dentistry practitioners had significantly lower knowledge scores compared to Oral Medicine Specialists and Periodontists. Other speciality groups did not show significant differences in knowledge scores.
Fig. 5.
Association of knowledge score with dental health care
Figure 6 displays the association between knowledge scores and years of practice. ANOVA results indicate a significant association (F = 5.016, p = 0.002). Post-hoc Tukey analysis reveals that participants with less than 5 years of practice had significantly lower knowledge scores than those with 5–10 years and more than 20 years of practice. No significant differences were observed between other groups.
Fig. 6.
Association between years of practice and knowledge scores among dental professionals
Discussion
This study, the first of its kind in Saudi Arabia as up to our knowledge, showed intermediate to very good levels of knowledge of dental practitioners on the potential associations between nutrition and oral health. The study unveiled gender-, speciality-, and years-of-experience-wise differences. Both together substantiate the need to bridge such gaps in knowledge with great emphasis on focusing on the subgroups with lower levels of knowledge, namely, males, general dental practitioners, and those with shorter experience.
Our study encapsulated a broad spectrum of expertise from general dental practitioners to specialists like Oral Medicine Specialists, Prosthodontists, and more. Furthermore, the distribution of years of practice, with notable representation from early-career to seasoned practitioners, adds a temporal dimension to our exploration. This diversity ensures a holistic understanding of the potential association between nutrition and oral health across the professional continuum. The findings revealed significant associations between knowledge scores and various demographic factors.
Gender-based disparities were evident, with female practitioners demonstrating significantly higher knowledge scores than their male counterparts. These results align with studies conducted among college athletes in Iran [13], the USA [14], and Nigeria [15], which found higher knowledge of nutrition among females compared to their male counterparts. However, prior research conducted in Edo state, Nigeria [16], and the Philippines [17] revealed contrasting findings. Meanwhile, other previous studies [18, 19] reported similar levels of knowledge among males and females. Regarding our results, the discrepancy may be ascribed to the females’ innate tendency to be more mindful of their health and body than males.
Regarding age and years of experience, respondents aged under 30 years had a significantly lower overall knowledge score compared to those over 60 years. Our results in this context align with the previous research that demonstrated a notable correlation between age groups and knowledge and even the total KAP (knowledge, attitude and practice) scores. In one study, the older nurses demonstrated higher knowledge scores [20]. In contrast, in a multicenter study conducted in Palestine, younger participants displayed higher scores than the older ones. Conversely, the total clinical nutrition knowledge score did not show any notable variation based on the years of experience and practice of healthcare providers (p = 0.827) [21], which aligns with previous research findings [22, 23]. This supports the notion that education surpasses clinical experience in nutrition care.
The present study discerned significant variations in knowledge scores among diverse dental healthcare specialisations. Oral Medicine Specialists and Periodontists exhibited notably higher mean knowledge scores. These elevated scores underscore an advanced understanding of the correlation between diet, nutrition, and oral health within these specialised fields. In contrast, general dental practitioners displayed a lower mean knowledge score, highlighting potential areas for improvement in comprehending the nuances of dietary influences on oral health. A previous study among nutrition/dietetics students reported a higher mean knowledge score, indicating potential differences in educational backgrounds and focuses between students and established professionals [24]. Another survey among dental students highlighted variations in nutritional knowledge, being better among postgraduate students [18]. Additionally, a noteworthy correlation was observed between the respondents’ speciality and their practice and the overall KAP score. The practical and staff nurses scored higher than the physicians [21]. This aligns with our findings, emphasising the importance of tailored educational interventions based on professionals’ specialisations.
In Ireland and the UK, 18% of dietitians, compared to 56% of dentists, considered that they had received sufficient diet and dental health training; both professions indicated the need for multi-disciplinary training [25]. Another fascinating study compared the nutritional knowledge of nutrition, dietetics, and dentistry students, highlighting conflicts in dietary recommendations and identifying differences in nutritional knowledge among dental, dietetic, and nutrition students. However, the emphasis on specific concerns differs: dental students prioritise oral health issues like acid erosion, while dietetic and nutrition students focus more on general health problems such as obesity [26].
Furthermore, the studies on dental students emphasise the importance of nutritional education for dental students [15, 19, 26, 27], signalling room for focused education to enhance their understanding of diet and nutrition in oral health. The findings from our research contribute unique perspectives to the current corpus of literature. The diversity of dental practitioners, their specialisations, and the intricate facets of nutritional knowledge explored in our study emphasises the need for tailored educational interventions and further research to bridge gaps in understanding across the dental profession.
