ABSTRACT
Context:
Adolescent girls suffer the brunt of malnutrition due to increased nutritional needs to facilitate rapid growth spurt including menstruation and increased physical activity. This vulnerable group has low social power and is subjected to peer and social pressures related to body image and weight. All these factors along with the sociocultural milieu may lead to a spectrum of nutritional problems in them.
Aims:
To determine factors associated with malnourishment among adolescent females of age 15–19 years in an urban slum of Raipur City.
Settings and Design:
The study setting was the urban field practice area of the institute in Raipur. The study was an analytical cross-sectional study done from January 2022 to June 2023 among 401 adolescent girls of age 15–19 years.
Methods and Material:
The sampling was done using the consecutive sampling method. The study tools used were a semi-structured questionnaire on sociodemographic variables and details of the respondents, anthropometric measurements, dietary assessment using the 24-hour food recall method, and food consumption patterns using a food frequency questionnaire.
Statistical Analysis Used:
The Chi-square test of significance was applied to find the association between malnourishment with the input variables. For calculating the strength of the association, the odds ratio was estimated for those variables with P value < 0.2 in the Chi-square test, and later the odds ratio was adjusted for confounding with the same variables, using multivariable logistic regression.
Results:
According to BMI-for-age Z scores, 2% were severely thin (< −3 SD), 9.7% were thin (−3 to − 2 SD), 5% were overweight (1 to 2 SD), and 1.5% were obese (>2SD). While measuring the height-for-age Z scores, 5.5% had severe stunting and 21.9% had moderate stunting. Those respondents with educational status of high school or below [AOR 3.5 (1.8–6.8), P < 0.001] and those who did not consume a non-vegetarian diet [AOR 2.1 (1.1–4.1), P = 0.02] had significantly higher adjusted odds of being undernourished (severely thin or thin) as compared to those with educational status above high school and those who consumed a mixed diet, respectively. The respondents who are currently not going to school/college had significantly higher adjusted odds [AOR 2.2 (1.2–3.8), P = 0.007] of being stunted when compared to those who are attending school/college.
Conclusions:
The significant levels of malnutrition observed in this study among late adolescent girls aged 15–19 years—11.7% undernourishment, 6.5% overnourishment, and 27.4% stunting—highlight the concerning vulnerability of this population. The higher prevalence of stunting throws light onto the chronicity of malnutrition. As seen from the significant associations, proper education, and a mixed diet will help nurture a healthy female adolescent population.
Keywords: Adolescents, dietary assessment, malnutrition, nutritional status assessment, late adolescent girls, over nourishment, stunting, undernourishment
Introduction
Adolescence, from the Latin ‘Adolescere’ meaning ‘to grow, to mature’, is defined by the World Health Organization (WHO) as 10–19 years, split into early (10–14) and late (15–19) stages.[1,2,3] Globally, there are 1.2 billion adolescents, with 87% in developing countries. In India, adolescents represent 21% of the population, with 243 million individuals.[4,5]
This developmental phase is characterized by significant physical, cognitive, and emotional changes, making adequate nutrition critical. Proper nutrition supports rapid growth and prevents long-term health issues. Adolescent girls, constituting about one-tenth of India’s population, are particularly vulnerable. They face reproductive health risks and various forms of malnutrition due to increased nutrient needs and societal pressures affecting their eating behaviour. These girls often lack social power and are subject to body image-related pressures, which can lead to unhealthy eating habits and malnutrition.[6,7]
Late adolescence is when the growth spurt stabilizes, and their nutritional status can be assessed more effectively. Among teenage girls, it is this time when most of them would have attained their menarche and thus remain vulnerable to adversities like anaemia and weakness due to inadequate nutrition to compensate for the blood loss and physical growth.
Ensuring adequate nutrition during this phase is crucial for breaking the intergenerational cycle of malnutrition and promoting healthier future generations. In the world, among the late adolescent girls of 15–19 years of age, 21% are married and these data go up to 30% in low- and middle-income countries like India.[8] Thus, pregnancy is yet another matter of concern in late adolescence. Focussing on the late adolescent girls will thus make a healthy population of pre-reproductive females who will give birth to healthy newborns, who then grow into healthy adolescents and adults, thereby stabilizing the healthcare continuum.
Malnutrition among adolescents presents as both undernutrition and overweight/obesity. The National Family Health Survey-4 (NFHS-4)[9] reported that 41.9% of Indian girls aged 15–19 were underweight, while 4.2% were overweight or obese. NFHS-5[10] showed a slight reduction in thinness (39.7%) but an increase in overweight/obesity (5.4%). Undernutrition results in stunted growth and reduced immunity, while overweight adolescents are at risk for non-communicable diseases like diabetes and hypertension.[11]
Despite several initiatives, comprehensive data and targeted interventions for adolescent nutrition in India are lacking. Adolescent health was incorporated into India’s Reproductive and Child Health (RCH) programme in 1997. The RMNCH + A programme in 2013 emphasized the nutritional status of adolescent girls, followed by the Scheme for Adolescent Girls in 2018, which focused on nutrition. The POSHAN Abhiyaan (2018) and POSHAN 2.0 (2022) further targeted late adolescent girls in underdeveloped regions. However, these efforts remain insufficient, with gaps in age- and sex-disaggregated data and a lack of robust, large-scale interventions.[12,13,14]
Urbanization has led to the growth of urban slums, home to over 65 million people in India.[15] Adolescent girls who live in urban slums are particularly vulnerable, having poor living conditions, and increased exposure to unhealthy, calorie-dense foods. These conditions increase the risk of infectious diseases, further impacting nutritional status.[16] Most studies on adolescent nutrition focus on school-going children and rural areas, leaving a significant gap in understanding the nutritional status of adolescents, particularly girls, in urban slums. Adolescents not attending school are often excluded from research, limiting the applicability of findings to the broader adolescent population.[17] Primary care physicians play a pivotal role in identifying and addressing malnutrition among adolescents as they are the first point of contact for healthcare. By understanding the specific determinants of malnutrition in this population, their approaches to screening, counselling, and treatment may be tailored through targeted interventions. This study was carried out to determine factors associated with malnourishment among adolescent females aged 15-19 years in an urban slum of Raipur city, providing insights that are directly applicable to the practice of primary care physicians.
