ABSTRACT
Background:
Adolescent substance abuse is a growing public health concern. Adolescence is the starting point for adult substance misuse. The likelihood of acquiring dependence in adulthood is significantly decreased when substance use is not initiated during adolescence. The purpose of this study was to estimate the prevalence of substance use among teenagers, as well as to determine the age of initiation and identify the factors that are linked to substance use.
Methods:
A community-based cross-sectional study was conducted in an urban community in Vellore by a tertiary care teaching hospital. A structured questionnaire was administered by the principal investigator to all adolescent boys aged between 10 and 19 years residing in that area for the past year who gave informed consent/assent to assess the prevalence of substance use among teenagers.
Results:
The total number of adolescent boys enrolled in the study was 266. The mean (standard deviation [SD]) age of the participants was 16.14 (2.2) years, with a median age of 16 years. Out of the 266 adolescent boys, 33.8% are currently using substances and 15% were past users. The common substance used was smoking tobacco (30%), followed by alcohol consumption (29%). The minimum age of initiation of smoking tobacco and ganja use was 9 and 7 years, respectively. Significant predictors of substance usage included the participant’s educational background and the substance use of their parents.
Conclusion:
According to this community-based study’s findings, smoking tobacco was the most frequently used substance by teenagers, with a higher prevalence of current substance use. Substance misuse in the family was substantially associated with increased drug usage among teenagers. Notwithstanding having an adequate comprehension of the negative results of substance utilisation, teenagers develop this habit, which they might carry into adulthood. It is therefore necessary to establish comprehensive prevention and control programs in schools and the community that target teenagers and their parents.
Keywords: Abuse, adolescent, alcohol, smoking, substance, tobacco
Background
Substance use is a major public health problem in both developed and developing nations.[1,2] Today, no place in the world is free from substance abuse. India is also affected by it, especially adolescents, and the numbers of individuals using substances are increasing each day.[3] The consumption of different types of substances has been prevalent in India for many centuries.[4,5] The earliest substance used was alcohol, dating back to the year 2000 BC. The use of cannabis and opium has been prevalent in different societies for centuries.[6]
In the last decade, India has witnessed accelerated economic growth. India has also experienced profound social changes associated with economic reforms, global travel, and exposure to Western media, advertising, fashion, and lifestyle. This is thought to have resulted in a shift in recreational activities among adolescent individuals.[7] Although India has made progress towards achieving the Millennium Development Goals, the health sector shows a slower progress rate, especially with regard to adolescent health.[8]
In India, many surveys have been conducted to address the prevalence of substance use using the door-to-door survey method.[9,10] Very few studies have been conducted in the community to establish the prevalence of substance use in India. Such studies will clarify the problems associated with substance use in the community and initiate specific interventional measures to address them. Since there is limited data on the pattern and factors associated with substance use in the community, a community-based cross-sectional study was carried out among adolescent males in the urban slums of Vellore, Tamil Nadu, Southern India, to assess the prevalence of substance use among them and the factors associated with it.
Materials and Methods
Study setting
A community-based cross-sectional study was conducted to estimate the prevalence of substance use among the adolescent males in an urban community of Vellore by a low-cost effective care unit (LCECU) of a tertiary care teaching hospital in Vellore between January 2017 and December 2017. Within a radius of two to three kilometres from the base hospital, LCECU provides care for nearly 2400 households spread over five areas of Vellore town. This study was approved by the Institutional Review Board and Ethics Committee (IRB No. 10526; dated 01 February 2017).
Inclusion and exclusion criteria
All adolescent boys aged between 10 and 19 years residing in that area for the past year and who gave informed consent/assent were included. Adolescent boys who were unable to communicate due to physical or mental disabilities, and those who were under 18 years old and whose parent or legal guardian were unavailable to give consent for them were excluded. Also, adolescent girls were excluded from the study to avoid possible negative repercussions from the family.
Sample size and design
The sample size was calculated based on a previous community-based study conducted among urban adolescents in Sambalpur, Orissa, with a prevalence of 43.4%.[11] Using the formula n = 4pq/d2, where p = 0.43, q = 0.57, and d = 6% absolute precision, the sample size was calculated to be 272. A systematic random sampling method was adopted in this study. The first house was chosen by a random method, following which every eighth house was included. If the selected house did not have a male adolescent who met the criteria, the next house was selected. If a house had more than one eligible participant, the lot method was used to choose one participant. The details of the study were explained to the participants.