The knowledge on the role of calcium in alveolar bone density, the positive impact of Vitamin C-rich foods on gingival inflammation, and the link between high-glycemic foods and the increased risk of periodontal inflammation and dental caries was impressive. Simply, this reflects a deep-rooted knowledge about well-established facts by which literature is saturated and learnt repeatedly in successive levels of undergraduate and postgraduate studies [28, 29]. Similarly, a high fraction of the participants (78.3%) reported sucrose as the most cariogenic sugar [27], almost similar to the results obtained by da Costa et al., where 82.3% of their participants reported sucrose as the most cariogenic sugar [19].
Contrastingly, 96.1% of the participants in our study reflected poor knowledge regarding the relative cariogenicity of extrinsic sugars compared to intrinsic sugars, like the results of Bapat et al. [24]. In line with that, only 29% of the respondents reported that individuals who follow a vegetarian diet exhibit healthier gums and superior oral hygiene compared to non-vegetarians; 52.6% and 18% responded with “NO” or I don’t know, respectively. As per Staufenbiel’s study, vegetarians exhibited notably reduced probing pocket depths, bleeding on probing, periodontal screening index, a superior hygiene index, and fewer mobile teeth [30]. Similarly, in another study on raw vegans exhibited significantly improved oral hygiene compared to other groups (P = 0.001). The measurements of probing depth, bleeding on probing, and simplified oral hygiene index were notably lower in individuals following a raw vegan diet [31]. However, the link between vegetarianism and good periodontal health might be at the expense of the health of hard dental structures; Laffranchi et al. found a higher prevalence of demineralisation and white spots in the vegan participants compared to the omnivorous group [32]. Iwasaki et al. conducted a longitudinal study involving 264 Japanese participants, which revealed a statistically significant positive correlation between saturated fatty acids and the occurrence of periodontal lesions [33]. Omega-3 fatty acids have received considerable attention recently due to their correlation with reduced systemic inflammation [34]. Multiple studies have demonstrated that inflammation is primarily stimulated by detrimental saturated fats, such as trans fats and omega-6 fatty acids [6, 35, 36]. To summarise, this study’s and other studies’ evidence emphasises the importance of dietary fats in maintaining good periodontal health. Unhealthy saturated fats and trans fats can worsen inflammation, while omega-3 fatty acids have a protective effect. This emphasises the significance of dietary decisions in managing periodontal inflammation.
This study offers significant insights into dental professionals’ diet and oral health knowledge; it is essential to acknowledge certain limitations that may have influenced the results. One potential limitation of this study was the reliance on a self-reported questionnaire, which is less sensitive in obtaining objective data and implies a potential for social desirability and recall biases. In addition, this type of study design (cross-sectional) is classified as a low-level-evidence approach. Another limitation was the convenience sampling method as the participants were recruited through online social media platforms. This may have resulted in a sampling bias via inducing overrepresentation of certain demographic groups or dental specialisations, potentially limiting the generalizability of the findings. A further limitation was the potential presence of confounders like participants’ educational backgrounds, cultural beliefs, and access to continuing education opportunities. Keeping these limitations in mind, the results of this study must be interpreted cautiously, with special emphasis given to their generalizability.
Conclusion
The present study assessed Saudi Arabian dental practitioners’ knowledge of the relationship between nutrition and oral health. The findings revealed variations in knowledge levels, with females, oral medicine and periodontology specialists, and practitioners with more years of experience scoring higher. However, knowledge gaps persist, particularly among general dentists and those early in their careers. These results highlight the need for targeted educational interventions and incorporating nutrition-related content into dental education curricula to enhance knowledge and improve patient care. A visual summary highlighting the study’s key findings, including the association between diet and oral health knowledge among dental professionals in Saudi Arabia, emphasising the influence of gender, age, specialization, and years of experience, is provided in Fig. 7.
Fig. 7.
A visual summary of key findings on diet and oral health knowledge among Saudi dental professionals, emphasizing the influence of gender, age, specialization, and experience
Future research directions
To address the identified knowledge gaps, future studies should explore developing and implementing targeted educational interventions tailored to the unique needs of dental practitioners. Incorporating consistent nutrition guidelines into dental education curricula can play a pivotal role in enhancing practitioners’ understanding of the relationship between diet and oral health. Further research could investigate interdisciplinary collaboration among dental professionals, nutritionists, and public health experts to foster a more integrated oral health care delivery approach. This collaboration can potentially improve patient outcomes through holistic and evidence-based care. Additionally, studies should focus on designing and evaluating continuous professional development programs that provide ongoing training on the latest advancements in oral health and nutrition. Such initiatives can ensure practitioners remain updated and equipped to deliver high-quality, patient-centred care. Expanding future research to assess knowledge levels across other healthcare disciplines may also provide valuable insights into the broader impact of nutrition education on interdisciplinary healthcare delivery and community health outcomes.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
The authors gratefully acknowledge the funding of the Deanship of Graduate Studies and Scientific Research, Jazan University, Saudi Arabia, through Project Number GSSRD-24. The authors also express their sincere gratitude to Dr Essam Halboub for validating the questionnaire for the present study.