Subjects and Methods
Study design, setting, and population
This study was a cross-sectional analytical study in the urban field practice area (UFPA) of the Department of Community and Family Medicine of AIIMS Raipur. The study population included adolescent girls aged 15–19 years who gave consent if ≥18 years and assent if <18 years, along with consent from mother/caregiver. Adolescents who were suffering from any acute illnesses (fever, cough, diarrhoea, etc.) in the previous week were excluded as their nutritional status may differ from usual.[18] Any adolescent with a known chronic disease or congenital anomaly was also excluded.
Sample size and sampling procedure
The sample size of 401 was estimated using Cochran’s Formula for sample size determination, using the prevalence of 46.1% malnutrition (both undernutrition and overnutrition) in the females of age group 15–19 according to NFHS-4, an absolute error of 5% and a non-response rate of 5%. To select survey participants from the UFPA area, a centre point was identified, and in the direction of the spinning bottle, the first street was selected, and the starting house was chosen by lottery. Subsequent houses were visited consecutively in an anticlockwise direction. One adolescent aged 15–19 was chosen per house using the Kish grid if needed.[19] The duration of the study was 1.5 years.
Variables and study instruments
Dependent variables were:
WHO BMI-for-age classification for 5–19 year old[20] according to Z scores, i.e. severe thinness (< −3 SD), thinness (−3 to < −2 SD), normal (−2 to 1 SD), overweight (>1 to 2 SD), and obese (>2 SD). Severe thinness and thinness were classified into undernourished status and overweight and obesity into overnourished status, while analysing for associations.
WHO height-for-age classification for 5–19 year old[21] according to Z scores, i.e. severe stunting (< −3 SD), moderate stunting (−3 to < −2 SD), and normal (≥ −2 SD).
Independent variables were:
Caste, single parenting, educational status of parents, occupational status of parents, socioeconomic status, type of family, vaccination history, whether respondent goes to school, educational status of the respondent, adequate calorie intake (estimated average requirement—EAR), adequate protein intake (EAR), dietary diversity, and certain food frequency patterns.
The study tools used were a semi-structured questionnaire on sociodemographic variables and details of the respondents, anthropometric measurements using an analogue weighing scale and non-stretchable measuring tape, dietary assessment using the 24-hour food recall method,[22] and food consumption patterns using food frequency questionnaire.[23]
Data Analysis: The Chi-square test of significance was applied to find the association between malnourishment with the input variables. For calculating the strength of the association, the odds ratio was estimated for those variables with P value <0.2 in Chi-square test, and later the odds ratio was adjusted for confounding with the same variables, using multivariable logistic regression.
Ethical committee approval: Ethical clearance was obtained from the Institute Ethics Committee of All India Institute of Medical Sciences, Raipur, with Ref No: AIIMSRPR/IEC/2021/944; dated 11/10/2021.
Observations and results
The data collected from 401 respondents were analysed and presented in the following tables and graphs. Table 1 gives the frequency distribution of the sociodemographic variables of the respondents.
Table 1.
Sociodemographic profile of the family of the respondent (n=401)
| Sociodemographic Profile of the Family | Frequency | % |
|---|---|---|
| Caste | ||
| SC | 38 | 9.5 |
| ST | 6 | 1.5 |
| OBC | 350 | 87.3 |
| General | 7 | 1.7 |
| Marital Status of the Parents | ||
| Married | 371 | 92.5 |
| Divorced | 1 | 0.2 |
| Separated | 3 | 0.7 |
| Widowed | 26 | 6.5 |
| Educational Status of Father | ||
| Illiterate | 57 | 14.2 |
| Literate, less than middle school certificate | 127 | 31.7 |
| Middle school certificate | 95 | 23.7 |
| High school certificate | 77 | 19.2 |
| Higher secondary certificate | 35 | 8.7 |
| Graduate degree | 10 | 2.5 |
| Educational Status of Mother | ||
| Illiterate | 102 | 25.4 |
| Literate, less than middle school certificate | 157 | 39.2 |
| Middle school certificate | 89 | 22.2 |
| High school certificate | 38 | 9.5 |
| Higher secondary certificate | 12 | 3.0 |
| Graduate degree | 3 | 0.7 |
| Occupational Status of Father * fathers of 24 (4.2%) respondents either passed away/separated/divorced | ||
| Unemployed | 6 | 3.2 |
| Unskilled worker | 120 | 29.9 |
| Semi-skilled worker | 34 | 8.5 |
| Skilled worker | 136 | 33.9 |
| Arithmetic skill jobs | 76 | 19.0 |
| Semi-professional | 3 | 0.7 |
| Professional | 2 | 0.5 |
| Occupational Status of Mother *mothers of 6 (0.5%) respondents either passed away/separated/divorced | ||
| Unemployed | 165 | 42.1 |
| Unskilled worker | 130 | 32.4 |
| Semi-skilled worker | 32 | 8.0 |
| Skilled worker | 43 | 10.7 |
| Arithmetic skill jobs | 25 | 6.2 |
| Semi-professional/professional | 0 | 0 |
| Type of Family | ||
| Nuclear | 275 | 68.6 |
| Extended | 44 | 11.0 |
| Joint | 82 | 20.4 |
| Kuppuswamy Scale of SES | ||
| Lower | 1 | 0.2 |
| Upper lower | 259 | 58.1 |
| Lower middle | 122 | 28.7 |
| Upper middle | 18 | 4.7 |
| Upper | 1 | 0.2 |
58.1% of the families belonged to the upper lower class, and 28.7% belonged to the lower middle class of the modified Kuppuswamy socio-economic scale updated to the CPI of May 2023.
Table 2 summarizes the details of the respondents. Though all of the respondents were educated at least till middle school, 19.7% of the respondents do not go to school presently.
Table 2.
