Abstract
Purpose
The suprascapular nerve is situated between the prevertebral fascia and the superficial layer of deep cervical fascia and on the surface of the middle and posterior scalene muscles before it reaches the suprascapular notch. Consequently, we hypothesized that injecting local anesthetics (LAs) there would introduce a new block approach for blocking the suprascapular nerve, ie, extra-prevertebral fascial block. We assessed the postoperative analgesic effect, as well as the incidence of diaphragmatic paralysis 30 minutes after the block.
Methods
30 patients undergoing elective shoulder arthroscopic rotator cuff repair surgery were recruited in this study. Before the induction of general anesthesia, 15 mL of 0.5% ropivacaine was administered to perform an extra-prevertebral fascia suprascapular nerve block (10 mL) and an infraclavicular brachial plexus block (5 mL, primarily targeting the axillary nerve). All patients received intravenous patient-controlled analgesia (PCA) after surgery. The postoperative pain was scored with Numeric Rating Scale (NRS), along with the opioid consumption in the first 24 h after surgery. The incidence of hemi-diaphragmatic paralysis (HDP) was measured 30 minutes after the block.
Results
All patients received the successful block. The resting NRS pain scores at 1h, 6h, 12h, and 24h postoperatively were 0 [0, 2], 0 [0, 2], 1 [0, 2], and 2 [1, 3], respectively. The oral morphine equivalent (OME) consumption at 24 hours after surgery was 18 [12,30] mg. No patients experienced HDP (complete or partial) 30 minutes after the block.
Conclusion
Compared with the posterior approach, this novel technique is efficient and has a higher success rate of blockade. It eliminates the need for patients to change positions, thereby improving comfort. Additionally, when combined with the infraclavicular brachial plexus block, it can effectively block the suprascapular nerve, providing satisfactory postoperative analgesia without the HDP at 30min after blockade compared to the anterior approach.
Keywords: suprascapular nerve block, ultrasound, diaphragm, prevertebral fascia
Introduction
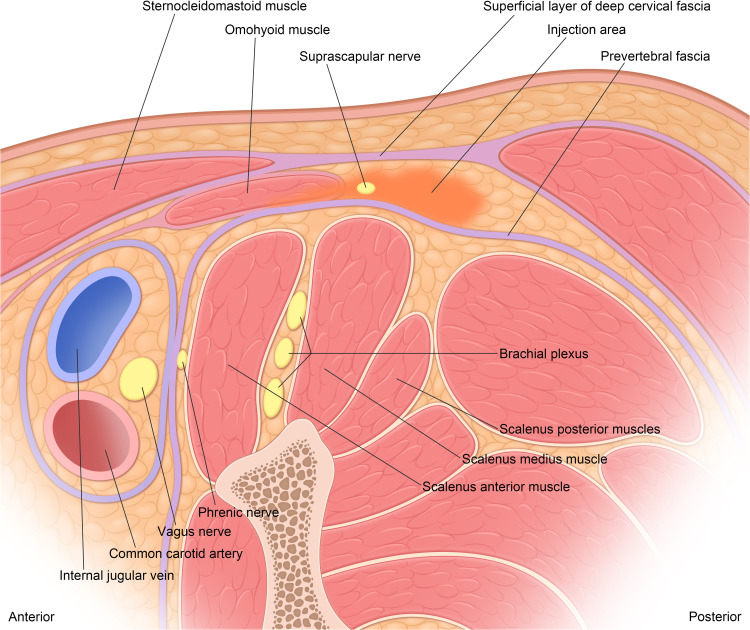
Shoulder arthroscopic surgeries offer several advantages, including reduced trauma, rapid recovery, and a low infection rate.1 Nevertheless, the procedures are associated with significant postoperative pain and effective analgesia is essential.2 The interscalene block (ISB) has been considered the gold standard for postoperative pain management in shoulder surgery.3 Patients who receive the ISB typically require fewer opioids postoperatively and tend to recover faster.4 Unfortunately, some studies have reported an incidence of phrenic nerve palsy as high as 100%.5 This condition can lead to dyspnea and reduced oxygen saturation which may be problematic for healthy patients and can pose significant risks for those with underlying pulmonary diseases. The suprascapular and axillary nerves are responsible for innervating most sensory functions of the glenohumeral joint.6 Therefore, the combined suprascapular and the infraclavicular brachial plexus block (mainly targeting the posterior cords, thereby anesthetizing the axillary nerve) may serve as an effective alternative to the ISB.3 Based on previous anatomical studies related to the shoulder joint,7 we found that the suprascapular nerve originates from the upper trunk of the brachial plexus and traveled posteriorly and laterally within the intermediate space between the superficial layer of deep cervical fascia of the omohyoid muscle and the prevertebral fascia before entering the suprascapular notch. This fascial plane is situated far from the phrenic nerve and could be visualized in sonographic imaging, potentially providing an avenue for suprascapular nerve block, which we refer to as the extra-prevertebral fascial approach.