Study tool
The participants meeting the inclusion criteria were enrolled in this study after receiving written informed consent, whereas assent was obtained for those who were less than 18 years of age. The structured questionnaire was administered by the principal investigator in the local language. The questionnaire was primarily based on the Youth Risk Behaviour Surveillance System (YRBSS) and Car, Relax, Alone, Forget, Friends (CRAFT).[12] Additionally, socio-demographic details, particulars of substance use, activities related to substance use, and substance use among family members were also collected. Two bilingual translators translated the questionnaire from English to Tamil which was then translated back to English by another two bilinguals to verify the meaning of the questions.
Data analysis
The EpiData software, version 3.1, was used to enter the data and was analysed using Statistical Package for the Social Sciences (SPSS) version 24. The prevalence of substance use, frequency of use, age at initiation, as well as the risk factors associated with substance use, such as age, parental education and occupation, education of the participant, socio-economic status of the family, and substance use among the family members, and reasons attributed to substance use were dichotomized. For continuous and discrete variables such as the age of the participants, age at initiation, duration, and amount of substance use, the mean and standard deviation (SD) were calculated. A Chi-square test and odds ratio (OR) with a 95% confidence interval (CI) were calculated to analyse the factors that are associated with substance use. A bivariate analysis was done to check for associations between various factors and substance use.
Results
Socio-demographics
Of the 282 adolescent boys who were contacted, 266 were enrolled in the study and 16 declined to take part. The profile of the study participants is described in Table 1. The participant ages ranged from 11 to 19 years old, with a mean (SD) of 16.14 (2.2) years and a median age of 16.0 years. Nearly half of the participants belonged to the mid-adolescent age group and had studied up to high school. The majority of the adolescents (91.7%) were from nuclear families. The fathers of 43 participants (16.2%) and the mothers of 77 participants (28.9%) had never attended school. Only the fathers of two participants (0.8%) and the mother of one participant (0.4%) had been to college.
Table 1.
Socio-demographic distribution of the study participants
| Variables | Number (%) |
|---|---|
| Age in years | |
| Early adolescent (10–14) | 56 (21.1) |
| Mid-adolescent (15–17) | 125 (46.9) |
| Late adolescent (18–19) | 85 (32.0) |
| Education | |
| Primary school (1–5) | 11 (4.1) |
| Middle school (6–8) | 57 (21.4) |
| High school (9–10) | 128 (48.1) |
| Higher secondary (11–12) | 52 (19.5) |
| College | 18 (6.7) |
| Occupation | |
| Student | 163 (61.3) |
| Skilled | 48 (18.0) |
| Unskilled | 38 (14.3) |
| Unemployed | 12 (4.5) |
| Small business | 5 (1.9) |
| Type of family | |
| Nuclear | 244 (91.7) |
| Joint/extended | 22 (8.3) |
| Living with parents | |
| Both parents | 210 (78.9) |
| With father or mother | 45 (16.9) |
| No parents | 11 (4.2) |
Prevalence of substance abuse among adolescents
According to this study, 15% of adolescents had previously used drugs in any form, and 33.8% of adolescents are current substance users. Among the participants, 29.7% (n = 79) currently smoke and 28.9% (n = 77) of the adolescent’s drink alcohol. Only a small fraction (1.9%) of substance users, both past and present, reported using sniffing solutions or chemicals. Table 2 highlights the prevalence of current and past substance use among adolescents. In this study, the median age of adolescents using smoking and chewing tobacco products was 14 years and 14.5 years, whereas the mean age of adolescents using smoking and chewing tobacco products was 13.6 and 14.9 years, respectively. Adolescents who used both alcohol and ganja had a median age of 15 years, while their mean ages were 14.8 and 14.4, respectively. The mean and median age of adolescents using the sniffing solution were 13.9 and 14 years, respectively [Figure 1]. The minimal age to start using chewing tobacco and sniffing solution was 8 years old, while the minimum age to start using alcohol and tobacco was 9 years old [Figure 2]. However, the age to start using marijuana was just 7 years old. According to this study, 82% of the parents drank alcohol, 87.6% used drugs of any kind, 9.4% used ganja, and 77.8% and 16.2% of the parents had a history of using smoking tobacco and chewing tobacco, respectively.