Details of the respondents (n=401)
| Details of the respondents | Frequency | % |
|---|---|---|
| Age in Years | ||
| 15 | 111 | 27.7 |
| 16 | 71 | 17.7 |
| 17 | 51 | 12.7 |
| 18 | 163 | 40.6 |
| 19 | 5 | 1.2 |
| Birth Order | ||
| ≤2 | 279 | 69.6 |
| >2 | 122 | 30.4 |
| Respondent Going to School | ||
| Yes | 322 | 80.3 |
| No | 79 | 19.7 |
| Educational Status | ||
| Illiterate | 0 | 0 |
| Primary school | 0 | 0 |
| Middle school | 7 | 1.7 |
| High school | 172 | 42.9 |
| Higher secondary school | 133 | 33.2 |
| College | 89 | 22.2 |
Distribution of nutritional status according to WHO BMI-for-age Z scores and height-for-age Z scores
Figure 1 illustrates the distribution of the nutritional status according to WHO BMI for Age z scores. 2% of the respondents were severely thin (< -3 SD), 9.7% were thin (-3 to -2 SD), 5% were overweight (1 to 2 SD) and 1.5% were obese (>2SD). Figure 2 shows the classification according to the height for age Z scores: 5.5% had severe stunting and 21.9% had moderate stunting. Table 3 gives the details of the dietary assessment of the respondents. The mean calorie intake per day from 24-hour food recall, expressed as mean (SD), is 1200.4 (342.1) kcal, whereas the mean protein intake per day according to EAR is 31.2 (10.6) g.
Figure 1.
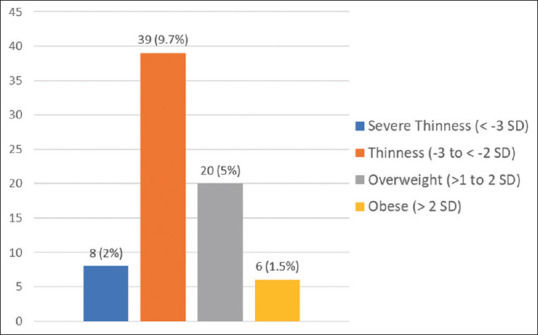
Bar diagram showing the distribution of nutritional status according to WHO BMI-for-age Z scores
Figure 2.
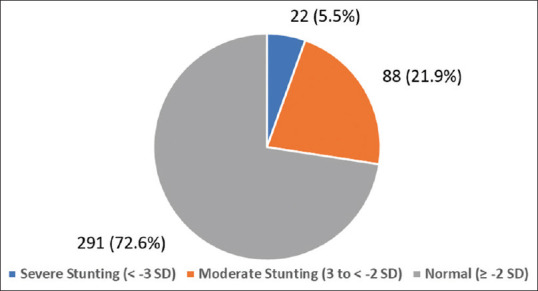
Pie chart showing the distribution of nutritional status according to WHO height-for-age Z scores
Table 3.
Dietary Assessment of the Respondents (n=401)
| Dietary Assessment | Frequency | % |
|---|---|---|
| Adequate calorie intake (EAR) per day by the 24 h recall | ||
| Yes | 8 | 2 |
| No | 393 | 98 |
| Adequate protein intake (EAR) per day by the 24 h recall | ||
| Yes | 113 | 28.2 |
| No | 288 | 71.8 |
Food consumption patterns of various food groups assessed by one-year food frequency questionnaire
All the respondents had cereals daily as a staple. 77.1% of the respondents had vegetables daily either in the form of curry or salads. 27.4% of the respondents had pulses daily. 26.9% of the respondents never had non-vegetarian foods including eggs. Milk products are consumed daily by 18.5% of the respondents. Fruits are consumed daily by 25.4% of the respondents. 53.6% of the respondents consume beverages such as tea, coffee, or packaged drinks daily. 67.6% of the respondents have snacks such as chips, panipuri, etc., daily.
For finding associations of various factors with nutritional status, the BMI-for-age categories of severe thinness and thinness was combined into ‘undernourished’ (BMI-for-age <-2SD); overweight and obese were combined into ‘overnourished’ (BMI-for-age > 2SD). Height-for-age categories of severe stunting and moderate stunting was combined into ‘stunted’ (Height-for-age <-2SD).
In Table 4 by using Chi-square test, there were statistically significant associations between the educational status of the respondent and consumption of a mixed diet, with the nutritional status according to BMI for age. The vaccination status and school going status were found to be statistically significantly associated with the nutritional status of the adolescent girls according to the height for age.
Table 4.
Association between the variables and the nutritional status of the respondents according to BMI for age and height for age (n=401)
| Nutritional status | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||||||
| BMI for age | Height for age | |||||||||||||||||
|
| ||||||||||||||||||
| Under nourished (n=47) | Normal (n=328) | Over nourished (n=26) | χ2 | P | Severe stunting (n=22) | Moderate stunting (n=88) | Normal (n=291) | χ2 | P | |||||||||
|
|
|
|
|
|
|
|||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |||||||
| Sociodemographic Profile of the Family | ||||||||||||||||||
| Caste | ||||||||||||||||||
| OBC | 42 | 89.4 | 285 | 86.9 | 23 | 88.5 | 0.3 | 0.88 | 20 | 90.9 | 77 | 87.5 | 253 | 86.9 | 0.3 | 0.86 | ||
| Other than OBC | 5 | 10.6 | 43 | 13.1 | 3 | 11.5 | 2 | 9.1 | 11 | 12.5 | 38 | 13.1 | ||||||
| Single Parenting | ||||||||||||||||||
| No | 43 | 91.5 | 303 | 92.4 | 25 | 96.2 | 0.6 | 0.75 | 21 | 95.5 | 81 | 92.0 | 269 | 92.4 | 0.3 | 0.86 | ||