Author contributions
“Conceptualization and Methodology, S.P., Data curation, R.S.P., S.S.K., H.A.; Formal analysis, S.A.A., H.E.H; Investigation, O.Y.D., A.A.A., A.Y.O., Methodology, S.P., Project administration, S.P., M.B., S.A.A., Resources, N.H.H.E., Software; O.Y.D., S.A.A Supervision, S.P. R.S.P., original draft; S.P., and Writing - review & editing all co-authors.”
Funding
None.
Data availability
“Data is provided as supplementary information.”
Declarations
Ethics approval and consent to participate
The Jazan University Standing Committee on the Ethics of Scientific Research (REC-45/05/895, HAPO-10-Z-001) approved the study, ensuring ethical guidelines were followed. Informed consent was obtained from all participants before the study began, and the study complied with the principles established in the Helsinki Declaration.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Touger-Decker R, Mobley CC, American Dietetic Association. Position of the American Dietetic Association: oral health and nutrition. J Am Diet Assoc. 2003;103:615–25. [DOI] [PubMed] [Google Scholar]
- 2.Sheetal A, Hiremath VK, Patil AG, Sajjansetty S, Kumar SR. Malnutrition and its oral outcome – a review. J Clin Diagn Res. 2013;7:178–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baiju R, Peter E, Varghese N, Sivaram R. Oral health and quality of life: current concepts. J Clin Diagn Res. 2017;11:ZE21–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tinanoff N, Palmer CA. Dietary determinants of dental caries and dietary recommendations for preschool children. J Public Health Dent. 2000;60:197–206. discussion 207–209. [DOI] [PubMed] [Google Scholar]
- 5.Tungare S, Paranjpe AG. In: StatPearls, editor. Diet and Nutrition to Prevent Dental problems. Treasure Island (FL): StatPearls Publishing; 2023. [PubMed] [Google Scholar]
- 6.Santonocito S, Polizzi A, Palazzo G, Indelicato F, Isola G. Dietary factors affecting the prevalence and impact of Periodontal Disease. Clin Cosmet Investig Dent. 2021;13:283–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alhazmi YA, Parveen S, Alfaifi WH, Najmi NM, Namazi SA, Abuzawah LH, et al. Assessment of Knowledge, attitude and practice of Diabetic patients towards oral health: a cross-sectional study. World J Dentistry. 2022;13:239–44. [Google Scholar]
- 8.Branch-Mays GL, Dawson DR, Gunsolley JC, Reynolds MA, Ebersole JL, Novak KF, et al. The effects of a calorie-reduced diet on periodontal inflammation and disease in a non-human primate model. J Periodontol. 2008;79:1184–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Najeeb S, Zafar MS, Khurshid Z, Zohaib S, Almas K. The role of Nutrition in Periodontal Health: an update. Nutrients. 2016;8:530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parveen S. Impact of calorie restriction and intermittent fasting on periodontal health. Periodontol 2000. 2021;87:315–24. [DOI] [PubMed] [Google Scholar]
- 11.Hujoel P. Dietary carbohydrates and dental-systemic diseases. J Dent Res. 2009;88:490–502. [DOI] [PubMed] [Google Scholar]
- 12.Li X, Wen M, Liu H, Shen Y, Su L, Yang X. Dietary magnesium intake is protective in patients with periodontitis. Front Nutr. 2022;9:976518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jessri M, Jessri M, RashidKhani B, Zinn C. Evaluation of Iranian college athletes’ sport nutrition knowledge. Int J Sport Nutr Exerc Metab. 2010;20:257–63. [DOI] [PubMed] [Google Scholar]
- 14.Yahia N, Brown CA, Rapley M, Chung M. Level of nutrition knowledge and its association with fat consumption among college students. BMC Public Health. 2016;16:1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elizabeth A, Mosuro A, Adeniyi B, Ogundele A, Akinrefe O, Bodunde I et al. Assessment of Nutritional Knowledge, Dietary Habits and Oral Health Practices of Undergraduate Students in Lead City University Ibadan. 2023;11:11–7.
- 16.Vocational, Department T, Faculty of Education, Ambrose Alli University, Ekpoma, Edo State, Aluyor N, Oligbi P. E, Department of Home Economics, College of Education, Igueben, Edo State, Nigeria. An assessment on the level of nutritional knowledge among undergraduate students in Edo state. Res J Food Sci Nutr. 2020;5:53–7.