Table 2.
Prevalence of current and past substance use among adolescents (n=266)
| Substance | Past users number (%) | Current users number (%) | 95% CI (current users) |
|---|---|---|---|
| Smoking tobacco | 39 (14.7) | 79 (29.7) | 27.4–32 |
| Chewing tobacco | 14 (5.3) | 47 (17.7) | 16–19.3 |
| Alcohol use | 37 (13.9) | 77 (28.9) | 27–30.8 |
| Ganja use | 25 (9.4) | 32 (12) | 10.6–13.4 |
| Sniffing solution/chemical | 5 (1.9) | 5 (1.9) | 1.3–2.4 |
| Any substance use | 40 (15) | 90 (33.8) | 31.8–35.8 |
Figure 1.
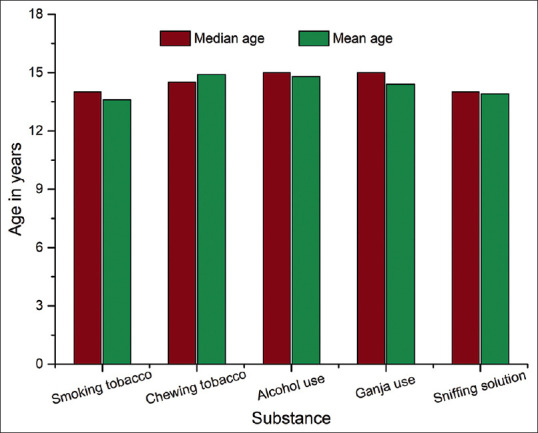
Distribution of median and mean age of participants with initiation of substance use
Figure 2.
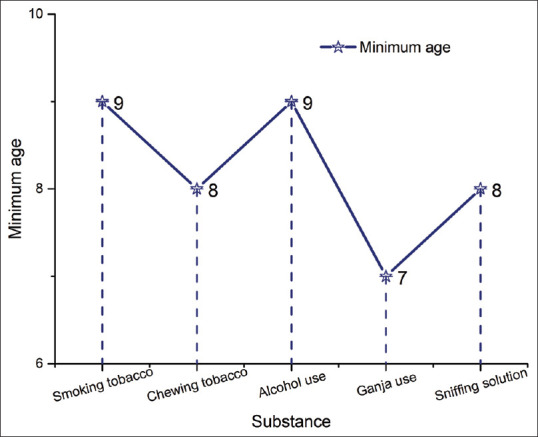
Distribution of participants according to age of initiation of substance use
Factors related to substance abuse
The majority of participants highlighted peer pressure, stress relief, happiness, and experimentation as their primary reasons for using drugs. Also, the adolescents mentioned that they could easily buy these substances from the shops on their own, or they could ask their friends to get them for them. The results of this study highlight that 94% of participants had attended raven parties either under the influence of drugs or not, and 35% of both current and past users had driven vehicles after substance use. In this study, 46 (51.1%) of the current substance users desired to quit substance use due to a progressive decline in academic performance, constant pressure from the parents, or major side effects. Following substance use, 18% of the participants have observed a significant decline in their academic performance. In addition, 7.5% of the participants said that consuming drugs had led them into trouble. The day-to-day activities were affected by 10.5% of the participants. Table 3 describes the type of substance abuse as well as the frequency of use.
Table 3.
Type of substance use and its frequency
| Substance | Type of substance | Frequency of use |
|---|---|---|
| Smoking tobacco | Beedi, cigarette | 10–15 times/day |
| Alcohol | Beer, rum, brandy | 1–3 times/week |
| Chewing tobacco | Hans | 1–3 times/day |
| Ganja | Leaf powder | 1–3 times/week |
| Solution | Whitener, gum patch solution | 1–3 times/day |
Risk factors influencing current substance use
The association between the risk of substance use and the following factors such as age, education, current educational status, living with parents and a family member with a history of using any substance was analysed and tabulated in Table 4. All the above variables were cross-tabulated after dichotomization to obtain the OR along with the P-value for significance. In the bivariate analysis, age between 15 and 19 years (OR: 5.56; 95% CI: 2.28–13.54; P-value <0.001), not currently studying (OR: 12.17; 95% CI: 6.65–22.25; P-value <0.001), living with a single parent or no parent (OR: 0.51; 95% CI: 0.280.92; P-value 0.038) and having a family member with a history of using any substance (OR: 2.4; 95% CI: 1.1–5.49; P-value 0.017) were significantly associated with higher risk of using substances.