| Yes | 4 | 8.5 | 25 | 7.6 | 1 | 3.8 | 1 | 4.5 | 7 | 8.0 | 22 | 7.6 | ||||||
| Educational Status of Father | ||||||||||||||||||
| Illiterate | 10 | 21.3 | 46 | 14.0 | 1 | 3.8 | 5.6 | 0.23 | 2 | 9.1 | 13 | 14.8 | 42 | 14.4 | 1.7 | 0.80 | ||
| Up to middle school | 26 | 55.3 | 182 | 55.5 | 14 | 53.8 | 15 | 68.2 | 49 | 55.7 | 158 | 54.3 | ||||||
| Above middle school | 11 | 23.4 | 100 | 30.5 | 11 | 42.3 | 5 | 22.7 | 26 | 29.5 | 91 | 31.3 | ||||||
| Educational Status of Mother | ||||||||||||||||||
| Illiterate | 16 | 34.0 | 82 | 25.0 | 4 | 15.4 | 4.8 | 0.30 | 5 | 22.7 | 22 | 25.0 | 75 | 25.8 | 0.9 | 0.93 | ||
| Up to middle school | 23 | 48.9 | 204 | 62.2 | 19 | 73.1 | 13 | 59.1 | 53 | 60.2 | 180 | 61.9 | ||||||
| Above middle school | 8 | 17.0 | 42 | 12.8 | 3 | 11.5 | 4 | 18.2 | 13 | 14.8 | 36 | 12.4 | ||||||
| Occupational Status of Father* | ||||||||||||||||||
| Skilled and above | 27 | 61.4 | 209 | 68.1 | 14 | 56.0 | 2.1 | 0.35 | 11 | 52.4 | 49 | 59.8 | 190 | 69.6 | 4.7 | 0.09 | ||
| Unemployed/Unskilled | 17 | 38.6 | 98 | 31.9 | 11 | 44.0 | 10 | 47.6 | 33 | 40.2 | 83 | 30.4 | ||||||
| Occupational Status of Mother# | ||||||||||||||||||
| Skilled and above | 7 | 15.2 | 87 | 26.9 | 6 | 23.1 | 3.0 | 0.23 | 6 | 27.3 | 19 | 21.8 | 75 | 26.1 | 0.7 | 0.70 | ||
| Unemployed/unskilled | 39 | 84.8 | 237 | 73.1 | 20 | 76.9 | 16 | 72.7 | 68 | 78.2 | 212 | 73.9 | ||||||
| Kuppuswamy Socio-economic Scale | ||||||||||||||||||
| Upper middle/upper | 3 | 6.4 | 16 | 4.9 | 0 | 0.0 | 3.9 | 0.42 | 1 | 4.5 | 2 | 2.3 | 16 | 5.5 | 2.9 | 0.59 | ||
| Lower middle | 11 | 23.4 | 100 | 30.5 | 11 | 42.3 | 5 | 22.7 | 31 | 35.2 | 86 | 29.6 | ||||||
| Lower/upper lower | 33 | 70.2 | 212 | 64.6 | 15 | 57.7 | 16 | 72.7 | 55 | 62.5 | 189 | 64.9 | ||||||
| Type of Family | ||||||||||||||||||
| Nuclear | 38 | 80.9 | 222 | 67.7 | 15 | 57.7 | 4.8 | 0.09 | 15 | 68.2 | 53 | 60.2 | 207 | 71.1 | 3.7 | 0.16 | ||
| Extended/joint | 9 | 19.1 | 106 | 32.3 | 11 | 42.3 | 7 | 31.8 | 35 | 39.8 | 84 | 28.9 | ||||||
| Details of the respondent | ||||||||||||||||||
| Age in Years | ||||||||||||||||||
| <17 | 28 | 59.6 | 140 | 42.7 | 14 | 53.8 | 5.6 | 0.06 | 9 | 40.9 | 42 | 47.7 | 131 | 45 | 0.4 | 0.82 | ||
| ≥17 | 19 | 40.4 | 188 | 57.3 | 12 | 46.2 | 13 | 59.1 | 46 | 52.3 | 160 | 55 | ||||||
| Birth Order | ||||||||||||||||||
| ≤2 | 35 | 74.5 | 227 | 69.2 | 17 | 65.4 | 0.8 | 0.68 | 12 | 54.5 | 59 | 67 | 208 | 71.5 | 3.1 | 0.21 | ||
| >2 | 12 | 25.5 | 101 | 30.8 | 9 | 34.6 | 10 | 45.5 | 29 | 33 | 83 | 28.5 | ||||||
| Vaccination History | ||||||||||||||||||
| Appropriate for age | 24 | 51.1 | 154 | 47.0 | 18 | 69.2 | 4.9 | 0.09 | 17 | 77.3 | 45 | 51.1 | 134 | 46 | 8.2 | 0.02 | ||
| Partially/not immunized | 23 | 48.9 | 174 | 53.0 | 8 | 30.8 | 5 | 22.7 | 43 | 48.9 | 157 | 54 | ||||||
| Respondent Goes to School or College? | ||||||||||||||||||
| Yes | 41 | 87.2 | 259 | 79.0 | 22 | 84.6 | 2.1 | 0.35 | 14 | 63.6 | 63 | 71.6 | 245 | 84.2 | 10.9 | 0.004 | ||
| No | 6 | 12.8 | 69 | 21.0 | 4 | 15.4 | 8 | 36.4 | 88 | 28.4 | 291 | 15.8 | ||||||
| Educational Status | ||||||||||||||||||
| >10 | 15 | 31.9 | 196 | 59.8 | 11 | 42.3 | 14.8 | 0.001 | 8 | 36.4 | 45 | 51.1 | 169 | 58.1 | 4.7 | 0.10 | ||
| ≤10 | 32 | 68.1 | 132 | 40.2 | 15 | 57.7 | 14 | 63.6 | 43 | 48.9 | 122 | 41.9 | ||||||
| Dietary assessment | ||||||||||||||||||
| Adequate calorie intake (EAR) by the 24-hour recall | ||||||||||||||||||
| Yes | 47 | 100.0 | 326 | 99.4 | 26 | 100.0 | 0.5 | 0.78 | 0 | 0 | 0 | 0 | 8 | 2.7 | 3.1 | 0.21 | ||
| No | 0 | 0.0 | 2 | 0.6 | 0 | 0.0 | 22 | 100 | 88 | 100 | 283 | 97.3 | ||||||
| Adequate protein intake (EAR) by the 24-hour recall | ||||||||||||||||||
| Yes | 28 | 59.6 | 187 | 57.0 | 12 | 46.2 | 1.5 | 0.48 | 3 | 13.6 | 25 | 28.4 | 85 | 29.2 | 2.5 | 0.29 | ||
| No | 19 | 40.4 | 141 | 43.0 | 14 | 53.8 | 19 | 19 | 86.4 | 63 | 71.6 | 206 | 70.8 | |||||
| Food frequency patterns | ||||||||||||||||||
| Vegetables daily | ||||||||||||||||||
| Yes | 32 | 68.1 | 260 | 79.3 | 17 | 65.4 | 5.1 | 0.08 | 16 | 72.7 | 62 | 70.5 | 231 | 79.4 | 3.3 | 0.19 | ||
| No | 15 | 31.9 | 68 | 20.7 | 9 | 34.6 | 6 | 27.3 | 26 | 29.5 | 60 | 20.6 | ||||||
| Pulses daily | ||||||||||||||||||