We aimed to evaluate the postoperative analgesic efficacy of the extra-prevertebral fascial suprascapular nerve block in combination with the infraclavicular brachial plexus block. Additionally, we assessed the impact on the incidence of hemi-diaphragmatic paralysis (HDP), which was diagnosed via ultrasound 30 minutes after the administration of these blocks for arthroscopic shoulder surgery.
Methods
The Ethics Committee of Beijing Friendship Hospital, Capital Medical University, China, approved the study protocol on April 1, 2024, under the reference number 2024-P2-088-01. The study was registered at the Chinese Clinical Trial Registry on April 19, 2024, with the registration number ChiCTR2400083270. The study adhered to the Consolidated Standards of Reporting Trials (CONSORT) statement and the principles outlined in the Helsinki Declaration.
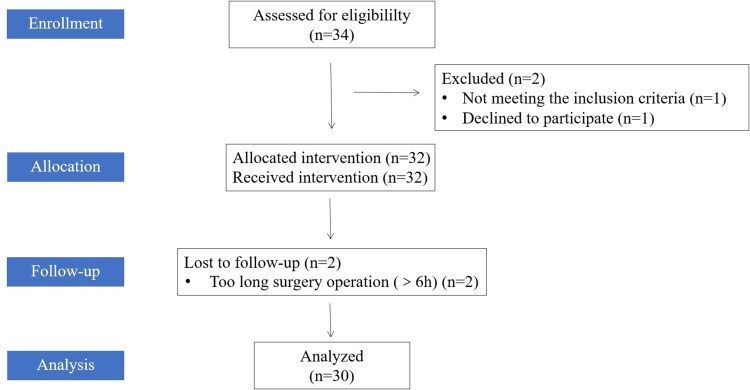
All patients in the study gave written informed consent (Figure 1). The inclusion criteria were as follows: American Society of Anesthesiologists (ASA) physical status I–III, body mass index (BMI) 18–30 kg /m2, age 18–70 years old. The exclusion criteria included allergy to medications used in the standardized anesthesia regimen, local or systemic infections, pregnancy, and the inability to complete pain assessments for any reason. Patient demographics, including gender, age, BMI, ASA classification, and any pre-existing conditions, were recorded. A total of 30 patients scheduled for elective shoulder arthroscopic rotator cuff repair were recruited from April 20, 2024, to June 30, 2024, at Beijing Friendship Hospital of Capital Medical University in Beijing, China.
Figure 1.
CONSORT study flow diagram.
Abbreviations: CONSORT, Consolidated Standards of Reporting Trials.
Nerve Blocks
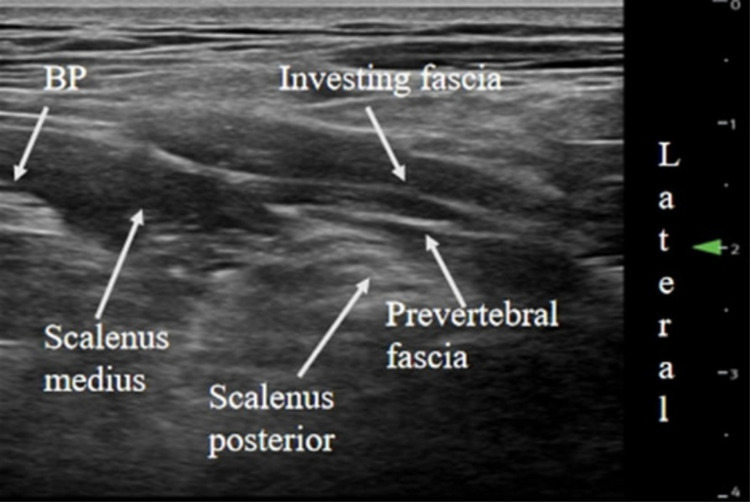
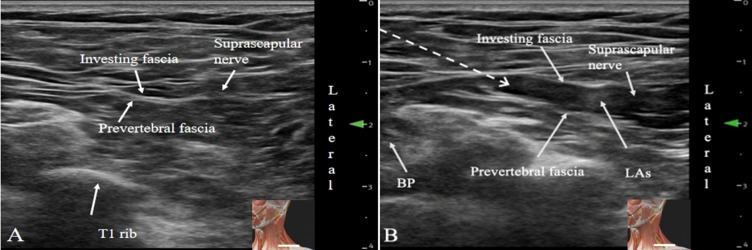
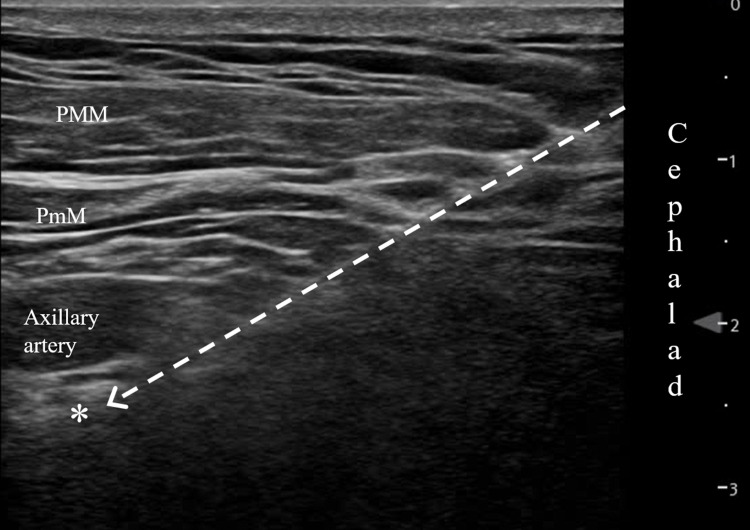
For all patients, standard vital sign monitors were placed, and oxygen was delivered through a facemask. Intravenous access was established contralateral to the surgical site. An anesthesiologist experienced in ultrasound imaging and interventional injections conducted the nerve blocks. A combined suprascapular and infraclavicular brachial plexus block was performed prior to the induction of general anesthesia. Additionally, 1–2 mg of midazolam and 5 μg of sufentanil were administered appropriately before the block. With the patients in the supine position, a high-frequency linear ultrasound probe (L12-3RCs, 3–12 MHz frequency, Mindray, Shenzhen, China) was positioned on the side of the neck in a transverse plane to visualize the brachial plexus. The probe was then moved distally and laterally to the supraclavicular region to track the middle and posterior scalene muscles. The ultrasound image displayed the middle and posterior scalene muscles, the brachial plexus, and the omohyoid muscle (which was sometimes not visible) (Figure 2). The LAs (10 mL of 0.5% ropivacaine) were injected above the prevertebral fascia covering the middle and posterior scalene muscles using an in-plane technique with a medial-to-lateral direction. The