Table 4.
Factors influencing current substance use
| Variables | Current user | Current non-user | P | Odds ratio (95% CI) | ||
|---|---|---|---|---|---|---|
|
|
|
|||||
| No | % | No | % | |||
| Age (years) | ||||||
| 15–19 | 84 | 40 | 126 | 60 | <0.001* | 5.56 (2.28–13.54) |
| 11–14 | 6 | 10.7 | 50 | 89.3 | ||
| Education | ||||||
| Up to 12th grade | 72 | 36.7 | 124 | 63.3 | 0.107 | 0.59 (0.32–1.1) |
| >12th grade | 18 | 25.7 | 52 | 74.3 | ||
| Currently studying | ||||||
| No | 67 | 66.3 | 34 | 33.7 | <0.001* | 12.17 (6.65–22.25) |
| Yes | 23 | 13.9 | 142 | 86.1 | ||
| Parent available | ||||||
| No/single parent | 26 | 46.4 | 30 | 53.6 | 0.038* | 0.51 (0.28–0.92) |
| Both parents are available | 64 | 30.5 | 146 | 69.5 | ||
| Family member using the substance | ||||||
| Yes | 85 | 36.5 | 148 | 63.5 | 0.017* | 2.4 (1.1–5.49) |
| No | 5 | 15.2 | 28 | 84.8 | ||
*P-value of 0.05 or less is statistically significant
Discussion
Drug abuse is a persistent issue in both developed and developing countries. This never-ending cycle of substance abuse is also engulfing India, with the number of cases rising daily.[13] Drug use usually starts during the teenage years, but teen drug users are rarely seen in treatment centres. The global public health issue of adolescent substance use persists, and further research is necessary to determine the true prevalence of substance use. Community-based programs are therefore helpful for preventing and treating substance abuse among children and teenagers.
Of the adolescents in this study, 48% were in high school and one-third of the participants were not currently enrolled in education at school. This contrasts with two studies that were carried out in the urban slums of Sambalpur, where 52% of the participants were school dropouts, and Mumbai, where 44% of the participants were school dropouts.[7] The low dropout rate could probably be due to the effective implementation of compulsory high school education in the state. It was noted that 29% of the participants’ mothers and 16% of their fathers had never attended school. Merely 3% of fathers and 41.9% of mothers had completed higher secondary education. The lower educational status of the parents could be the reason for the higher prevalence of substance use among teenagers. A similar outcome was noted in a study carried out in secondary schools in Sarajevo and Gracanica.[14] This study found that most of the participants (79%) were living with both parents, which is similar to the study conducted in Sarajevo city, where 70% of respondents lived with both parents, and 22% lived with a single parent.[15]
A total of 34% of adolescents were found to be current users of any substance, including tobacco chewers (18%), drinkers (29%), smokers (30%), and ganja users (12%). These results are comparable to a study done on upper secondary school students in Imphal, Manipur, where the participants’ highest prevalence of tobacco use was 46%, followed by alcohol use (29%).[16] A study conducted among school-going male adolescents in Dehradun district, Uttarakhand, showed that the most common form of tobacco use among them was smokeless tobacco use (56%), followed by smoking tobacco forms (33%) and consuming alcohol (9%).[12] According to a study done on street children in Delhi, the prevalence of using smokeless tobacco was 44%, smoking tobacco was 24%, and alcohol use was 22%.[13] The mean age of initiation for alcohol use and chewing tobacco was 15 years, and for smoking tobacco, it was 14 years, as opposed to the 12 years observed in a study carried out in government schools in Noida.[13] Another study indicated that teenagers in the urban slums of Udupi district in Karnataka started smoking and drinking alcohol on average at the age of 16.8 years.[15] As compared to these studies, the age of initiation of substance use in our study was earlier. This could be due to parental use, poor socio-economic status, and low educational level. Also, these results imply that there are regional differences in the onset age of substance use.