| Yes | 14 | 29.8 | 91 | 27.7 | 5 | 19.2 | 1.0 | 0.60 | 7 | 31.8 | 19 | 21.6 | 84 | 28.9 | 2.0 | 0.36 | ||
| No | 33 | 70.2 | 237 | 72.3 | 21 | 80.8 | 15 | 68.2 | 69 | 78.4 | 207 | 71.1 | ||||||
| Consumes non-vegetarian | ||||||||||||||||||
| Yes | 27 | 57.4 | 247 | 75.3 | 19 | 73.1 | 6.7 | 0.04 | 17 | 77.3 | 62 | 70.5 | 214 | 73.5 | 0.5 | 0.77 | ||
| No | 20 | 42.6 | 81 | 24.7 | 7 | 26.9 | 5 | 22.7 | 26 | 29.5 | 77 | 26.5 | ||||||
| Milk products daily^ | ||||||||||||||||||
| Yes | 11 | 23.9 | 61 | 19.9 | 2 | 8.7 | 2.3 | 0.32 | 3 | 15.0 | 13 | 15.5 | 58 | 21.3 | 1.7 | 0.43 | ||
| No | 35 | 76.1 | 246 | 80.1 | 21 | 91.3 | 17 | 85.0 | 71 | 84.5 | 214 | 78.7 | ||||||
| Fruits daily` | ||||||||||||||||||
| Yes | 14 | 29.8 | 80 | 24.6 | 8 | 30.8 | 1.0 | 0.62 | 7 | 31.8 | 19 | 21.8 | 76 | 26.3 | 1.2 | 0.56 | ||
| No | 33 | 70.2 | 245 | 75.4 | 18 | 69.2 | 15 | 68.2 | 68 | 78.2 | 213 | 73.7 | ||||||
| Beverages daily” | ||||||||||||||||||
| No | 15 | 34.9 | 129 | 42.9 | 7 | 31.8 | 1.9 | 0.40 | 7 | 31.8 | 38 | 46.3 | 106 | 40.5 | 1.8 | 0.42 | ||
| Yes | 28 | 65.1 | 172 | 57.1 | 15 | 68.2 | 15 | 68.2 | 44 | 53.7 | 156 | 59.5 | ||||||
| Snacks daily | ||||||||||||||||||
| No | 17 | 36.2 | 105 | 32.0 | 8 | 30.8 | 0.4 | 0.84 | 12 | 54.5 | 27 | 30.7 | 91 | 31.3 | 5.2 | 0.07 | ||
| Yes | 30 | 63.8 | 223 | 68.0 | 18 | 69.2 | 10 | 45.5 | 61 | 69.3 | 200 | 68.7 | ||||||
*n=376 #n=396 ^n=376 `n=398 ”n=366
Those variables which produced a Chi-square value with a significance level of P ≤ 0.2 were further analysed using simple logistic regression for obtaining the crude odds ratio and then multivariable logistic regression for the adjusted odds ratio.
In Table 5, it was found that those respondents with an educational status up to the 10th standard had 3.5 times more adjusted odds of being undernourished as compared to those with an educational status above the 10th standard and this finding is statistically significant. Those respondents who did not consume non-vegetarian were at 2.3 times more adjusted odds of being undernourished when compared to those who consumed non-vegetarian and this finding was also statistically significant. It was also found that those who did not consume vegetables daily were at 1.9 times more adjusted odds of being undernourished when compared to those who consumed vegetables daily, but this finding was not statistically significant.
Table 5.
Strength of association between the variables and undernourishment of the respondents according to BMI for age (n=375^)
| Nutritional Status | Crude OR | 95% CI | P | Adjusted OR | 95% CI | P | ||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Undernourished (n=47) | Normal (n=328) | |||||||||
|
|
|
|||||||||
| n | % | n | % | |||||||
| Type of family | ||||||||||
| Extended/joint | 9 | 19.2 | 106 | 32.3 | 0.5 | 0.2–1.1 | 0.07 | 0.5 | 0.2–1.0 | 0.05 |
| Nuclear | 38 | 80.8 | 222 | 67.7 | 1 | – | – | 1 | – | – |
| Vaccination History | ||||||||||
| Partially/not immunized | 23 | 48.9 | 174 | 53.0 | 0.9 | 0.5–1.6 | 0.60 | 0.8 | 0.4–1.5 | 0.59 |
| Appropriate for age | 24 | 51.1 | 154 | 47.0 | 1 | – | – | 1 | – | – |
| Educational Status | ||||||||||
| ≤10 | 15 | 31.9 | 196 | 59.8 | 3.2 | 1.7–6.1 | <0.001 | 3.5 | 1.8–6.8 | <0.001 |
| >10 | 32 | 68.1 | 132 | 40.2 | 1 | – | – | 1 | – | – |
| Vegetables daily | ||||||||||
| No | 15 | 31.9 | 68 | 20.7 | 1.8 | 1.0–3.5 | 0.08 | 1.9 | 1.0–3.9 | 0.07 |
| Yes | 32 | 68.1 | 260 | 79.3 | 1 | – | – | 1 | – | – |
| Consumes non-vegetarian | ||||||||||
| No | 20 | 42.6 | 81 | 24.7 | 2.3 | 1.2–4.2 | 0.01 | 2.3 | 1.1–4.1 | 0.02 |
| Yes | 27 | 57.4 | 247 | 75.3 | 1 | – | – | 1 | – | – |
^To find the association with undernourishment, 26 overnourished respondents are excluded
In Table 6, it was found that those respondents who do not go to school or college at present had 2.2 times more adjusted odds of being stunted when compared to those who are going to school or college and this finding was statistically significant. It was also found that the respondents whose fathers were unemployed or unskilled had higher unadjusted odds of 1.6 times compared to those with fathers employed in skilled jobs. This was a statistically significant finding; however, upon adjusting for confounders this finding became statistically insignificant.