LAs diffused laterally, following the same trajectory as the suprascapular nerve (Figure 3). Subsequently, the infraclavicular brachial plexus block was performed according to a previously described technique.8 The transducer was positioned in the lateral infraclavicular fossa, medially to the coracoid process, to obtain a short-axis view of the axillary artery. By employing an in-plane technique with a cephalad-to-caudad direction, the block needle was advanced until its tip was positioned dorsal to the axillary artery (Figure 4). A total of 5 mL of 0.5% ropivacaine was injected into this site.
Figure 2.
Relationship of the scalenus medius, scalenus posterior, prevertebral fascia, and the superficial layer of deep cervical fascia.
Abbreviations: BP, brachial plexus.
Figure 3.
Changes before and after ultrasound-guided extra-prevertebral fascial block. (A) before the block; (B) after the block. The dashed arrow line shows the needle path.
Abbreviations: BP, brachial plexus; LAs, local anesthetics. The embedded graph shows the site of the probe.
Figure 4.
Paracoracoid infraclavicular brachial plexus block. The dashed arrow line shows the needle path. *Target for local anesthetic injection.
Abbreviations: PMM, pectoralis major muscle; PmM, pectoralis minor muscle.
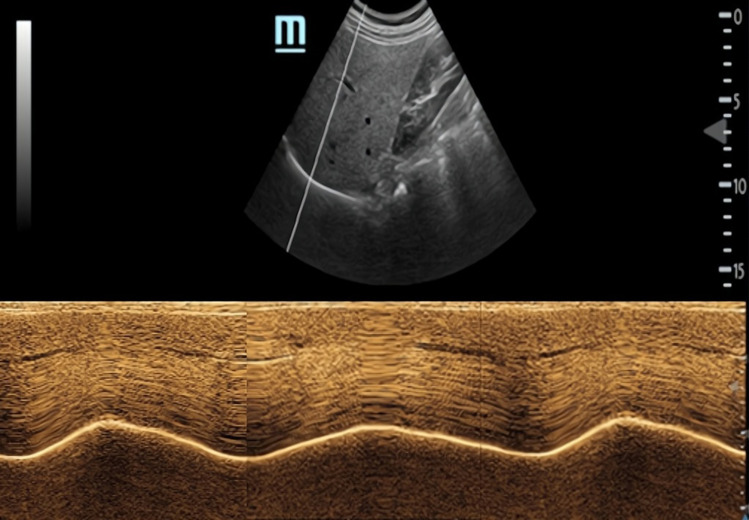
Assessment of Block Efficacy and Diaphragmatic Movement
The efficacy of our combined blocks was evaluated 30 minutes after injection of LAs. The top of the shoulder (axillary nerve) and the posterior surface of the scapula (suprascapular nerve) were tested for cold sensitivity, respectively.9,10 Sensory block was graded using a three-point scale: 0 = no block; 1 = partial block (patient can feel touch); and 2 = complete loss of cold sensation.10 Diaphragmatic excursion was assessed using ultrasound both at baseline and 30 minutes after block in all patients, conducted by a single anesthesiologist experienced in the technique. The function of the diaphragm was evaluated through ultrasonography employing previously described techniques.11,12 A curvilinear probe (C5-2a, 2–5 MHz frequency, Mindray, Shenzhen, China) was positioned beneath the costal margin, between the anterior axillary and the mid-clavicular lines, with the probe oriented cephalically to visualize the posterior third of the hemidiaphragm. The liver or the spleen served as acoustic windows. The ultrasound was set to motion mode, allowing the diaphragm to appear as a white hyperechoic line that undulated during the respiratory cycle. Diaphragmatic movement, defined as a cranio-caudal movement of the diaphragm, was measured in centimeters during a voluntary “sniff test”. The amplitude of three respiratory cycles was recorded, and the average value was calculated (Figure 5). The incidence of HDP was defined as a reduction of ≥25% in diaphragmatic excursion as measured by ultrasound. Complete diaphragmatic paralysis was defined as a reduction in diaphragmatic shift of ≥75% from baseline, or by paradoxical movement of the diaphragm. Partial diaphragmatic paralysis was defined as a 25–75% reduction in diaphragmatic excursion.13
Figure 5.