In this study, 88% of the parents used drugs of any kind, including smokeless tobacco; of those, 78% were smokers and 82% drank alcohol. The prevalence of substance abuse among rural and urban adolescents with a family history of substance use was found to be 35% and 29%, respectively, in a study conducted among students in Gangtok, Sikkim, but the prevalence among adolescents without a family history of substance use was found to be 13.3% and 8.8%, respectively.[17] According to this study, adolescents were also more likely to use drugs if there was a family history of substance abuse. According to a study conducted in Sambalpur, Orissa, adolescents from broken families are the ones who use drugs the most (51%).[7] This finding is consistent with another study done on children living in slums in Bangalore, which found that 55% of the adolescents who abuse substances belong to broken families.[18] This study reveals that adolescents who were older than 14 years old, lived in broken families, or had a family member who had used drugs in the past were among the groups most at risk of substance use.
The effects of substance use after many years of use were examined. Numerous studies conducted in the community have demonstrated that adolescents who abuse substances are more likely to experience extreme violence, marital disharmony, traffic accidents, sexual abuse, and antisocial behaviour.[19,20] According to the results of our study, 94% of participants attended rave parties, whether they were under the influence of drugs or not, and 35% of participants including both current and past drug users drove vehicles under the influence of a substance. Approximately 18% of the participants reported that their academic performance worsened after the initiation of substances. The majority of respondents stated that their main reasons for using drugs were peer pressure, stress relief, experimentation, and happiness. Most of the participants either had acquaintances who could deliver it for them or were able to buy these substances from the stores on their own. 51.1% of the current drug users said they wanted to quit substance use because of the significant side effects, the steadily declining academic performance, and the ongoing parental pressure.
Due to its community-based design and urban setting, this study has limitations that may prevent it from accurately representing the entire population. Only male adolescents were included in this study, which may not accurately represent the true prevalence of substance use in the community. Finally, given that this is a delicate subject, underreporting may have happened.
A few physical, psychological, psychosocial, and legal issues can arise from substance use disorder, which is a curable mental illness.[21] As a result, this creates a significant burden on the affected individuals and their families. This might lead to anxiety, depression, personality disorders and schizophrenia.[22] Through a variety of mutual support programs, there are numerous efficient community-based interventions and therapies available to assist families and individuals struggling with substance use. The interventions include engaging the family members to facilitate their involvement in the care plan, educating them about the ill effects of drugs, offering them emotional support, and identifying the early warning signs of relapse.
Conclusion
The findings of this community-based study indicated a high prevalence of current substance use, with smoking tobacco being the most used substance among adolescents. Furthermore, this study finds that 51.1% of participants were willing to give up drugs because of the significant side effects, ongoing parental pressure, and a progressive decline in academic performance. Despite having a sufficient understanding of the negative consequences of substance use, teenagers develop this habit, which they may carry into adulthood. Thus, comprehensive prevention and control programs aimed at teenagers and their parents must be implemented in schools and the community. Reducing this serious issue will require intervention activities that address the risk factors, adverse effects, and long-term effects of substance use.
List of abbreviations
| Abbreviation | Definition |
|---|---|
| WHO | World Health Organisation |
| YRBSS | Youth Risk Behaviour Surveillance System |
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
| Name | Role |
|---|---|
| Dr. Ann Helan Prasad | Technical help |
| Dr. Finlay Godson | Material support |
References
- 1.Lo TW, Yeung JWK, Tam CHL. Sustance abuse and public health: A multilevel perspective and multiple responses. Int J Environ Res Public Health. 2020;17:2610. doi: 10.3390/ijerph17072610. doi:10.3390/ijerph 17072610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mclellan AT. Substance misuse and substance use disorders: Why do they matter in healthcare? Trans Am Clin Climatol Assoc. 2017;128:112–30. [PMC free article] [PubMed] [Google Scholar]
- 3.Ganguly K. Pattern and process of drug and alcohol use in India. ICMR Bull. 2008;38:1–8. [Google Scholar]
- 4.Somasundaram O, Raghavan DV, Murthy AGT. Drinking habits in ancient India. Indian J Psychiatry. 2016;58:93–6. doi: 10.4103/0019-5545.174396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crocq MA. Historical and cultural aspects of man's relationship with addictive drugs. Dialogues Clin Neurosci. 2007;9:355–61. doi: 10.31887/DCNS.2007.9.4/macrocq. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nath A, Choudhari SG, Dakhode SU, Rannaware A, Gaidhane AM, Dakhode S, et al. Substance abuse amongst adolescents: An issue of public health significance. Cureus. 2022;14:e31193. doi: 10.7759/cureus.31193. doi:10.7759/cureus. 31193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sârbu EA, Marici M, Bostan S, Gavrila-Ardelean L. Physical and recreational activities, sedentary screen time, time spent with parents and drug use in adolescents. Int J Environ Res Public Health. 2023;20:1434. doi: 10.3390/ijerph20021434. doi:10.3390/ijerph 20021434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.India_and_the_MDGs_0.pdf. [Last accessed on 2024 Mar 03]. Available from:https://www.unescap.org/sites/default/files/India_and_the_MDGs_0.pdf .