Table 6.
Strength of association between the variables and stunting of the respondents according to height for age (n=401)
| Nutritional status | Crude OR | 95% CI | P | Adjusted OR | 95% CI | P | ||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| Stunted (n=110) | Normal (n=291) | |||||||||
|
|
|
|||||||||
| n | % | n | % | |||||||
| Occupational Status of Father* | ||||||||||
| Unemployed/unskilled | 43 | 41.7 | 83 | 30.4 | 1.6 | 1.0–2.6 | 0.03 | 1.5 | 0.9–2.4 | 0.12 |
| Skilled employee and above | 60 | 58.3 | 190 | 69.6 | 1 | – | – | 1 | – | – |
| Type of Family | ||||||||||
| Extended/joint | 42 | 38.2 | 84 | 28.9 | 1.5 | 1.0–2.4 | 0.07 | 1.2 | 0.7–2.0 | 0.48 |
| Nuclear | 68 | 61.8 | 207 | 71.1 | 1 | – | – | 1 | – | – |
| Vaccination History | ||||||||||
| Partially/not immunized | 48 | 43.6 | 157 | 54.0 | 0.7 | 0.4–1.0 | 0.07 | 0.7 | 0.4–1.1 | 0.13 |
| Appropriate for age | 62 | 56.4 | 134 | 46.0 | 1 | – | – | 1 | – | – |
| Respondent Goes to School or College? | ||||||||||
| No | 33 | 30.0 | 46 | 15.8 | 2.3 | 1.4–3.8 | 0.001 | 2.2 | 1.2–3.8 | 0.007 |
| Yes | 77 | 70.0 | 245 | 84.2 | 1 | – | – | 1 | – | – |
| Educational Status | ||||||||||
| ≤10 | 57 | 51.8 | 122 | 41.9 | 1.5 | 1.0–2.3 | 0.08 | 1.3 | 0.8–2.2 | 0.23 |
| >10 | 53 | 48.2 | 169 | 58.1 | 1 | – | – | 1 | – | – |
| Vegetables daily | ||||||||||
| No | 32 | 29.1 | 60 | 20.6 | 1.6 | 1.0–2.6 | 0.07 | 1.6 | 0.9–2.7 | 0.10 |
| Yes | 78 | 70.9 | 231 | 79.4 | 1 | – | – | 1 | – | – |
| Snacks daily | ||||||||||
| Yes | 71 | 64.5 | 200 | 68.7 | 0.8 | 0.5–1.3 | 0.43 | 0.9 | 0.5–1.4 | 0.57 |
| No | 39 | 35.5 | 91 | 31.3 | 1 | – | – | 1 | – | – |
*n=376
Discussion
In this study, based on BMI for age Z scores, 2% of participants were severely thin, 9.7% were thin, 5% were overweight, and 1.5% were obese. For height for age Z scores, 5.5% had severe stunting, and 21.9% had moderate stunting. Participants with a high school education or less, and those who did not have non-vegetarian diet, were more likely to be underweight compared to those with more education and those who ate a mixed diet. Additionally, those not attending school or college were more likely to be stunted compared to those who were in school or college. In a community-based cross-sectional study in 2009, by Prashant et al.,[24] among 223 adolescent girls of age 10–18 years, the prevalence of thinness (low BMI) calculated at the cut-off level of less than the 5th percentile was 20.6%. The prevalence of stunting as per Indian standard was 28.3%. This was comparable to our study.
In the cross-sectional study by Patanwar et al.[6] among 500 adolescent girls of age 16–19 years from higher secondary schools of Raipur city, Chhattisgarh, done in 2013, 53.8% were thin (BMI < 18.5), 3.6% were overweight (BMI > 25), and similar to our study, those who were vegetarian had a significantly low BMI when compared to those who were non-vegetarian. This shows the importance of inclusion of vegetables in the diet, daily.
Ganesan et al.,[25] in a school-based cross-sectional study done in rural Coimbatore, in 2014 to 2015, among 753 adolescent girls of age 10–18 years, 3.1% were severely thin, 14.5% thin, 73.2% normal, 5% overweight, and 4.2% obese, based on WHO BMI-for-age Z scores. The results were comparable with the present study.
A comparable association was found between educational status and nutritional status by Azupogo et al.[26] in their analysis of the 2014 Ghana Demographic and Health Survey Data for 15–19 Years Adolescent Boys and Girls. In the study, it was found that when compared to secondary/higher education, adolescent boys and girls of 15–19 years, who have done only primary education, were at a higher risk of stunting. This association was stronger for girls than boys. Hence, education is an important determinant of proper nourishment among adolescent girls.
In the study by Gayakwad et al.[17] in 2015–16, in Bagalkot, out of 400 study subjects, the prevalence of thinness and severe thinness was found to be 19.5% and 6.3%, respectively (total 25.8%). 4.3% of girls were overweight and 1.2% of girls were obese with the overall prevalence of overweight to be 5.5%. The prevalence of overweight and obesity was comparable to the current study. According to height for age, 24.8% were stunted and 4.5% were severely stunted (total 29.3%). This result was also similar to the current study.
In the study done by Kumar et al.[16] in 2016, 12.9% of adolescent girls of age 10–19 years had no schooling, 26.9% had schooling between 1 and 7th class, 28.0% 8–9th, and 32.2 above 10th class. In agreement with our study results, a negative association was found between the years of schooling and coexistence of thinness and stunting. Thus, the importance of education in proper nourishment of adolescent girls is being reiterated.
In 2019, Taklual et al.[27] conducted a school-based cross-sectional study in Bahir Dar City, Ethiopia, among 682 female adolescent senior secondary students of age 10–19 years; according to BMI-for-age Z scores by WHO, 102 (15%), 57 (8.4%), and 32 (4.7%) of them were found to be underweight, overweight, and obese, respectively. 12.1% of fathers and 23.2% of mothers were illiterate, comparable to our study. Participants who did not eat meat once a week were 1.6 times more likely to be underweight than those who ate meat two or more times per week (AOR: 1.6, 95% CI: 1.90–2.82). Thus, acquiring proper nutrition through the inclusion of non-vegetarian foods or vegetarian substitutes with similar nutritional value may play an important role in the good nutritional status of adolescent girls.