Curvilinear transducer ultrasound image of the right diaphragm using the liver as an acoustic window in two-dimensional B-mode (above) and M-mode (below).
General Anesthesia Regimen and Postoperative Analgesia
Regardless of whether the block failed or not, all patients received a standardized anesthetic protocol. Propofol (1.5–2.5 mg/kg), sufentanil (0.15 μg/kg) and rocuronium bromide (0.9 mg/kg) were administered intravenously to induce general anesthesia, followed by tracheal intubation and mechanical ventilation. Anesthesia was maintained with a continuous intravenous infusion of propofol (0.12–0.15 mg/kg/min), BIS 40–60, and remifentanil (0.15–0.3 μg/kg/min) was pumped as needed. Flurbiprofen (50 mg) and tropisetron (5 mg) were given intravenously for postoperative pain control and prevention of nausea at the end of surgery. After extubation, all patients were transferred to the anesthesia recovery room. In the recovery room, the subjects received an intravenous PCA system containing 1 μg/mL of sufentanil. The system was programmed to deliver a 2 mL intravenous bolus on demand, with a 15-minute lockout interval. All patients were given preoperative instructions regarding the intravenous PCA system and the pain severity scale, where 0 was defined as “no pain” and 10 as “worst pain”. When the NRS was >4, rescue analgesia was provided by administering tramadol at a dose of 0.1 g intravenously. At 1, 6, 12, and 24 hours postoperatively, an anesthesia nurse, who was blinded to the study, recorded pain intensity at rest using NRS. Patient satisfaction with analgesia at 24 hours was evaluated by using a detailed Likert scale, where 1 = very dissatisfied, 2 = dissatisfied, 3 = neutral, 4 = satisfied, and 5 = very satisfied.14
Demographic data, including age, gender, ASA score, duration of surgery, and intraoperative remifentanil consumption were recorded. The primary outcome was OMEs on postoperative day 1, and the second outcomes were NRS scores, time of first pain medication for shoulder pain, rescue analgesia, the incidence of HDP, and patient satisfaction score. Additionally, possible adverse events, such as nausea-vomiting, pruritus, dyspnea, and complications related to block were documented.
Statistical Analysis
Since this was a pilot study, the sample size was determined empirically. Previous literature indicated that a sample size of 10 to 40 was appropriate.15 In this study, the sample size was initially set at 25 patients. But was later adjusted to 30 taking into account a 10% dropout rate. Continuous variables were represented as mean ± standard deviation (SD) for normal distribution, while median and interquartile range (IQR) were presented for those not subject to normal distribution. Categorical variables were presented as numbers and percentages. The normality of data distribution was identified by the Kolmogorov–Smirnov test. Statistical analysis was conducted using SPSS software (version 24.0, IBM Corporation, Armonk, NY, USA).
Results
From April 19, 2024, to June 30, 2024, a total of 34 patients scheduled for arthroscopic shoulder surgery were assessed for eligibility. One patient was excluded for not meeting the inclusion criteria, and another patient declined to participate. Besides, two patients were excluded for prolonged surgery duration (greater than 6 hours) (Figure 1). Finally, 30 patients were recruited and the demographics and surgical details of the subjects are presented in Table 1.
Table 1.
Patient Characteristics
| Characteristic | Patients (n=30) |
|---|---|
| Age (years) | 59.0 ± 8.2 |
| Body mass index (kg/m2) | 24.6 ± 2.6 |
| Gender | |
| Male | 6 (20%) |
| Female | 24 (80%) |
| ASA PS | |
| I | 3 (10%) |
| II | 24 (80%) |
| III | 3 (10%) |
| Side of operation | |
| Right | 21 (70%) |
| Left | 9 (30%) |
| Length of surgery (min) | 109.2 ± 29.1 |
| Intraoperative remifentanil consumption (mcg) | 363.1 ± 177.4 |
Notes: Values are mean ± SD or number (proportion).