- 9.Avasthi A, Basu D, Subodh BN, Gupta PK, Malhotra N, Rani P, et al. Pattern and prevalence of substance use and dependence in the Union Territory of Chandigarh: Results of a rapid assessment survey. Indian J Psychiatry. 2017;59:284–92. doi: 10.4103/psychiatry.IndianJPsychiatry_327_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61:807–16. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- 11.Sarangi L, Acharya HP, Panigrahi OP. Substance abuse among adolescents in urban slums of Sambalpur. Indian J Community Med. 2008;33:265–7. doi: 10.4103/0970-0218.43236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.CRAFFT-2.0_Clinician-Interview.pdf. [Last accessed on 2024 Mar 03]. Available from:https://crafft.org/wp-content/uploads/2019/02/CRAFFT-2.0_Clinician-Interview.pdf .
- 13.Sharma B, Arora A, Singh K, Singh H, Kaur P. Drug abuse: Uncovering the burden in rural Punjab. J Family Med Prim Care. 2017;6:558–62. doi: 10.4103/2249-4863.222037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mesic S, Ramadani S, Zunic L, Skopljak A, Pasagic A, Masic I. Frequency of substance abuse among adolescents. Mater Sociomed. 2013;25:265–9. doi: 10.5455/msm.2013.25.265-269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Licanin I. Impact of parental attitude to adolescents who abuse drugs. Med Arh. 2009;63:278–9. [PubMed] [Google Scholar]
- 16.Ningombam S, Hutin Y, Murhekar MV. Prevalence and pattern of substance use among the higher secondary school students of Imphal, Manipur, India. Natl Med J India. 2011;24:11–5. [PubMed] [Google Scholar]
- 17.Tsering D, Pal R, Dasgupta A. Substance use among adolescent high school students in India: A survey of knowledge, attitude, and opinion. J Pharm Bioallied Sci. 2010;2:137–40. doi: 10.4103/0975-7406.67005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Benegal V, Bhushan K, Seshadri S, Karott M. Drug abuse among street children in Bangalore. A project in Collaboration between NIMHANS, Bangalore and the Bangalore Forum for street and working children. CRY. 1998. [Last accessed on 2018 Aug 28]. [Internet] Available from:http://www.nimhans.ac.in/child-and-adolescent-psychiatry/research .
- 19.Bergen HA, Martin G, Richardson AS, Allison S, Roeger L. Sexual abuse, antisocial behaviour and substance use: Gender differences in young community adolescents. Aust N Z J Psychiatry. 2004;38:34–41. doi: 10.1111/j.1440-1614.2004.01295.x. [DOI] [PubMed] [Google Scholar]
- 20.Lo TW, Tse JWL, Cheng CHK, Chan GHY. The association between substance abuse and sexual misconduct among macau youths. Int J Environ Res Public Health. 2019;16:1643. doi: 10.3390/ijerph16091643. doi:10.3390/ijerph 16091643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.US Department of Health and Human Services. Substance use and cooccurring mental disorders. National Institute of Mental Health. 2022 [Google Scholar]
- 22.Ennis E, Bunting BP. Family burden, family health and personal mental health. BMC Public Health. 2013;13:255. doi: 10.1186/1471-2458-13-255. [DOI] [PMC free article] [PubMed] [Google Scholar]