A cross-sectional study was conducted among 400 female adolescent students of age 15–19 years in Darchula, Nepal, by Giri et al.[28] in 2021–22. 284 (71%) had normal BMI, 99 (24.7%) were thin, and 17 (4.3%) were overweight. The main occupation of the student’s father remained significantly associated with thinness (OR = 4.384: 95% CI = 1.135–16.928). This further threw light on the importance of the employment of the guardian on the nutritional status of the late adolescent girls. In another cross-sectional study by Balat M et al among 115 female school going adolescents of Ahmedabad city of age 10-19 years, 17.4% were underweight and 16.5% were overweight according to BMI-for-age Z scores by WHO.[29] A cross-sectional study among 426 adolescent girls of 10-19 years age in an urban resettlement colony in New Delhi by Santra A et al, 18.9% were thin, 10.6% overweight and 3.9% obese according to BMI-for-age Z scores by WHO. When compared to these studies, our study deviates marginally with respect to the prevalence values, probably owing to the specific focus on the late adolescent age group.[30]
Primary care providers and family physicians are in a pivotal position to identify and address malnutrition in adolescents, especially those from urban slum areas. The significant associations found in this study—between lower educational attainment, non-vegetarian diet, and school dropping out with higher odds of malnutrition—provide actionable insights for clinical practice.
Conclusion
The significant levels of malnutrition observed in this study among late adolescent girls aged 15–19 years—11.7% undernourishment, 6.5% overnourishment, and 27.4% stunting—highlight the concerning vulnerability of this demographic segment. The higher prevalence of stunting elucidates the chronicity of malnutrition in this study population. The employment status of parents may play a role in determining malnutrition, highlighting the influence of socio-economic factors on nutritional outcomes. Moreover, the educational attainment of the girls plays a pivotal role in shaping their nutritional status, underlining the importance of education in promoting overall well-being. Ensuring a balanced diet remains essential for maintaining good nutritional health among this demographic. Incorporating a wide variety of food groups into daily dietary consumption, encompassing both vegetarian and non-vegetarian options, is vital for sustaining optimal nutritional status and supporting healthy growth and development. This study underscores the need for comprehensive, community-based approaches that involve healthcare providers, educators, and policymakers in addressing the nutritional needs of adolescents in urban slums. Such collaborative efforts can significantly contribute to the overall well-being and health equity of this vulnerable population.
Limitations
Single administration of the 24-hour food recall method may not be sufficient in assessing daily nutrient intake. Also, the adolescent girls may not have been very upfront in revealing data about their diet intake.
Strengths
Nutritional status assessment is being done using both anthropometry and dietary assessment. The dietary assessment itself is comprehensive as it involves both the 24-hour dietary recall and the food frequency questionnaire. The anthropometric measurements being done in the late adolescent population is more reliable as the growth spurt slows down.
Key messages
The need to focus on improving the socioeconomic status, educational status, and nutritious diet to deal with the high prevalence of malnutrition and the increased demands of late adolescent girls in urban slums.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Venugopal R, Varoda A, Srivastava P. Growth pattern and nutritional status of adolescent girls of Chhattisgarh. Int J Curr Res. 2016;8:36643–7. [Google Scholar]
- 2.World Health Organization, Regional Office for South-East Asia. WHO; Adolescent health in the South-East Asia Region. [[Last accessed on 2021 Jul 07]]. Available from: https://www.who.int/southeastasia/health-topics/adolescenthealth .
- 3.Bhargava M, Bhargava A, Ghate SD, Rao RS. Nutritional status of Indian adolescents (15-19 years) from National Family Health Surveys 3 and 4: Revised estimates using WHO 2007 Growth reference. PLoS One. 2020;15:e0234570. doi: 10.1371/journal.pone.0239923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization, Regional Office for South-East Asia. Adolescent Nutrition: A Review of the Situation in Selected South-East Asian Countries. New Delhi: World Health Organization; 2006. Mar, [[Last accessed on 2021 Jul 07]]. Available from: https://apps.who.int/iris/handle/10665/204764 . [Google Scholar]
- 5.Census tables. Office of the Registrar General and Census Commissioner, Ministry of Home Affairs, Government of India. [[Last accessed on 2021 Jul 07]]. Available from: https://censusindia.gov.in/census.website/data/censustables# .
- 6.Patanwar P, Sharma K. Nutritional status of Kurmi adolescent girls of Raipur city Chhattisgarh, India. [[Last accessed on 2021 Jul 25]];Int J Sci Res Publ. 2013 3 Available from: http://www.ijsrp.org/research-paper-1113/ijsrpp2335.pdf . [Google Scholar]
- 7.Kumar A. Nutritional assessment of adolescent in Punjab [Master's Thesis] New Delhi: Indira Gandhi National Open University; 2018. [Google Scholar]
- 8.World Health Organization. Adolescent Pregnancy. WHO; 2020. [[Last accessed on 2021 Jul 07]]. Jan 31. Available from: https://www.who.int/news-room/factsheets/detail/adolescent-pregnancy . [Google Scholar]
- 9.International Institute for Population Sciences. National Family Health Survey (NFHS-4) 2015-16. Mumbai: Ministry of Health and Family Welfare (MoHFW), Government of India; 2017. Dec, [[Last accessed on 2021 Jul 25]]. Available from: http://rchiips.org/nfhs/NFHS-4Reports/India.pdf 13 . [Google Scholar]
- 10.International Institute for Population Sciences. National Family Health Survey 2019-21 (NFHS-5) Mumbai: Ministry of Health and Family Welfare (MoHFW), Government of India; 2021. Sep, [[Last accessed on 2023 June 20]]. Available from: http://rchiips.org/nfhs/NFHS-5_FCTS/India.pdf . [Google Scholar]
- 11.Leroy J L, Ruel M, Frongillo E A, Harris J, Ballard TJ. Measuring the food access dimension of food security: A critical review and mapping of indicators. Food Nutr Bull. 2015;36:167–95. doi: 10.1177/0379572115587274. [DOI] [PubMed] [Google Scholar]
- 12.Gupta A, Kumar R, Khera A, Agrawal D, Mohan A, Pandey R, et al. A Strategic approach to reproductive, maternal, newborn, child and adolescent health in India for healthy mother and child. 2013. pp. 1–83. Available from: https://nhm.gov.in/images/pdf/RMNCH+A/RMNCH+A_Strategy.pdf .