Abbreviation: ASA PS, American Society of Anesthesiologists Physical Status.
Block success was assessed after 30 minutes, and the results are presented in Table 2. We confirmed sensory abnormalities and numbness in the dermatomal areas of the suprascapular nerve (0 = 1 (3.3%); 1 = 6 (20.0%); 2 = 23 (76.7%)) and the axillary nerve (0 = 2 (6.7%); 1 = 2 (6.7%); 2 = 26 (86.6%)). No diaphragmatic paralysis was observed. The details of the blocks, including procedure time, success rates, and incidence of HDP are summarized in Table 2. The resting NRS pain scores at 1, 6, 12, and 24 hours postoperatively were 0 [0, 2], 0 [0, 2], 1 [0, 2], and 2 [1, 3], respectively. The amount of OMEs consumed 24 hours after surgery was 18 [12, 30] mg. The time (in hours) to the first opioid request of the PCA pump was 4 [1, 19]. The postoperative QoR-15 score at 24 hours was 135.8 ± 10.0. Patient satisfaction was rated at 4.7 ± 0.6. Two subjects experienced postoperative nausea and vomiting. No respiratory depression or LAs systemic toxicity was observed (Table 3).
Table 2.
Blocking Related Data
| Index | Patients (n=30) |
|---|---|
| Blocking operation time (min) | 6 [5.3,6.3] |
| Sensory assessment after block at 30 minutes | |
| Suprascapular nerve | |
| 0 | 1(3.3%) |
| 1 | 6(20.0%) |
| 2 | 23(76.7%) |
| Axillary nerve | |
| 0 | 2(6.7%) |
| 1 | 2(6.7%) |
| 2 | 26(86.6%) |
| Incidence of hemi-diaphragmatic paralysis at 30 minutes | |
| None | 30(100%) |
| Partial | 0 |
| Complete | 0 |
Notes: Sensory block was graded according to a three-point scale: 0 = no block; 1 = analgesia (patient can feel touch, not cold); 2 = anesthesia (patient cannot feel touch). Values are median [IQR] or number of patients.
Table 3.
Postoperative Outcomes
| Outcome | Patients (n=30) |
|---|---|
| Resting NRS score (0–10) | |
| 1h postoperative | 0 [0,2] |
| 6h postoperative | 0 [0,2] |
| 12h after surgery | 1 [0,2] |
| 24h after surgery | 2 [1,3] |
| Cumulative opioid consumption in the first 24h postoperatively (OMEs, mg) | 18 [12,30] |
| Proportion of rescue analgesia | 2 (6.7%) |
| Time to first analgesia (h) | 4 [1,19] |
| Patient satisfaction | 4.7 ± 0.6 |
| Adverse event rate at 24 hours | |
| Horner's syndrome | 0 |
| Swelling of soft tissue due to internal hemorrhage | 0 |
| Nausea and vomiting | 2 (6.7%) |
| Pruritus | 0 |
| Dyspnea | 0 |
| Excessive sedation | 0 |
| QoR-15 score | 135.8 ± 10.0 |
Notes: Values are means ± SD, median [IQR], or number of patients.
Abbreviations: NRS, numerical rating scale; IQR, interquartile range; OME, oral morphine equivalent; SD, standard deviation; QoR, quality of recovery.
Discussion
This prospective descriptive study demonstrated that suprascapular nerve block performed outside the prevertebral fascia (Figure 6), in combination with the infraclavicular brachial plexus block, provided effective analgesia and significantly reduced the incidence of HDP measured 30 minutes after the block.
Figure 6.
Relationship between the fascia compartment and the suprascapular nerve. Local anesthetic acts to block the suprascapular nerve by entering the fascia space between the prevertebral fascia and the superficial layer of deep cervical fascia, that is the extra-prevertebral fascial block.
ISB provides analgesia for shoulder surgery; however, it is associated with a high incidence of HDP. Consequently, the search for diaphragm-sparing nerve blocks for analgesia in shoulder surgeries is ongoing, with a combined suprascapular and axillary nerve block emerging as one of the most popular alternatives. The anterior approach for suprascapular nerve block is located in the supraclavicular region.16 Furthermore, there remains a risk of LAs diffusion to the phrenic nerve, with the incidence of HDP reported to be as high as 40%.9 Besides, the anatomical proximity of the suprascapular nerve to the brachial plexus in the supraclavicular fossa is noteworthy. In the study conducted by Siegenthaler et al, the distance from suprascapular nerve to plexus in the supraclavicular fossa was measured at 9 mm in volunteers and 8 mm in cadavers.16 It should be noted that a supraclavicular brachial plexus block may occur due to the spread of LAs following anterior suprascapular nerve block performed with high volumes. Moreover, there is no clinically-relevant dose at which HDP can be reliably avoided between local anesthetic volume and HDP after supraclavicular block, most likely due to the investment of the phrenic nerve and brachial plexus within the same prevertebral fascial sheath.17 The incidence of HDP observed 30 minutes after blocks in our study was lower than that reported in previous studies.18 This discrepancy may be attributed to the prevertebral fascia acting as a barrier, lower doses of LAs, and the medial-to-lateral approach, suggesting this block may help preserve the function of phrenic nerve. The posterior approach of suprascapular nerve can effectively reduce the incidence of HDP.11 However, the implementation is technically difficult and requires the patients’ position change, which the novel technique of suprascapular nerve block can optimize. Other measures such as subparaneural upper trunk block,19 low-dose LAs,20 or intravenous dexamethasone21 may help to reduce the incidence of HDP.