- 17.Montecalbo RC, Cardenas RC. Nutritional Knowledge and Dietary habits of Philippine Collegiate athletes. Int J Sports Sci. 2015;5:45–50. [Google Scholar]
- 18.Chalmuri Y, Padma TM, Pratap KVNR, Vineela P, Varma LSC, Vidyasagar Y. Do the Dental students have enough nutritional knowledge? A Survey among students of a Dental College in Telangana State. J Indian Association Public Health Dentistry. 2018;16:38. [Google Scholar]
- 19.da Costa FD, Prashant GM, Sushanth VH, Imranulla M, Prabhu A, Kulkarni SS. Assessment of knowledge, attitude and practices of diet and nutrition on oral health among dental students. JGOH. 2019;2:29–35. [Google Scholar]
- 20.Schaller C, James EL. The nutritional knowledge of Australian nurses. Nurse Educ Today. 2005;25:405–12. [DOI] [PubMed] [Google Scholar]
- 21.Shakhshir M, Alkaiyat A. Healthcare providers’ knowledge, attitude, and practice on quality of nutrition care in hospitals from a developing country: a multicenter experience. J Health Popul Nutr. 2023;42:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Crogan NL, Evans BC. Nutrition assessment: experience is not a predictor of knowledge. J Contin Educ Nurs. 2001;32:219–22. [DOI] [PubMed] [Google Scholar]
- 23.Laur C, Marcus H, Ray S, Keller H. Quality Nutrition Care: Measuring Hospital Staff’s knowledge, attitudes, and practices. Healthc (Basel). 2016;4:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bapat S, Asawa K, Bhat N, Tak M, Gupta VV, Chaturvedi P, et al. Assessment of Dental Nutrition Knowledge among Nutrition/Dietetics Students. J Clin Diagn Res. 2016;10:ZC37–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kingsnorth J, Cushen SJ, Janiszewska K, Avery A. Health professionals’ knowledge, views and advice on diet and dental health: a survey of UK and Ireland dietitians and dentists. J Hum Nutr Diet. 2021;34:705–14. [DOI] [PubMed] [Google Scholar]
- 26.Shah K, Hunter ML, Fairchild RM, Morgan MZ. A comparison of the nutritional knowledge of dental, dietetic and nutrition students. Br Dent J. 2011;210:33–8. [DOI] [PubMed] [Google Scholar]
- 27.Abdullah. Assessment of dental nutrition knowledge among dental students in Chennai. https://www.ijcommdent.com/article.asp?issn=2589-8388;year=2021;volume=9;issue=1;spage=24;epage=28;aulast=Abdullah. Accessed 18 Jan 2024.
- 28.Tanaka K, Miyake Y, Okubo H, Hanioka T, Sasaki S, Miyatake N, et al. Calcium intake is associated with decreased prevalence of periodontal disease in young Japanese women. Nutr J. 2014;13:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Murererehe J, Uwitonze AM, Nikuze P, Patel J, Razzaque MS. Beneficial Effects of Vitamin C in maintaining optimal oral health. Front Nutr. 2022;8:805809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Staufenbiel I, Weinspach K, Förster G, Geurtsen W, Günay H. Periodontal conditions in vegetarians: a clinical study. Eur J Clin Nutr. 2013;67:836–40. [DOI] [PubMed] [Google Scholar]
- 31.Atarbashi-Moghadam F, Moallemi-Pour S, Atarbashi-Moghadam S, Sijanivandi S, Baghban AA. Effects of raw vegan diet on periodontal and dental parameters. Tzu Chi Med J. 2020;32:357–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laffranchi L, Zotti F, Bonetti S, Dalessandri D, Fontana P. Oral implications of the vegan diet: observational study. Minerva Stomatol. 2010;59:583–91. [PubMed] [Google Scholar]
- 33.Iwasaki M, Manz MC, Moynihan P, Yoshihara A, Muramatsu K, Watanabe R, et al. Relationship between saturated fatty acids and periodontal disease. J Dent Res. 2011;90:861–7. [DOI] [PubMed] [Google Scholar]
- 34.Serhan CN. Treating inflammation and infection in the 21st century: new hints from decoding resolution mediators and mechanisms. FASEB J. 2017;31:1273–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vach K, Al-Ahmad A, Anderson A, Woelber JP, Karygianni L, Wittmer A, et al. Analysing the relationship between Nutrition and the Microbial composition of the oral biofilm-insights from the analysis of individual variability. Antibiot (Basel). 2020;9:479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Parveen S, Alhazmi YA. Impact of intermittent fasting on metabolic syndrome and Periodontal Disease-A suggested preventive strategy to reduce the Public Health Burden. Int J Environ Res Public Health. 2022;19:14536. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
“Data is provided as supplementary information.”