- 13.Ministry of Women and Child Development, Government of India. Scheme for Adolescent Girls: Administrative Guidelines 2018. Ministry of Women and Child Development, Government of India; 2018 Aug 31. [[Last accessed on 2023 Jul 25]]. Available from: https://164.100.94.126/sites/default/files/Administrative%20guidelines%20for%20implementation%20of%20Scheme%20for%20Adolescent%20Girls.pdf .
- 14.Ministry of Women and Child Development, Government of India. Saksham Anganwadi and Poshan 2.0: Scheme Guidelines. Ministry of Women and Child Development, Government of India; 2022. [[Last accessed on 2023 Aug 12]]. Available from: https://wcd.gov.in/documents/uploaded/Mission%20Saksham%20Anganwadi%20and%20Poshan%202.0%20scheme%20guidelines.pdf .
- 15.Slum population-census 2011. Office of the Registrar General and Census Commissioner, Ministry of Home Affairs, Government of India. [[Last accessed on 2023 May 31]]. Available from: https://www.census2011.co.in/slums.php .
- 16.Kumar P, Srivastava S, Chauhan S, Patel R, Marbaniang SP, Dhillon P. Associated factors and socio-economic inequality in the prevalence of thinness and stunting among adolescent boys and girls in Uttar Pradesh and Bihar, India. PLoS One. 2021;16:e0247526. doi: 10.1371/journal.pone.0247526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gayakwad VS, Shankar G. Nutritional status of adolescent girls residing in the urban field practice area of S. N. Medical College, Bagalkot. Indian J Public Health Res Dev. 2020;11:448–52. [Google Scholar]
- 18.Ministry of Health and Family Welfare (MoHFW), Government of India, UNICEF, Population Council. Comprehensive National Nutrition Survey (CNNS) National Report. New Delhi: MoHFW; 2019. [[Last accessed on 2021 Jul 28]]. Available from: https://nhm.gov.in/WriteReadData/l892s/1405796031571201348.pdf . [Google Scholar]
- 19.Nemeth R. Respondent selection within the household - A modification of the Kish grid [Internet] ResearchGate. 2001. [[Last accessed on 2021 Jul 28]]. Available from: https://www.researchgate.net/publication/237794222_Respondent_Selection_Within_the_Household-A_Modification_of_the_Kish_Grid .
- 20.World Health Organisation. BMI-for-age (5-19 years) WHO; 2007. Available from: https://www.who.int/tools/growthreference-data-for-5to19-years/indicators/bmi-for-age . [Google Scholar]
- 21.Cashin K, Oot L. Guide to Anthropometry: A Practical Tool for Program Planners, Managers, and Implementers. Washington, DC: Food and Nutrition Technical Assistance III Project (FANTA); 2018. [[Last accessed on 2023 May 24]]. Available from: https://www.fantaproject.org/sites/default/files/resources/FANTAAnthropometry-Guide-May2018.pdf . [Google Scholar]
- 22.Gerald J, Dorothy R. International Dietary Data Expansion Project (INDDEX). 24-hour dietary recall. Tufts University. Friedman School of Nutrition Science and Policy. [[Last accessed on 2021 Jul 02]]. Available from: https://inddex.nutrition.tufts.edu/data4diets/data-source/24-hour-dietaryrecall-24hr .
- 23.Lin P-I, Bromage S, Mostofa Md, Allen J, Oken E, Kile M, et al. Validation of a Dish-based semiquantitative food questionnaire in rural Bangladesh. Nutrients. 2017;9:49. doi: 10.3390/nu9010049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prashant K, Shaw C. Nutritional status of adolescent girls from an urban slum area in South India. Indian J Pediatr. 2009;76:501–4. doi: 10.1007/s12098-009-0077-2. [DOI] [PubMed] [Google Scholar]
- 25.Ganesan S, Chacko TV, Muhammad GM. Are our rural adolescents eating healthy?Implications for redesigning school health interventions-A cross sectional study in rural Coimbatore. Indian J Public Health. 2019;63:293–7. doi: 10.4103/ijph.IJPH_420_18. [DOI] [PubMed] [Google Scholar]
- 26.Azupogo F, Abizari AR, Aurino E, Gelli A, Osendarp SJM, Bras H, et al. Malnutrition, hypertension risk, and correlates: An analysis of the 2014 Ghana demographic and health survey data for 15–19 years adolescent boys and girls. Nutrients. 2020;12:1–23. doi: 10.3390/nu12092737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taklual W, Baye S, Mekie M, Andualem T. Double Burden of Malnutrition among Female Adolescent Students in Bahir Dar City, Amhara, Ethiopia. Biomed Res Int. 2020;2020:6249524. doi: 10.1155/2020/6249524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Giri D, Vajanapoom N, Langkulsen U. Factors influencing undernutrition among female adolescent students in Darchula District, Nepal. Nutrients. 2023;15:1699. doi: 10.3390/nu15071699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Balat M, Vidja J, Patel M, Algotar PD. A study on dual burden of malnutrition among 387 school going adolescents of Ahmedabad city. Natl J Physiol Pharm Pharmacol 388. 2023;13:2089–93. [Google Scholar]
- 30.Santra A, Rai S, Misra P, Yadav K, Goswami K, Kaur G. Comparison of Different 390 Anthropometric Indicators for Assessment of Nutritional Status Among Adolescent 391 Girls in an Urban Resettlement Colony in New Delhi: A Cross-Sectional Study. Cureus. 392. 2023;15:e37242. doi: 10.7759/cureus.37242. [DOI] [PMC free article] [PubMed] [Google Scholar]