When the preservation of pulmonary function is critical, combined blocks would be a viable option to perform on a patient population (respiratory compromised) normally precluded from brachial plexus blockade. Given that general anesthesia and opioids could potentially impact diaphragmatic function,22 we measured diaphragm movement at baseline and 30 minutes after block, rather than postoperative period.
Although it involves manipulation of the prevertebral fascial region, we think that it is a safe method. The injection target is between the prevertebral fascia and the superficial layer of deep cervical fascia, which is shallow, and the whole length of the injection could be seen by ultrasound to avoid damage to the pleura. In this study, no patient developed pneumothorax. Although intravascular injection under ultrasound and the possibility of vascular and organ damage is small, suction is performed before injection, and the block procedures were operated by an experienced anesthesiologist.
In this study, the majority of patients (28 out of 30) acquired successful nerve blocks, which were associated with lower NRS scores at several postoperative time points. When compared to the NRS scores at postoperative 2, 4, 6, 12, and 24 hours, which were 4 (4), 4 (2), 4 (1), 3.5 (1), 3 (1), respectively, using intravenous PCA alone,23 the NRS scores were lower at all time points in this study. This suggests that the analgesic effect of the nerve blocks was both stable and long-lasting. Regarding opioid consumption (converted into OMEs), patients in the protocol consumed significantly fewer opioids (18 [12,30] mg) compared to those receiving anterior suprascapular nerve block combined with an axillary nerve block (0.375% ropivacaine 10 mL each, 58 [30,86] mg),9 ang infraclavicular-suprascapular blocks (0.25% levobupivacaine 20 mL+10 mL, 28.5±27 mg),8 which was similar to patients receiving the superior trunk block (0.5% ropivacaine 15 mL, 15 [7.5,30] mg).24 It was challenging to compare postoperative opioid consumption by any factor due to the differences in dosages, volumes and injection methods among the different studies. Nonetheless, we hypothesized that this disparity may be attributed to the following several factors. Firstly, 70% of the sensory nerve fibers of the shoulder joint are innervated by the suprascapular nerve, with the supraspinatus and infraspinatus muscles being directly innervated by this nerve; the remaining 30% are innervated by the axillary, musculocutaneous and lateral thoracic nerves.25,26 Our combined nerve blocks utilize a higher concentration of LA, which can more effectively address the analgesic requirements of the shoulder surgical site. In addition, the supraclavicular nerve, which innervates the acromioclavicular joint, runs in the prevertebral extrafascial space and may be blocked through the diffusion of LA.27 Besides, the block of the posterior subclavian brachial plexus bundle may also inhibit the subscapular nerve and the lateral thoracic nerve, resulting in an analgesic effect comparable to that of the upper trunk block. We will do further study to assess the advantages and risks associated with this technique.
Further, the QoR-15 is a valid, reliable, responsive, and simple-to-use outcome measure that can be applied across a wide range of surgical settings. A QoR-15 score of 118 or higher indicates a favorable postoperative recovery.28 In our study, the recovery scores of most patients (28 out of 30) reached a good level, suggesting that this blocking regimen can effectively facilitate the implementation of enhanced recovery after surgery. In addition, there were no complications related to the block, such as HDP, indicating a high level of safety associated with this protocol.
Our novel approach for suprascapular nerve block offers several advantages. First, visualization of the nerve itself is not required, as this technique utilizes an interfascial block. Second, the LA is administered outside the prevertebral fascia, which helps maintain the natural barrier between the drug and the phrenic nerve. Third, the medial-to-lateral injection approach facilitates diffusion of the LAs laterally. There is minimal medial spread, further reducing the risk of phrenic nerve involvement. Additionally, the technique does not require the patient to change positions, which enhances patient comfort. Therefore, the block is poised to be an appealing addition to current multimodal analgesic protocols for shoulder arthroscopy.
However, this study has several limitations. First, it is descriptive with a limited sample size; therefore, larger randomized trials are necessary to quantify the success and failure rates of the described technique. In addition, this study was designed to focus on the efficacy and safety of this new block. Future research should compare this block with other techniques to determine its role in improving surgical outcomes. Finally, further cadaveric or radiographic studies are needed to investigate drug diffusion patterns.
Conclusions
The extra-prevertebral fascial suprascapular nerve block, when combined with the infraclavicular brachial plexus block for shoulder surgery, demonstrated a rapid onset of action, a high success rate, a significantly lower incidence of diaphragmatic paralysis 30 minutes after the block, and a perioperative opioid-sparing effect. Further randomized trials are needed to determine the role of the block in enhancing surgical outcomes.
Funding Statement
There is no funding to report.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
The study was approved by the Ethics Committee of Beijing Friendship Hospital, Capital Medical University (No: 2024-P2-088-01) on April 1, 2024, and the guidelines outlined in the Declaration of Helsinki were followed. Written informed consent was obtained from all study participants.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Jenssen KK, Lundgreen K, Madsen JE, Kvakestad R, Pripp AH, Dimmen S. No functional difference between three and six weeks of immobilization after arthroscopic rotator cuff repair: a prospective randomized controlled non-inferiority trial. Arthroscopy. 2018;34(10):2765–2774. doi: 10.1016/j.arthro.2018.05.036 [DOI] [PubMed] [Google Scholar]
- 2.Uquillas CA, Capogna BM, Rossy WH, Mahure SA, Rokito AS. Postoperative pain control after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25(7):1204–1213. doi: 10.1016/j.jse.2016.01.026 [DOI] [PubMed] [Google Scholar]
- 3.Toma O, Persoons B, Pogatzki-Zahn E, Van de Velde M, Joshi GP, PROSPECT Working Group collaborators. PROSPECT guideline for rotator cuff repair surgery: systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia. 2019;74(10):1320–1331. doi: 10.1111/anae.14796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abdallah FW, Halpern SH, Aoyama K, Brull R. Will the real benefits of single-shot interscalene block please stand up? A systematic review and meta-analysis. Anesth Analg. 2015;120(5):1114–1129. doi: 10.1213/ANE.0000000000000688 [DOI] [PubMed] [Google Scholar]
- 5.Urmey WF, Talts KH, Sharrock NE. One hundred percent incidence of hemidiaphragmatic paresis associated with interscalene brachial plexus anesthesia as diagnosed by ultrasonography. Anesth Analg. 1991;72(4):498–503. doi: 10.1213/00000539-199104000-00014 [DOI] [PubMed] [Google Scholar]
- 6.Eckmann MS, Bickelhaupt B, Fehl J, et al. Cadaveric study of the articular branches of the shoulder joint. Reg Anesth Pain Med. 2017;42(5):564–570. doi: 10.1097/AAP.0000000000000652 [DOI] [PubMed] [Google Scholar]
- 7.Zhang H, Miao Y, Qu Z. Upper trunk block for shoulder analgesia with potential phrenic nerve sparing: a preliminary anatomical report one fascia, two blocks, and a concern on diaphragm-sparing. Reg Anesth Pain Med. 2019;1532–8651. doi: 10.1136/rapm-2019-100746 [DOI] [PubMed] [Google Scholar]
- 8.Aliste J, Bravo D, Finlayson RJ, Tran DQ. A randomized comparison between interscalene and combined infraclavicular-suprascapular blocks for arthroscopic shoulder surgery. Can J Anaesth. 2018;65(3):280–287. doi: 10.1007/s12630-017-1048-0 [DOI] [PubMed] [Google Scholar]
- 9.Ferre F, Pommier M, Laumonerie P, et al. Hemidiaphragmatic paralysis following ultrasound-guided anterior vs. posterior suprascapular nerve block: a double-blind, randomised control trial. Anaesthesia. 2020;75(4):499–508. doi: 10.1111/anae.14978 [DOI] [PubMed] [Google Scholar]
- 10.Dhir S, Sondekoppam RV, Sharma R, Ganapathy S, Athwal GS. A comparison of combined suprascapular and axillary nerve blocks to interscalene nerve block for analgesia in arthroscopic shoulder surgery: an equivalence study. Reg Anesth Pain Med. 2016;41(5):564–571. doi: 10.1097/AAP.0000000000000436 [DOI] [PubMed] [Google Scholar]
- 11.El-Boghdadly K, Chin KJ, Chan VWS. Phrenic nerve palsy and regional anesthesia for shoulder surgery: anatomical, physiologic, and clinical considerations. Anesthesiology. 2017;127(1):173–191. doi: 10.1097/ALN.0000000000001668 [DOI] [PubMed] [Google Scholar]
- 12.Matamis D, Soilemezi E, Tsagourias M, et al. Sonographic evaluation of the diaphragm in critically ill patients. Technique and clinical applications. Intensive Care Med. 2013;39(5):801–810. doi: 10.1007/s00134-013-2823-1 [DOI] [PubMed] [Google Scholar]
- 13.McCool FD, Tzelepis GE. Dysfunction of the diaphragm. N Engl J Med. 2012;366(10):932–942. doi: 10.1056/NEJMra1007236 [DOI] [PubMed] [Google Scholar]
- 14.Kang R, Jeong JS, Chin KJ, et al. Superior trunk block provides noninferior analgesia compared with interscalene brachial plexus block in arthroscopic shoulder surgery. Anesthesiology. 2019;131(6):1316–1326. doi: 10.1097/ALN.0000000000002919 [DOI] [PubMed] [Google Scholar]
- 15.Hertzog MA. Considerations in determining sample size for pilot studies. Res Nurs Health. 2008;31(2):180–191. doi: 10.1002/nur.20247 [DOI] [PubMed] [Google Scholar]
- 16.Siegenthaler A, Moriggl B, Mlekusch S, et al. Ultrasound-guided suprascapular nerve block, description of a novel supraclavicular approach. Reg Anesth Pain Med. 2012;37(3):325–328. doi: 10.1097/AAP.0b013e3182409168 [DOI] [PubMed] [Google Scholar]
- 17.Tedore TR, Lin HX, Pryor KO, et al. Dose-response relationship between local anesthetic volume and hemidiaphragmatic paresis following ultrasound-guided supraclavicular brachial plexus blockade. Reg Anesth Pain Med. 2020;45(12):979–984. doi: 10.1136/rapm-2020-101728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Campbell AS, Johnson CD, O’Connor S. Impact of peripheral nerve block technique on incidence of phrenic nerve palsy in shoulder surgery. Anesthesiol Res Pract. 2023;2023:9962595. doi: 10.1155/2023/9962595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang H, Qu Z, Miao Y, Jia R, Li F, Hua Z. Comparison between subparaneural upper trunk and conventional interscalene blocks for arthroscopic shoulder surgery: a randomized noninferiority trial. Anesth Analg. 2022;134(6):1308–1317. doi: 10.1213/ANE.0000000000005990 [DOI] [PubMed] [Google Scholar]
- 20.Wang H, Bao Q, Cao D, Zhu L, Chen L, Yu Y. Effect of low-volume ropivacaine in ultrasound-guided superior trunk block on diaphragmatic movement in patients undergoing shoulder arthroscopy: a randomized controlled trial. J Orthop Surg Res. 2024;19(1):604. doi: 10.1186/s13018-024-05083-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim Y, Yoo S, Kim SH, et al. Comparison between low-volume local anesthetic with intravenous dexamethasone and conventional volume without dexamethasone for superior trunk block after arthroscopic shoulder surgery: a randomized controlled non-inferiority trial. Reg Anesth Pain Med. 2024;49(8):558–564. doi: 10.1136/rapm-2023-104520 [DOI] [PubMed] [Google Scholar]
- 22.Sasaki N, Meyer MJ, Eikermann M. Postoperative respiratory muscle dysfunction: pathophysiology and preventive strategies. Anesthesiology. 2013;118(4):961–978. doi: 10.1097/ALN.0b013e318288834f [DOI] [PubMed] [Google Scholar]
- 23.Pehlivan SS, Gergin OO, Aksu R, Guney A, Guler E, Yildiz K. A randomized comparison between interscalene and combined interscalene-suprascapular blocks for arthroscopic shoulder surgery: a prospective clinical study. J Pain Res. 2024;17(1178):335–343. doi: 10.2147/JPR.S435685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim DH, Lin Y, Beathe JC, et al. Superior trunk block: a phrenic-sparing alternative to the interscalene block: a randomized controlled trial. Anesthesiology. 2019;131(3):521–533. doi: 10.1097/ALN.0000000000002841 [DOI] [PubMed] [Google Scholar]
- 25.Heron M, Dattani R, Smith R. Interscalene vs suprascapular nerve block for shoulder surgery. Br J Hosp Med. 2016;77(8):494. doi: 10.12968/hmed.2016.77.8.494 [DOI] [PubMed] [Google Scholar]
- 26.Checcucci G, Allegra A, Bigazzi P, Gianesello L, Ceruso M, Gritti G. A new technique for regional anesthesia for arthroscopic shoulder surgery based on a suprascapular nerve block and an axillary nerve block: an evaluation of the first results. Arthroscopy. 2008;24(6):689–696. doi: 10.1016/j.arthro.2008.01.019 [DOI] [PubMed] [Google Scholar]
- 27.Leurcharusmee P, Maikong N, Kantakam P, Navic P, Mahakkanukrauh P, Tran D. Innervation of the clavicle: a cadaveric investigation. Reg Anesth Pain Med. 2021;46(12):1076–1079. doi: 10.1136/rapm-2021-103197 [DOI] [PubMed] [Google Scholar]
- 28.Bu XS, Zhang J, Zuo YX. Validation of the Chinese version of the quality of recovery-15 score and its comparison with the post-operative quality recovery scale. Patient. 2016;9(3):251–259. doi: 10.1007/s40271-015-0148-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.